Abstract
Objectives
Epidemiological studies suggest that cyclothymic disorder is the most prevalent subtype of bipolar disorder (BD). However, it is rarely diagnosed, especially in youth. This may be because it can be difficult to ascertain whether a youth meets diagnostic criteria. Clearer, easy-to-apply criteria could reduce misdiagnosis. The objective of this study was to determine whether proposed research diagnostic criteria for cyclothymic disorder (RDCyc), based on DSM-5 criteria, could be quantified and validated in youth.
Methods
Participants from the Longitudinal Assessment of Manic Symptoms (LAMS) study were recruited based on symptoms of mania and followed prospectively. RDCyc criteria were: 1) At least one core symptom each of mania and depression; 2) one additional symptom of mania and of depression; 3) persistence over two consecutive six-month periods, and 4) impairment. Exclusionary criteria were having a [hypo]manic or depressive episode. Outcomes at the two-year follow-up were compared between RDCyc youth and other diagnostic groups (BD I/II, BD NOS/non-RDCyc cyclothymic disorder, disruptive behavior disorders [DBD], depression).
Results
Thirty-seven youth met RDCyc criteria. There were no consistent differences between the RDCyc youth and youth with other BD subtypes (ps=.001–.960, with all-but-one p value >.02). RDCyc youth had higher depression (p<.0005) and mania scores (p=.001), lower functioning (p=.012), and higher suicide risk than DBD youth (p=.001). They had higher mania scores than depressed youth (p.018).
Limitations
The majority of youth in the sample were recruited due to elevated symptoms of mania, which may limit the generalizability of the results. Youth were followed for two years, which may not be long enough to determine whether or not they will eventually develop a manic or depressive episode.
Conclusions
Applying RDCyc criteria identified youth who were similar to others with BD and were more impaired than those with DBD. Using these criteria could reduce misdiagnosis and increase our understanding of this prevalent, but largely ignored, diagnosis.
Keywords: cyclothymic disorder, diagnosis, youth, longitudinal
Mood lability and irritability are common among youth with mental health problems, and there has been debate about how best to classify these symptoms (Geller et al., 2002; Leibenluft and Stoddard, 2013; Vidal-Ribas et al., 2016). Cyclothymic disorder – a chronic form of bipolar disorder, characterized by less extreme mood states – could be one valid diagnostic “home” for some of these cases. However, despite the fact that cyclothymic disorder has been listed in the DSM since its third revision (American Psychiatric Association, 1980), and epidemiological studies suggest that it is one of the most prevalent mood disorders (Van Meter et al., 2011a; Van Meter et al., 2012b), it is very rarely diagnosed – particularly in young people (Van Meter and Youngstrom, 2012; Youngstrom et al., 2005). Studies of youth who do not meet criteria for bipolar I or II are almost always labeled bipolar disorder not otherwise specified, or BP-NOS (or, in the DSM-5 nomenclature, other specified bipolar disorder – for the purposes of brevity and clarity, we will use the term “BP-NOS” in this paper to refer to those youth who have a bipolar spectrum disorder that does not meet criteria for bipolar I, bipolar II, or cyclothymic disorder).
One reason posed for the mismatch between epidemiological data, which suggest that cyclothymic disorder is prevalent, and the low/nonexistent rate of clinical or research diagnoses, is that the criteria are too vague and difficult to ascertain with any degree of accuracy, particularly in clinical settings where time and resources are limited. Given the degree of specificity (i.e., must have both hypomanic and depressive symptoms for at least one year, without ever having met criteria for a hypomanic, manic, or depressive episode) and the need for long-term (one year+) retrospective recall (American Psychiatric Association, 2013), accurately making this diagnosis requires a lot of attention to detail from clinicians and informants. Consequently, other diagnostic categories (e.g., BP-NOS) tend to be used instead (Jensen-Doss et al., 2014; Youngstrom, 2009). An accurate diagnosis can make a significant difference in the outcomes a young person can achieve by guiding personalized, evidence-based intervention. Currently, because the diagnosis of cyclothymic disorder is so rarely made, we know little about how – or if – its course and treatment response differ from other childhood disorders. And, because youth who meet criteria for cyclothymic disorder are often misdiagnosed, our information about the diagnostic groups to which they are usually (incorrectly) assigned is also imperfect (Van Meter and Youngstrom, 2012).
We do not yet have clear longitudinal data demonstrating whether cyclothymic disorder and BP-NOS share similar trajectories over time. What we do know is that the diagnostic criteria for cyclothymic disorder require chronicity of symptoms, whereas, in some cases, BP-NOS is diagnosed due to brevity of symptoms (Axelson et al., 2006). Further, we know that some youth with mood symptoms that do not meet criteria for bipolar I or bipolar II (i.e., cyclothymic disorder and BP-NOS) tend to get better over time, while others get worse, and some stay about the same (Birmaher et al., 2009; Birmaher et al., 2014; Cicero et al., 2009); without distinguishing cyclothymic disorder for BP-NOS in these studies, the inferences we can make are limited.
Being able to predict the expected trajectory of a youth with significant mood problems is valuable; youth with bipolar disorder usually require pharmacological intervention to manage their symptoms, but the medications prescribed can have significant side effects (Lauxen Peruzzolo et al., 2013). However, some youth who experience significant mood lability may outgrow it (Birmaher et al., 2009; Cicero et al., 2009); if we were able to predict these cases, a more conservative approach to treatment could be taken.
With more systematically-defined groups, the process of diagnostic validation – including treatment response and long-term outcome (Robins and Guze, 1970) can gain stronger footing. The primary objective of the present study was to determine whether a research operational definition based on the DSM-5 criteria for cyclothymic disorder could be quantified and validated in a sample of youth. The Research Diagnostic Criteria (RDC) were originally developed to improve reliability of psychiatric diagnoses (Ghaemi et al., 2008; Perugi et al., 2015; Spitzer et al., 1978). Our goal is consistent with objective of improving reliability; by clearly quantifying criteria for cyclothymic disorder and making the criteria easier to apply, researchers and clinicians may be able to diagnose youth with chronic mood lability more accurately and reliably. With more accurate diagnoses, we gain an opportunity to fill the gap in our understanding of the phenomenology and trajectory of cyclothymic disorder in youth.
We hypothesized the RDCyc group and youth with other DSM-IV bipolar diagnoses would endorse similar mood symptom severity, impairment, and family characteristics, consistent with their inclusion on the bipolar spectrum, and that there would be more severe mood symptoms and impairment in the RDC group than in youth with non-mood, disruptive behavior disorders. In addition to experiencing symptoms consistent with a bipolar presentation, we expected youth with an RDC diagnosis of cyclothymic disorder to have a positive family history of mental illness (Van Meter et al., 2012a; Van Meter et al., 2011b). Related, we expected caregivers for youth with cyclothymic disorder to report high stress and burden related to caregiving, particularly in light of the fact that they might be coping with their own symptoms (Perez Algorta et al., 2015).
