ABSTRACT
This study aimed to determine the economic burden and affecting factors in adult community-acquired pneumonia (CAP) patients (≥ 18 years) by retrospectively evaluating the data of 2 centers in Istanbul province, Turkey. Data of outpatients and inpatients with CAP from January 2013 through June 2014 were evaluated. The numbers of laboratory analyses, imaging, hospitalization days, and specialist visits were multiplied by the relevant unit costs and the costs of the relevant items per patient were obtained. Total medication costs were calculated according to the duration of use and dosage. The mean age was 61.56 ± 17.87 y for the inpatients (n = 211; 48.6% female) and 53.78 ± 17.46 y for the outpatients (n = 208; 46.4% male). The total mean cost was €556.09 ± 1,004.77 for the inpatients and €51.16 ± 40.92 for the outpatients. In the inpatients, laboratory, medication, and hospitalization costs and total cost were significantly higher in those ≥ 65 y than in those <65 y. Besides the hospitalization duration, specialist visit, imaging, laboratory, medication, and hospitalization costs and total cost were significantly higher in those hospitalized more than once than in those hospitalized once. While the specialist visit cost was higher in the inpatients with comorbidities, the imaging cost was higher in the outpatients with comorbidities. CAP poses a higher cost in inpatients, elders, and individuals with comorbidities. Costs can be decreased by rational decisions about hospitalization and antibiotic use according to the recommendations of guidelines and authorities. Vaccination may decrease medical burden and contribute to economy by preventing the disease, especially in risk groups.
KEYWORDS: adults, burden, Community-acquired pneumonia, cost, vaccination
Introduction
Community-acquired pneumonia (CAP) is still one of the reasons of morbidity and mortality all over the world. In adult population, the annual incidence of CAP has been reported as 5–11 in 1000 people in the prospective population studies from the UK,1 Finland,2 and North America.3 The economic burden of CAP, which is one of the most important reasons of deaths caused by infectious diseases in the developed countries, is also quite high.4 The annual expenditure for CAP is estimated to be 8.4–10 billion Dollars in the hospitals of United States of America and 10 billion Euros in Europe.4
Community-acquired pneumonia can cause a wide range of clinical entity from rapid improvement of the symptoms to severe complications and to death and CAP is life-threatening particularly in elders and individuals having comorbid diseases.5 There are many microorganisms leading to CAP; Streptococcus pneumoniae and Haemophilus influenza are the main causative agents.6,7 The most effective way to prevent CAP caused by S. pneumonia is vaccination. The 7-valent pneumococcal conjugate vaccine (PCV-7), which had been included in the national immunization program for children in our country, was replaced with 13-valent pneumococcal conjugate vaccine (PCV-13) in 2011.8 For adults, 2 pneumococcal vaccines are available, one of which is PCV-13 and the other is 23-valent pneumococcal polysaccharide vaccine (PPV-23).
While the advances in the knowledge about the natural course and prognosis of the disease, usage of biological markers (such as C-reactive protein and procalcitonin), and treatment approaches being more suitable with the introduction of national and international guidelines provide an improvement in CAP treatment, emergence of new pathogens and evolution of resistance to antibiotics as well as limited options of new antibiotics lead to difficulties in the treatment.9 Besides the ways to improve outcomes in CAP patients, the ways to reduce the costs are also being investigated. For this reason, in the scope of ensuring rational use of antibiotics, there are ongoing studies aiming at establishing current strategies on evaluating the approaches to decrease duration of use and dosage of antibiotics, treating patients at home rather than at hospital, switching to oral treatment from intravenous treatment in a short period of time, and decreasing the duration of hospitalization.4 Additionally, there is a gradual increase in penicillin resistance and multidrug resistance among S. pneumoniae isolates worldwide.10 In this context, it is important to know the current medical and economic burden of CAP in order for each geographical region to be able to make its own planning. The present study aimed to determine the economic burden and the affecting factors in adult CAP patients ≥ 18 y of age by retrospectively evaluating the data of 2 centers in Istanbul province, Turkey.
Results
Data of 208 inpatients (females, 48.6%) and 211 outpatients (females, 46.4%) were analyzed. The mean ages of the inpatients and outpatients were 61.56 ± 17.87 y and 53.78 ± 17.46 years, respectively. Of the patients, 42.6% were admitted to outpatient clinic, 12.4% were admitted to emergency services, and 1.1% were admitted by ambulance. Among inpatients, 36.5% had chronic obstructive pulmonary disease (COPD), 18.3% had hypertension, and 12.0% had diabetes mellitus. Among outpatients, 22.7% had COPD, 20.4% had asthma, and 7.1% had hypertension. The mean hospitalization duration of the inpatients was 6.81 ± 4.68 d (Table 1). When being ≥ 65 y of age or having any comorbidity was defined as a risk group for pneumococcal and influenza vaccination, 48.6% of the inpatients and 28.9% of the outpatients were in the ≥ 65 y of age group and 80.8% of the inpatients and 71.6% of the outpatients had a comorbid disease. However, only 2 patients, one from inpatients and one from outpatients, had previous pneumococcal vaccination.
Table 1.
