Abstract
Background: In recent years, evidence has been accumulating linking subjective tinnitus to the somatosensory system. Somatic tinnitus is defined as tinnitus in which forceful contractions of jaw and neck muscles modulate the psychoacoustic attributes of tinnitus, such as pitch and loudness. Being a somatosensory-based treatment modality, needling might well be more effective for treating somatic than nonsomatic tinnitus.
Objective: The aim of this study was to compare the outcomes of electroacupuncture (EA) treatment between patients with somatic and nonsomatic tinnitus.
Materials and Methods: A single-blinded prospective study was carried wherein 27 patients with tinnitus were divided into either a somatic or a nonsomatic group, based on whether their tinnitus could be modulated by at least one of a series of forceful jaw and neck muscular contraction maneuvers. Tinnitus responses were evaluated after a single session of EA on selected acupoints for 30 minutes.
Results: Seventeen of the 27 patients (63.0%) studied were found to have somatic tinnitus. Generalized estimating equation model analysis did not find any overall statistically significant difference in EA response between patients with somatic and nonsomatic tinnitus. However, patients with somatic tinnitus who were consistent in their responses to the muscular contraction maneuvers were more likely to improve with EA than variable responders to these maneuvers (62.5% versus 22.0%).
Conclusions: EA did not provide increased benefits for patients with somatic tinnitus, compared to those with nonsomatic tinnitus overall. However, within the somatic tinnitus group, a subpopulation of patients appeared to be relatively more responsive to EA treatment.
Keywords: : Tinnitus, Somatic Tinnitus, Acupuncture, Electroacupuncture
Introduction
With an estimated prevalence of 10%–15%, tinnitus is a common symptom with about 20% of adult sufferers requiring clinical intervention.1 For many years, tinnitus was thought to arise almost exclusively from abnormal neuronal activity within the auditory pathways and the resultant compensatory adaptation of the central auditory system, presumably because tinnitus commonly occurs in people with hearing loss.
In recent years, however, tinnitus-related neuronal activity is believed to be much more complex and multimodal than previously thought. Evidence has been accumulating linking subjective tinnitus to the somatosensory system and, therefore, identifying and managing the effects of the somatosensory system in patients with tinnitus is important.2
Acupuncture has been used to treat tinnitus for more than 4000 years in Traditional Chinese Medicine (TCM) practice and is still widely used for this indication. Although there are reports that suggest acupuncture is beneficial for tinnitus, acupuncture has not been demonstrated to be efficacious as a treatment for tinnitus with evidence from rigorous randomized controlled trials.3 Marks et al.,4 however, pointed out that it was challenging to study treatment of a symptom such as tinnitus, which has multiple etiologies; a treatment may work for some etiologies but not for others. There may well be small subgroups of people with tinnitus for whom acupuncture is effective but could not be identified unless very large numbers of study subjects were accrued to distinguish these small groups of responders from the whole population of people with tinnitus.
Somatic tinnitus is defined as tinnitus for which forceful contractions of the jaw and neck muscles can modulate the psychoacoustic attributes of the tinnitus, such as pitch and loudness.5,6 This can be used to identify a subgroup of patients with tinnitus who are responsive to somatic stimulation and, therefore, are optimal candidates for somatosensory-based treatment.7 Interestingly, osteopathic physicians have studied this connection and have used manual manipulative medicine to help patients with somatic tinnitus.8 Acupuncture is a modality of somatosensory-based treatment, and Levine et al.9 opined that many of the patients with tinnitus who are responders to acupuncture are, in fact, people with somatically induced tinnitus.
The aim of this study was to compare the outcomes of electroacupuncture (EA) treatment between patients with somatic and nonsomatic tinnitus.
Materials and Methods
A single-blinded prospective study was carried out on patients presenting with tinnitus. This study was approved by the local ethical committee (the SingHealth Centralized Institutional Review Board). Written informed consent was obtained from each subject before enrollment.
