ABSTRACT
Background: To obtain the baseline data on the incidence and cost of community acquired pneumonia among under-5 children for future studies, and provide evidence for shaping China's strategies regarding pneumococcal conjugate vaccine (PCV).
Methods: Three townships from Heilongjiang, Hebei and Gansu Province and one community in Shanghai were selected as study areas. A questionnaire survey was conducted to collect data on incidence and cost of pneumonia among children under 5 y old in 2012.
Results: The overall incidence of clinically diagnosed pneumonia in children under 5 y old was 2.55%. The incidence in urban area was 7.97%, higher than that in rural areas (1.68%). However, no difference was found in the incidences of chest X-ray confirmed pneumonia between urban and rural areas (1.67% vs 1.23%). X-ray confirmed cases in rural and urban areas respectively accounted for 73.45% and 20.93% of all clinically diagnosed pneumonia. The hospitalization rate of all cases was 1.40%. Incidence and hospitalization rate of pneumonia decreased with age, with the highest rates found among children younger than one year and the lowest among children aged 4 (incidence: 4.25% vs 0.83%; hospitalization: 2.75% vs 0.36%). The incidence was slightly higher among boys (2.92% vs 2.08%). The total cost due to pneumonia for the participants was 1138 733 CNY. The average cost and median cost was 5722 CNY and 3540 CNY separately. Multivariate analysis showed that the only factor related to higher cost was hospitalization.
Conclusions: The disease burden was high for children under 5 y old, especially the infant. PCV has not been widely used among children, and thus further health economics evaluation on introducing PCV into National Immunization Program should be conducted.
KEYWORDS: costs, disease burden, incidence, pneumonia
Background
Pneumonia is inflammation of the lung caused by various pathogens such as bacteria and viruses. The main clinical signs include fever, productive cough, and sputum with blood, with or without chest pain or dyspnea. Globally, pneumonia became the second cause of deaths in children under 5, and nearly one million children under 5 died from pneumonia in 2015.1 It is estimated that the global annual incidence of community acquired pneumonia (CAP) is 1–12% and the hospitalization of CAP is between 22% and 50%. Usually, the overall case fatality rate (CFR) of CAP is about 4% while the CFR for outpatients is about 1%.2-4 The CAP is more severe and leads to more mortalities in developing countries.5-7 Pneumonia is one of the largest killers of children under 5 y old in China. According to the Report on Women and Children's Health Development in China (2011), pneumonia is the second leading cause of death in under-5 children in China.8 An investigation of death causes for children under 5 y old in China in 2008 showed that pneumonia accounted for 16.5% of all the causes.9
Pneumococcal conjugate vaccine (PCV) is one of the most effective measures to prevent pneumonia. World Health Organization (WHO) recommends that the PCV should be introduced into National Immunization Program (NIP), especially in countries where the mortality of children under 5 y old is higher than 50/1000 live births. As of the end of 2013, the PCV has been introduced into NIP in 103 countries, with a global coverage of 25%. By 2007, there were 11 vaccines included in China NIP, however there are still several important vaccines which are not in NIP, but paid by parents, including PCV, Haemophilus influenza type b, Rotavirus, varicella, etc. One study conducted in 2011 showed the coverage of PCV7 was only 9.9% in children aged 1–2 in China.10 After 2015, no PCV is available in China while several PCVs are in stage of clinical trials or pre-market approval process. The introduction of PCV into NIP needs evidence base, including data on pneumococcal disease burden (pneumonia, meningitis and otitis media) and related economic burden of disease. However, the diagnosis of pneumococcal disease is difficult, so the disease burden can be estimated through the syndrome of pneumonia. Pneumonia is not a notifiable disease in China, and relevant data are absent from national monitoring data. Studies on pneumonia in China are mainly based on outpatients and inpatients records.11-12 Only one study from Hongkong investigated the population based hospitalization rate of CAP.13 There is inadequate data on community population-based incidence and cost of pneumonia in China.
Results
Incidence of pneumonia in children under 5 y old in 2012
A total of 7811 children under 5 y old were investigated, among whom 199 children had pneumonia in 2012, including 101 (accounting for 50.75%) cases confirmed by chest X-ray test. The median age of the patients was 21 months (range: 1 month to 58 months). The incidence was the highest among children less than 1 y old, and the lowest among children of 4 y old (4.40% vs 0.77%, RR = 5.70, 95% CI = 3.13–10.37). There were 127 male patients and 72 female patients, with a higher incidence rate for the male (2.92% vs 2.08%, RR = 1.40, 95% CI = 1.05–1.86). Totally, 113 pneumonia patients were found in rural areas, and 83 (73.45%) of them were confirmed by chest X-ray test. Meanwhile, 86 pneumonia cases were found in urban areas, among which 18 cases (20.93%) were chest X-ray confirmed pneumonia. Incidence of all cause pneumonia was higher in urban areas (7.97% vs 1.68%, RR = 4.75, 95% CI = 3.61–6.24), however, the incidence of X-ray confirmed pneumonia was not statistically different between rural and urban areas (Table 1).
