ABSTRACT
Background: The suspension of compulsory scheduling of some pediatric vaccines has been discussed for a long time by health authorities in Italy but the current decrease of vaccination rates is a matter of concern. YouTube is the most popular video-based social media website. Considering the demonstrated impact of internet on vaccination decision-making and the increasing use of social media to share and disseminate health information, the aim of this study was to explore the message available on YouTube videos about vaccination.
Methods: An observational study was conducted searching for YouTube videos in September 2015 and updated in January 2016, by using the keyword “vaccinations.” We included recently posted videos in Italian on child vaccination (2014–2015). Videos were classified according to the message tone.
Results: A total of 123 videos were selected. Pro-vaccination videos were 62 (50%), anti-vaccination 28 (23%), neutral or without a clear position in favor or against vaccination 33 (27%). Focusing on the first 2 groups, pro-vaccination videos had a higher number of views compared with those unfavorable (1602 ± 6544 vs 1482 ± 2735) (p < 0.001). However, anti-vaccination videos were liked more by viewers (17.8 ± 31.3) than positive ones (13.2 ± 44.7) (p < 0.001) in addition to being more shared (23 ± 22.6 vs 3.8 ± 5.5, p < 0.001).
Conclusions: Most of the videos were positive in tone, but those that disapproved of immunization were the most liked and shared. Considering the growing number of viewers, it is important to monitor the web to understand audience characteristics and what influences public opinions to use communication strategies more effectively.
KEYWORDS: communication, internet, vaccination, YouTube videos
Introduction
In Italy the shift from compulsory to voluntary immunization has been a matter of discussion for a long time.1,2 Italy's National Vaccination Plan (NVP-2005–7)3 brought for the first time the possibility for regions to suspend the sanctions associated with compulsory pediatric vaccinations, i.e. diphtheria, tetanus, poliomyelitis and hepatitis B vaccinations. Since then, only the Veneto region suspended compulsory immunization because they met the criteria provided by the NVP, i.e., high immunization coverage and effective surveillance system. Vaccine coverage monitoring, performed in this region in 2013 and regarding the 2008–2012 birth cohorts,4 revealed a slight decline of immunization coverage rates for all the mandatory vaccinations, though levels remain above the 95% target, recommended by the World Health Organization to eliminate measles from the European Region.5
Overall, in recent years in Italy there has been a gradual decrease in vaccination coverage. More than half of the Italian regions do not meet the 95% coverage rate for pediatric immunization programs, set by the Ministry of Health.6 At the national level, measles-mumps-rubella (MMR) vaccination coverage dropped from 90.6% to 86.7% between 2010 and 2014.6
The Italian situation is characterized by significant different immunization policies among regions arising also from conflicting opinions on mandatory vaccination. Those who are in favor of compulsory vaccination argue that it is a public health interest issue and it is the way to guarantee high coverage rate. In contrast, freedom of choice in health matters, parental autonomy, the right to refuse health care are some of the main arguments against mandatory vaccination.1,2 In fact, as clearly discussed by Pelullo and colleagues,2 the major obstacle to moving toward voluntary immunization in Italy is the fear of reducing coverage rates, arising from the awareness of significant sociocultural and economic differences among Italian regions that lead to think that the positive experience of Veneto region would not be followed by all the other regions. It should be noted that the shift to voluntary immunization implies effective and clear public communication, necessary to motivate free individual choice,7 however this uneven situation in terms of immunization policies may contribute to create further uncertainty in the population. This uncertainty obviously does not benefit a widespread loss of confidence in vaccines in the general population, a phenomenon known as vaccine hesitancy.7-9 The increasing use of internet as a source of health-related information,10,11 and particularly web 2.0 applications contributed to feed vaccine hesitancy.7,12 Twitter, Facebook, Google+ and YouTube have gained popularity mainly because they allow and promote interactions among users, enabling also people to easily find health information outside of a scientific context. This means more chances of running into information lacking quality and accuracy.8 The problem is that these channels are widely used by anti-vaccine movements13-15 allowing the spread of misinformation about vaccination and contributing to foster the doubts and uncertainties particularly about safety and efficacy of vaccines, also in people that are aware that vaccines have an important role in public health.8,12 This is a critical aspect considering that the probability to find negative contents related to vaccination in the discussions of online forums and social networks is higher than the probability to find positive messages about vaccination.13
The influence of internet on vaccination-related decisions16,17 is well documented. For instance, the main source of information for parents who decided to postpone or abstain from MMR vaccination was media including internet as reported in a survey performed in Sweden.18 Another research found that accessing vaccine-critical websites for 5 to 10 minutes decreased the intention to vaccinate compared with viewing a controlled website hosted by an health institution.19
YouTube has become the most successful networked video-sharing platform with more than a billion users, almost a third of all users on the Internet, and every day people watch hundreds of millions of hours of videos on this platform and generate billions of views.20 A recent Italian survey performed at a national level showed that YouTube is an important source of information used by 54% of young people aged 14–29 and 34% of adults aged 30–44.12
Recently a systematic review about healthcare information on YouTube21 showed that the probability of YouTube disseminating misleading information to healthcare consumers is high.