The patients were divided into either a somatic or a nonsomatic group, based on whether their tinnitus could be modulated by contractions of jaw and neck muscles. The hearing of each patient was assessed by pure tone audiograms. The effect of acupuncture on the loudness of tinnitus was assessed using a visual analogue scale (VAS) and on the status of the outer hair cells in the cochleae, using transient-evoked otoacoustic emissions (TEOAE). The VAS and TEOAE findings in the somatic-modulation–responsive group were compared with the somatic-modulation–nonresponsive group.
Study Subjects
Patients studied were adults presenting with tinnitus in an ear with a hearing level of 25 dB or better averaged over 250–2000 Hz. The ear studied was considered to have a hearing loss if the average frequency over 250–8000 Hz was 25 dB or worse. For those with bilateral tinnitus, the ear studied was the side where the tinnitus was louder. Where the loudness in both sides was the same, the side chosen was at random. Exclusions were patients on medications for alleviation of tinnitus; or the inability to understand the instructions, perform voluntary contraction maneuvers, or report the effects of the maneuvers on tinnitus. The acupuncturist and the person doing the VAS and TEOAE tests were blinded to whether a patient belonged to the somatic-modulation–positive or –negative group.
Somatic Maneuvers
A series of somatic maneuvers adapted from Levine et al.9 were performed to evaluate if modulation of tinnitus occurred (Box 1). In a sound-treated acoustic room, the subjects were asked if the forceful contractions of the relevant jaw and neck muscles had momentarily changed the psychoacoustic attributes of tinnitus, such as pitch and loudness. These exercises were aimed to identify a subgroup of patients whose tinnitus could be modulated by at least one of this series of maneuvers and thus serve as a comparison to those patients whose tinnitus could not be modulated.
Box 1.
Forceful Muscle Contraction Maneuvers to Identify Patients with Somatic Tinnitus
| Jaw contractions |
| Patients were instructed to perform the following jaw maneuvers (restorative pressure is maximal pressure applied by the examiner in an attempt to restore the original resting position of the jaw): |
| 1. Clench teeth together forcefully. |
| 2. Maximally open mouth, with and without restorative pressure. |
| 3. Maximally protrude jaw, with and without restorative pressure. |
| 4. Maximally slide jaw to left, with and without restorative pressure. |
| 5. Maximally slide jaw to right, with and without restorative pressure. |
| 6. Maximally retract jaw |
| Head-and-neck contractions |
| With the head in the neutral position, contractions were made to resist maximal pressure applied by the examiner to the: |
| 1. Forehead |
| 2. Occiput |
| 3. Vertex |
| 4. Mandible (upward) |
| 5. Left temple |
| 6. Right temple |
| Instructions to the patients were: |
| 7. With the head turned to the left, maximally resist the tortional force on the left zygoma. |
| 8. With the head turned to the right, maximally resist the tortional force on the right zygoma. |
| 9. With the head turned to the right and tilted to the left, maximally resist force applied to the left temple (left sternocleidomastoid). |
| 10 With the head turned to the left and tilted to the right, maximally resist force applied to the right temple (right sternocleidomastoid). |
Loudness of Tinnitus
The loudness of tinnitus was assessed with a VAS with a scale of 0–10.
TEOAE Recordings
TEOAE recordings were performed in a soundproof room using an ILO 292 device. Recordings were made using nonlinear clicks at regular 80-ms pulses, rarefaction polarity, and a repetition frequency of 50 cycles per second. A series of 260 stimuli were computed in 8-click blocks for each test, according to the nonlinear technique. The intensity used was 80 dB ±3dBpeSPL [3 decibel peak equivalent sound pressure level].
Acupuncture
Done in a sound-treated acoustic room, acupuncture needling was performed on the side where tinnitus was reported. For patients who complained of bilateral tinnitus, needling was done on the side where tinnitus was more intense; or on a side chosen randomly when both sides were the same.