Table 1.
Incidence rate of pneumonia in children under 5 y old in 2012.
| Population size | Cases in 2012 | Incidence rate (%) | RR | 95% CI | |
|---|---|---|---|---|---|
| Onset age | |||||
| 0- | 1272 | 56 | 4.40 | 5.70 | 3.13–10.37 |
| 1- | 1604 | 57 | 3.55 | 4.60 | 2.53–8.37 |
| 2- | 1630 | 39 | 2.39 | 3.10 | 1.66–5.78 |
| 3- | 1622 | 34 | 2.10 | 2.71 | 1.44–5.12 |
| 4- | 1683 | 13 | 0.77 | REF | — |
| Gender | |||||
| Male | 4355 | 127 | 2.92 | 1.40 | 1.05–1.86 |
| Female | 3456 | 72 | 2.08 | REF | — |
| Residency type | |||||
| Urban | 1079 | 86 | 7.97 | 4.75 | 3.61–6.24 |
| Rural | 6732 | 113 | 1.68 | REF | — |
| X-ray confirmed pneumonia | |||||
| Urban | 1079 | 18 | 1.67 | 1.35 | 0.82–2.24 |
| Rural | 6732 | 83 | 1.23 | REF | — |
| Total | 7811 | 199 | 2.55 | ||
Pneumococcal vaccination history before onset
Of the 199 pneumonia cases, 25 patients (12.56%) were vaccinated with pneumococcal vaccines before the onset of pneumonia, 159 were not vaccinated, and 15 were unknown vaccine history. Among the 25 vaccinated patients, 2 of them (1.77%) were from rural areas and the source of information was guardians' memory; and the other 23 patients (26.74%) were from urban areas and the source of information was as follows: guardians' memory: 3 cases; vaccination certificate: 5; vaccination card: 2; and vaccination data: 13.
The number of pneumonia cases with a pneumococcal vaccination history for children aged 0 to 4 y was 1, 2, 9, 11, and 2 respectively, accounting for 1.79%, 3.51%, 23.08%, 32.35% and 15.38% of all cases in each age group. Among chest X-ray confirmed pneumonia, 7 patients (6.93%) received pneumococcal vaccine before; while in clinical diagnosed pneumonia, 18 patients (18.37%) were vaccinated.
Vaccine types and doses: In total, 20 cases received only 1 dose of 23-valent polysaccharide vaccine, 5 cases received 2 doses of 7-valent PCV (Table 2).
Table 2.
Pneumococcal vaccination of subjects before onset.
| Patients with vaccination history |
||||||
|---|---|---|---|---|---|---|
| 1 dose PPSV | 2 doses PCV7 | Subtotal | 0 dose | unknown | Total | |
| Onset age(year) | ||||||
| 0 | 1 | 0 | 1 | 53 | 2 | 56 |
| 1 | 1 | 1 | 2 | 52 | 3 | 57 |
| 2 | 7 | 2 | 9 | 24 | 6 | 39 |
| 3 | 9 | 2 | 11 | 20 | 3 | 34 |
| 4 | 2 | 0 | 2 | 10 | 1 | 13 |
| Resident type | ||||||
| Urban | 18 | 5 | 23 | 63 | 0 | 86 |
| Rural | 2 | 0 | 2 | 96 | 15 | 113 |
| Gender | ||||||
| Male | 14 | 4 | 18 | 100 | 9 | 127 |
| Female | 6 | 1 | 7 | 59 | 6 | 72 |
| X-ray confirmed pneumonia | ||||||
| Yes | 7 | 0 | 7 | 87 | 7 | 101 |
| No | 13 | 5 | 18 | 72 | 8 | 98 |
| Total | 20 | 5 | 25 | 159 | 15 | 199 |
Hospitalization due to pneumonia
For the 199 pneumonia cases, bronchial pneumonia was the most common type (159), followed by lobar pneumonia (4) and interstitial pneumonia (2). The diagnosis was not clear for 34 cases. Most of the cases were found in winter and least in summer (Fig. 1).
Figure 1.
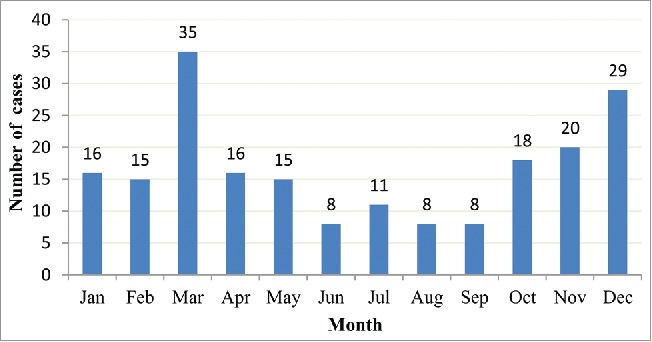
Distribution of pneumonia by month in 2012.
