Abstract
Background
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey is used by the Centers of Medicare and Medicaid (CMS) to assess inpatient satisfaction. HCAHPS survey results are publicly reported, and performance began to affect CMS reimbursement to hospitals as of FY2013. However, the impact of severity of illness on patients' self-reported inpatient satisfaction as measured by HCAHPS survey scores remains unknown.
Objective
To determine the impact of severity of illness on patients' self-reported inpatient satisfaction.
Design
The All Patient-Refined, Diagnosis Related Group (APR-DRG) classifies every patient into one of four levels of severity of illness. We evaluated the impact of APR-DRG severity of illness on five HCAHPS domains, two reputation and two environmental questions, using linear regression analysis.
Setting
Adult inpatients discharged from a large, academic, tertiary care hospital
Patients
37,223 patients' HCAHPS survey data were combined with their APR-DRG severity of illness rating over a 39-month period between April 2008 and June 2011.
Measurements
HCAHPS scores
Results
Higher severity of illness was consistently and inversely associated with lower patients' self-reported perception of inpatient hospital satisfaction as measured by HCAHPS scores. For each one-unit increase in severity of illness, the average HCHAPS scores across all five domains were approximately 3 percent lower.
Conclusions
Hospitals treating patients with a higher severity of illness will have lower HCAHPS scores, potentially leading these hospitals to receive lower reimbursement from CMS. Conversely, hospitals with lower severity of illness will receive greater reimbursement. Failure to adequately adjust for severity of illness is a serious flaw in the current HCAHPS reporting system that should be corrected.
Introduction
Under Medicare's value-based purchasing (VBP) program, a portion of a hospital's Medicare reimbursement is impacted by its performance on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.1 The HCAHPS survey is a component of the Centers for Medicare and Medicaid Services (CMS) hospital inpatient quality reporting program.2 Since fiscal year 2008, hospitals that fail to report HCAHPS data, along with certain quality measures, receive reduced annual Medicare payments by 2 percent; this model is referred to as pay-for-reporting.3 In 2013, CMS transitioned from a pay-for-reporting model to a pay-for-performance model, whereby hospitals are still required to report HCAHPS data and certain quality metrics, but their Medicare reimbursement is impacted by their performance on these measures relative to their ranking against all other participating United States hospitals.1
The HCAHPS survey is a standardized survey designed by the Agency for Healthcare Research and Quality, and its use is required by Medicare. The instrument queries recently discharged hospital inpatients with 22 questions in six domains, or dimensions, of care, two questions for reputation (overall rating and would recommend), and two questions on the hospital environment (quiet at night and cleanliness). The survey instrument is believed to accurately assess the primary drivers of adult inpatient satisfaction and is designed to provide a standard and objective comparison of a hospital's performance relative to other hospitals. Survey results are publicly available on the CMS website, Hospital Compare, which is updated each calendar quarter.3
The HCAHPS survey also collects basic patient demographics from five additional survey questions, including self-reported health status. CMS utilizes the demographic information and additional administrative data from hospital records to calculate and apply a patient mix adjustment (PMA) to each hospital's score prior to publication.4
CMS states that “the goal of adjusting for patient mix is to estimate how different hospitals would be rated if they all provided care to comparable groups of patients.”4 The self-reported health status is a key variable in the patient mix adjustment that CMS applies to the scores. The HCAHPS process does not require reporting of additional patient clinical variables or other administrative data such as billing codes that could be used to strengthen the patient mix adjustment.
Under the value-based purchasing program, hospitals are ranked nationally against all other participating hospitals. The impact of patient variables such as clinical risk on HCAHPS performance is not known. We sought to determine whether patient-related factors such as comorbidity may independently impact HCAHPS performance and subsequent hospital ranking. Developed by 3M (St. Paul, Minnesota) to allow hospitals to analyze patient risk, the All Patient Refined Diagnosis Related Group (APR-DRG) severity index score is a standard measure for analyzing and risk adjusting administrative data.5 We tested whether a patient mix adjustment model based on a patient's severity index, as measured by APR-DRG, would provide a more robust risk adjustment methodology for HCAHPS scores.
Methods
The Cleveland Clinic Health System (CCHS) main campus hospital is a 1,200-bed academic tertiary care specialty center located in Cleveland, Ohio. The HCAHPS survey process for CCHS is administered by a CMS-approved vendor, and the survey data are stored on an internal, IRB- approved database. Fifty-eight percent of eligible main campus inpatient discharges are randomly sampled to receive the HCAHPS survey. The average response rate is 35 percent.