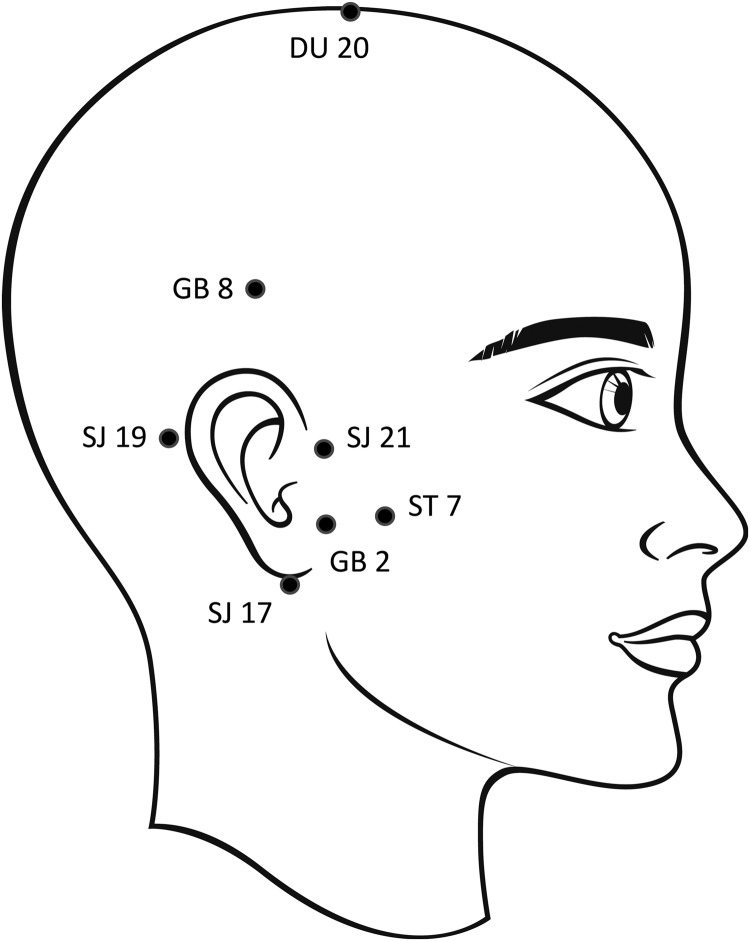
Acupuncture in either group was performed mainly by a government-accredited TCM physician with 30 years of clinical experience in acupuncture treatment (Acupuncturist A). An alternative government-accredited acupuncturist (a Western-trained otologist with a graduate diploma in acupuncture and who has 10 years of acupuncture experience) carried out the procedure using the same techniques in 5 patients (2 in the acupuncture responsive and 3 in the nonresponsive groups; Acupuncturist B). A single session, using the following acupoints was carried out: Shuaigu (GB 8); Ermen (SJ 21); Tinghui (GB 2); Yifeng (SJ 17); Luxi (SJ 19); Baihui (DU 20); and Xiaguan (ST 7). See Figure 1. The acupoints were selected based on standard textbooks on acupuncture.10–12
FIG. 1.
Acupoints used in the study. Electroacupuncture was performed by applying sparse and dense electrical pulse waves across: (1) GB 8 and SJ 21 (2) GB 2 and ST 7.
The acupuncture needles used were disposable 0.25 × 25 mm, G = 32, sterile stainless-steel needles (Huan Qiu, China, ISO9001:2008/ISO13485:2003 certified). A total of 7 needles were used. The skin was cleaned with an alcohol swab before acupuncture was administered. Depending on the points selected, needles were inserted 10–20 mm deep into the skin.
The needling technique was such that the needle was placed at an appropriate angle, rotated until De Qi was achieved, and left in situ for 30 minutes. Throughout this period, sparse and dense electrical pulse waves (100 Hz) generated from a low-frequency electric pulse machine (Acu-Stimulator, G-6805-II) was applied to the following pairs of acupoints: (1) Shuaigu (GB 8) and Ermen (SJ 21) and (2) Tinghui (GB 2) and Xiaguan (ST 7).