Demographic and clinical characteristics of the patients with community-acquired pneumonia and the costs per patient.
| Inpatients n = 208 |
Outpatients n = 211 |
|
|---|---|---|
| Age, year, mean ± SD | 61.56 ± 17.87 | 53.78 ± 17.46 |
| Age group, n (%) | ||
| <65 | 107 (51.4) | 150 (71.1) |
| ≥ 65 | 101 (48.6) | 61 (28.9) |
| Gender, n (%) | ||
| Female | 101 (48.6) | 98 (46.4) |
| Male | 107 (51.4) | 113 (53.6) |
| Hospitalization duration day, mean ± SD | 6.81 ± 4.68 | — |
| Comorbid diseases, n (%) | ||
| COPD | 76 (36.5) | 48 (22.7) |
| Hypertension | 38 (18.3) | 15 (7.1) |
| Diabetes Mellitus | 28 (13.5) | 7 (3.3) |
| Heart diseases | 25 (12.0) | 6 (2.8) |
| Asthma | 14 (6.7) | 43 (20.4) |
| Costs per patient, €, mean ± SD | ||
| Specialist visit | 25.59 ± 17.98 | 7.63 ± 2.71 |
| Imaging | 26.78 ± 26.19 | 15.12 ± 14.8 |
| Laboratory | 48.94 ± 48.71 | 17.04 ± 22.37 |
| Medication | 314.65 ± 831.52 | 25.12 ± 23 |
| Hospitalization | 140.89 ± 148.11 | — |
| Total | 556.09 ± 1,004.77 | 51.16 ± 40.92 |
COPD, chronic obstructive pulmonary disease; SD, standard deviation.
The total mean cost per patient was €556.09 ± 1,004.77 for the inpatients and €51.16 ± 40.92 for the outpatients (Table 1). Medication cost had the highest share of total cost both in the inpatients and outpatients (Fig. 1).
Figure 1.
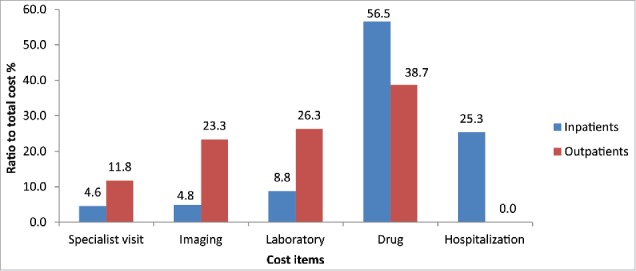
Ratios of cost items to the total cost in the inpatients and outpatients with community-acquired pneumonia.
In the inpatients, the costs of laboratory, medication, and hospitalization and the total cost were significantly higher in those ≥ 65 y than in those <65 y (Table 2).
Table 2.
Comparison of costs in the patients with community-acquired pneumonia regarding age groups.
| Inpatients |
Outpatients |
|||||
|---|---|---|---|---|---|---|
| Costs per patient, € | <65 y n = 107 Mean ± SD | ≥ 65 y n = 101 Mean ± SD | p | <65 y n = 150 Mean ± SD | ≥ 65 y n = 61 Mean ± SD | p |
| Specialist visit | 23.87 ± 17.09 | 27.41 ± 18.78 | 0.079 | 7.57 ± 2.65 | 7.80 ± 2.88 | 0.604 |
| Imaging | 25.90 ± 23.67 | 27.7 ± 28.68 | 0.745 | 14.33 ± 13.48 | 17.08 ± 17.64 | 0.360 |
| Laboratory | 42.11 ± 36.95 | 56.18 ± 57.98 | 0.014 | 18.19 ± 23.2 | 14.38 ± 20.32 | 0.097 |
| Medication | 203.6 ± 400.24 | 432.29 ± 1,110.98 | 0.004 | 22.98 ± 18.87 | 30.31 ± 30.39 | 0.300 |
| Hospitalization | 117.84 ± 88.39 | 165.31 ± 189.62 | 0.034 | — | — | — |
| Total | 412.37 ± 506.75 | 708.34 ± 1,331.19 | 0.014 | 49.25 ± 38.22 | 55.83 ± 46.92 | 0.459` |
SD, standard deviation.
There were 17 patients hospitalized more than once due to the diagnosis of CAP within the study period. In addition to the hospitalization duration, the costs of specialist visit, imaging, laboratory, medication, and hospitalization and the total cost were significantly higher in those hospitalized more than once compared with those hospitalized once (Table 3).
Table 3.
Characteristics of the patients regarding number of hospitalization due to community-acquired pneumonia and cost comparisons.
| More than one hospitalization n = 17 | One hospitalization n = 191 | p | |
|---|---|---|---|
| Age, year, mean ± SD | 69.41 ± 18.89 | 60.86 ± 17.66 | 0.050 |
| Hospitalization duration, day, mean ± SD | 14.35 ± 4.74 | 6.14 ± 4.06 | <0.001 |
| Costs per patient, €, mean ± SD | |||
| Specialist visit | 45.52 ± 22.56 | 23.82 ± 16.44 | <0.001 |
| Imaging | 42.96 ± 29.88 | 25.3 ± 25.4 | <0.001 |
| Laboratory | 78.76 ± 35.94 | 46.29 ± 48.88 | <0.001 |
| Medication | 589.40 ± 895.78 | 290.19 ± 823.62 | <0.001 |
| Hospitalization | 196.26 ± 63.86 | 135.97 ± 152.51 | <0.001 |
| Total | 952.89 ± 960.54 | 520.77 ± 1,003.42 | <0.001 |
SD, standard deviation.