For each patient with an HCAHPS survey, the APR-DRG severity index was determined. To compare and assess the effect of the severity index on HCAHPS scores, it is necessary to determine a national severity index for all hospitals in the United States. Because there is no published, national severity index benchmark that represents the average of all hospitals, to accurately assess how HCAHPS performance may change with severity index modeling, we selected three theoretical national severity indices: 1, 1.5 and 2.0, so that we could observe the change in HCAHPS scores across a range of severity indices.
Five HCAHPS domains (doctor, nurse, medication communication, responsiveness and pain management), two questions for reputation (overall rating and would recommend) and two questions for hospital environment (cleanliness and quiet at night) were analyzed. The discharge domain is a dichotomous variable based on receiving written instructions and was excluded from the analysis.
We first calculated the unadjusted score for each domain/question for every patient survey. We then calculated the CMS patient-mix adjusted score of each domain of every patient survey based on the method used by CMS.6 National means for patient mix adjusted variables and coefficients for adjustment were obtained from online HCAHPS published reports for patient mix coefficients by patient discharge year.6, 7, 8
CMS patient mix adjustment data for 2011 were not available, and the most recent CMS patient mix adjustment algorithms, as published by CMS (October 2011, publicly reported patient mix coefficients of 2010 patient discharges) were used. For each of the five domains and four questions, a regression of the calculated patient mix adjusted score on severity within each year was performed to obtain the annual regression coefficients for patient mix adjustment. Because we have data from four years for each domain, there were four sets of such coefficients. Finally, the calculated patient mix adjusted score for each patient was further adjusted for the severity index based on these regression coefficients. The amount of adjustment was equal to the regression coefficient of severity index times the difference between the CCF mean severity index and the assumed levels of the benchmark national severity index (1.0, 1.5, or 2.0) and then multiplying by −1.0 This was consistent with the usage of CMS patient-mix adjustment.6 Statistical significance was accessed at the p < 0.05 level, and all analyses were performed using SAS 9.2 (Cary, NC).
Results
There were 174,164 inpatients discharged from the Cleveland Clinic main campus between April 2008 and June 2011. Of the patients randomly selected to receive the HCAHPS survey, 37,223 (21 percent) returned a survey during that time period. In total, 37.2 percent of the discharges were APR-DRG severity of illness level three or four (Table 1).
Table 1.
Number of hospitalizations by year and severity of illness
| 2008(N=7,074) | 2009(N=12,469) | 2010(N=12,343) | 2011(N=5,337) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | SOI | N | n(%) | N | n(%) | N | n (%) | N | n (%) |
| SOI | 1 | 6951 | 1812(26) | 12239 | 3042(25) | 12137 | 2888(24) | 5047 | 1158(23) |
| 2 | 2673(38) | 4645(38) | 4462(37) | 1866(37) | |||||
| 3 | 1912(28) | 3488(28) | 3730(31) | 1528(30) | |||||
| 4 | 554(8) | 1064(8.7) | 1057(8.7) | 495(9.8) | |||||
Table 2 presents the unadjusted HCAHPS scores, the patient mix adjusted HCAHPS scores based on the current CMS model and the adjusted HCAHPS scores for each modeled national severity index. Overall, increasing severity index was inversely associated with self-reported patient satisfaction in all of the areas we evaluated.
Table 2.
The unadjusted key HCAHPS domain scores, PMA adjusted score, and PMA and SOI adjusted score after SOI adjustment.