VAS and TEOAE were measured at 3 different times: (1) before acupuncture; (2) at the conclusion of acupuncture; and (3) 30 minutes after acupuncture. In addition, the VAS score was also recorded the day following the acupuncture.
Statistical Analysis
The generalized estimating equation (GEE) model was used to examine differences from baseline in scores between the patients with and without responses to somatic maneuvers. Each score was standardized; an interaction term between visit and group was examined for its significance by means of the GEE model. Within-person correlation in outcomes was correctly accounted for in the model using the appropriate covariance structure as determined by the quasi-information criteria. Data analysis was performed in R3.1.3 and level of significance was set at 5%.
Results
Of the 27 patients studied, 17 (63.0%) had somatic and 10 (37.0%) had nonsomatic tinnitus. There were 19 patients with normal hearing and 8 patients with hearing loss. Among the patients with somatic tinnitus, only 4 (23.5%) had hearing loss. The results of the GEE model analysis are listed in Table 1. The GEE model did not show any statistically significant different mean change from baseline to any follow-up period between patients with somatic and nonsomatic tinnitus.
Table 1.
Results from the Gee Model, Comparing Mean Change of Tinnitus Based on the VAS and TEOAE, from Baseline in Outcomes Between Patients With and Without Response to Somatic Maneuvers
| Mean (95% CI) | |||
|---|---|---|---|
| Test | Patients without response | Patients with response | P-value |
| VAS | |||
| Change immediately after acupuncture | −0.2 (−0.45, 0.05) | −0.06 (−0.5, 0.39) | 0.587 |
| Change 30 minutes after acupuncture | −0.3 (−0.58, −0.02) | −0.24 (−0.58, 0.11) | 0.777 |
| Change 1 day after acupuncture | −0.35 (−0.63, −0.07) | 0.07 (−0.47, 0.61) | 0.175 |
| TEOAE (dBSPL) | |||
| Change immediately after acupuncture | 2.09 (−0.62, 4.8) | 0.02 (−0.65, 0.69) | 0.145 |
| Change 30 minutes after acupuncture | −4.68 (−12.05, 2.69) | 0.25 (−0.3, 0.8) | 0.191 |
GEE, generalized estimating equation; VAS, visual analogue scale; TEOAE, transient-evoked otoacoustic emissions; CI, confidence interval; dBSPL, decibel sound pressure level.
The responses to the series of muscular contraction maneuvers for each patient were analyzed further, as shown in Tables 2 and 3. Some somatic tinnitus patients had responses that were consistent (i.e., the responses to maneuvers in the same individual had all resulted in either an increase or decrease in the intensity of tinnitus). In contrast, other patients with somatic tinnitus had responses to the maneuvers that resulted in increased as well as decreased loudness of tinnitus in the same individual. While the proportion of all patients with somatic tinnitus in the needling-responsive and -nonresponsive groups were 58.3% (7 of 12 patients) and 66.7% (10 of 15 patients), respectively, the proportion of patients with somatic tinnitus who had consistent responses to muscular contraction maneuvers were 41.7% (5 of 12 patients) and 20.0% (3 of 15 patients), respectively.
Table 2.