There are few studies that evaluate how YouTube is used as a channel to share immunization information,22 and among these ones, HPV (Human papilloma virus)-vaccination is the major topic being addressed.23-26 The aim of the current research is thus to examine the content of Italian YouTube videos related to pediatric vaccinations in general and understand the potential of messages in influencing public awareness and opinions. It is interesting to emphasize that the World Health Organization, in a recent public notice, recommends to constantly monitor vaccine hesitancy and all determinants related with it.27 In a context where there is a will, at the national level, to move from compulsory to voluntary immunization, web monitoring could be important in guiding immunization policies.
Results
Out of 200 videos sorted by upload date, we selected 123 (62%) (Supplemental Material-Appendix 1). Out of the 77 videos that did not meet the inclusion criteria, 63 were not pertinent to child immunization in Italy, 7 were duplications, 5 didn't run, and 2 were in English. All the videos available in September 2015 were also active in January 2016.
Sixty-two (50%) YouTube videos supported vaccinations, 28 (23%) were against vaccination, 18 (15%) were neutral and 15 (12%) were ambiguous. In the statistical analyses, neutral and ambiguous videos were collapsed into one group called “others.” The results did not change when the 4 categories were considered. The main characteristics of videos according to the message tone are reported in Table 1.
Table 1.
Characteristics of YouTube videos according to the video tone.
| Parameter | Positive (N = 62) | Negative (N = 28) | Others (N = 33) | P value |
|---|---|---|---|---|
| Length, min (mean ± SD) | 6.7( ± 13.4) | 28.6( ± 44) | 21.7( ± 45.6) | <0.001* |
| Time since upload, days (mean ± SD) | 368( ± 121) | 384( ± 133) | 416( ± 130) | Ns** |
| Total views (mean ± SD) | 1602( ± 6544) | 1482( ± 2735) | 270( ± 406) | <0.001* |
| Likesa (mean ± SD) | 13.2( ± 44.7) | 17.8( ± 31.3) | 5.2( ± 6.2) | <0.001** |
| Precence of likes n(%) | 19 (31%) | 25 (89%) | 14 (42%) | <0.001# |
| Dislikesb (mean ± SD) | 1.7( ± 1) | 2.4( ± 2.8) | 1.5( ± 0.7) | Ns** |
| Presence of dislikes n(%) | 14 (23%) | 13 (46%) | 2 (6%) | 0.001 |
| Commentsc (mean ± SD) | 3.7( ± 5) | 3.9( ± 5.7) | 1.6( ± 0.5) | Ns** |
| Presence of comments n(%) | 10 (16%) | 14 (50%) | 7(21%) | 0.001# |
| Sharesd (mean ± SD) | 3.8( ± 5.5) | 23( ± 22.6) | 4.9( ± 6.6) | <0.001** |
| Presence of shares n(%) | 17 (27%) | 24 (86%) | 18(55%) | <0.001# |
| Source n(%) | ||||
| Health professional | 27(44%) | 7(25%) | 3(9%) | 0.002# |
| No health professional | 35(56%) | 21(75%) | 30(91%) | |
| Topic n(%) | ||||
| General vaccination | 25(40%) | 24(86%) | 18(55%) | <0.001# |
| Specific vaccinationse | 37(60%) | 4(14%) | 45(45%) |
Anova test;
Kruskal-Wallis rank test; # Fisher's exact test
ns: not significant
n = 19 positive, n = 25 negative andn = 14 other videos where at least a “like” was present;
n = 14 positive, n = 13 negative and n = 2 other videos where at least a “dislike” was present;
n = 10 positive, n = 14 negative, n = 7 other videos where at least a “comment” was present;
n = 17 positive, n = 24 negative, n = 18 other videos where at least a “share” was present;
Specific vaccinations regarded MMR, flu, meningococcus, human papillomavirus, hepatitis B virus and hexavalent.
Positive videos had a shorter duration (6.7 ± 13.4 minutes) with respect to negative videos (28.6 ± 44 minutes) and “others” (21.7 ± 45.6) (p < 0.001).
In regard to ratings and views, only data regarding January 2016 are reported. The distribution of ratings and views of the first analysis (September 2015) was not different from the second analysis (January 2016) (Data not shown in table).
Positive videos were the most viewed (1602 ± 6544 views vs 1482 ± 2735 views of negative videos, p < 0.001). Otherwise, negative videos were received more ratings in terms of “likes,” both as mean and percentage, than the other ones. At the same time at least a “dislike” or a comment was more likely in negative videos compared with the others. No significant differences were noted with “dislikes” and comments means. Furthermore negative videos were more shared (23 ± 22.6) compared with positive ones (3.8 ± 5.5) and “others” (4.9 ± 6.6) both as mean and percentage (p < 0.001). All the statistical significant differences were confirmed when limiting the analysis to positive and negative videos.