| Domain | Year | CCF mean SOI | Unadj. score | PMA adj. score | Further SOI adjusted score if national mean | ||
|---|---|---|---|---|---|---|---|
| SOI=1 | SOI=1.5 | SOI=2 | |||||
| Nurse | 2008 | 2.174 | 65.56 | 66.47 | 68.65 | 67.72 | 66.79 |
| Comm | 2009 | 2.21 | 71.09 | 72.16 | 74.15 | 73.33 | 72.51 |
| 2010 | 2.244 | 74.71 | 75.87 | 77.46 | 76.82 | 76.18 | |
| 2011 | 2.269 | 76.45 | 77.69 | 78.77 | 78.35 | 77.92 | |
| Doctor | 2008 | 2.174 | 74.69 | 73.41 | 75.52 | 74.62 | 73.72 |
| Comm | 2009 | 2.21 | 76.61 | 75.56 | 77.05 | 76.43 | 75.82 |
| 2010 | 2.244 | 76.92 | 76.68 | 78.63 | 77.84 | 77.06 | |
| 2011 | 2.269 | 78.87 | 78.67 | 80.64 | 79.86 | 79.09 | |
| Staff | 2008 | 2.174 | 44.64 | 45.82 | 49.02 | 47.66 | 46.29 |
| Response | 2009 | 2.21 | 52.81 | 54.28 | 57.68 | 56.28 | 54.87 |
| 2010 | 2.244 | 56.58 | 58.32 | 60.90 | 59.87 | 58.83 | |
| 2011 | 2.269 | 58.02 | 59.82 | 62.42 | 61.39 | 60.37 | |
| Medication | 2008 | 2.174 | 50.84 | 51.78 | 54.09 | 53.11 | 52.12 |
| Comm | 2009 | 2.21 | 54.23 | 55.41 | 58.51 | 57.23 | 55.95 |
| 2010 | 2.244 | 58.06 | 59.60 | 62.19 | 61.15 | 60.11 | |
| 2011 | 2.269 | 60.85 | 62.37 | 64.54 | 63.69 | 62.84 | |
Communication with doctor
At the modeled national benchmarks of APR-DRG severity index (1.0, 1.5 and 2.0), applying a severity of illness adjustment using APR-DRG severity index to the CMS patient mix adjusted score significantly elevated the HCAHPS scores for doctor communication. For example, assuming national benchmark of APR-DRG severity index as 1, after severity index adjustment, the score for doctor communication of year 2010 increased from 75.87 (PMA adjusted) to 77.46. A visualization of score change after adjustment for each year was shown in Graph 1. The regression coefficients of severity index were −1.80, −1.23, −1.56, −1.55 for years 2008, 2009, 2010 and 2011, respectively (All p<=0.0029).
Responsiveness of staff
At the modeled national benchmarks of APR-DRG severity index (1.0, 1.5 and 2.0), applying a severity of illness adjustment using APR-DRG severity index to the CMS PMA-adjusted score significantly elevated the HCAHPS scores for staff responsiveness (Graph 1). The regression coefficients of severity index (Column 3 of Table 2) were consistently negative and ranged from −2.05 and −2.81(All p<=0.0054).
Communication of medication
At the modeled national benchmarks of APR-DRG severity index (1.0, 1.5 and 2.0), applying a severity of illness adjustment using APR-DRG severity index to the CMS PMA-adjusted score significantly elevated the HCAHPS scores for medication communication (Graph 1). The regression coefficients of severity index (Column 3 of Table 2) were consistently negative and ranged from −1.71 and −2.56 (All p<=0.0165).
Communication with nurse
At the modeled national benchmarks of APR-DRG severity index (1.0, 1.5 and 2.0), applying a severity of illness adjustment using APR-DRG severity index to the CMS PMA-adjusted score significantly elevated the HCAHPS scores for nurse communication for years 2008, 2009 and 2010 (Graph 1). The regression coefficients of severity index (Column 3 of Table 2) were consistently negative and ranged from –.85 and −1.86 (All p<=0.004 for years 2008, 2009 and 2010, and p=0.12 for year 2011).
Other domains and questions
For pain management, cleanliness and quiet at night, the effect of severity of illness adjustment was not significant, and the direction of the effect was variable when evaluating the coefficients. For the overall rating and recommendation, higher severity of illness adjustment was associated with a higher score in general when looking at the regression coefficients. However, there was no evidence that the effect was significant for every year.
Comment
Since 2013, the HCHAPS scores impact the reimbursement of all U.S. hospitals. The intent of the value-based purchasing program is to financially reward hospitals for achieving high rates of patient satisfaction and penalize hospitals with low patient satisfaction. Accordingly, the process of case-mix adjustment must be accurate and reliable.
We examined the relationship between patients' severity of illness as measured by their APR-DRG severity index and self-reported patient satisfaction as measured by the HCAHPS survey over a 39-month period from April 2008 through June 2011 at a single tertiary care, academic medical center. Unadjusted HCAHPS scores, and HCAHPS scores adjusted by the CMS patient mix adjustment model, were further analyzed with a risk adjustment model developed utilizing a severity index defined by APR DRG.