The number of outpatient visit was more than twice (74.42%) for the majority of cases in urban areas and less than one time (73.45%) in the rural areas. The hospital for the first visit was mainly municipal hospital in urban areas and village or township clinics and private clinics in rural areas (Table 3). The hospitalization rate of children under 5 y old due to pneumonia was 1.40%, and decreased with age. There was no statistical difference in the hospitalization rate of pneumonia between urban and rural areas (Table 4). Among the 109 hospitalized cases, 80 ones were chest X-ray confirmed pneumonia. The hospitalization rate for pneumonia was 54.77% and 79.21% for X-ray confirmed pneumonia. The proportion of hospitalization in urban areas was lower than that in rural areas; and those with pneumococcal vaccine history were less likely to be hospitalized than those without the history (Table 5). The average length of hospital stay was 9.75 days, with a median of 7 d (interquartile range: 7–11 days; range: 1 to 50 days). The average disease duration was 13.57 days, with a median of 11 d (interquartile range: 8–15 days, range: 3 to 70 days).
Table 3.
Outpatient visit due to pneumonia in the study areas in 2012.
| Urban areas |
Rural areas |
Total |
||||
|---|---|---|---|---|---|---|
| Case No. | Proportion | Case No. | Proportion | Case No. | Proportion | |
| No. of outpatient service | ||||||
| 0 | 0 | 0.00 | 28 | 24.78 | 28 | 14.07 |
| 1 | 22 | 25.58 | 55 | 48.67 | 77 | 38.69 |
| 2 | 36 | 41.86 | 19 | 16.81 | 55 | 27.64 |
| ≥ 3 | 28 | 32.56 | 11 | 9.73 | 39 | 19.60 |
| Hospital grade for the 1st visit | ||||||
| Not reported | 3 | 3.49 | 28 | 24.78 | 31 | 15.58 |
| Municipal | 77 | 89.53 | 2 | 1.77 | 79 | 39.70 |
| County | 6 | 6.98 | 14 | 12.39 | 20 | 10.05 |
| Township or village | 0 | 0.00 | 34 | 30.09 | 34 | 17.08 |
| Private clinic | 0 | 0.00 | 35 | 30.97 | 35 | 17.59 |
| Total | 86 | 100.00 | 113 | 100.00 | 199 | 100.00 |
Table 4.
Hospitalization rate of children under 5 y old due to pneumonia in the study areas in 2012.
| Population size | Hospitalized cases | Hospitalization rate (%) | χ2 | P | |
|---|---|---|---|---|---|
| Onset age | |||||
| 0- | 1272 | 35 | 2.75 | 37.74a | < 0.0001 |
| 1- | 1604 | 33 | 2.06 | ||
| 2- | 1630 | 18 | 1.10 | ||
| 3- | 1622 | 17 | 1.05 | ||
| 4- | 1683 | 6 | 0.36 | ||
| Gender | |||||
| Male | 4355 | 68 | 1.56 | 1.97 | 0.1604 |
| Female | 3456 | 41 | 1.19 | ||
| Residency type | |||||
| Urban | 1079 | 16 | 1.48 | 0.07 | 0.7921 |
| Rural | 6732 | 93 | 1.38 | ||
| Total | 7811 | 109 | 1.40 | ||
Note: a: trend Chi square value.
Table 5.
Hospitalization proportion of pneumonia patients in 2012.
| No. of cases | Hospitalized cases | Hospitalization proportion (%) | χ2 | P | |
|---|---|---|---|---|---|
| Onset age | |||||
| 0- | 56 | 35 | 62.50 | 3.44 | 0.4861 |
| 1- | 57 | 33 | 57.89 | ||
| 2- | 39 | 18 | 46.15 | ||
| 3- | 34 | 17 | 50.00 | ||
| 4- | 13 | 6 | 46.15 | ||
| Gender | |||||
| Male | 127 | 68 | 53.54 | 0.21 | 0.6432 |
| Female | 72 | 41 | 56.94 | ||
| Residency type | |||||
| Urban | 86 | 16 | 18.60 | 79.98 | < 0.0001 |
| Rural | 113 | 93 | 82.30 | ||
| Chest X-ray confirmed pneumonia | |||||
| Urban | 18 | 3 | 16.67 | 43.96 | < 0.0001 |
| Rural | 83 | 77 | 92.77 | ||
| Vaccine history before onset | |||||
| Yes | 25 | 3 | 12.00 | 21.12 | < 0.0001 |
| No | 159 | 97 | 61.01 | ||
| Unknown | 15 | 9 | 60.00 | ||
| Total | 199 | 109 | 54.77 | ||
The cost of pneumonia
The total cost due to pneumonia for the 199 subjects were 1138733 CNY, with an average of 5722 CNY and a median of 3540 CNY (interquartile range: 2230–5460 CNY). The detail on the cost is presented in Table 6. Univariate analysis was performed after log conversion, showing that factors related to cost included residency type, whether hospitalized, whether Chest X-ray confirmed and prior vaccines in urban areas (Table 7). Further multivariate linear regression analysis showed that the only factor associated with cost was whether hospitalized (Table 8).