While 19.7% (n = 41) of the inpatients had no comorbidities, 39.9% (n = 83) had one comorbidity, 24.0% (n = 50) had 2 comorbidities, 16.3% (n = 34) had 3 or more comorbidities. While 19.7% (n = 60) of the outpatients had no comorbidities, 35.5% (n = 75) had one comorbidity, 24.2% (n = 51) had 2 comorbidities, 11.8% (n = 25) had 3 or more comorbidities. Both in the inpatients and outpatients, the costs of laboratory and medication and the total costs were higher in those with comorbidities than in those without. The cost of specialist visit was higher in the inpatients with comorbidities whereas the cost of imaging was higher in the outpatients with comorbidities (Table 4).
Table 4.
Comparison of costs in the patients with community-acquired pneumonia regarding the presence of comorbidities.
| Inpatients | Outpatients | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Comorbidity |
Comorbidity |
||||||||
| Costs per patient, € | Present n = 168 mean ± SD | Absent n = 40 mean ± SD | p | Present n = 151 mean ± SD | Absent n = 60 mean ± SD | p | |||
| Specialist visit | 27.22 ± 18.90 | 18.75 ± 11.20 | 0.003 | 7.71 ± 2.74 | 7.45 ± 2.65 | 0.338 | |||
| Imaging | 26.94 ± 25.36 | 26.10 ± 29.88 | 0.356 | 16.69 ± 15.81 | 10.78 ± 10.53 | 0.002 | |||
| Laboratory | 51.27 ± 50.17 | 39.17 ± 41.17 | 0.018 | 18.37 ± 22.70 | 12.39 ± 20.89 | 0.009 | |||
| Medication | 326.36 ± 892.82 | 265.47 ± 503.42 | 0.041 | 27.46 ± 24.74 | 17.64 ± 14.00 | 0.019 | |||
| Hospitalization | 136.67 ± 134.24 | 158.65 ± 197.14 | 0.118 | — | — | — | |||
| Total | 567.81 ± 1,056.84 | 506.84 ± 756.76 | 0.016 | 58.06 ± 44.01 | 33.77 ± 24.63 | <0.001 | |||
SD, standard deviation.
In the outpatients, the mean medication cost was €39.56 ± 25.17 in those with ≥ 3 comorbidities and it was significantly higher than in those with one or 2 comorbidities (p = 0.008). Moreover, the mean total cost was €73.88 ± 54.96 and it was significantly higher in those with ≥ 3 comorbidities than in those with 1 comorbidity (Table 5).
Table 5.
Comparison of costs in the patients with community-acquired pneumonia according to the number of comorbidities.
| Inpatients | Outpatients | |||||||
|---|---|---|---|---|---|---|---|---|
| Number of comorbidities |
Number of comorbidities |
|||||||
| 1 | 2 | ≥ 3 | 1 | 2 | ≥ 3 | |||
| n = 83 | n = 50 | n = 34 | n = 75 | n = 51 | n = 25 | |||
| Costs per patient, € | mean ± SD | mean ± SD | mean ± SD | p | mean ± SD | mean ± SD | mean ± SD | p |
| Specialist visit | 25.93 ± 18.88 | 25.74 ± 15.12 | 33.11 ± 23.01 | 0.397 | 7.38 ± 2.27 | 8.10 ± 3.28 | 7.89 ± 2.86 | 0.495 |
| Imaging | 27.51 ± 24.88 | 24.15 ± 25.31 | 29.70 ± 26.90 | 0.328 | 16.77 ± 13.84 | 15.87 ± 16.26 | 18.22 ± 20.13 | 0.851 |
| Laboratory | 50.97 ± 59.04 | 48.05 ± 38.44 | 58.10 ± 41.88 | 0.179 | 14.62 ± 16.84 | 22.71 ± 27.27 | 19.93 ± 25.99 | 0.504 |
| Medication | 281.37 ± 660.95 | 342.68 ± 748.02 | 420.86 ± 1449.23 | 0.633 | 23.24 ± 22.10c | 26.89 ± 26.24c | 39.56 ± 25.17aba,b | 0.008 |
| Hospitalization | 139.79 ± 156.98 | 116.69 ± 57.05 | 160.77 ± 154 | 0.319 | — | — | — | — |
| Total | 524.56 ± 884.52 | 557.31 ± 817.63 | 702.55 ± 1638.7 | 0.428 | 48.82 ± 36.39c | 63.89 ± 45.97 | 73.88 ± 54.96a | 0.045 |
SD, standard deviation.
different from those with 1 comorbidity;
different from those with 2 comorbidities
different from those with ≥ 3 comorbidities.