Subjects Who Had Improvement After Electroacupuncture
| Improvement after acupuncture (%) | |||||||
|---|---|---|---|---|---|---|---|
| Subject | Age (in years) | Sex | Hearing | # of maneuvers with a change in tinnitus responses | I | II | III |
| 1a | 19 | M | Normal | 6↑ | 60.0 | 60.0 | 60.0 |
| 2b | 51 | F | Normal | 2↑ | 33.3 | 33.3 | 33.3 |
| 3a | 41 | M | Loss | Nil | 0 | 0 | 25.0 |
| 4a | 43 | M | Normal | 5↓, 6↑, | 0 | 25.0 | 25.0 |
| 5a | 64 | F | Loss | Nil | 0 | 0 | 16.7 |
| 6a | 52 | F | Normal | Nil | 16.7 | 33.3 | 50.0 |
| 7b | 59 | M | Loss | Nil | 28.6 | 28.6 | 28.6 |
| 8a | 45 | F | Normal | 2↓, 5↑ | 16.7 | 16.7 | 25.0 |
| 9a | 61 | M | Normal | Nil | 50.0 | 50.0 | 75.0 |
| 10a | 52 | F | Normal | 8↓ | 16.7 | 16.7 | 16.7 |
| 11a | 60 | F | Loss | 9↓ | 33.3 | 33.3 | 33.3 |
| 12a | 48 | F | Normal | 1↑ | 16.7 | 16.7 | 16.7 |
Acupuncturist A.
Acupuncturist B.
↓ = decrease; ↑ = increase in loudness of tinnitus in response to a somatic maneuver.
I = conclusion of acupuncture; II = 30 minutes after acupuncture; III = 1 day after acupuncture.
M, male; F, female.
Table 3.
Subjects Who Had No Improvement After Electroacupuncture
| Subject | Age (in years) | Sex | Hearing | # of maneuvers with a change in tinnitus responses |
|---|---|---|---|---|
| 1a | 51 | F | Normal | 4↓, 2↑ |
| 2a | 49 | F | Normal | Nil |
| 3a | 76 | F | Normal | 4↓, 5↑ |
| 4a | 55 | F | Loss | 10↑ |
| 5a | 66 | F | Normal | Nil |
| 6a | 61 | F | Loss | 4↓, 5↑ |
| 7a | 34 | F | Normal | 4↓, 8↑ |
| 8a | 40 | M | Normal | 1↓ |
| 9a | 46 | M | Normal | 1↓ |
| 10a | 74 | F | Normal | Nil |
| 11b | 47 | M | Normal | 2↓, 5↑ |
| 12a | 49 | M | Normal | Nil |
| 13a | 56 | M | Normal | 5↓, 6↑ |
| 14b | 63 | M | Loss | 6↓, 8↑ |
| 15b | 79 | M | Loss | Nil |
Acupuncturist A.
Acupuncturist B.
↓ = decrease; ↑ = increase in loudness of tinnitus in response to a somatic maneuver.
M, male; F, female.
The same set of data could also be interpreted such that consistent responders to muscular contraction maneuvers had a 62.5% (5 of 8) chance of being needling-responsive, while variable responders to muscular contraction maneuvers had only a 22% (2 of 9) chance. Patients who did not respond to muscular contraction maneuvers had a 50% (5 of 10) chance of being needling-responsive.
Discussion
Relationship Between Tinnitus and Head/Neck Disorders
The physiologic relationship among the ear, jaw, and facial musculature has been observed for many years. In the well-described Costen syndrome, various otologic symptoms such as pain, deafness, blockage, and tinnitus are related to temporomandibular joint (TMJ) dysfunction. It has been observed that there was an increased prevalence of somatoform disorders in individuals with tinnitus.13 There have also been reports of tinnitus occurring after dental pulpagia that resolved after endodontic therapy.14 Tinnitus has been noted to be associated with upper craniocervical imbalances, such as prolapsed intervertebral discs or instability of the craniocervical junction, which resolved following stabilization surgery.15 Tinnitus occurs more frequently in patients who have craniocervical and mandibular disorders such as TMJ joint dysfunction.16–18
Neural Connections
These observations suggest that there are neural connections between the somatosensory and auditory centers. Indeed, it has been shown that the trigeminal and dorsal root ganglia relay afferent somatosensory information from the periphery to secondary sensory neurons in the brainstem, specifically the spinal trigeminal nucleus and dorsal column nuclei (DCN) respectively.5 Each of these structures was shown to send excitatory projections to the cochlear nucleus. Activation of the trigeminal ganglion elicited excitation in some DCN units and inhibition in others. The modulation of firing rate and synchrony in DCN neurons by somatosensory input was shown to be physiologically correlated with somatic tinnitus.