The source of the videos was identified for all and those published by health professionals, i.e., health care professionals or medical centers, were 30%. Positive videos were mainly developed by health professionals (44%) as compared with other videos. “Non-health professional” sources, such as forums, news, television, individuals, anti-vaccine and other associations were characterized mainly by negative (75%) and neutral/ambiguous videos (91%) (p = 0.002).
“Non-health professional” or “consumer” videos had a higher number of average likes (15.7 ± 38.1), dislikes (2.3 ± 2.4) and comments (3.5 ± 5.4) than “health professional” videos (6.9 ± 8.3; 1.6 ± 0.9; 2.6 ± 2.0 respectively). The differences were not statistically significant (p > 0.05) (data not shown in table).
General vaccination was the topic mainly discussed by negative videos (86%), compared with positive ones (40%) and “others” (55%) (p < 0.001).
The time trend of videos selected according to the message tone is shown in Fig. 1A. Positive videos outnumbered negative ones for the entire observation period. Two spikes are evident, one in December 2014, with a total of 17 published videos, and the other one in April 2015, with a total of 13 published videos. Out of 17 videos published in December 2014, 10 were positive, 4 negative and 3 were “others.” The ratings in terms of “likes” were 30% (3 out of 10) for positive and all for negative and “others” videos. “Shares” were only 20% (2 out of 10) of positive and all in the case of other videos.
Figure 1.
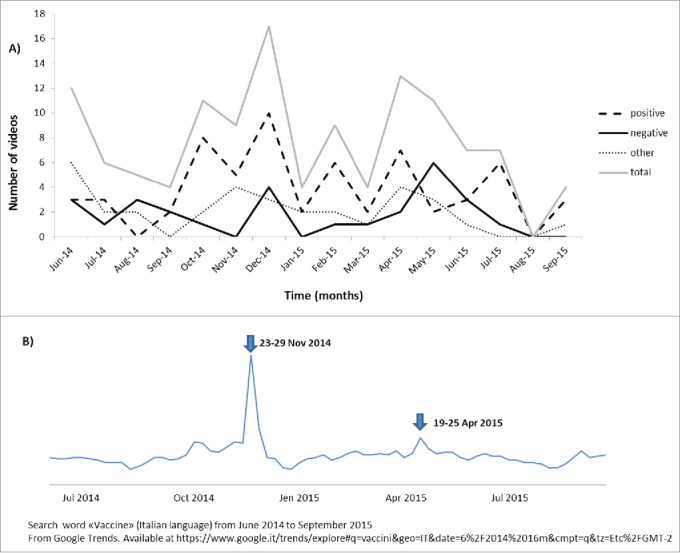
Time trend of videos selected according to the message tone (A) and corresponding Google Trend (B).
Limiting the analysis to the videos having at least some rating, it was found that the negative videos had more “likes” and more “shares” (19 ± 10 and 34.8 ± 34.8, respectively) than the positive ones (likes: 2.3 ± 2.3; shares: 4 ± 4.2). The differences were not statistically significant, both in the case of “likes” and “shares” (p > 0.05). A similar trend was found for videos published in April 2015, where 7 were positive, 2 negative and 4 were “others.” The ratings, in terms of “likes” were 29% (2 out 7) in positive videos and 100% in the other ones. ”Shares” were in 3 out of 7 positive videos, in both negative ones and 3 out of 4 “others.” Even if the difference was not statistically significant, negative videos had more “likes” (81.5 ± 112.4) than positive ones (2.5 ± 2.1) and “others” (1 ± 0). Furthermore, they had more “shares” (39.5 ± 53) than the positive (4 ± 1.7) and “others” (1.3 ± 0.6) videos. (p>0.05).
Figure 1B shows the Google Trend of the word “vaccine” over the study observation period (June 2014-September 2015). There was a big interest in “vaccines” particularly at the end of November 2014. The second greatest number of searches, although less evident, was at the end of April 2015. The 2 spikes shown in Fig. 1A seem to match to the spikes indicated in Fig. 1B.
The themes of the videos were clearly identified in 77 videos (67%). The rest of the videos provided mainly positive (72%) or neutral (22%) information. Table 2 reports the list of prevalent themes according to the message tone. “Others” includes ambiguous and neutral videos. In some videos, more than one argument was identified. Fear appeal is the theme more present in negative (29%) and ambiguous/neutral videos (30%) compared with positive ones (13%); however the difference was not statistically significant (p > 0.05). The same result was found when we collapsed the videos, in which fear appeal appeared at least one time in positive and negative videos (52% vs 71%, respectively; p>0.05). Out of 26 videos where only fear appeal occurred, 22 (85%) were produced by non-health professionals.
Table 2.