There was no significant increase in the mean total cost with an increase in the number of comorbidities in the inpatients <65 y of age (€444.94 ± 437.79 for 1 comorbidity, €424.37 ± 530.60 for 2 comorbidities, and €420.65 ± 303.32 for ≥ 3 comorbidities; p = 0.822). There was also no significant increase in the mean total cost with an increase in the number of comorbidities in the inpatients ≥ 65 y of age (€ 598.62 ± 1,156.66 for 1 comorbidity, €653.58 ± 972.61 for 2 comorbidities, and €984.44 ± 2,297.32 for ≥ 3 comorbidities; p = 0.365). Similarly, in the outpatients, there was also no significant increase in the mean total cost with an increase in the number of comorbidities in those <65 y of age (€46.74 ± 34.13 for 1 comorbidity, €64.17 ± 47.87 for 2 comorbidities, and €65.93 ± 39.64 for ≥ 3 comorbidities; p = 0.091). However, the mean medication cost was found to be €37.80 ± 25.17 in those with ≥ 3 comorbidities and it was significantly higher than in those with 1 comorbidity (€20.88 ± 18.21; p = 0.021). In the outpatients ≥ 65 y of age, no significant increase was noted in the mean total cost with an increase in the number of comorbidities (€52.98 ± 40.95 for 1 comorbidity, €63.24 ± 42.62 for 2 comorbidities, €90.76 ± 79.28 for ≥ 3 comorbidities; p = 0.452).
The linear regression analysis performed to examine the impact of the factors on the total cost in all patients revealed that age (≥ 65 years), male gender, and being inpatient were the significant factors (p = 0.041, p = 0.027, and p<0.001, respectively; Table 6). When the analysis was performed separately for inpatients and outpatients, it was observed that the significant factors affecting the total cost were the length of hospital stay and admission to intensive care unit in the inpatients and the presence of comorbidity in the outpatients (p<0.001 for each; Table 7).
Table 6.
Factors affecting the total cost in all patients.
| Factors | p | Coefficients |
|---|---|---|
| Constant | 0.375 | −76.136 |
| Age (≥ 65 years) | 0.041 | 153.763 |
| Gender (Male) | 0.027 | 157.797 |
| Patient status (Inpatient) | <0.001 | 477.457 |
| Presence of comorbidity | 0.997 | −0.319 |
Total cost = −76.136+153.763 * (Age (≥ 65 years))+ 157.797*(Gender (Male))+ 477.457*(Patient status (Inpatient))+ −0.319*Presence of comorbidity.
Table 7.
Factors affecting the total cost in the inpatients and outpatients.
| Inpatientsa | ||
|---|---|---|
| Factors | p | Coefficients |
| Constant | 0.001 | −415.577 |
| Age (≥ 65 years) | 0.506 | 65.376 |
| Gender (Male) | 0.864 | 16.711 |
| Presence of comorbidity | 0.469 | 88.377 |
| Length of hospital stay | <0.001 | 119.664 |
| Admission to ICU | <0.001 | 752.723 |
| Outpatientsb | ||
| Factors |
p |
Coefficients |
| Constant | <0.001 | 32.432 |
| Age (≥ 65 years) | 0.500 | 4.100 |
| Gender (Male) | 0.857 | 0.996 |
| Presence of comorbidity | <0.001 | 23.759 |
ICU, intensive care unit.
Total cost = −415.577+65.376* (Age (≥ 65 years))+ 16.711*(Gender (Male))+ 88.377*Presence of comorbidity+752.723* Admission to ICU.
Total cost = 32.432+4.100* (Age (≥ 65 years))+ 0.996*(Gender (Male))+ 23.759*Presence of comorbidity.
Discussion
Community-acquired pneumonia continues to be one of the main public health problems due to its medical and economic burden. While the incidence of CAP varies across countries, it is estimated to be 12 cases in 1000 people annually. According to the results of the Project of National Disease Burden and Cost-Effectiveness, pneumonia ranked 15th by 1.15% among the first 20 acute and chronic diseases diagnosed by a physician in the household survey.11 In patients with CAP, hospitalization rate varies between 30% and 60%.12,13 Besides, it has been reported that more than 95% of treatment costs of CAP account for hospitalized patients.12 In their review including studies on clinical and economic burden of CAP published within a period of 18 y in Europe, Welte et al.14 observed increases in the disease incidence and hospitalization throughout the years. It is known that the elderly population is gradually increasing worldwide.15 This condition will cause more of an increase in the clinical and economic burden of CAP in the future.
The costs of CAP for outpatients and inpatients are being investigated in many regions of the world (Table 8). The reasons such as using different cost analysis methods and including different parameters in the calculations, evaluating different adult groups (≥ 18 y, ≥ 50 y, ≥ 65 y etc.), including patients with microbiologically proven diagnosis or clinical diagnosis, and selecting patients from the general population or admitted to tertiary hospital lead to difficulties in comparing study results. Nevertheless, the common point in the studies is that cost per patient is high and its reflection to total annual cost is expressed in million dollars.
Table 8.