Table 6.
Cost due to pneumonia in children under 5 y old (CNY).
| Number | Total Cost | Average | Median | 25% Percentile | 75% percentile | Maximum | minimum | |
|---|---|---|---|---|---|---|---|---|
| Outpatient cost | 171b | 146193 | 855 | 500 | 210 | 1050 | 10000 | 12 |
| Hospitalization cost | 109 | 476852 | 4375 | 2000 | 1443 | 3000 | 50000 | 322 |
| OTC drug | 195c | 23640 | 121 | 0 | 0 | 100 | 3800 | 0 |
| Transportation | 199 | 45887 | 231 | 150 | 90 | 260 | 2000 | 0 |
| Other related costs | 197d | 68508 | 348 | 200 | 20 | 500 | 3000 | 0 |
| Productivity lose | 198e | 377653 | 1907 | 1200 | 680 | 1900 | 23400 | 0 |
| Total cost | 199 | 1138733 | 5722 | 3540 | 2230 | 5460 | 56167 | 920 |
Note: b: 28 patients were directly admitted to hospital without the outpatient service;
c: the cost of OTC drug was not reported for 4 cases;
d: other costs associated with the disease was not reported for 2 cases;
e: the income of care givers was not provided for 1 case.
Table 7.
Influencing factors on cost: univariate analysis.
| Number | Total Cost | Average | Median | Log mean | F or t | P | |
|---|---|---|---|---|---|---|---|
| Onset age | |||||||
| 0- | 56 | 307041 | 5483 | 3900 | 4107 | 1.89 | 0.1707 |
| 1- | 57 | 341897 | 5998 | 4024 | 4138 | ||
| 2- | 39 | 228066 | 5848 | 2900 | 3513 | ||
| 3- | 34 | 209228 | 6154 | 3050 | 3413 | ||
| 4- | 13 | 52501 | 4039 | 3514 | 3445 | ||
| Gender | |||||||
| Male | 127 | 696072 | 5481 | 3514 | 3802 | −0.29 | 0.7744 |
| Female | 72 | 442661 | 6148 | 3662 | 3891 | ||
| Residency type | |||||||
| Urban | 86 | 345444 | 4017 | 2380 | 2818 | −5.20 | < 0.0001 |
| Rural | 113 | 793289 | 7020 | 4250 | 4898 | ||
| Whether hospitalized | |||||||
| Yes | 109 | 808455 | 7417 | 4270 | 5129 | 6.28 | < 0.0001 |
| No | 90 | 330278 | 3670 | 23220 | 2692 | ||
| Whether Chest X-ray confirmed pneumonia | |||||||
| Yes | 101 | 599841 | 5939 | 4150 | 4537 | −3.15 | 0.0019 |
| No | 98 | 538892 | 5499 | 2698 | 3205 | ||
| Prior vaccines in urban areas | |||||||
| 0 doses | 63 | 271136 | 4304 | 2610 | 3049 | 4.28 | 0.0416 |
| 1 dose | 18 | 65718 | 3651 | 2040 | 2362 | ||
| 2 doses | 5 | 8591 | 1718 | 1600 | 1652 | ||
| Prior vaccines in rural areas | |||||||
| 0 doses | 96 | 598923 | 6239 | 4257 | 4703 | 1.47 | 0.2275 |
| 1 dose | 2 | 9780 | 4890 | 4890 | 4543 | ||
| Unknown | 15 | 184586 | 12306 | 4233 | 6048 | ||
| Diagnosis | |||||||
| Lobar pneumonia | 4 | 22371 | 5593 | 3637 | 4677 | 3.42 | 0.0661 |
| Bronchial pneumonia | 159 | 941135 | 5919 | 3587 | 3981 | ||
| Interstitial pneumonia | 2 | 28100 | 14050 | 14050 | 10000 | ||
| Unknown | 29 | 127234 | 4387 | 2584 | 2884 | ||
Table 8.
Influencing factors on cost: multivariate linear regression analysis.
| Variable | Parameter estimates | Standard error | t | P |
|---|---|---|---|---|
| Whether hospitalized | −0.25267 | 0.04839 | −5.22 | < 0.0001 |
| Prior doses of pneumococcal vaccines | −0.1122 | 0.05758 | −1.95 | 0.0528 |
F = 21.17, P < 0.0001.R2 = 0.1815, Adj-R2 = 0.1729.