List of prevalent themes of videos according to the tone.
| Themes | Positive(N = 62) | Negative(N = 28) | Others(N = 33) |
|---|---|---|---|
| Fear appeal | 8 (13%) | 8 (29%) | 10(30%) |
| Solidarity, herd immunity | 8 (13%) | — | — |
| Economic interests | — | 2 (7%) | — |
| Parents' right of choice | — | — | 4(12%) |
| Duty to their child protection | 5 (8%) | 1 (4%) | 1(3%) |
| Fear and Solidarity | 6 (9%) | — | — |
| Fear and Economic interests | — | 10 (35%) | 1(3%) |
| Fear and Parents' right of choice | — | — | 1(3%) |
| Fear and Duty to their child protection | 1 (2%) | — | — |
| Fear and Economic interests and Parents' right of choice | — | 2 (7%) | 1(3%) |
| Solidarity and Duty to their child protection | 1 (2%) | — | — |
| Economic interests and Parents' right of choice | — | 4 (14%) | — |
| Parents' right of choice and Duty to their child protection. | — | — | — |
| Informative | 33 (53%) | 1 (4%) | 12(36%) |
Discussion
To our knowledge, this is the first study that analyzed the content of YouTube videos on general vaccination in Italy. In agreement with other studies that performed a content analysis on YouTube videos about HPV vaccination23,25 the majority of analyzed videos were favorable to vaccinations. However, negative videos were more rated in terms of number of “likes,” “dislikes,” and comments. Moreover, they were more shared and viewed than positive videos. This aspect was confirmed and particularly evident when analyzing the time trend of videos according to message tone. The time trend of selected videos showed that the month when the largest number of videos was published is the same as that shown by the Google trend for the word “vaccine,” i.e., December 2014, meaning that the web search on vaccines was particularly intensive during that period. In that period there was a large debate about the safety of Fluad flu vaccine due to some deaths in the elderly population that was vaccinated.28 In the same way, the other spike, even less evident, pertains to April 2015, during World Immunization Week 2015 (24–30 April). Although it is not possible to attribute with certainty web searches to a specific event, it is worth noting that despite the fact that positive videos outnumbered negative ones in both periods, the negative videos were significantly more liked and shared than all the other ones.
A higher number of likes for negative videos than positive ones could mean the probability of a lay user paying more attention to such videos. Furthermore, it seems that these videos generate more debate. These findings are consistent with previous studies.22-26 As underlined by Keelan and colleagues,22 this suggests the presence of an active community of YouTube users critical of vaccinations. In this regard, the high probability should be considered to be negatively influenced if exposed to misinformation about vaccination. A recent research focused on tweets about HPV vaccination showed that the likelihood of a user posting a negative tweet after exposure to negative opinions was significantly higher than for users exposed to positive and neutral tweets.29
Negative videos were also significantly longer than positive ones and they dealt mainly with general rather than specific vaccinations. This could mean that anti-vaccination videos need more time to be argued and the idea of risk is related to vaccination in general. It can be assumed that the more information is given the less likely people are to process it. However 2013 data30 showed that more than a third of all viewing time on YouTube can be attributed to videos that are 20 minutes or longer. The increase in viewing time on YouTube has accelerated, and for a period of 3 consecutive years, recorded a minimum annual increase of 50% since 2014.20
Interestingly, content analysis revealed that the argument mostly present both in positive (52%) and negative (71%) videos was fear appeal, related to the side effects or toxicity of adjuvants in vaccines on one hand and fear of the possible negative consequences of a natural communicable disease on the other hand. Fear appeal to persuade people about health behaviors is a controversial issue. A large meta-analysis showed that fear appeal was effective in influencing attitudes, intentions and behaviors in different health communication contexts.31 However, a recent randomized trial32 showed that different interventions, some based on narrative and images of dramatic consequences of measles on children, did not increase parental intent to vaccinate a child in the future. Another study33 showed that both disease risk awareness and autism correction interventions improved the intention to vaccinate, particularly among fence-sitters and this fact should be considered as a communication strategy for that large group of people who are neither for nor against vaccination, because they may be more responsive to interventions.34,35 As highlighted by Bester,36 beyond coercive approaches and increased education, it is crucial to create a trusting relationship with a healthcare provider responsible for providing clear information about vaccination risks and benefits. This “ideal” situation can be threatened by the web, which allows people to search for health information while bypassing health care professional. It is a sort of “digital disintermediation,” a term used in the e-commerce field and underscored by a recent Italian report,12 which means the possibility to buy goods and services directly from producers via the internet, thus bringing economic advantages. An important aspect pointed out by the report is that beyond an economic advantage, Italians who use internet to get information, are convinced that there are benefits in terms of information in general. If there is no doubt with regard to the economic advantage, one wonders if there is a real benefit in terms of correct information and acquiring a correct behavior.