Inpatient and outpatient costs for community-acquired pneumonia in different studies from the literature.
| Number of Cases or Episodes |
Costs |
|||||||
|---|---|---|---|---|---|---|---|---|
| Reference | Study Location | Data Source | Period | Age (years) | Inpatients | Outpatients | Inpatients | Outpatients |
| Sato et al.16 | USA | A large, proprietary US health insurance database | 2006–2008 | ≥ 50 years | 8,121 patients | 20,454 patients | US$27,661 per episode | US$2,212 per episode |
| Yu et al.17 | USA | Medicare Standard Analytic Files (Nationwide) | 2007–2008 | ≥ 18 years | 25,114 episodes | 40,690 episodes | US$18,670 per episode | US$2,394 per episode |
| Reyes et al.18 | Spain | Hospital-based | N/A | ≥ 18 years | 271 | N/A | €1,683 (median total cost) | N/A |
| Tichopad et al.19 | Czech Republic, Slovakia, Poland, and Hungary | Health ministry and insurance reimbursement claims | 2009 | ≥ 50 years | N/A | N/A | €431.54-€1,044.70 (total cost per case) | €4.44-€71.04 (total cost per case) |
| Song et al.20 | Asia-Pacific region | Literature-based | 1990–2010 | ≥ 18 years | N/A | N/A | US$3,456 per episode | US$165 per episode |
| Doruk et al.21 | Turkey | Hospital-based | 2004–2005 | Average age of 70.9 years | 114 | N/A | €1,630.77 (total cost) | N/A |
| Current study | Turkey | Hospital-based | 2013–2014 | ≥ 18 years | 208 | 211 | €556.09 ± 1,004.77 (total mean cost per patient) | €51.16 ± 40.92 (total mean cost per patient) |
N/A, Not available.
One of the important points in the decision of approaching CAP patients is whether a patient should be treated as inpatient or outpatient and many factors affect this decision. These factors include severity of the clinical condition of a patient, presence of risk factors (such as age and comorbidity), and duration and route of antibiotic treatment as well as socioeconomic factors such as patients' compliance, use of medical resources, and insurance status. The objective decision of hospitalization using pneumonia severity index (PSI) at baseline is recommended.22 Nevertheless, in their study, Kozma et al.23 evaluated 1,471,295 CAP admissions and found the mean hospitalization duration to be 6.3 d. They showed that reducing the hospitalization due to CAP by one day provided a decrease in cost per hospitalization by US$2,273-US$2,373. Raut et al.24 investigated the economic effect of reducing the duration of hospitalization due to CAP, the mean of which was 5.3 d. They reported that a half-day reduction in hospitalization would decrease in cost per case by US$724 (range, US$457-US$846) when the cost per day was estimated US$1,448. They indicated that its reflection in saving across the USA would be 813 million Dollars (range, 513–950 million dollars) annually considering the prevalence of CAP and the rate of hospitalization. In the present study, the mean hospitalization duration was 6.81 days, which was higher than those reported in the above-mentioned studies. Since daily packet price is applied for CAP in Turkey, every extra day of hospitalization will increase total cost. Accordingly, hospitalizing patients according to their indications based on national guidelines, continuing the treatments of patients at home within the shortest possible time after eliminating the criteria for hospitalization, and improving home care facilities would decrease total cost. Moreover, providing switching to oral antibiotic therapy from intravenous therapy by shortening hospitalization duration may be another intervention that would reduce total cost.
Advanced age is one the effective factors for the cost of CAP. It has been reported that medical burden of CAP increases with age and that the incidence, mortality, and hospitalization of CAP increase with advanced age.19 In the study by Tokgöz et al.,25 direct hospital costs and factors affecting these costs for inpatients (n = 87) with the diagnosis of CAP were evaluated and mean duration of hospitalization and total cost did not differ between the inpatients divided into 2 groups considering the age of 65 y. Bartolomé et al.26 compared total direct cost per case between patients aged <65 y and ≥ 65 y and found that there was no difference between 2 groups in inpatients, whereas the cost was found to be significantly higher in outpatients aged ≥ 65 y (€190 ± 77 vs. €263 ± 145, p = 0.031). Reyes et al.18 reported that age did not increase the cost, which might be attributed to the high mean age (70 ± 15 years) of their patients. Lee et al.27 investigated the burden of CAP in adults aged ≥ 50 y in 11 hospitals in Korea and total per-capita medical fees were found to be higher in patients aged ≥ 65 y than in those aged <65 y (US$2,088 vs. US$1,701). In the present study, the laboratory, medication, hospitalization, and total costs were found to be significantly higher in CAP inpatients aged ≥ 65 y compared with those aged <65 y.
Presence of comorbidity is reported to be another factor with an increasing effect on costs.21,28 Polsky et al.28 investigated the contributions of some selected comorbid conditions to cost of CAP in the working population in the USA and evaluated 402,831 CAP cases identified in asthma, diabetes, COPD or congestive heart failure patients. While the mean excess cost was determined as US$14,429, the minimum cost increase was determined in asthma and the maximum cost increase was determined in congestive heart failure. They also reported the cost increase reaching up to 2–3 times in patients with comorbidity compared with those without. In the study by Lee et al.,27 hospitalization was found to be longer and total per-capita medical fees was found to be higher (US$2074 vs. US$1440) in patients with comorbidity compared with those without. In the present study, the costs increased both in outpatients and inpatients in the presence of comorbidity. Therefore, better management of comorbidities would decrease hospitalization and thereby would reduce cost in patients with comorbidities such as asthma, COPD, diabetes mellitus, congestive heart failure, and chronic renal failure. In the present study, the mean cost per patient was found to be lower than those reported in the studies from other countries. This low cost in Turkish setting can be attributed to the lower reimbursed prices of both pharmaceuticals and medical operations (e.g., surgery, magnetic resonance emergency, hospitalization, etc.) due to low level of unit prices as compared with those in other countries.