Discussion
This study is a community population based retrospective survey to find out the disease burden of pneumonia in children under 5 y old. The incidence rate of pneumonia in children under 5 y old was 7.97% in urban areas, which was similar to the incidence of clinical pneumonia reported in children under 4 y old in Columbia (6.28%) and Brazil (9.60%). Meanwhile, the incidence rate in rural areas was 1.68%, similar to the incidence of X-ray confirmed pneumonia in Columbia (2.12%) and Brazil (3.43%)14-15 and incidence of all cause pneumonia in children under 5 y old in Columbia (1.18%).16 Incidence of pneumonia in rural areas and urban areas were both higher than that reported in Latin America and the Caribbean (0.92%).17 The incidence of pneumonia decreased with age, with the highest rate in 0 y old and the lowest rate in 4 y old. The pneumonia was more common in boys, consistent with the results reported by Felix Gutierrez.18 The incidence was high in winter and spring, consistent with the results in Australia (the highest rate in spring [34%], followed by that in winter [26%]).19
The hospitalization rate due to pneumonia in children under 5 y old was 1.40%, which was higher than that in Hongkong (0.78%).13 This study showed that the hospitalization rate decreased with age, with the highest rate in 0 y old and the lowest in 4 y old. There was no statistical difference regarding hospitalization rates between male and female in both rural and urban areas. The proportion of hospitalized patients with pneumonia under 5 y old in urban areas was 18.60% and 82.30% in rural areas. The figure in rural areas was much higher than that in Latin American (25%).17 The incidence rate of pneumonia in urban areas was higher than that in rural areas, while the hospitalization rate due to pneumonia was lower than that in rural areas. Number of outpatient visits in urban areas was higher than that in rural areas, and the grade of hospitals was also higher. Therefore, it is estimated that some mild cases did not seek medical service or seek medical service at lower grade hospital, leading to mis-diagnosis in rural areas because of traffic inconvenience, limited medical resources, low economic development, etc. This may explain why the incidence was lower but hospitalization rate was higher in rural areas. In addition, this study showed that the coverage of pneumococcal vaccines was low (1.77% in rural areas, 26.74% in urban areas, 12.56% on average), which cannot induce the herd immunity. However, the proportion of hospitalization in patients with prior pneumococcal vaccination was lower, and the cost of pneumonia in the urban areas was lower for those with prior pneumococcal vaccination compared with those without. This is consistent with a study reporting that the cost of inpatients due to PCV7 serotype pneumonia was lower for those with at least 1 dose of PCV7 than those without it.20 The cost due to pneumonia of patients with prior pneumococcal vaccination in rural areas did not decrease, possibly because the coverage was very low (1.77%).
The average cost of pneumonia was 5722 CNY, with a median of 3540 CNY. The average cost due to outpatient was 855 CNY, with a median of 500 CNY. The average cost due to hospitalization was 4375 CNY, with a median of 2000 CNY. Median length of stay was 7 d. The results on length of hospital stay and cost were consistent with the data in China's Health and Family Planning Statistics Yearbook 2013 (length of stay in hospital: 7.2 d for bronchial pneumonia, 10 d for bacterial pneumonia; average cost: 2219 CNY for bronchial pneumonia hospitalizations, 5080.8 CNY for bacterial pneumonia hospitalization).21 The Cost due to productivity loss (average: 1907 CNY, median: 1200 CNY) was the highest among other costs, and only second to the hospitalization costs. Costs for inpatient cases were higher than outpatients.
According to the sixth census data in 2010 in China,22 there were a total of 75.5326 million children under 5 y old, with 44.5961 million in rural areas and 30.9365 million in urban areas. It is estimated that there will be a total of 3.2149 million children under 5 y old who developed pneumonia in 2012 based on incidence found by this study. Based on the cost in rural areas and urban areas caused by pneumonia in this study, the total cost due to pneumonia was 15.164 billion CNY annually.
A China and Finland cooperative study23 recruited 102 pediatric pneumonia patients in Beijing and 54 ones in Hefei, among whom 12 (12%) and 9 (17%) were pneumococcal positive respectively. According to estimates by WHO,24 8% of the clinical pneumonia cases were caused by pneumococcus, 36% of chest X-ray confirmed pneumonia cases caused by pneumococcus globally. This study found that 83 (73.45%) were chest X-ray confirmed pneumonia in rural areas, and 18 (20.93%) in urban areas. It is estimated that there are 706.5 thousands pneumococcal pneumonia in children under 5 y old in China, among which 227.9 thousand were in rural areas and 478.6 in urban areas with an assumption that 15% of clinical pneumonia cases were caused by pneumococcus and 36% of chest X-ray confirmed pneumonia cases were caused by pneumococcus. According to a review on the serotype distribution among invasive pneumococcal infections in children under 5 y old in China between 2005 and 2013, the 7-valent PCV covered about 60.2% and 13-valent PCV about 87.7%.25 It can be projected that using PCV7 will prevent 425.3 thousands pneumococcal pneumonia cases and save 2.12 billion CNY annually; and vaccination of PCV13 will cut down 619.6 thousand cases and save 3.089 billion CNY, without taking into account the PCV vaccination cost, other disease caused by pneumococcus, and indirect protection by the vaccines. This study found that the coverage of PCV was not high, reflecting the fact that the vaccine has not been widely used in the community. Further economic assessment with regard to including PCV into NIP should be conducted to promote the use of PCV to reduce the disease burden caused by pneumococcus.