We found that greater patient severity of illness significantly and negatively impacted patients' perception of their inpatient hospital experience. This effect was demonstrated on important HCAHPS domains including doctor communication, staff responsiveness, medication communication and nurse communication. For these domains, the HCAHPS scores adjusted for both the severity index and the CMS patient mix adjustment were higher than the scores adjusted using the CMS patient mix adjustment alone. Thus, for hospitals with a high average severity of illness, the current CMS process results in artificially depressed HCAHPS scores, whereas a hospital with a low severity of illness will appear to have artificially high HCAHPS scores.
The HCAHPS survey instrument and its corresponding patient mix adjustment were developed to provide a meaningful and objective process to compare consumer perceptions of their satisfaction with inpatient hospital admissions across hospitals of any size. CMS has appropriately identified patient mix adjustment as an important component of the reporting process to ensure that hospitals' reported data is ranked against comparable patients. However, the current HCAHPS process does not include information such as clinical data or DRG billing data that could be used in a traditional risk adjustment model and instead relies on surrogate markers such as self-reported health status to adjust for intrinsic patient factors that may impact the HCAHPS results. Our use of the APR-DRG severity index, a direct variable defining patient risk, was an attempt to apply a risk adjustment model that can potentially account for patient-related factors such as severity of illness.
Hospitals' average severity of illness is affected primarily by the complexity of patients they treat, and large academic tertiary care hospitals will naturally have a higher average severity of illness than smaller community hospitals. The APR-DRG classification system, developed by 3M, offers hospitals a model to classify patients by severity.5 3M reports that the average severity of illness, based on 21 million patients in its national database, is 1.0719. By comparison, the Cleveland Clinic main campus hospital's severity of illness is 2.38; this higher severity of illness likely reflects the finding at other large, academic medical centers.
Because there are more than 4,000 hospitals in the United States, and the true national average severity of illness is not known, we wanted to include in our analysis the possibility that the national average was higher than 1.0719. Therefore, we modeled our hypothesis against three possible national severity of illness benchmarks (1.0, 1.5, 2.0). We believe our findings demonstrate that because all hospitals are judged as equals in the current CMS process, it is necessary to understand average national severity of illnesses to adequately adjust HCAHPS data.
Incorporating our patients' severity index into our CMS patient mix adjusted scores, and further modeling those scores to adjust for severity of illness compared to the three estimated national benchmarks, revealed that as the national severity of illness benchmark declines, our scores consistently increase in four pivotal HCAHPS domains. This means that if the national severity of illness average is truly low, then large hospitals with complex patients, whose average severity of illness is high, will have lower scores attributable to the complexity of their patients. We believe that these findings support our hypothesis that there is a direct impact of patient risk on HCAHPS performance.
The average percent change across the five key domains (nurse communication, doctor communication, staff responsiveness, medication communication and pain management) using the combined CMS patient mix adjustment and the APR-DRG severity index adjustment at a modeled national hospital severity of illness of 1.0, compared to the CMS patient mix adjustment alone, was nearly 3 percent.
Figure I.
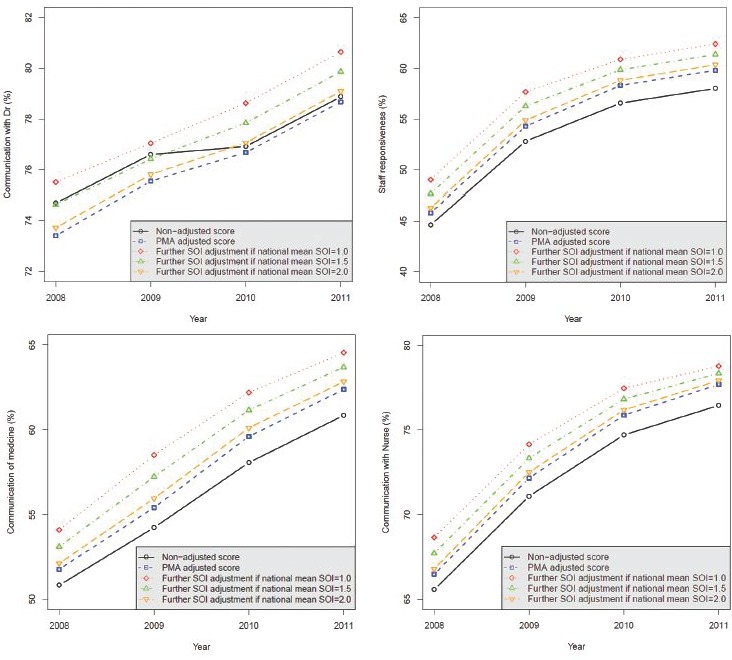
- Key HCAHPS Domains
While the absolute HCAHPS score percent change incorporating the new severity index seems small, the change has significant consequences for hospital percentile rankings nationally. If the doctor communication domain score for 2011 was 78.67 using the CMS-only adjustment, after further applying a severity index adjustment, the score would change to 80.64, which would change the percentile ranking from the 37th to the 53rd percentile respectively. For some domains (e.g. nurse communication), the difference between scoring in the 25th compared to the 90th percentile is only 10 percentage points difference.