In the present study, medication cost was found to have the highest share in the total cost in both outpatients and inpatients with CAP (38.7% and 56.5%, respectively). In the study by Bartolomé et al.,26 the share of antibiotic therapy was 22% in the total cost (inpatient care 18.9%, outpatient care 3.1%). To decrease the economic burden of CAP, investigators suggest various recommendations. In approaching to CAP patients, following the recommendations of the guidelines has been reported to reduce the use of wide spectrum antibiotics and the rate of hospitalization in patients without risk factors.29 This will also cause a decrease in direct costs. It has been also shown in studies that antibacterial treatment applied according to the guidelines shortens the duration of hospitalization and reduces the costs.12 Studies have also demonstrated that medication costs and treatment failure are increased and this cause economically negative outcomes in regions where antibiotic resistance is a problem. 30 For this reason, especially in case empirical therapy is initiated, beside following the current guidelines, it is necessary to be aware of the regional resistance patterns.
In the large scale study by Broulette et al.31 on the cost of CAP, it was reported that to decrease the morbidity and cost of CAP, strategies including vaccination for working-age adults having underlying medical problems might be the best method of prevention. Moreover, to date, vaccination has been reported as only proven method of prevention from CAP. In the present study, only 2 patients had previous pneumococcal vaccination. This low vaccination rate could be attributed to the retrospective design of the study. Yet currently, adult pneumococcal vaccination schedule has also been defined in the content of “Risk Group Immunization” document in 201632 by the Ministry of Health. PCV13 is available in the national risk group immunization program and PPV-23 has been reimbursed only for risk groups.
The main limitation of the present study was the evaluation of only direct costs. Since the study had a retrospective design, indirect costs could not be taken into consideration within the scope of the study. Future studies including the evaluation of indirect costs may show further increase in the economic burden of pneumonia. Another limitation was the calculation of the medication cost. As medication costs for CAP are reimbursed as a daily packet price (including costs for antibiotics, analgesics, antipyretics, parenteral fluids, antiemetics, and oxygen and medications related to comorbid diseases) in Turkey, it was not possible to perform sub-analyses for individual medication costs from the existing data, especially for antibiotics. Moreover, yet due to the retrospective design of the study, another limitation was lack of information about whether low severity CAP patients were inappropriately hospitalized, whether any patient received broad-spectrum antibiotics inappropriately, and whether any patient stayed in hospital unnecessarily after attaining clinical stability.
Conclusion
In conclusion, CAP, a disease with a high medical and economic burden, poses a higher cost in inpatients, elders, and individuals with comorbidities. Costs can be decreased by rational decisions about hospitalization and antibiotic use according to the recommendations of guidelines and authorities; moreover, vaccination may decrease the medical burden and contribute to economy by preventing the disease, especially in risk groups. Further large-scale studies conducted in different hospitals are needed to support the above-mentioned outcomes, particularly in Turkey.
Methodology
Data of the patients aged ≥ 18 years, who were admitted with the diagnosis of CAP identified through ICD-10 coding (J13, J15-J18) and confirmed by radiologic evaluations from January 2013 through June 2014, were retrospectively evaluated from the database of 2 centers. One center was Acıbadem Maslak Hospital, a private hospital, and the other center was Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, a public hospital, both which are qualified according to the Ministry of Health in terms of registration of database. From each hospital, approximately 200 patients corresponding to the monthly average number of CAP patients in these hospitals were enrolled using a computer-based randomization stratified by gender. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Acibadem University Medical Research Assessment Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Patients who received treatment at a hemodialysis center within the last 30 days, were hospitalized for ≥ 2 d in the last 90 days, and were receiving home infusion therapy and/or decubitus ulcer treatment and/or chemotherapy, those with suspicion of pregnancy, pregnant women, and those on breastfeeding were excluded due to the possibility of having hospital-acquired pneumonia.
In addition to the demographic data of the patients, comorbidities, laboratory analyses, imaging, treatments, clinical units where the patients were examined, hospitalization days in the wards and intensive care units, number of consultations during hospitalization and the specialties of the physicians performing the consultations, examination findings and suggested treatments during control visits were recorded from the hospital database. The numbers of laboratory analyses, imaging, hospitalization days, and specialist visits of all patients were multiplied by the unit price indicated in the Health Practices Statement (HPS) Appendix-2B (Updated Statement of Changes 2013 HPS, dated August 30, 2014) and the costs of the relevant items per patient were obtained. Reimbursed pack prices of the medications were obtained from the RxMediaPharma® Interactive Drug Information Resource in December 2014 and the total medication costs were calculated according to the duration of use and dosage. All costs were expressed in Euros according to the 2014 currency of Turkish Liras (€1.00 = 2.9 Turkish Liras, without inflation adjustment).