Limitations of this study include: 1) The results are subject to recall bias. The cost of outpatient and hospitalization was reliably obtained through the reimbursement record of NRCMS and URBMI or receipts, but other costs were obtained by guardian' report and receipts, which may influence the accuracy of the information; 2) Death and case fatality could not be obtained due to the retrospective property; 3) Random sample was not taken in this study and subjects were children under 5 y old, therefore the results was only a representative for the children under 5 y old in study areas and cannot be accurately extrapolated to other regions.
Meanings of this study include: 1) Although this study has some limitations, the selected study sites are from the eastern, central and western provinces of China, including urban and rural areas, therefore the results are able to reflect the burden of pneumonia to a certain extent in children under 5 y old in China, and provide reference for future studies. 2) At present, there are limited data on disease burden of pneumonia under 5 y old in China, and most data are acquired by studies based on hospitals or systematic review.11-12,26-27 Only one study from Hongkong investigated the population based hospitalization rate of CAP.13 There is inadequate data on community population-based incidence and cost of pneumonia in China. This study can provide disease burden based on population which would supplement the limited data.
Conclusion
The disease burden of pneumonia was high for children under 5 y old, especially the infant. And PCV has not been widely used among children in China. This paper provided important evidence to know the disease burden of pneumonia in China before introducing PCV into NIP and basic data for further health economics evaluation on introducing PCV into NIP.
Method
Study areas and participants
Considering China's geographical characteristics, one township in each of Heilongjiang, Hebei and Gansu Province was chosen as rural representative (rural areas) and one community in Shanghai as urban representative (urban areas). The retrospective study in 4 areas was performed and participants were children who were born between January 1, 2008 and December 31, 2012 and developed pneumonia (clinical diagnosis) in 2012.
Data collection and calculation of the incidence rate
Demography information for children under 5 y old: The demographic information of children under 5 y old in 2012 was from the citizenship registration data in community (or village) or data from local institution in charge of children vaccination.
Case searching: Based on data from local vaccination institution, a screening for all children under 5 y old living in the study areas was conducted via asking the question “whether or not the child has developed pneumonia in 2012.” Information for all pneumonia cases in 2012 was collected and verified, and then all cases were investigated through face to face interview by trained investigators.
Case verification: For children reported pneumonia in 2012, their outpatient or inpatient records, and/or diagnostic imaging data such as CSR, etc were checked to verify pneumonia cases.
Calculation of the incidence rate
Data collection method and contents
The face to face interview using a uniformed questionnaire was conducted to collect data on basic demographic information, clinical manifestations, pneumococcal vaccination history, treatment and cost.
Basic demographic information: This part included gender, date of birth, and type of residence. The information was provided by the guardian.
Clinical manifestations: This part included the date of onset, the date of treatment, fever or not, cough or not, shortness of breath or not, difficulty in breathing or not, auscultation of the chest and chest X-ray results, white cell counts. The information was obtained through review of the outpatient and/or inpatient records or health care insurance records.
Pneumococcal vaccination history: The vaccination history included doses, vaccination date, types of vaccine and source of vaccination information. The information was obtained by checking vaccination certificate, vaccination card or data in vaccination institutions. If no vaccine information were available through the 3 approaches while the guardian was totally sure that the child was vaccinated, then the status was recorded as vaccinated.
Treatment: Treatment information included the total number of outpatient visit, the hospital type of the first 3 visits, the course and the outcome of pneumonia, and the hospital type of each hospitalization for the first 3 times, the length of stay if the child was hospitalized.
Cost: Cost information included: 1) outpatient expenses; 2) hospitalization expenses; and 3) other expenses which included the cost of Over-The-Counter (OTC) drug, transportation cost for medical service, productivity loss (caring for the patient), and other costs considered to be associated with the disease. Other expenses were obtained by the receipts and/or the memory of care giver, while outpatient and inpatient expenses were obtained through receipts provided by guardians and review of reimbursement records of the New Rural Cooperative Medical Scheme (NRCMS) (covering more than 90% of the rural population) or Urban Residents' Basic Medical Insurance (URBMI) (covering more than 90% of urban residents).
Definitions of various pneumonia
Lobar pneumonia is a form of pneumonia that affects a large and continuous area of the lobe of a lung.
Bronchial pneumonia, also known as bronchopneumonia, is an infection of the respiratory system that affects the bronchial tubes with patches on one or both lungs.
Interstitial pneumonia is a form of lung disease characterized by progressive scarring of both lungs. The scarring (fibrosis) involves the supporting framework (interstitium) of the lung.
Statistical analysis
EPI data3.1 was used to establish database, and double data entry was taken to ensure the accuracy of data input. Statistical product and service solution (SPSS 17.0) was used for statistical analysis. Chi square test was used to test for qualitative data with relative risk (RR) and 95% confidence intervals (95% CI); and variance analysis, t-test and multiple linear regression were used for the quantitative data. The first type error level was set to be 0.05.