Data from the Longitudinal Assessment of Manic Symptoms study (LAMS; (Findling, 2010; Findling et al., 2013) were well-suited for this study: The majority of participants were recruited based on elevated scores on a parent-rated measure of manic symptoms, resulting in a sample of youth at elevated risk for having or developing a bipolar spectrum disorder, including cyclothymic disorder. Youth in the study were assessed at six-month intervals for at least two years, allowing for the one year duration criteria of cyclothymic disorder to be evaluated without relying solely on retrospective report.
Method
Participants
Participants, aged 6–12 years, from nine clinics located among four universities enrolled in a longitudinal study of youth with elevated symptoms of mania (Horwitz, 2010). The majority of youth (N=621) had scores above 12 on the Parent General Behavior Inventory 10 Item Mania scale (PGBI-10M; Youngstrom et al., 2008)); a demographically matched sample of 86 youth with PGBI-10M scores below 11 were also enrolled. Participants completed evaluations every six months to assess for changes in mood or other symptoms. The present study includes data collected through the two-year follow-up, at which time retention was strong (94%).
Measures
KSADS-PL-W (Findling et al., 2010; Geller et al., 1996; Kaufman et al., 1997) was administered by a trained interviewer to youth and their parent/caregiver separately. Reliability for the KSADS items used to evaluate symptom and impairment criteria for the RDCyc diagnosis (detailed below) had Cronbach’s alphas ranging from 0.93 (baseline, six-month, and 18-month time points) to 0.94 (12-month and 24-month time points). Inter-rater reliability for K-SADS diagnoses was good, K =0.82 (Findling et al., 2010) in the present study. In addition to informing diagnoses, the KSADS assessed for suicidal ideation and behavior.
Treatment with medication was assessed using the parent report version of the Service Assessment for Children and Adolescents (SACA; Horwitz et al., 2001; Kowatch et al., 2013; Stiffman et al., 2000), which inquires about the child’s history of mental health services use. For this study, we examined medications the child was taking between the 18- and 24-month follow-ups. Additionally, youth engagement with psychosocial services (therapy, counseling) was measured at baseline.
The Family History Screen (FHS; Milne et al., 2009) assessed the presence of mental illness among members of a family. Diagnoses were based on the presence of specific symptoms; for example, bipolar disorder was assessed by asking whether the parent has experienced “extreme, elated mood,” plus at least three other symptoms of mania. For purposes of this study, we evaluated presence/absence of bipolar disorder and of any psychiatric illness in the youth’s biological mother or father.
The Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski et al., 1984) is a 17-item clinician-rated instrument for measuring severity of depression in children. We compared youths’ 24-month follow-up scores; Cronbach’s alpha in the present sample was .85.
The Young Mania Rating Scale (YMRS; Young et al., 1978) is an 11-item, clinician-rated measure of the severity of a child’s manic symptoms. In the present study we assessed youths’ 24-month follow-up scores, Cronbach’s alpha was .78.
Child’s Global Assessment Scale (C-GAS; Shaffer et al., 1983) is a clinician-rated measure of youth overall functioning. In this study, we used current C-GAS scores from the 24-month follow-up.
Parent General Behavior Inventory (P-GBI; Youngstrom et al., 2001). The P-GBI was modified from the original General Behavior Inventory to be answered by caregivers about their child. The questionnaire includes the seven-item P-GBI sleep disturbance scale (Meyers and Youngstrom, 2008) assessed at 24-months, where Cronbach’s alpha was .85.
The Revised Questionnaire for Measuring Health-Related Quality of Life in Children and Adolescents (KINDL-R; Bullinger et al., 2008; Ravens-Sieberer and Bullinger, 2000; Wee et al., 2005). The KINDL-R measured youth quality of life across six dimensions (physical, emotional, self-esteem, family, friends, and school). The KINDL scales are short – four items each – which tends to result in lower reliability; in this sample, the median Cronbach’s alpha for the youth scales was 0.40 and for the parent scales was 0.72 at 24 months.
The Parent Stress Survey (Sisson and Fristad, 2001) is a 25-item questionnaire that asks whether caregivers have experienced certain stressful events related to parenting and, if so, to rate how stressful it was. Cronbach’s alpha was 0.91.
Procedure
All youth and their caregiver were interviewed about both present and lifetime symptoms using the KSADS. Additionally, caregivers and youth over the age of 11 filled out a series of questionnaires about their mental health, functioning, and related topics. All diagnoses were reviewed by a licensed clinical psychologist or child psychiatrist and followed DSM-IV-TR criteria. Diagnoses were made without knowledge of responses on self-report measures.
Research Diagnostic Criteria Operational Definition of Cyclothymic Disorder
The RDC definition (RDCyc) required having at least one “A criterion” symptom of mania (elated mood, irritability, increased energy), (2) depressed mood, (3) at least one additional symptom of mania and one additional symptom of depression, (4) duration of 12 months (two consecutive six month follow-ups) and (5) impairment. If, at baseline or during any of the follow-up periods, a youth met criteria for a hypomanic, manic or major depressive episode, s/he was excluded from the cyclothymic group. Additionally, if a child was hospitalized for mania or depression s/he was excluded, as this would be consistent with a diagnosis of mania or a major depressive episode (American Psychiatric Association, 2013). These criteria differ from the DSM-5 criteria for cyclothymic disorder in that they require an A criterion for both depression and mania, and they require at least two co-occurring symptoms of both mania and depression; we believe this more specific definition will be easier to apply than the more vague criteria from the DSM, “numerous periods of hypomanic symptoms that do not meet criteria for a hypomanic episode and numerous periods with depressive symptoms that do not meet criteria for a major depressive episode” (American Psychiatric Association, 2013, p. 139).
Youth who met RDCyc criteria were then compared to youth with other diagnoses in the sample. Youth were sorted into the following four categories based on consensus diagnoses (a) bipolar I or bipolar II, (b) BP-NOS1 or cyclothymic disorder (note that youth with a consensus diagnosis of cyclothymic disorder were not subsumed into the RDCyc category unless they met the research diagnostic criteria2), (c) depression, (d) disruptive behavior disorders (ODD, CD) or ADHD. ANOVAs compared RDCyc to the other diagnostic groups on number of comorbid diagnoses, depressive and manic symptom severity, C-GAS score, sleep disturbance, and KINDL-R quality of life scales using Tukey’s HSD test. Additionally, chi-squared analyses examined differences in medications prescribed, family history of psychiatric illness disorder, and suicidal thoughts and behaviors. All comparisons used data from the 24-month follow-up. Due to the large number of comparisons made, we set a more conservative threshold of p=.01 to indicate statistical significance.
Results
Demographic Statistics
The average age at the 24-month follow-up of the youth included in the analyses was 10.9 years (SD=1.9). There were no differences in average age across the diagnostic groups. The sample was 64% male, 64% White, 26% Black, 10% Biracial, and <1% other. There were no significant differences in demographics across the groups; see Table 1.
Table 1.