Statistical analysis
Data analyses were performed using the Predictive Analytics Software (PASW) version 18.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were expressed as number and percentage for categorical variables and as mean ± standard deviation for numerical variables. For non-normally distributed numerical variables, independent 2 group comparisons were performed using Mann-Whitney U test and independent multiple group comparisons were performed using Kruskal-Wallis test. A linear regression analysis was performed to determine the factors affecting the total cost. A p value <0.05 was considered significant.
Disclosure of potential conflicts of interest
This research is sponsored by Pfizer Pharmaceuticals.
Filiz Kosar and Caglar Cuhadaroglu received honorarium approved by the ethical committee.
Acknowledgment
Thank Omega CRO for their support in the statistical analysis of the study.
References
- [1].Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987; 1(8534):671-4; PMID:2882091; https://doi.org/ 10.1016/S0140-6736(87)90430-2 [DOI] [PubMed] [Google Scholar]
- [2].Jokinen C, Heiskanen L, Juvonen H, Kallinen S, Karkola K, Korppi M, Kurki S, Rönnberg RR, Seppä A, Soimakallio S, et al.. Incidence of community-acquired pneumonia in the population of four municipalities in eastern Finland. Am J Epidemiol 1993; 137(9):977-88; PMID:8317455; https://doi.org/ 10.1093/oxfordjournals.aje.a116770 [DOI] [PubMed] [Google Scholar]
- [3].Foy HM, Cooney MK, Allan I, Kenny GE. Rates of pneumonia during influenza epidemics in Seattle, 1964 to 1975. JAMA 1979; 241(3):253-8; PMID:758528 [PubMed] [Google Scholar]
- [4].Mertz D, Johnstone J. Modern management of community-acquired pneumonia: Is it cost-effective and are outcomes acceptable? Curr Infect Dis Rep 2011; 13(3):269-77; PMID:21400249; https://doi.org/ 10.1007/s11908-011-0178-8 [DOI] [PubMed] [Google Scholar]
- [5].Brar NK, Niederman MS. Management of community-acquired pneumonia: a review and update. Ther Adv Respir Dis 2011; 5(1):61-78; PMID:20935033; https://doi.org/ 10.1177/1753465810381518 [DOI] [PubMed] [Google Scholar]
- [6].Gadsby NJ, Russell CD, McHugh MP, Mark H, Conway Morris A, Laurenson IF, Hill AT, Templeton KE. Comprehensive molecular testing for respiratory pathogens in community-acquired pneumonia. Clin Infect Dis 2016; 62(7):817-23; PMID:26747825; https://doi.org/ 10.1093/cid/civ1214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM. Community-acquired pneumonia requiring hospitalization among U.S. Adults N Engl J Med 2015; 373(5):415-27; https://doi.org/ 10.1056/NEJMoa1500245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sağlık Bakanlığı Temel Sağlık Hizmetleri Genel Müdürlüğü. Genişletilmiş Bağışıklama Programı Genelgesi. Sayı: B100TSH0110005, Tarih: 13.03.2009/7941. [Google Scholar]
- [9].Niederman MS. Recent advances in community-acquired pneumonia: inpatient and outpatient. Chest 2007; 131(4):1205-15; PMID:17426229; https://doi.org/ 10.1378/chest.06-1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Dagan R, Klugman KP. Impact of conjugate pneumococcal vaccines on antibiotic resistance. Lancet Infect Dis 2008; 8(12):785-95; PMID:19022193; https://doi.org/ 10.1016/S1473-3099(08)70281-0 [DOI] [PubMed] [Google Scholar]
- [11].T.C. Sağlık Bakanlığı. Refik Saydam Hıfzıssıhha Merkezi Başkanlığı, Hıfzıssıhha Mektebi Müdürlüğü, Başkent Üniversitesi Ulusal Hastalık Yükü ve Maliyet-Etkililik Projesi; 2004 [Google Scholar]
- [12].Brown PD. Adherence to guidelines for community-acquired pneumonia: does it decrease cost of care? Pharmacoeconomics 2004; 22(7):413-20; PMID:15137880; https://doi.org/ 10.2165/00019053-200422070-00001 [DOI] [PubMed] [Google Scholar]
- [13].Polverino E, Torres Marti A. Community-acquired pneumonia. Minerva Anestesiol 2011; 77(2):196-211; PMID:21242952 [PubMed] [Google Scholar]
- [14].Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax 2012; 67(1):71-9; PMID:20729232; https://doi.org/ 10.1136/thx.2009.129502 [DOI] [PubMed] [Google Scholar]
- [15].United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Ageing 2013 ST/ESA/SER.A/348 Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf [Google Scholar]