Declarations
Ethics approval and consent to participate
The protocol was approved by the Ethics Review Committee of Chinese Center for Disease Control and Prevention (the approval number: 201314). The legal guardians of all the children signed the informed consent before their children were recruited in the survey.
Availability of data and material
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplementary Material
Abbreviations
- CAP
community acquired pneumonia
- CFR
case fatality rate
- CI
confidence intervals
- NRCMS
the New Rural Cooperative Medical Scheme
- OTC
Over-The-Counter
- PCV
Pneumococcal conjugate vaccine
- RR
relative risk
- URBMI
Urban Residents' Basic Medical Insurance
- WHO
World Health Organization
Disclosure of potential conflicts of interest
The authors declare that they have no competing interests.
Acknowledgments
We gratefully appreciated the efforts of the health workers from Huangpu CDC, Qinan CDC, Fujin CDC, Wuan CDC and their affiliated community health service centers or township hospitals who have participated in the field investigation.
Funding
The article was funded by China 12th five-year national science and technology major projects (2012ZX10004703).
References
- [1].Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable development goals. Lancet 2016; 388:3027-35; PMID:27839855; https://doi.org/ 10.1016/S0140-6736(16)31593-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Campbell GD. Overview of community-acquired pneumonia. Prognosis and clinical features. Med Clin N Am 1994; 78:1035-48; PMID:8078367; https://doi.org/ 10.1016/S0025-7125(16)30118-3 [DOI] [PubMed] [Google Scholar]
- [3].Foy HM, Cooney MK, Allan I, Kenny GE. Rates of pneumonia during influenza epidemics in Seattle, 1964 to 1975. JAMA 1979; 241:253-8; PMID:758528; https://doi.org/ 10.1001/jama.1979.03290290021018 [DOI] [PubMed] [Google Scholar]
- [4].Marrie TJ. Community-acquired pneumonia. Clin Infect Dis 1994; 18:501-5; PMID:8038304; https://doi.org/ 10.1093/clinids/18.4.501 [DOI] [PubMed] [Google Scholar]
- [5].Niederman MS, Bass JB Jr, Campbell GD, Fein AM, Grossman RF, Mandell LA, Marrie TJ, Sarosi GA, Torres A, Yu VL. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am Rev Respir Dis 1993; 148:1418-26; PMID:8239186; https://doi.org/ 10.1164/ajrccm/148.5.1418 [DOI] [PubMed] [Google Scholar]
- [6].Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis 2002; 2:25-32; PMID:11892493; https://doi.org/ 10.1016/S1473-3099(01)00170-0 [DOI] [PubMed] [Google Scholar]
- [7].World Health, Organization Pneumococcal vaccines. WHO position paper. Wkly Epidemiol Rec 1999; 74:177-83; PMID:10437429 [PubMed] [Google Scholar]
- [8].Ministry of Health, People's Republic of China Report on the development of women and children health in China(2011). [Google Scholar]
- [9].Rudan I, Chan KY, Zhang JS, Theodoratou E, Feng XL, Salomon JA, Lawn JE, Cousens S, Black RE, Guo Y, et al.. Causes of deaths in children younger than 5 years in China in 2008. Lancet 2010; 375:1083-89; PMID:20346815; https://doi.org/ 10.1016/S0140-6736(10)60060-8 [DOI] [PubMed] [Google Scholar]
- [10].jing-shan Zheng, lei Cao, shi-cheng Guo, et al.. Survey on the immunization Status of Category B Vaccine among Children aged 1 to 2 years in China. Chinese J Vaccines Immunization 2012; 18(3):233-7. [Google Scholar]
- [11].Zhang Y, Yao Z, Zhan S, Yang Z, Wei D, Zhang J, Li J, Kyaw MH. Disease burden of intensive care unit-acquired pneumonia in China: a systematic review and meta-analysis. Int J Infect Dis 2014; 29:84-90; PMID:25449241; https://doi.org/ 10.1016/j.ijid.2014.05.030 [DOI] [PubMed] [Google Scholar]
- [12].Qing-tao Z, Bei H, Hong Z. Potential for cost-savings in the care of hospitalized Low-Risk Community-Acquired Pneumonia patients in China. Value Health 2009; 12(1):40-6; PMID:18637052; https://doi.org/ 10.1111/j.1524-4733.2008.00410.x [DOI] [PubMed] [Google Scholar]
- [13].Chiu SS, Ho PL, Khong PL, Ooi C, So LY, Wong WH, Chan EL. Population-based incidence of community acquired pneumonia hospitalization in Hong Kong children younger than 5 years before universal conjugate pneumococcal immunization. J Microbiol Immunol Infect 2016; 49(2):225-9; PMID:25070281; 22484295https://doi.org/10.1016/j.jmii.2014.05.007 [DOI] [PubMed] [Google Scholar]