Demographic information and average clinical scale scores measured at two-year follow-up (scored using percentage of maximum possible)
| Disruptive behavior /Attention deficit hyperactivity disorder | Depression | RDC Cyclothymic | Bipolar I or II | Bipolar NOS/ cyclothymic disorder | |
|---|---|---|---|---|---|
| Demographic | n=172 | n=38 | n=29 | n=86 | n=38 |
| Female | 23% | 46% | 44% | 44% | 41% |
| White | 53% | 46% | 59% | 76% | 74% |
| Age (SD) | 10.93 (2.0) | 10.80 (1.8) | 10.45 (1.9) | 11.29 (2.0) | 11.08 (2.1) |
| Number of comorbid diagnoses | 1.84 (9.5)*** | 3.22 (1.2) | 2.83 (1.3) | 2.70 (1.3) | 3.42 (1.3) |
| Treatment | |||||
| Antidepressant | 15% | 22% | 28% | 22% | 18% |
| Antipsychotic | 16% | 14% | 38% | 59% | 55% |
| Mood stabilizer | 6% | 11% | 4% | 30%* | 9% |
| Stimulant | 56% | 27% | 52% | 50% | 45% |
| Psychosocial treatment | 50% | 59% | 59% | 43% | 58% |
| Family History | |||||
| Bipolar Disorder | 14% | 11% | 17% | 37% | 32% |
| Any Psychiatric Illness | 87% | 97% | 97% | 91% | 92% |
| Mean Mood Symptoms and Functioning | |||||
| CDRS-R Depression (SD) | 12.08 (8.6)*** | 34.89 (13.9) * | 25.00 (16.8) | 20.42( 18.4) | 24.38 (15.7) |
| YMRS Mania (SD) | 23.14 (15.7)*** | 24.75 (17.0) † | 35.97 (19.0) | 36.50 (22.9) | 43.18 (16.8) |
| C-GAS Global Functioning (SD) | 62.65 (9.0) † | 53.61 (8.9) | 57.38 (9.8) | 58.37 (11.1) | 53.44 (9.8) |
| P-GBI Sleep Disturbance (SD) | 21.82 (19.8) | 25.03 (22.1) | 28.41 (23.6) | 25.91 (20.4) | 34.36 (24.6) |
| Parent Stress Survey (SD) | 21.32 (17.3) † | 25.53 (20.1) | 31.15 (23.6) | 32.65 (22.2) | 30.09 (22.4) |
| Suicidal thoughts/behaviors | |||||
| Suicidal Ideation | 4% | 22% | 11% | 17% | 21% |
| Suicidal Behavior | 1% | 3% | 4% | 8% | 3% |
| Suicide Attempt | 0%† | 0% | 4% | 1% | 0% |
| Mean KINDL-R Quality of Life Scores (higher scores indicate better quality of life) | |||||
| Self-report | |||||
| Physical Well-Being (SD) | 73.19 (17.2) | 69.29 (16.6) | 68.53 (16.9) | 67.57 (17.0) | 70.39 (15.7) |
| Self-Esteem (SD) | 52.66 (26.3) | 37.32 (24.8) | 42.89 (27.5) | 50.96 (28.7) | 47.70 (27.1) |
| Family Functioning (SD) | 69.01 (17.4) | 60.48 (15.3) | 64.65 (18.5) | 64.34 (19.0) | 63.49 (16.0) |
| Friendship Quality (SD) | 70.41 (21.7) | 63.24 (20.8) | 66.16 (17.5) | 62.72 (20.2) | 66.39 (23.2) |
| School Functioning (SD) | 54.45 (18.1) | 48.90 (16.6) | 59.82 (17.5) | 58.64 (17.3) | 59.03 (13.2) |
| Parent report | |||||
| Emotional Well-Being (SD) | 74.87 (16.7)** | 70.18 (19.3) | 63.79 (17.9) | 72.50 (17.6) † | 75.49 (15.3) † |
| Physical Well-Being (SD) | 76.02 (15.1) | 62.50 (16.4) | 67.02 (17.7) | 66.86 (19.0) | 69.74 (20.4) |
| Self-Esteem (SD) | 50.48 (23.6) | 36.21 (15.4) | 44.40 (16.4) | 46.37 (18.8) | 53.78 (19.6) |
| Family Functioning (SD) | 60.60 (19.8) | 54.78 (24.9) | 53.66 (19.7) | 53.02 (20.1) | 51.81 (17.7) |
| Friendship Quality (SD) | 69.81 (18.0) | 53.49 (18.1) | 63.79 (19.9) | 59.45 (19.7) | 61.49 (15.3) |
| School Functioning (SD) | 60.19 (16.7) | 54.55 (16.2) | 62.07 (14.6) | 56.77 (17.3) | 61.79 (13.8) |
| Emotional Well-Being (SD) | 82.53 (12.8)** | 63.60 (19.1) | 69.61 (19.5) | 69.77 (16.4) | 74.01 (15.4) |
significantly different from RDCyc;
p<.05 above threshold of p<.01 set for this study,
p<.01,
p<.005,
p<.0005
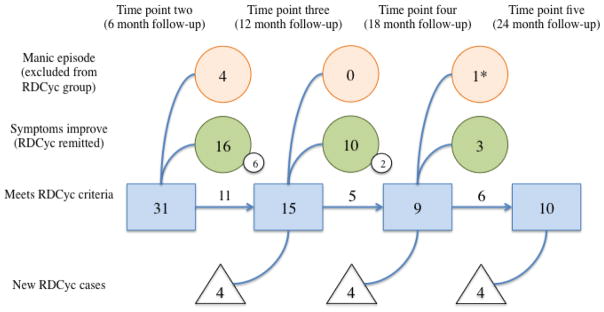
Diagnostic Subtyping
Of the youth assessed, 37 met criteria for RDCyc at some point over the two-year follow-up. Of the 37, eight did not have data from the 24-month time point either because they missed the appointment (n=6) or because they dropped out of the study (n=2). Consequently, analyses include 29 participants with the RDCyc diagnosis. This group includes youth whose symptoms improved over follow-up (i.e., such that they no longer met criteria, n=19), but it does not include youth who got worse (i.e., if they met criteria, but later had a manic or depressive episode, they were not counted in the RDCyc group; n=5). See Figure 1. This decision was made in order to represent cyclothymic disorder as accurately as possible and without individuals who would have a major depressive or manic episode in the near future. As a sensitivity analysis, we compared youth who met the RDCyc criteria, but later became manic (none of the RDCyc youth experienced an episode of depression during the follow-up period), with those who stayed in the RDCyc group, on the 24-month outcome measures. The youth who had a manic episode reported higher CDRS-R scores (p=.001), lower emotional well-being (p=.036), and greater suicidal ideation (p=.043) and suicidal behaviors (p=.003). There were no differences in the medications prescribed between the two groups at 24 months, but those who stayed in the RDCyc group were more likely to be engaged in psychosocial services (at baseline) than those youth who developed mania (p=.015).
Figure 1.
Trajectory of RDC cyclothymic disorder diagnosis across time points; number of youth meeting criteria at each follow-up is shown in boxes, circles show how many youth either got better (bottom circles) or became manic (top circles) between time points and, consequently, did not meet RDCyc criteria at the next follow-up. Triangles show number of new cases introduced at each follow-up. * One individual got better between the 12 and 18 month follow-up appointments and then became manic between the 18 and 24 month follow-ups.