Considering the increasing use of social media, it would be worth to further investigate how this tool can be used to promote vaccination. It should be also considered that young people are shown to be more sensitive to immunization promotion messages received through social media.37 Currently there is insufficient evidence yet on the use of web 2.0 tools as regards increasing immunization coverage rates, unlike other tools such as text messaging, immunization campaign websites, patient-held web portals and computerized reminders for which this has been demonstrated.38 So, these findings encourage putting more effort into implementing interventions that include new healthcare communication web tools.
Some limitations of the study should be underlined. First, information quality evaluation was not performed. However, it might not be influential, considering that in general the lay user does not have the tools to understand the accuracy of online information.39 Secondly, the use of only one keyword could be considered too generic, however this choice allowed the identification of a different set of videos. Third, the results were sorted by upload date and not by ranking, but as underlined by others,24 it is reasonable to think that people who want to get information about vaccines searched for the most updated videos. Moreover, the limitation of the research to the first 200 videos could have led to the loss of other eligible videos. However this web search was performed assuming to be a lay user and it was shown that users tend not to browse beyond the first result pages.40
Finally, it should be noted that the YouTube content may shift over time because many videos were uploaded every minute and it's difficult to understand the dynamics that influence videos ratings. For these reasons the results may not be generalized and should be interpreted with caution. However, the main findings of this study are similar to other studies performed in this field.23-26 This fact makes less significant the exclusion of non-Italian language videos which could have provided another perspective on the issue. Therefore, it is possible to conclude that the matter under consideration is not only an Italian problem.
In fact, vaccine hesitancy is a global phenomenon.41 It is now a unanimous opinion that health communication involving different actors such us health institutions, health professionals, scientific societies28,42-44 should be invested in.
It should be noted that in our research only 30% of videos were produced by health professionals. In the same way, considering the communication about vaccinations on Italian websites, it was shown that only 15% of websites were institutional and the use of web 2.0 tools that allow an interaction with consumers was absent.45
In a perspective of communication advocacy actions, public health institutions and scientific societies should not only be more present on the web exploiting new web channels,46 but they need to become skilled “influencers”47 which means to capture a significant amount of attention in social media conversation so as to disseminate more effectively accurate and credible information regarding vaccination at the individual, community and society level.48 In agreement with Ward and colleagues49 future research should also focus more on the actors who publish vaccine critical contents and the strategies they use to mobilize the population.
In conclusion, different vaccination policies and communication strategies as well may contribute to increase uncertainty, making people more vulnerable to misinformation running through the web. New media platforms including YouTube, have the potential to reach a wide and diverse audience. In the light of the fact that the number of videos on vaccination is high and the number of viewers is growing, it is important to monitor the web to understand audience characteristics, what and who influences public opinions and in which way; in other terms, to understand the dynamics of vaccine criticism so as to design and use more effective dissemination strategies.45,49
Materials and methods
The keyword “vaccinations” was searched in Italian on YouTube (www.youtube.com) on September, 30 2015. The search results were sorted by posting date and we decided to analyze the most recent ones (posted between June 2014 and September 2015). The research was limited to the first 200 videos sorted by posting date and in Italian language or with Italian subtitles that dealt with vaccination in children. Videos that were duplicated or were not active were excluded. The selection of videos was limited to childhood immunization, considering that the obligation regards only vaccinations for children and the online debates focus mainly on them. The videos selected were analyzed for a second time in January 2016 to check for their presence online. In particular, we characterized videos according to title, posting date, number of days since upload, author/source type, clip length, number of views, comments, number of “likes” and “dislikes,” topic and message tone.
The source represents the person or organization that produced the video and was classified into 2 categories: “health professionals,” including health care professionals or medical centers and “non-health professionals,” including television, anti-vaccination movements, governmental agencies, user generated content (a lay person's opinion about the issue) and other associations (videos that don't belong to any other category).
The videos were categorized according to tone, adopting a classification already used in other studies.22,24 In particular, the videos were classified as “positive” if vaccination was clearly recommended, “negative” if arguments were against immunization, “ambiguous” if they contained both approving and disapproving information about immunization, therefore not clear, and as “neutral” if there weren't statements of either approval or disapproval. Ambiguous and neutral videos were analyzed together.
A thematic analysis was conducted followed established steps commonly used to analyze qualitative data.50 Themes were developed mainly through an inductive method characterized by an absence of pre-existing coding frame.51 The key elements that were relevant to the area of research were identified and those with similar content were subsequently grouped and organized under analytical categories. The main themes identified were: “fear appeal,” which can be considered in both positive and negative terms e.g. – you need to vaccinate because the diseases will occur again – in positive videos or –don't vaccinate because the vaccine causes to autism- in negative ones; “solidarity, herd immunity” i.e., the appeal to the health at community level; “economic interest” i.e., the appeal to pharmaceutical industry profit; “parents' right of choice” and “duty to their child protection” i.e., duty to protect children from a disease through the prevention but also duty to protect them from possible damage caused by vaccination; “informative” when the videos provided only information about vaccination.