- [14].Benavides JA, Ovalle OO, Salvador GR, Gray S, Isaacman D, Rodgers GL. Population-based surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Bogota, Colombia. Vaccine 2012; 30:5886-92; PMID:22484295; https://doi.org/ 10.1016/j.vaccine.2012.03.054 [DOI] [PubMed] [Google Scholar]
- [15].Andrade AL, Oliveira R, Vieira MA, Minamisava R, Pessoa V Jr, Brandileone MC, Alves SL, Alfieri F, Pagliarini R, Moraes JC, et al.. Population-based surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Goiania, Brazil. Vaccine 2012; 30:1901-9; PMID:22178522; https://doi.org/ 10.1016/j.vaccine.2011.12.012 [DOI] [PubMed] [Google Scholar]
- [16].Alvis-Guzman N, Orozco-Africano J, Paternina-Caicedo A, Coronell-Rodríguez W, Alvis-Estrada L, Jervis-Jálabe D, De la Hoz-Restrepo F. Treatment costs of diarrheal disease and all-cause pneumonia among children under-5 years of age in Colombia. Vaccine 2013; 31S:C58-62; https://doi.org/ 10.1016/j.vaccine.2013.05.035 [DOI] [PubMed] [Google Scholar]
- [17].Gentile A, Bardach A, Ciapponi A, Garcia-Marti S, Aruj P, Glujovsky D, Calcagno JI, Mazzoni A, Colindres RE. Epidemiology of community-acquired pneumonia in children of Latin America and the Caribbean: a systematic review and meta-analysis. Int J Infect Dis 2012; 16:e5-e15; PMID:22056731; https://doi.org/ 10.1016/j.ijid.2011.09.013 [DOI] [PubMed] [Google Scholar]
- [18].Gutiérrez F, Masiá M, Mirete C, Soldán B, Rodríguez JC, Padilla S, Hernández I, Royo G, Martin-Hidalgo A. The influence of age and gender on the population-based incidence of community- acquired pneumonia caused by different microbial pathogens. J Infect 2006; 53:166-74; PMID:16375972; https://doi.org/ 10.1016/j.jinf.2005.11.006 [DOI] [PubMed] [Google Scholar]
- [19].Murdoch KM, Mitra B, Lambert S, Erbas B. What is the seasonal distribution of community acquired pneumonia over time? A systematic review. Australasian Emergency Nursing J 2014; 17:30-42; PMID:24507181; https://doi.org/ 10.1016/j.aenj.2013.12.002 [DOI] [PubMed] [Google Scholar]
- [20].Brotons P, Gelabert G, Launes C, Sicuri E, Pallares R, Muñoz-Almagro C. Cost of hospitalizing children with invasive pneumococcal pneumonia. Vaccine 2013; 31:1117-22; PMID:23262168; https://doi.org/ 10.1016/j.vaccine.2012.12.025 [DOI] [PubMed] [Google Scholar]
- [21].Meng Q, Wang C, Zhang F, eds. China's health and family planning statistics yearbook 2013. Beijing, China: Peking Union Medical College Press; 2013. [Google Scholar]
- [22].Feng N, Cui H, eds. Tabulation on the 2010 population census of the people's republic of China (Book I). Hong Kong, China: China Statistics Press, 2012. [Google Scholar]
- [23].Wang Y, Vuori Holopinen E, Yaug YH, Wang Y, Hu Y, Leboulleux D, Hedman K, Leinonen M, Peltola H. Relative frequency of Haemophilus influenzae type b pneumonia in Chinese children as evidenced by serology[J]. Pediatr Infect Dis J 2002; 21:271; PMID:12075755; https://doi.org/ 10.1097/00006454-200204000-00002 [DOI] [PubMed] [Google Scholar]
- [24].O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T. Burden of disease caused by Streptococcus pneumonia in children younger than 5 years: global estimates. Lancet 2009; 374:893-902; PMID:19748398; https://doi.org/ 10.1016/S0140-6736(09)61204-6 [DOI] [PubMed] [Google Scholar]
- [25].Ning W, Zhijie A, Huaqing W. A systematic review of the serotype distribution of Streptococcus Pneumonia (Pneumococcus) among all Cases under 18 years old of Pneumococcal infection in China. Chinese J Vaccines Immunization 2014; 20(6):547-55. [Google Scholar]
- [26].Chen Y, Deng W, Wang SM, Mo QM, Jia H, Wang Q, Li SG, Li X, Yao BD, Liu CJ, et al.. Burden of Pneumonia and Meningitis caused by Streptococcus pneumoniae in China among children under 5 Years of Age: A systematic literature review. PLoS One 2011; 6(11):e27333; PMID:22110628; https://doi.org/ 10.1371/journal.pone.0027333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Guan X, Silk BJ, Li W, Fleischauer AT, Xing X, Jiang X, Yu H, Olsen SJ, Cohen AL. Pneumonia incidence and mortality in mainland China: Systematic review of Chinese and English Literature,1985–2008. PLoS One 2010; 5(7):e11721; PMID:20668535; https://doi.org/ 10.1371/journal.pone.0011721 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