Note: Small circles denote participants for whom there were no data at the 24-month follow-up. Only one individual met RDCyc criteria at all time points.
KSADS Diagnoses
At the 24-month follow-up, youth who met RDCyc criteria were listed with the following KSADS consensus primary diagnoses: BP-NOS (n=12), ADHD (n=4), Asperger’s Disorder (n=2), major depression (n=2), depression NOS (n=2), cyclothymic disorder (n=1), or mood disorder NOS, generalized anxiety disorder, oppositional defiant disorder (each n=1). Three youth had no diagnosis (V71.09).
Other consensus diagnoses included in the analyses were bipolar I (n=86) or II (n=5), cyclothymic disorder (n=6) or BP-NOS (n=33), depression (MDD; n=38), ADHD (n=156) and disruptive behavior disorders (DBD; n=16). To reduce the number of comparisons made, we formed four comparison diagnostic groups: 1) bipolar I or II; 2) BP-NOS or cyclothymic disorder; 3) ADHD and/or DBD; and 4) depression. For the following comparisons, groups 3–4 are described as “non-bipolar.”
Comorbid Diagnoses
The average number of comorbid diagnoses (see Table 1) differed significantly between RDCyc and the non-bipolar groups (F(2,235)=33.71, p<.0005). Youth with RDCyc or depression had more comorbid diagnoses than youth with ADHD and/or DBD (p<.0005). Among the bipolar subtypes (F(2,150)=4.24, p=.016), there was a trend toward youth with BP-NOS/cyclothymic disorder having more comorbid diagnoses than youth with BD I/II (p=.012).
Medication Use
Chi-squared analyses were used to determine whether there were differences in the medications prescribed to youth in the sample (see Table 1).
Antidepressants
Rates of antidepressant prescriptions did not vary between RDCyc and non-bipolar diagnostic categories (X2(2)=3.56, p=.169), or the bipolar subtypes (X2(2)=0.80, p=.670).
Antipsychotics
The prevalence of antipsychotic use among the RDCyc group (X2(2)=8.90, p=.012) was higher (38%) than among youth with depression (14%) or ADHD (16%). Antipsychotic prescriptions did not vary among bipolar subtypes (X2(2)=4.01, p=.135).
Mood stabilizers
Rates of mood stabilizer prescriptions (including lithium) did not differ significantly between RDCyc and the non-bipolar diagnoses (X2(2)=1.51, p=.470). Prescriptions for mood stabilizers varied among youth with bipolar spectrum disorders (X2(2)=14.27, p=.001). Thirty percent of youth with bipolar I or II, 8% of youth with cyclothymic disorder/BP-NOS, and 3% of RDCyc youth were prescribed a mood stabilizer, including lithium.
Stimulants
Rates of stimulant medication prescriptions varied between RDCyc and non-bipolar diagnoses (X2(2)=10.11, p=.006 ); 52% of the RDCyc youth were prescribed a stimulant, 56% of youth with ADHD/DBD, 37% of youth with depression. There were no differences in the prevalence of stimulant medication prescriptions among youth with bipolar spectrum disorders (X2(2)=0.40, p=.820).
Family History
Bipolar disorder
History of parental bipolar disorder was compared between RDCyc and the non-bipolar diagnostic groups (X2(2)=0.57, p=.753) and across the bipolar subtypes (X2(2)=1.94, p=.380); there were no significant differences (see Table 1).
Psychiatric illness
Overall parental history of mental illness (see Table 1) did not differ significantly between RDCyc and non-bipolar disorders (X2(2)=5.02, p=.081) or youth with bipolar spectrum disorders (X2(2)=1.03, p=.598).
Severity of Mood Symptoms
Depression symptom severity
CDRS-R scores at 24 months (see Table 1) varied significantly between RDCyc and non-bipolar disorders (F(2,234)=75.41, p<.0005). RDCyc youth scored higher than youth with ADHD/DBD (p<.0005), and lower than youth with depression (p=.001) based on Tukey’s HSD post-hoc test. RDCyc youth CDRS-R scores were consistent with other youth with bipolar spectrum disorders (F(2,150)=1.11, p=.332).
Manic symptom severity
YMRS scores at 24 months (see Table 1) differed between RDCyc and the non-bipolar groups (F(2,234)=7.65, p=.001); RDCyc youth scored higher than youth with ADHD/DBD (p=.001) and youth with MDD (p=.018). Within the bipolar spectrum there were no differences in YMRS scores (F(2,150)=1.54, p=.218).
Global Functioning
Comparing RDCyc and the non-bipolar youth (F(2, 234)=16.82, p<.0005), youth in both the RDCyc (p=.012) and depression groups (p<.0005) had lower C-GAS scores than youth with ADHD/DBD (see Table 1). There were no differences in C-GAS scores between the bipolar groups (F(2, 150)=2.92, p=.057).
Sleep Disturbance
P-GBI sleep disturbance scores did not differ significantly between RDCyc and the non-bipolar groups (F(2,233)=1.44, p=.238) or the bipolar subtypes (F(2,149)=1.89, p=.154) (see Table 1).
Suicide and Self-Harm
Ideation
The rates of suicidal ideation at 24 months were different between RDCyc and non-bipolar groups (X2(2)=13.81, p=.001) with 22% of youth with depression, 12% of RDCyc youth, and 4% of youth with ADHD and/or DBD reporting ideation (see Table 1). Among the bipolar subtypes, the presence of suicidal ideation did not differ significantly (X2(2)=1.23, p=.540).
Suicidal behavior
The number of youth reporting suicidal gestures at 24 months was low (see Table 1) and did not differ between RDCyc and the non-bipolar groups (X2(2)=1.14, p=.573; 4 out of 235 youth) or among the bipolar subtypes (X2(2)=1.78, p=.412; 9 out of 152 youth).
Suicide attempt
The difference in suicide attempts at 24 months was not significant between the RDCyc group and the non-bipolar diagnoses (X2(2)=7.50, p=.024); one youth with RDCyc and none with ADHD/DBD or depression attempted suicide (see Table 1). History of suicide attempt did not differ across the bipolar subtypes (X2(2)=1.62, p=.445). One youth with bipolar I and one youth from the RDCyc group reported a past suicide attempt.
Quality of life
There were no significant differences between bipolar subtypes on the parent- rated KINDL-R scales (ps=.069–.921) at 24 months (see Table 1).
Physical well-being
There were no differences between RDCyc and non-bipolar disorders (p=.247) or between the bipolar subtypes (p=.696) on child-reported physical well-being. Parent report varied between RDCyc and the non-bipolar diagnoses (F(2, 231)=13.04, p<.0005); ADHD/DBD reported better physical well-being than RDCyc (p=.012) and depression (p<.0005).
Self-esteem
Child-reported self-esteem varied between RDCyc and non-bipolar diagnostic groups (F(2,230)=5.89, p=.003), youth with depression scored lower than youth with ADHD/DBD (p =.005). Parent-rated self-esteem between RDCyc and the non-bipolar diagnoses did vary (F(2,231)=6.44, p=.002); ADHD scored higher than depression (p=.002). Child-reported self-esteem did not vary between bipolar subtypes (F(2,149)=0.92, p=.402).