The videos selected were categorized and analyzed independently by 2 coders (C.P. and M.B.). The agreement on classification of videos reached the 95% and discordance were solved by a third party coder (U.G.).
Data analysis
Continuous variables were summarized as means' of standard deviation (SD) and categorical variables as frequency and percentage. Comparisons between groups were made by using the the χ2 test or Fisher's exact probability test for categorical data and Student t-test or the Mann–Whitney U-test for comparison of 2 continuous variables. To perform multiple-comparison analysis-of-variance (ANOVA) model or Kruskal-Wallis rank test were used. Two-sided P-values < 0.05 were considered statistically significant.
For the statistical analysis STATA program was used (Stata statistical software: release 12.0, College station, TX: Stata Corporation).
Supplementary Material
Abbreviations
- HPV
human papilloma virus
- MMR
measles-mumps-rubella
- NVP
National Vaccination Plan
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- [1].Moran NE, Gainotti S, Petrini C. From compulsory to voluntary immunisation: Italy's National Vaccination Plan (2005–7) and the ethical and organizational challenges facing public health policy-makers across Europe. J Med Ethics 2008; 34:669-74; https://doi.org/ 10.1136/jme.2007.022343 [DOI] [PubMed] [Google Scholar]
- [2].Pelullo CP, Marino S, Valdes Abuadili AJ, Signoriello G, Attena F. Is it reasonable to abandon obligatory vaccinations in Italy? a 2013 survey. Euro Surveill 2014; 19(35):20889; PMID:25210983; https://doi.org/ 10.2807/1560-7917.ES2014.19.35.20889 [DOI] [PubMed] [Google Scholar]
- [3].State-Regions Conference. National Plan for Vaccination 2005–2007 [Conferenza Stato-Regioni. Nuovo Piano Nazionale Vaccini 2005–2007. Gazzetta Ufficiale n. 86 del 14-04-2005. Supplemento ordinario n. 63]; http://www.salute.gov.it/imgs/C_17_pubblicazioni_543_allegato.pdf [accessed 2017April3] [Google Scholar]
- [4].Regione Veneto ALLEGATOA alla Dgr n. 1679 del 24 settembre 2013. Monitoraggio Della Sospensione Dell'Obbligo Vaccinale semestrale al 31/03/2013; http://bur.regione.veneto.it/BurvServices/Pubblica/Download.aspx?name=1679_AllegatoA_258386.pdf&type=9&storico=False [accessed 2016August03] [Google Scholar]
- [5].European Center for disease prevention and Control Technical Report. Review of outbreaks and barriers to MMR vaccination coverage among hard-to-reach populations in Europe. http://ecdc.europa.eu/en/publications/Publications/MMR-vaccination-hard-to-reach-population-review-2013.pdf [accessed 2016August03] [Google Scholar]
- [6].Italian Ministry of Health official website : http://www.salute.gov.it/portale/documentazione/p6_2_8_3_1.jsp?lingua=italiano&id=20 [accessed 2016August03] [Google Scholar]
- [7].Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014; 32:4860-5; PMID:24262311; https://doi.org/ 10.1016/j.vaccine.2013.11.006 [DOI] [PubMed] [Google Scholar]
- [8].Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines 2015; 14:99-117; PMID:25373435; https://doi.org/ 10.1586/14760584.2015.964212 [DOI] [PubMed] [Google Scholar]
- [9].Shrivastava SR, Shrivastava PS, Ramasamy J. The growing global problem of vaccine hesitancy: Time to take action. Int J Prev Med 2016; 7:19; https://doi.org/ 10.4103/2008-7802.173926 eCollection 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].European Commission European citizens' digital health literacy. 2014. http://ec.europa.eu/public_opinion/flash/fl_404_sum_en.pdf [accessed 2016August03] [Google Scholar]
- [11].Census Report , 2015. L'economia della disintermediazione digitale. http://www.economyup.it/upload/images/03_2015/150327114816.pdf [accessed 2016August03] [Google Scholar]
- [12].Rosselli R, Martini M, Bragazzi NL. The old and the new: vaccine hesitancy in the era of the Web 2.0. Challenges and opportunities. J Prev Med Hyg 2016; 57:E47-50; PMID:27346940 [PMC free article] [PubMed] [Google Scholar]
- [13].Stahl JP, Cohen R, Denis F, Gaudelus J, Martinot A, Lery T, Lepetit H. The impact of the web and social networks on vaccination. New challenges and opportunities offered to fight against vaccine hesitancy. Med Mal Infect 2016; 46:117-22; PMID:26987960; https://doi.org/ 10.1016/j.medmal.2016.02.002 [DOI] [PubMed] [Google Scholar]
- [14].Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012; 30:3778-89; PMID:22172504; https://doi.org/ 10.1016/j.vaccine.2011.11.112 [DOI] [PubMed] [Google Scholar]