It has also been suggested that changes in auditory perception with somatic testing were due to changes in otoacoustic emissions (OAE).6 Acupuncture has, indeed, been shown to increase the amplitude of OAE, suggesting an effect on the activity of the outer hair cells.19 It is believed that the efferent system modulates outer hair-cell movement through the medial olivocochlea tract. However, the present study did not show any statistical difference in OAE changes between the somatic and nonsomatic groups.
Somatic Tinnitus
For many years, tinnitus was thought to arise almost exclusively from abnormal neuronal activity within the auditory pathways. Treatment has conventionally been based on such an assumption and, not surprisingly, is far from satisfactory for many patients. Not a disease in and of itself, tinnitus is actually a symptom that can be associated with multiple causes and aggravating cofactors, including the somatosensory system. It has been shown that up to 65% of patients have tinnitus that can be modulated by certain somatic maneuvers involving the jaw and head/neck contractions. The present study revealed that this was especially prevalent in patients without hearing loss. Won et al.7 identified factors that could modulate tinnitus with forceful contraction of the neck and jaw muscles. In females, buzzing tinnitus tended to decrease, whereas loud and low-pitched tinnitus tended to increase with muscle contraction.
According to Sanchez and Rocha,2 tinnitus was more likely to be somatically related if it was unilateral or asymmetrical tinnitus in the presence of symmetrical pure tone thresholds in both ears. Levine20 remarked that somatic tinnitus had often been underappreciated and stated that a belief that identification and appropriate treatment of this subgroup could lead to better outcomes. There is evidence to suggest that this subgroup of patients respond to somatosensory-based treatment such as acupuncture.9,21
The present study showed that, overall, whether or not a patient's tinnitus could be modulated by muscular contraction maneuvers did not predict the patient's response to EA. However, if the consistency of responses to muscular contraction maneuvers was considered, patients who reported only increased or decreased (but not both) loudness of tinnitus to these maneuvers appeared to be more responsive to needling. This could well be a subpopulation of patients with somatic tinnitus for whom somatically based treatment programs have a higher success rate.
Comparing the Pain and Tinnitus Models
Unlike for tinnitus, acupuncture has widely been accepted as an effective treatment modality for pain.22 Marks et al.4 examined the relationship of tinnitus to pain and made an interesting theoretical case for the possible use of acupuncture in the treatment of tinnitus. The researchers pointed out that neural reflex arcs, consisting of afferent and efferent components, existed in both auditory and pain neural systems. In particular, efferent neurons that had become intimately associated with the modality of pain, might have relevance in treatment of tinnitus. After all, it had been shown that the efferent olivocochlear bundle of Rasmussen, when stimulated, reduced both sound-evoked and spontaneous activity in the auditory nerve.
To illustrate, the researchers gave the example of local anesthetic agents such as lignocaine, which had been observed to cause a transient, and occasionally prolonged, effect in reducing or abolishing tinnitus. The researchers used the phenomenon of masking to illustrate a similarity. They pointed out that, for centuries, it had been observed that counterirritation alleviated painful stimuli. This led Melzac and Wall23 to propose the “gate theory” of pain. In this theory, it was postulated that the threshold for painful stimuli could be raised by suppressing the transmission of pain impulses in the dorsal horn, by the activity of the descending (efferent) pathways acting on these synapses. These researchers argued that masking might work in the auditory system in a similar way. In both pain and tinnitus, a refractory period of symptom relief could occur after treatment had ceased. In the case of pain, it is now widely accepted that endorphins are released that act on opiate receptors within the pain pathways, resulting in a sustained period of symptom relief. The researchers suggested that, in tinnitus, a similar mechanism might well exist in the auditory pathways.