Family
There were no significant differences between RDCyc and non-bipolar diagnostic groups on child-rated family functioning (F(2,228)=3.82, p=.023) nor were scores different between the bipolar subtypes (F(2,149)=0.04, p=.960). Parent-rated family functioning did not vary between RDCyc and non-bipolar diagnoses (p=.113).
Friends
There were no significant differences between non-bipolar disorders (F(2,228)=1.89, p=.153) or bipolar subtypes (F(2,148)=0.57, p=.570) on child-rated friendship quality. Based on parent report (F(2,231)=11.72, p<.0005), youth with ADHD scored higher than youth with depression (p<.0005).
School functioning
There were no differences on child-rated school functioning between RDCyc and the non-bipolar diagnoses (F(2,219)=3.02, p=.051) or between the bipolar subtypes (F(2,142)=0.057, p=.944). Parent-rated school functioning (F(2,224)=2.02, p=.136) did not vary among non-bipolar diagnoses.
Emotional well-being
Child self-reported emotional well-being varied between RDCyc and non-bipolar diagnoses (F(2,230)=5.56, p=.004); RDCyc youth scored lower than youth with ADHD (p=.005). Child self-reported emotional well-being was not different across the bipolar subtypes (F(2,149)=4.01, p=.018). On parent-rated emotional well-being (F(2, 231)=28.89, p<.0005), youth with ADHD scored higher than youth with RDCyc (p<.0005) and youth with depression (p<.0005).
Parent Stress
There were no differences in parental stress across the non-bipolar disorders (F(2,235)=3.81, p=.024) or across the bipolar subtypes (F(2,150)=0.18, p=.834) at 24 months (see Table 1).
Discussion
We sought to determine whether operationalized criteria for DSM-5 cyclothymic disorder could be applied to a youth sample to identify youth with chronic, impairing symptoms of mania and depression. Consistent with previous studies of cyclothymic disorder in youth (Lewinsohn et al., 1995; Van Meter et al., 2012a; Van Meter et al., 2011b), we found few differences between youth in the RDCyc group and youth diagnosed with bipolar I, II, NOS or non-RDC cyclothymic disorder. Apparently, the lower intensity of mood symptoms is counterbalanced by greater chronicity, resulting in a similar degree of burden. In this sample, 5% of youth met RDCyc criteria; this is slightly less than in other studies that include cyclothymic disorder as a diagnostic category (e.g., 6% [Van Meter et al., 2011b], 6% [Van Meter et al., 2012a]), but these other samples were all treatment-seeking youth, which may result in higher prevalence of psychopathology.
The DSM-IV diagnoses that RDCyc youth were assigned varied. Although about a third had bipolar spectrum diagnoses, the majority did not. Because early treatment is associated with better outcomes for youth with bipolar spectrum disorders (Elanjithara et al., 2011), and because some data suggest that medications commonly used for other disorders (e.g., anti-depressants and stimulants) are less effective and can be harmful (Goldsmith et al., 2011; Pacchiarotti et al., 2013), accurate diagnosis and intervention is essential. Of course, the diagnostic picture can change over time – particularly for young people – but the presence of manic symptoms is associated with later bipolar disorder in many youth (Van Meter et al., 2016), and should be weighed accordingly when considering next clinical steps.
Interestingly, only one youth had a prior diagnosis of cyclothymic disorder and met criteria for RDCyc. Though it is not possible to know why this particular person received the diagnosis and others did not (the individual met at just one follow-up, so it is not a situation of a stronger phenotype than other cases), this finding suggests that, in addition to being used infrequently, clinical diagnoses of cyclothymic disorder may have poor reliability. This is not surprising; if a diagnosis is used rarely, there are fewer opportunities to learn about it through one’s clinical experience or to get feedback on the accuracy of one’s initial clinical judgment.
The fact that the majority of the RDCyc youth had non-bipolar diagnoses is a reminder that our knowledge about other diagnoses may be contaminated by youth with subthreshold but chronic and impairing mood symptoms. Chronic mood problems in youth with other childhood disorders is attracting increased attention (Blader et al., 2016; Burke, 2012; Mayes et al., 2016), but before broadening the conceptualization of these non-mood disorders, or creating new labels to suit the changing conceptualizations, it might be worthwhile to check whether there are youth in clinical service (or research studies) who, in fact, have cyclothymic disorder. If so, this would help to explain the large discrepancies in the rates of diagnoses of cyclothymic disorder between the epidemiological data, adult literature, and clinical diagnoses in youth.
Consistent with our hypothesis, a high rate (97%) of the youth in the RDCyc group had a family history of mental illness. Past research has found that people with cyclothymic disorder often have family members with psychiatric illnesses, including, but not limited to, bipolar disorder (Akiskal et al., 1977; Depue, 1981; Van Meter et al., 2012b). This has been hypothesized as a reason why people with cyclothymic disorder experience more chronic symptoms and are less likely to achieve remission with standard treatment; a more varied genetic profile (relative to someone with bipolar I or II) could result in a presentation that is a combination of multiple disorders and that is less episodic than bipolar I or II (Van Meter et al., 2012a; Van Meter et al., 2011b). This has important implications for both the treatment approach and expected course of illness.
Five individuals who were identified as meeting the RDCyc criteria developed a manic episode during the two-year follow-up (none of the RDCyc youth experienced a depressive episode). This is a lower rate of conversion to BD I or II for youth with subthreshold subtypes than another prospective study found (Birmaher et al., 2009), but the other study did not differentiate cyclothymic disorder and BP-NOS, which could account for the discrepancy. Similarly, in the LAMS sample, of those with a baseline KSADS diagnosis of BP-NOS or cyclothymic disorder, 28 people (out of 74) developed mania and eight developed depression. Though we cannot directly compare this conversion rate to the one seen in the RDCyc youth (RDCyc diagnoses take conversion into account and were made at the 24-month follow-up, whereas this result is prospective conversion in people who had a baseline KSADS diagnosis of BP-NOS or cyclothymic disorder), this is undoubtedly a larger proportion of cases with a trajectory toward mania. BP-NOS is commonly diagnosed in youth and, in some situations, serves as the “catch-all” diagnosis for those who do not meet criteria for bipolar I or II (Van Meter & Youngstrom, 2012). These youth are impaired and often have severe, though short-lasting, symptoms (Van Meter, Burke, Kowatch, Findling, & Youngstrom, 2016). This phenotype – relative to cyclothymic disorder, which requires long lasting, less severe symptoms – may be more likely to convert to bipolar I or II. Importantly, our results suggest that the severity of the mood episode is not the only driver of impairment; youth in the RDCyc group who never had a manic episode were equally impaired as those who did develop mania.