- [15].Venkatraman A, Garg N, Kumar N. Greater freedom of speech on Web 2.0 correlates with dominance of views linking vaccines to autism. Vaccine 2015. Mar 17; 33(12):1422-5; PMID:25665960; https://doi.org/ 10.1016/j.vaccine.2015.01.078 [DOI] [PubMed] [Google Scholar]
- [16].Betsch C, Brewer NT, Brocard P, Davies P, Gaissmaier W, Haase N, Leask J, Renkewitz F, Renner B, Reyna VF, et al.. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine 2012; 30:3727-33; PMID:22365840; https://doi.org/ 10.1016/j.vaccine.2012.02.025 [DOI] [PubMed] [Google Scholar]
- [17].Witteman HO, Zikmund-Fisher BJ. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine 2012; 30:3734-40; PMID:22178516; https://doi.org/ 10.1016/j.vaccine.2011.12.039 [DOI] [PubMed] [Google Scholar]
- [18].Dannetun E, Tegnell A, Hermansson G, Giesecke J. Parents' reported reasons for avoiding MMR vaccination. A telephone survey. Scand J Prim Health Care 2005; 23:149-53; PMID:16162466 [DOI] [PubMed] [Google Scholar]
- [19].Betsch C, Renkewitz F, Betsch T, Ulshöfer C. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol 2010; 15:446-55; PMID:20348365; https://doi.org/ 10.1177/0272989X11400419 [DOI] [PubMed] [Google Scholar]
- [20].YouTube Statistics 2016. https://www.youtube.com/yt/press/it/statistics.html [accessed 2016August03]. [Google Scholar]
- [21].Madathil KC, Rivera-Rodriguez AJ, Greenstein JS, Gramopadhye AK. Healthcare information on YouTube: A systematic review. Health Informatics J 2015; 21:173-194; PMID:24670899; https://doi.org/ 10.1177/1460458213512220 [DOI] [PubMed] [Google Scholar]
- [22].Keelan J, Pavri-Garcia V, Tomlinson G, Wilson K. YouTube as a source of information on immunization: a content analysis. JAMA 2007; 298:2482-4; PMID:18056901; https://doi.org/ 10.1001/jama.298.21.2482 [DOI] [PubMed] [Google Scholar]
- [23].Ache KA, Wallace LS. Human papillomavirus vaccination coverage on YouTube. Am J Prev Med 2008; 35:389-92; PMID:18675530; https://doi.org/ 10.1016/j.amepre.2008.06.029 [DOI] [PubMed] [Google Scholar]
- [24].Briones R, Nan X, Madden K, Waks L. When vaccines Go Viral: An analysis of HPV Vaccine Coverage on YouTube. Health Communication 2012; 27:478-85; PMID:22029723; https://doi.org/ 10.1080/10410236.2011.610258 [DOI] [PubMed] [Google Scholar]
- [25].Tuells J, Martinez-Martinez PJ, Duro-Torrijos JL, Caballero P, Fraga-Freijeiro , Navarro-Lopez V. Characteristics of the Videos in Spanish Posted on YouTube about Human Papillomavirus Vaccines. Rev Esp Salud Publica 2015; 89:107-15; PMID:25946591; https://doi.org/ 10.4321/S1135-57272015000100012 [DOI] [PubMed] [Google Scholar]
- [26].Basch CH, Hillyer GC, Berdnik A, Basch CE. YouTube™ videos related to human papillomavirus: the need for professional communication. Int J Adolesc Med Health 2016; PMID:27060736; https://doi.org/ 10.1515/ijamh-2015-0122 [DOI] [PubMed] [Google Scholar]
- [27].World Health Organization (WHO) Addressing vaccine hesitancy. http://www.who.int/immunization/programmessystems/vaccine_hesitancy [accessed 2017February02] [Google Scholar]
- [28].Signorelli C, Odone A, Conversano M, Bonanni P. Deaths after Fluad flu vaccine and the epidemic of panic in Italy. BMJ 2015; 350:h116; PMID:25589037; https://doi.org/ 10.1136/bmj.h116 [DOI] [PubMed] [Google Scholar]
- [29].Dunn AG, Leask J, Zhou X, Mandl KD, Coiera E. Associations between exposure to and expression of negative opinions about human Papillomavirus Vaccines on Social Media: An observational study. J Med Internet Res 2015. Jun 10; 17:e144; PMID:26063290; https://doi.org/ 10.2196/jmir.4343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Roettgers J. More than a third of all YouTube viewing comes from longform content. 2013. https://gigaom.com/tag/statistics/page/2/[accessed 2016August03] [Google Scholar]
- [31].Tannenbaum MB, Hepler J, Zimmerman RS, Saul L, Jacobs S, Wilson K, Albarracín D. Appealing to fear: A meta-analysis of fear appeal effectiveness and theories. Psychol Bull 2015; 141:1178-204; PMID:26501228; https://doi.org/ 10.1037/a0039729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Nyhan B, Reifler J, Richey S, Freed GL. Effective messages in vaccine promotion: a randomized trial. Pediatrics 2014; 133:e835-42; https://doi.org/ 10.1542/peds.2013-2365 [DOI] [PubMed] [Google Scholar]