- [16].Sato R, Gomez Rey G, Nelson S, Pinsky B. Community-acquired pneumonia episode costs by age and risk in commercially insured US adults aged ≥ 50 years. Appl Health Econ Health Policy 2013; 11(3):251-8; PMID:23605251; https://doi.org/ 10.1007/s40258-013-0026-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yu H, Rubin J, Dunning S, Li S, Sato R. Clinical and economic burden of community-acquired pneumonia in the Medicare fee-for-service population. J Am Geriatr Soc 2012; 60(11):2137-43; PMID:23110409 [DOI] [PubMed] [Google Scholar]
- [18].Reyes S, Martinez R, Vallés JM, Cases E, Menendez R. Determinants of hospital costs in community-acquired pneumonia. Eur Respir J 2008; 31(5):1061-7; PMID:18448502; https://doi.org/ 10.1183/09031936.00083107 [DOI] [PubMed] [Google Scholar]
- [19].Tichopad A, Roberts C, Gembula I, Hajek P, Skoczynska A, Hryniewicz W, Jahnz-Rozyk K, Prymula R, Solovič I, Kolek V. Clinical and economic burden of community-acquired pneumonia among adults in the Czech Republic, Hungary, Poland and Slovakia. PLoS One 2013; 8(8):e71375; PMID:23940743; https://doi.org/ 10.1371/journal.pone.0071375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Song JH, Thamlikitkul V, Hsueh PR. Clinical and economic burden of community-acquired pneumonia amongst adults in the Asia-Pacific region. Int J Antimicrob Agents 2011; 38(2):108-17; PMID:21683553 [DOI] [PubMed] [Google Scholar]
- [21].Doruk S, Tertemiz KC, Kömüs N, Uçan ES, Kilinç O, Sevinç C. Community acquired pneumonia and direct hospital cost. Tuberk Toraks 2009; 57(1):48-55; PMID:19533437 [PubMed] [Google Scholar]
- [22].Aujesky D, Fine MJ. Community-acquired pneumonia: treatment at home or in the hospital? Am J Med 2008; 121(12):1038-40; PMID:19028194 [DOI] [PubMed] [Google Scholar]
- [23].Kozma CM, Dickson M, Raut MK, Mody S, Fisher AC, Schein JR, Mackowiak JI. Economic benefit of a 1-day reduction in hospital stay for community-acquired pneumonia (CAP). J Med Econ 2010; 13(4):719-27; PMID:21091099; https://doi.org/ 10.3111/13696998.2010.536350 [DOI] [PubMed] [Google Scholar]
- [24].Raut M, Schein J, Mody S, Grant R, Benson C, Olson W. Estimating the economic impact of a half-day reduction in length of hospital stay among patients with community-acquired pneumonia in the US. Curr Med Res Opin 2009; 25(9):2151-7; PMID:19601711; https://doi.org/ 10.1185/03007990903102743 [DOI] [PubMed] [Google Scholar]
- [25].Tokgöz Akyıl F, Hazar A, Erdem İ, Pehlivan Öneş C, Yalçınsoy M, Irmak İ, Kasapoğlu US. Hospital treatment costs and factors affecting these costs in community-acquired pneumonia. Turk Thorac J 2015; 16:107-13; https://doi.org/ 10.5152/ttd.2015.4609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Bartolomé M, Almirall J, Morera J, Pera G, Ortún V, Bassa J, Bolíbar I, Balanzó X, Verdaguer A; maresme community-acquired pneumonia study group (GEMPAC). A population-based study of the costs of care for community-acquired pneumonia. Eur Respir J 2004; 23(4):610-6; PMID:15083763; https://doi.org/ 10.1183/09031936.04.00076704 [DOI] [PubMed] [Google Scholar]
- [27].Lee JY, Yoo CG, Kim HJ, Jung KS, Yoo KH. Disease burden of pneumonia in Korean adults aged over 50 years stratified by age and underlying diseases. Korean J Intern Med 2014; 29(6):764-73; PMID:25378975; https://doi.org/ 10.3904/kjim.2014.29.6.764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Polsky D, Bonafede M, Suaya JA. Comorbidities as a driver of the excess costs of community-acquired pneumonia in U.S. commercially-insured working age adults. BMC Health Serv Res 2012; 12:379; PMID:23113880; https://doi.org/ 10.1186/1472-6963-12-379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Barlow G, Nathwani D, Davey P. The effect of implementing the British Thoracic Society community-acquired pneumonia guidelines on antibiotic prescribing and costs in a UK teaching hospital. Clin Microbiol Infect 2006; 12(5):498-500; PMID:16643534; https://doi.org/ 10.1111/j.1469-0691.2006.01387.x [DOI] [PubMed] [Google Scholar]
- [30].Asche C, McAdam-Marx C, Seal B, Crookston B, Mullins CD. Treatment costs associated with community-acquired pneumonia by community level of antimicrobial resistance. J Antimicrob Chemother 2008; 61(5):1162-8; PMID:18310136; https://doi.org/ 10.1093/jac/dkn073 [DOI] [PubMed] [Google Scholar]
- [31].Broulette J, Yu H, Pyenson B, Iwasaki K, Sato R. The incidence rate and economic burden of community-acquired pneumonia in a working-age population. Am Health Drug Benefits 2013; 6(8):494-503; PMID:24991378 [PMC free article] [PubMed] [Google Scholar]
- [32].T. C. Sağlık Bakanlığı. Türkiye Halk Sağlığı Kurumu Risk Grubu Aşılamaları Tarih: 17.06.2016, Sayı: 21001706. [Google Scholar]