Interestingly, whereas relatively few in the RDCyc group got worse, more than two-thirds got better; cyclothymic disorder was not included as a diagnosis in the two longitudinal studies that show evidence for remitting symptoms over time (Birmaher et al., 2009; Cicero et al., 2009), but it is possible that the more developmentally-limited subtype is more consistent with RDCyc in childhood. Although one could suggest that these youth never had a bipolar spectrum disorder, we used conservative duration criteria, requiring both manic and depressive symptoms, in addition to impairment, for at least a year. Furthermore, the youth in the RDCyc group reported symptoms and functional impairment consistent with the other bipolar spectrum disorders. This is true even though two-thirds of the sample was in remission at the time of comparison, consistent with research suggesting poor functioning among people with bipolar spectrum disorders even in times of relative euthymic mood (Birmaher et al., 2014; Fagiolini et al., 2005), which may be related to the high prevalence of comorbid disorders. Though this lack of difference could be interpreted as justification for using the same treatment approach across the bipolar spectrum, given the side effect profile of many of the medications used in this population, a different treatment approach may be warranted for youth who experience significant mood-related impairment even in the absence of severe mood episodes. Future studies to evaluate the efficacy of mood stabilizing and anti-psychotic medications across the subtypes of bipolar disorder are necessary to answer this question.
Although we cannot say whether youth in the BP-NOS/cyclothymic disorder group had a different trajectory than the RDCyc group because we used the two-year follow-up diagnoses as the way by which the comparison groups were defined, this is an intriguing finding and highlights a potential discrepancy between the adult and child literature that has important implications for our expectations related to pediatric bipolar disorder. Longer follow-up with clearly delineated subtypes will be important to better answer some of the questions about the stability of the symptoms/diagnoses over time (Axelson et al., 2012; Axelson et al., 2011). Additionally, because we found that RDCyc youth who were engaged in psychosocial treatment were less likely to become manic, which is consistent with research suggesting that psychotherapy is important to the maintenance of mood in bipolar disorder (Fristad and MacPherson, 2014; Miklowitz, 2006), future studies should carefully assess the impact of different treatments on trajectory.
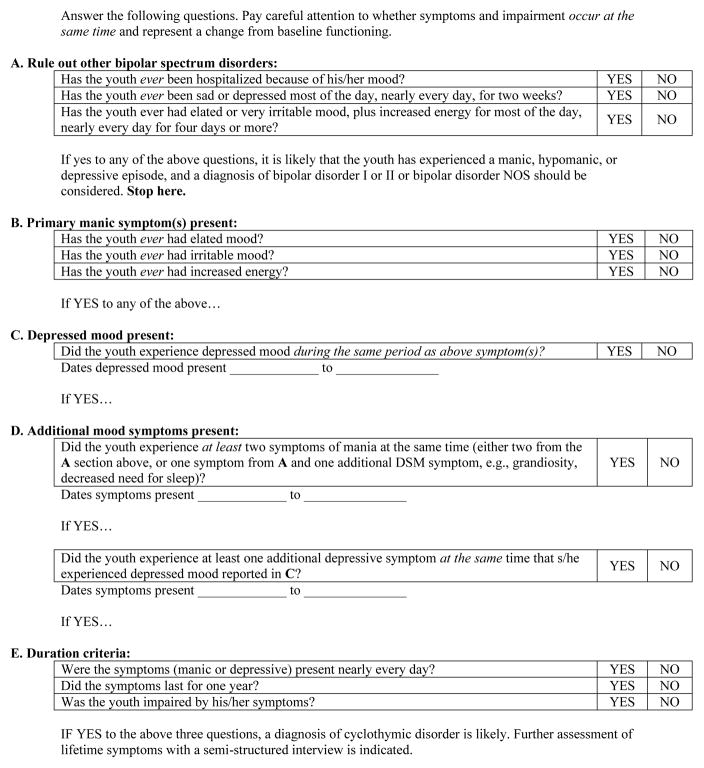
In addition to learning more about potential differences between youth who meet criteria for cyclothymic disorder and those who have BP-NOS, we were also interested in determining whether the DSM-5 criteria for cyclothymic disorder could be operationalized and applied in a way that would make it easier for clinicians and researchers to include this as a diagnostic category. The RDC definition was clear, in that the number and type of symptoms required were explicitly defined, and we believe this could help with accurate, reliable diagnosis. However, the duration and exclusionary criteria still represent a burden to families and clinicians. Specifically, being able to ascertain that the child has never met criteria for depression or [hypo]mania could be difficult, particularly since most people making diagnoses are used to thinking about inclusion rather than exclusion criteria. For youth with chronic mood problems, a checklist or other way of systematically checking their symptoms against a diagnostic algorithm would be helpful (see Figure 2). Importantly, our data do suggest that differentiating youth with cyclothymic disorder is important and worth the extra effort, so that we can learn more about the trajectory of these youth over time.
Figure 2.
Checklist to screen for cyclothymic disorder in youth
Limitations
Though this study is a step toward better understanding cyclothymic disorder in youth, there are important limitations. First, most of the youth in the sample were recruited due to elevated symptoms of mania (Findling, 2010), and this may have resulted in the non-bipolar comparison group being more similar to the RDCyc group than would be the case in another sample. Related, the elevated mood symptoms prohibited the evaluation of short duration cyclothymia (American Psychiatric Association, 2013), another diagnostic group of interest. In addition to symptom overlap, the recruitment strategy is also likely related to the high rates of family history of both bipolar disorder and other psychiatric illnesses seen in the non-bipolar comparison group. Because the youth in the sample are not yet through the period of highest risk for onset of bipolar disorder, it is also possible that some of the youth in the non-bipolar comparison group will develop bipolar disorder later. These factors help to explain the fact that relatively few differences were found between the RDCyc and non-bipolar groups, in particular. Relatedly, we looked only at differences at the two-year follow-up. As the youth in the sample age into the period of highest risk, both the diagnostic composition of the sample and the type and degree of difference between the groups may change. Finally, although the total sample size was quite large, we found only 29 youth who met the RDCyc criteria and had follow-up data, consequently, some analyses may be underpowered to detect differences, especially with alpha set at p<0.01 to prevent false positives from multiple tests. These limitations underscore the importance of future longitudinal studies with carefully defined diagnostic categories.
Conclusion
Our study suggests that clearly operationalized criteria for cyclothymic disorder can be applied to identify a distinct category of youth with symptoms and impairment similar to other youth with bipolar spectrum disorders and different from non-bipolar diagnoses. Importantly, our results also indicate that the cyclothymic phenotype may be associated with developmentally-limited presentations of bipolar disorder, as many of the youth experienced symptom remission over the two-year follow-up. It is also possible that the criteria used for cyclothymic disorder in youth – requiring only one year of symptoms – are capturing a different population than the adult criteria, which require two years of symptoms. This suggests a possible mismatch between the youth and adult literatures – among adults, cyclothymic disorder is associated with high comorbidity and progression to bipolar I or II, but in our sample the RDCyc youth had fewer comorbid disorders than the NOS/cyclothymic disorder group and only five got worse. Following youth with well-defined cyclothymic disorder alongside youth with BP-NOS will be important to linking the child and adult literature and to providing evidence about the expected course of this under-studied disorder.
Highlights.
Research diagnostic criteria for cyclothymic disorder, derived from DSM-5 criteria, identify a subgroup of youth with characteristics similar to other youth on the bipolar spectrum and distinct from youth with non-bipolar diagnoses.