- [33].Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. Proc Natl Acad Sci USA 2015; 112:10321-4; https://doi.org/ 10.1073/pnas.1504019112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Leask J. Target the fence-sitters. Nature 2011; 473:443-5; PMID:21614055; https://doi.org/ 10.1038/473443a [DOI] [PubMed] [Google Scholar]
- [35].Betsch C, Korn L, Holtmann C. Don't try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci USA 2015; 112:E6725-6; PMID:26598650; https://doi.org/ 10.1073/pnas.1516350112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bester JC. Vaccine refusal and trust: The trouble with Coercion and Education and suggestions for a cure. J Bioeth Inq 2015; 12:555-9; PMID:26626065; https://doi.org/ 10.1007/s11673-015-9673-1 [DOI] [PubMed] [Google Scholar]
- [37].Mena G, Llupià A, García-Basteiro AL, Aldea M, Sequera VG, Trilla A. The willingness of medical students to use Facebook as a training channel for professional habits: the case of influenza vaccination. Cyberpsychol Behav Soc Netw 2012; 15:328-31; PMID:22703040; https://doi.org/ 10.1089/cyber.2011.0457 [DOI] [PubMed] [Google Scholar]
- [38].Odone A, Ferrari A, Spagnoli F, Visciarelli S, Shefer A, Pasquarella C, Signorelli C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage. Hum Vaccin Immunother 2015; 11:72-82; PMID:25483518; https://doi.org/ 10.4161/hv.34313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Diviani N, van den Putte B, Giani S, van Weert JC. Low health literacy and evaluation of online health information: a systematic review of the literature. Med Internet Res 2015; 17:e112; PMID:25953147; https://doi.org/ 10.2196/jmir.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Spink A, Wolfram D, Jansen MBJ, Saracevi T. Searching the web: The public and their queries journal of The American Society for information science and technology. 2001; 52:226-34; https://doi.org/ 10.1002/1097-4571(2000)9999:9999 [DOI] [Google Scholar]
- [41].Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy – country-specific characteristics of a global phenomenon. Vaccine 2014; 32:6649-54; PMID:25280436; https://doi.org/ 10.1016/j.vaccine.2014.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Haverkate M, D'Ancona F, Giambi C, Johansen K, Lopalco PL, Cozza V, Appelgren E; VENICE project gatekeepers and contact points . Mandatory and recommended vaccination in the EU, Iceland and Norway: results of the VENICE 2010 survey on the ways of implementing national vaccination programmes. Euro Surveill 2012; 17:20183. [DOI] [PubMed] [Google Scholar]
- [43].Goldstein S, MacDonald NE, Guirguis S; SAGE Working Group on Vaccine Hesitancy . Health communication and vaccine hesitancy. Vaccine 2015; 33:4212-4; https://doi.org/ 10.1016/j.vaccine.2015.04.042 [DOI] [PubMed] [Google Scholar]
- [44].Nowak GJ, Gellin BG, MacDonald NE, Butler R; SAGE Working Group on Vaccine Hesitancy . Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine 2015; 33:4204-11; PMID:25900132; https://doi.org/ 10.1016/j.vaccine.2015.04.039 [DOI] [PubMed] [Google Scholar]
- [45].Tafuri S, Gallone MS, Gallone MF, Zorico I, Aiello V, Germinario C. Communication about vaccinations in Italian websites: a quantitative analysis. Hum Vaccin Immunother 2014; 10:1416-20; PMID:24607988; https://doi.org/ 10.4161/hv.28268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Ferro A, Odone A, Siddu A, Colucci M, Anello P, Longone M, Marcon E, Castiglia P, Bonanni P, Signorelli C. Monitoring the web to support vaccine coverage: results of two years of the portal VaccinarSì. Epidemiol Prev 2015; 39:88-93; PMID:26499422 [PubMed] [Google Scholar]
- [47].Freberg K, Grahamb K, McGaugheyc K, Frebergc LA. Who are the social media influencers? A study of public perceptions of personality. Public Relations Review 2011; 37:90-2; https://doi.org/ 10.1016/j.pubrev.2010.11.001 [DOI] [Google Scholar]
- [48].Odone A, Signorelli C. What are we told? A news media monitoring model for public health and the case of vaccines. Eur J Public Health 2016; 26:533-4; PMID:27423000; https://doi.org/ 10.1093/eurpub/ckw002 [DOI] [PubMed] [Google Scholar]
- [49].Ward JK, Peretti-Watel P, Verger P. Vaccine criticism on the Internet: Propositions for future research. Hum Vaccin Immunother 2016; 12:1924-9; PMID:26900646; https://doi.org/ 10.1080/21645515.2016.1146430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000; 320:114-6; https://doi.org/ 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3:77-101; https://doi.org/ 10.1191/1478088706qp063oa [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