Acupuncture for Tinnitus
Based on the clinical practice guideline for tinnitus, the American Academy of Otolaryngology–Head and Neck Surgery did not recommend against using acupuncture for the treatment of tinnitus.1 Instead, it is placed under the category of “no recommendation,” which implies that clinicians should feel little constraint in their decision making and be alert to new published evidence that clarifies the balance of benefits versus harms; and that patient preference should have a substantial influencing role.
Okada et al.24 observed patients experiencing immediate relief of tinnitus after a single session of acupuncture. Levine et al.9 also described a patient having tinnitus relief after a single session of acupuncture. The present study, based on a single session of acupuncture, did not show any statistically significant difference between the somatic and nonsomatic groups immediately, 30 minutes, and 1 day after treatment. It is possible that having multiple sessions of acupuncture administered over a period of time might work better than just a single session. Marks et al.4 believed that some patients responded to acupuncture only if the course of treatment lasted for more than 2 weeks.
A more-targeted approach in the choice of acupoints might also have led to a better treatment outcome. In a preliminary study on needling of the head and neck myofascial trigger points in patients with tinnitus, 25% of patients had complete cessation of tinnitus and another 25% experienced significant improvement.17 Another strategy could be based on the concept of scalp acupuncture. Okada et al.24 demonstrated the successful use of a point located 6.5 cm above the apex of the ear pavilion in the temporoparietal region. Located in the cochlear–vestibular area, as defined by the principles of scalp acupuncture, this point's precise identification was aided by the use of an acupuncture-point locating device.
From a TCM perspective, tinnitus could result from different etiologies. Emotions, such as anger, fright, and fear, could potentially lead to a reversal of the movement of Wind and Fire of the Liver and Gall Bladder, which, in turn, could result in blockage of the Shaoyang channels. Blockage could also be a result of Phlegm and Heat retention. Deficiency of Kidney Qi as well as Kidney and Liver essence could lead to malnutrition of the ear. In the present study, the same standard acupoints were applied to all subjects regardless of the underlying etiologies. In future studies, one could consider assigning acupoints based on TCM differentiation for each subject.
Conclusions
Tinnitus is common and yet, its treatment is far from satisfactory in many patients. The present study, based on a single session of EA on specific acupoints, failed to demonstrate increased benefits in patients with somatic tinnitus as compared to those with nonsomatic tinnitus, overall. However, within the somatic tinnitus group, a subpopulation of patients whose tinnitus was modulated in a consistent way by a series of forceful head and jaw muscular contractions was relatively more responsive to EA treatment. This observation should be substantiated by more elaborate and rigorous studies.
Acknowledgments
The support from Barrie Tan, MBBS, FRCS, Head of the Department of Otolaryngology at Singapore General Hospital, is much appreciated.
Author Disclosure Statement
The authors declare that no competing financial interests exist.