Youth who met criteria for the research diagnosis of cyclothymic disorder were more likely to have their symptoms remit over time than to progress to bipolar I or II
Including the diagnosis of cyclothymic disorder in research studies is important to the goal of better understanding factors that influence the longitudinal trajectory of mood symptoms in youth
Footnotes
The bipolar NOS diagnosis required: 1) elated mood plus two associated symptoms or irritable mood plus three associated symptoms; 2) change in level of functioning; 3) symptoms for a total of at least 4 hours within a 24-hour period; and 4) had at least 4 episodes of at least 4 hours’ duration or a total of at least 4 days of sufficient intensity over the lifetime (Birmaher, B., Axelson, D., Strober, M., Gill, M.K., Valeri, S., Chiappetta, L., Ryan, N., Leonard, H., Hunt, J., Iyengar, S., Keller, M., 2006. Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry 63, 175–183.et al., 2006).
One individual met both the RDCyc criteria and had a KSADS consensus primary diagnosis of cyclothymic disorder.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akiskal H, Djenderedjian A, Rosenthal R, Khani M. Cyclothymic disorder: Validating criteria for inclusion in the bipolar affective group. American Journal of Psychiatry. 1977;134:1227–1233. doi: 10.1176/ajp.134.11.1227. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Association; Washington, D.C: 2013. [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63:1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Axelson D, Findling RL, Fristad M, Kowatch RA, Youngstrom EA, McCue Horwitz S, Arnold E, Frazier T, Ryan N, Demeter C, Gill MK, Hauser-Harrington J, Depew J, Kennedy SM, Gron B, Brieana R, Birmaher B. Examining the Proposed Disruptive Mood Dysregulation Disorder Diagnosis in Children in the Longitudinal Assessment of Manic Symptoms Study. Journal of Clinical Psychology. 2012;73:1342–1350. doi: 10.4088/JCP.12m07674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Strober MA, Goldstein BI, Ha W, Gill MK, Goldstein TR, Yen S, Hower H, Hunt JI, Liao F, Iyengar S, Dickstein D, Kim E, Ryan ND, Frankel E, Keller MB. Course of Subthreshold Bipolar Disorder in Youth: Diagnostic Progression From Bipolar Disorder Not Otherwise Specified. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:1001–1016. e1003. doi: 10.1016/j.jaac.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito-Smythers C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: The course and outcome of bipolar youth (COBY) study. American Journal of Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Gill MK, Axelson DA, Goldstein BI, Goldstein TR, Yu H, Liao F, Iyengar S, Diler RS, Strober M, Hower H, Yen S, Hunt J, Merranko JA, Ryan ND, Keller MB. Longitudinal Trajectories and Associated Baseline Predictors in Youths With Bipolar Spectrum Disorders. American Journal of Psychiatry. 2014;171:990–999. doi: 10.1176/appi.ajp.2014.13121577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blader JC, Pliszka SR, Kafantaris V, Sauder C, Posner J, Foley CA, Carlson GA, Crowell JA, Margulies DM. Prevalence and Treatment Outcomes of Persistent Negative Mood Among Children with Attention-Deficit/Hyperactivity Disorder and Aggressive Behavior. Journal of Child and Adolescent Psychopharmacology. 2016;26:164–173. doi: 10.1089/cap.2015.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullinger M, Brütt AL, Erhart M, Ravens-Sieberer U. Psychometric properties of the KINDL-R questionnaire: Results of the BELLA study. European Child and Adolescent Psychiatry. 2008;17:125–132. doi: 10.1007/s00787-008-1014-z. [DOI] [PubMed] [Google Scholar]
- Burke JD. An affective dimension within oppositional defiant disorder symptoms among boys: personality and psychopathology outcomes into early adulthood. J Child Psychol Psychiatry. 2012;53:1176–1183. doi: 10.1111/j.1469-7610.2012.02598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero D, Epler A, Sher K. Are there developmentally limited forms of bipolar disorder? Journal of Abnormal Psychology. 2009;118:431–447. doi: 10.1037/a0015919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue R. A behavioral paradigm for identifying persons at risk for bipolar depressive disorder: A conceptual framework and five validation studies. Journal of Abnormal Psychology. 1981:90. doi: 10.1037//0021-843x.90.5.381. [DOI] [PubMed] [Google Scholar]
- Elanjithara TE, Frangou S, McGuire P. Treatment of the early stages of bipolar disorder. Advances in Psychiatric Treatment. 2011;17:283–291. [Google Scholar]
- Fagiolini A, Kupfer D, Masalehdan A, Scott J, Houck P, Frank E. Functional impairment in the remission phase of bipolar disorder. Bipolar Disorders. 2005;7:281–285. doi: 10.1111/j.1399-5618.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- Findling RL, Jo B, Frazier TW, Youngstrom EA, Demeter CA, Fristad MA, Birmaher B, Kowatch RA, Arnold E, Axelson DA, Ryan N, Hauser JC, Brace DJ, Marsh LE, Gill MK, Depew J, Rowles BM, Horwitz SM. The 24-month course of manic symptoms in children. Bipolar Disorders. 2013;15:669–679. doi: 10.1111/bdi.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findling RL, Youngstrom EA, Fristad MA, Birmaher B, Kowatch RA, Arnold LE, Frazier TW, Axelson D, Ryan N, Demeter CA. Characteristics of children with elevated symptoms of mania: the Longitudinal Assessment of Manic Symptoms (LAMS) study. The Journal of Clinical Psychiatry. 2010;71:1664–1672. doi: 10.4088/JCP.09m05859yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fristad MA, MacPherson HA. Evidence-Based Psychosocial Treatments for Child and Adolescent Bipolar Spectrum Disorders. Journal of Clinical Child & Adolescent Psychology. 2014;43:339–355. doi: 10.1080/15374416.2013.822309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Williams M, Zimerman B, Frazier J. WASH-U-KSADS (Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia) St. Louis, MO: Washington University; 1996. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Delbello MP, Bolhofner K, Craney JL, Frazier J, Beringer L, Nickelsburg MJ. DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. Journal of Child and Adolescent Psychopharmacology. 2002;12:11–25. doi: 10.1089/10445460252943533. [DOI] [PubMed] [Google Scholar]
- Ghaemi S, Bauer M, Cassidy F, Malhi G, Mitchell P, Phelps J, Vieta E, Youngstrom E. Diagnostic guidelines for bipolar disorder: A summary of the International Society for Bipolar Disorders Diagnostic Guidelines Task Force Report. Bipolar Disorders. 2008;10:117–128. doi: 10.1111/j.1399-5618.2007.00556.x. [DOI] [PubMed] [Google Scholar]
- Goldsmith M, Singh M, Chang K. Antidepressants and Psychostimulants in Pediatric Populations. Pediatr Drugs. 2011;13:225–243. doi: 10.2165/11591660-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz SM. Longitudinal Assessment of Manic Symptoms (LAMS) study: background, design, and initial screening results. The Journal of Clinical Psychiatry. 2010;71:1511–1517. doi: 10.4088/JCP.09m05835yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz SM, Hoagwood K, Stiffman AR, Summerfeld T, Weisz JR, Costello EJ, Rost K, Bean DL, Cottler L, Leaf PJ, Roper M, Norquist G. Reliability of the Services Assessment for Children and Adolescents. Psychiatric Services. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- Jensen-Doss A, Youngstrom EA, Youngstrom JK, Feeny NC, Findling RL. Predictors and moderators of agreement between clinical and research diagnoses for children and adolescents. Journal of Consulting and Clinical Psychology. 2014;82:1151–1162. doi: 10.1037/a0036657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kowatch RA, Youngstrom EA, Horwitz S, Demeter C, Fristad MA, Birmaher B, Axelson D, Ryan N, Frazier TW, Arnold LE, Young AS, Gill M, Findling RL. Prescription of Psychiatric Medications and Polypharmacy in the LAMS Cohort. Psychiatric Services. 2013;64:1026–1034. doi: 10.1176/appi.ps.201200507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauxen Peruzzolo T, Tramontina S, Rohde LA, Zeni CP. Pharmacotherapy of bipolar disorder in children and adolescents: an update. Revista Brasileira de Psiquiatria. 2013;35:393–405. doi: 10.1590/1516-4446-2012-0999. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Stoddard J. The developmental psychopathology of irritability. Development and Psychopathology. 2013;25:1473–1487. doi: 10.1017/S0954579413000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn P, Klein D, Seeley J. Bipolar disorders in a community sample of older adolescents: Prevalence, phenomenology, comorbidity, and course. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- Mayes SD, Waxmonsky JD, Calhoun SL, Bixler EO. Disruptive Mood Dysregulation Disorder Symptoms and Association with Oppositional Defiant and Other Disorders in a General Population Child Sample. Journal of Child and Adolescent Psychopharmacology. 2016;26:101–106. doi: 10.1089/cap.2015.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers O, Youngstrom E. A parent General Behavior Inventory subscale to measure sleep disturbance in pediatric bipolar disorder. Journal of Clinical Psychiatry. 2008;69:840–843. doi: 10.4088/jcp.v69n0518. [DOI] [PubMed] [Google Scholar]
- Miklowitz D. An update on the role of psychotherapy in the management of bipolar disorder. Current Psychiatry Reports. 2006;8:498–503. doi: 10.1007/s11920-006-0057-4. [DOI] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, Moffitt TE. The validity of the family history screen for assessing family history of mental disorders. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2009;150B:41–49. doi: 10.1002/ajmg.b.30764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacchiarotti I, Bond DJ, Baldessarini RJ, Nolen WA, Grunze H, Licht RW, Post RM, Berk M, Goodwin GM, Sachs GS. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. American Journal of Psychiatry. 2013;170:1249–1262. doi: 10.1176/appi.ajp.2013.13020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez Algorta GP, Van Meter A, Youngstrom EA. The Apple and the Tree. In: Yildiz A, Ruiz P, Nemeroff CB, editors. The Bipolar Book: History, Neurobiology, and Treatment. Oxford University Press; New York, NY: 2015. pp. 171–180. [Google Scholar]
- Perugi G, Angst J, Azorin JM, Bowden CL, Mosolov S, Reis J, Vieta E, Young AH. Mixed features in patients with a major depressive episode: the BRIDGE-II-MIX Study. The Journal of clinical psychiatry. 2015;76:351–358. doi: 10.4088/JCP.14m09092. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary Studies of the Reliability and Validity of the Children's Depression Rating Scale. Journal of the American Academy of Child Psychiatry. 1984;23:191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- Ravens-Sieberer U, Bullinger M. Revised Version, Manual. KINDL; Berlin, Germany: 2000. KINDL: Questionnaire for Measuring Health Related Quality of Life in Children and Adolescents. [Google Scholar]
- Robins E, Guze S. Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. American Journal of Psychiatry. 1970;126:983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children's Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Sisson D, Fristad M. The Parent Stress Survey, Psychology. The Ohio State University; Columbus, Ohio: 2001. [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Horwitz SM, Hoagwood K, Compton W, III, Cottler L, Bean DL, Narrow WE, Weisz JR. The Service Assessment for Children and Adolescents (SACA): Adult and Child Reports. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1032–1039. doi: 10.1097/00004583-200008000-00019. [DOI] [PubMed] [Google Scholar]
- Van Meter A, Moreira A, Youngstrom E. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. The Journal of Clinical Psychiatry. 2011a;72:1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- Van Meter A, Youngstrom E, Demeter C, Findling R. Examining the Validity of Cyclothymic Disorder in a Youth Sample: Replication and Extension. Journal of Abnormal Child Psychology. 2012a:1–12. doi: 10.1007/s10802-012-9680-1. [DOI] [PubMed] [Google Scholar]
- Van Meter A, Youngstrom E, Youngstrom J, Feeny N, Findling R. Examining the validity of cyclothymic disorder in a youth sample. Journal of Affective Disorders. 2011b;132:55–63. doi: 10.1016/j.jad.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Meter AR, Burke C, Youngstrom EA, Faedda GL, Correll CU. The Bipolar Prodrome: Meta-Analysis of Symptom Prevalence Prior to Initial or Recurrent Mood Episodes. Journal of the American Academy of Child & Adolescent Psychiatry. 2016;55:543–555. doi: 10.1016/j.jaac.2016.04.017. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Youngstrom EA. Cyclothymic disorder in youth: why is it overlooked, what do we know and where is the field headed? Neuropsychiatry. 2012;2:509–519. doi: 10.2217/npy.12.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Meter AR, Youngstrom EA, Findling RL. Cyclothymic disorder: A critical review. Clinical Psychology Review. 2012b;32:229–243. doi: 10.1016/j.cpr.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The Status of Irritability in Psychiatry: A Conceptual and Quantitative Review. Journal of the American Academy of Child & Adolescent Psychiatry. 2016;55:556–570. doi: 10.1016/j.jaac.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee H, Lee W, Ravens-Sieberer U, Erhart M, Li S. Validation of the English version of the KINDLR generic children’s health-related quality of life instrument for an Asian population – results from a pilot test. Quality of Life Research. 2005;14:1193–1200. doi: 10.1007/s11136-004-2957-2. [DOI] [PubMed] [Google Scholar]
- Young R, Biggs J, Ziegler V, Meyer D. A rating scale for mania: reliability, validity and sensitivity. The British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Youngstrom E. Definitional issues in bipolar disorder across the life cycle. Clinical Psychology: Science and Practice. 2009;16:140–160. [Google Scholar]
- Youngstrom E, Findling R, Danielson C, Calabrese J. Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychological Assessment. 2001;13:267–276. [PubMed] [Google Scholar]
- Youngstrom E, Youngstrom J, Starr M. Bipolar diagnoses in community mental health: Achenbach Child Behavior Checklist profiles and patterns of comorbidity. Biological Psychiatry. 2005;58:569–575. doi: 10.1016/j.biopsych.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Frazier TW, Findling RL, Calabrese JR. Developing a ten item short form of the Parent General Behavior Inventory to assess for juvenile mania and hypomania. Journal of Clinical Psychiatry. 2008;69:831–839. doi: 10.4088/jcp.v69n0517. [DOI] [PMC free article] [PubMed] [Google Scholar]