References
- 1.Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: Tinnitus. Otolaryngol Head Neck Surg. 2014;151(2[suppl]):S1–S40 [DOI] [PubMed] [Google Scholar]
- 2.Sanchez TG, Rocha CB. Diagnosis and management of somatosensory tinnitus: Review article. Clinics (Sao Paulo). 2011;66(6):1089–1094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park J, White AR, Ernst E. Efficacy of acupuncture as a treatment for tinnitus: A systematic review. Arch Otolaryngol Head Neck Surg. 2000;126(4):489–492 [DOI] [PubMed] [Google Scholar]
- 4.Marks NJ, Emery P, Onisiphorou C. A controlled trial of acupuncture in tinnitus. J Laryngol Otol. 1984;98(11):1103–1109 [DOI] [PubMed] [Google Scholar]
- 5.Shore S, Zhou J, Koehler S. Neural mechanisms underlying somatic tinnitus. Prog Brain Res. 2007;166:107–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abel MD, Levine RA. Muscle contractions and auditory perception in tinnitus patients and nonclinical subjects. Cranio. 2004;22(3):181–191 [DOI] [PubMed] [Google Scholar]
- 7.Won JY, Yoo S, Lee SK, Choi HK, Yakunina N, Le Q, Nam EC. Prevalence and factors associated with neck and jaw muscle modulation of tinnitus. Audiol Neurootol. 2013;18(4):261–273 [DOI] [PubMed] [Google Scholar]
- 8.Arab AM, Nourbakhsh MR. The effect of cranial osteopathic manual therapy on somatic tinnitus in individuals without otic pathology: 2 case reports with 1 year follow up. Int J Osteopath Med. 2014;17(2):123–128 [Google Scholar]
- 9.Levine RA, Nam EC, Oron Y, Melcher JR. Evidence for a tinnitus subgroup responsive to somatosensory based treatment modalities. Prog Brain Res. 2007;166:195–207 [DOI] [PubMed] [Google Scholar]
- 10.Cheng XN. Chinese Acupuncture and Moxibustion, 3rd printing. Beijing: Foreign Language Press; 1987 [Google Scholar]
- 11.Zuo YF, Zhoa JS, eds. Chinese Acupuncture and Moxibustion: A Newly Complied Practical English–Chinese Library of Traditional Chinese Medicine. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine; 2002 [Google Scholar]
- 12.Liu GW, Akira H, eds. Clinical Acupuncture and Moxibustion. Beijing: Huaxia Publishing House; 2006 [Google Scholar]
- 13.Hiller W, Janca A, Burke KC. Association between tinnitus and somatoform disorders. J Psychosom Res. 1997;43(6):613–624 [DOI] [PubMed] [Google Scholar]
- 14.Wright EF, Gullickson DC. Dental pulpalgia contributing to bilateral preauricular pain and tinnitus. J Orofac Pain. 1996;10(2):166–168 [PubMed] [Google Scholar]
- 15.Montazem A. Secondary tinnitus as a symptom of instability of the upper cervical spine: Operative management. Int Tinnitus J. 2000;6(2):130–133 [PubMed] [Google Scholar]
- 16.Chole RA, Parker WS. Tinnitus and vertigo in patients with temporomandibular disorder. Arch Otolaryngol Head Neck Surg. 1992;118(8):817–821 [DOI] [PubMed] [Google Scholar]
- 17.Morgan DH. Tinnitus of TMJ origin: A preliminary report. Cranio. 1992;10(2):124–129 [DOI] [PubMed] [Google Scholar]
- 18.Gelb H, Gelb ML, Wagner ML. The relationship of tinnitus to craniocervical mandibular disorders. Cranio. 1997;15(2):136–143 [DOI] [PubMed] [Google Scholar]
- 19.de Azevedo RF, Chiari BM, Okada DM, Onishi ET. Impact of acupuncture on otoacoustic emissions in patients with tinnitus. Braz J Otorhinolaryngol. 2007;73(5):599–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine RA. Tinnitus: Diagnostic approach leading to treatment. Semin Neurol. 2013;33(3):256–269 [DOI] [PubMed] [Google Scholar]
- 21.Latifpour DH, Grenner J, Sjödahl C. The effect of a new treatment based on somatosensory stimulation in a group of patients with somatically related tinnitus. Int Tinnitus J. 2009;15(1):94–99 [PubMed] [Google Scholar]
- 22.Ning Z, Lao L. Acupuncture for pain management in evidence-based medicine. J Acupunct Meridian Stud. 2015;8(5):270–273 [DOI] [PubMed] [Google Scholar]
- 23.Melzack R, Wall PD. Pain mechanisms: A new theory. Science. 1965;150(3699):971–979 [DOI] [PubMed] [Google Scholar]
- 24.Okada DM, Onishi ET, Chami FI, Borin A, Cassola N, Guerreiro VM. Acupuncture for tinnitus immediate relief. Braz J Otorhinolaryngol. 2006;72(2):182–186 [DOI] [PMC free article] [PubMed] [Google Scholar]