While we believe our study establishes a link between the impact of severity of illness and HCAHPS performance, what remains unanswered is why the impact is significant. Many of the HCAHPS questions are perception metrics – patients rate satisfaction based on their perception of the service they receive (i.e.: Did the doctor treat you with courtesy and respect?). It is unclear if the decrement of the perception of service quality with rising severity of illness is real or perceived. For example, for patients who rate hospital service low, is the patient perceiving that the service standard is lower because of intrinsic factors affecting perception (i.e. depression, complicated disease processes, or other), or is the service quality really lower because of intrinsic hospital factors (i.e. poorer service to chronically ill patients).
There are other potential factors that may negatively impact satisfaction in this patient population. Severity index may be a surrogate marker for inpatients suffering from medical or procedural complications. The occurrence of natural and pathogenic complications may negatively impact patients' perception of their experience. Patients with higher severity index may have multiple specialists and many caregivers involved in their care, thereby increasing the complexity of their management and the potential for poor care coordination, leading to dissatisfaction. In addition, patients transferred to an academic medical center for emergency treatment or for access to advanced tertiary services may have their health care perception defined by the transferring hospital. The impact of these variables on patient satisfaction will be important to understand as hospitals work to improve their HCAHPS scores, and we work to improve the HCAHPS reporting process.
Other variables have been identified as having a significant impact on HCAHPS results. The Centers for Medicare and Medicaid Services currently authorizes surveys to be conducted in four modes, mailed questionnaire only, telephone interview only, mixed mode (mailed questionnaire with telephone followup) and interactive voice recognition response.2 A CMS-sponsored study completed in 2008 demonstrated that patients responding to telephone surveys had higher overall scores than those responding to paper surveys.4
Others have demonstrated that HCAHPS scores can be affected by demographic patient variables such as age, education and language, and other nontraditional adjustment variables such as self-reported health status, service line and language spoken at home.7 These variables represent the basis for the current patient mix adjustment that CMS applies to HCAHPS data before public reporting of the data on Hospital Compare.6 If HCAHPS scores are affected by demographic patient variables, mode of survey administration and other nontraditional risk adjustment variables used in the CMS model, then it is not surprising that the behavior of the HCAHPS scores will change with other important clinical variables such as severity of illness.
Under the current CMS Hospital Inpatient Quality Reporting, 2 percent of hospitals' Medicare reimbursement is at risk contingent upon reporting of core measures and HCAHPS data.3 As a requirement of the Affordable Care Act of 2010, CMS instituted a value-based incentive payment structure for hospitals beginning in FY 2013. With this requirement, pay-for-reporting transitioned to pay-for-performance, which uses HCAHPS data, combined with other metrics including core measures and hospital-acquired conditions, to determine each hospital's overall value-based purchasing score. The value-based purchasing score then determines the amount each hospital is eligible to receive back. The overall hold back for each hospital at risk began at 1 percent in FY 2013, escalating to 2 percent in 2017, with 30 percent of this amount at risk based on HCAHPS performance.1
Hospitals today are operating under increasing regulatory requirements, rising patient expectations and decreasing reimbursement. The average hospital operating margin in the United States is approximately 2.2 percent.8 Given the impact of the value-based purchasing model on hospitals' financial performance, the model that compares hospital performance and determines reimbursement must be robust. If a hospital has a significant amount of Medicare reimbursement, the effect of placing 2 percent of its reimbursement at risk and its ultimate impact on the bottom line is significant.
CMS has demonstrated how a variety of variables impact patient perception. If hospitals will be required to submit their results for public reporting, and if they are to be held financially accountable for their performance, then it is essential to understand how variables such as severity of illness, length of stay, depression and other factors may affect HCAHPS scores so as to establish an appropriate model that treats the hospital fairly. There remain a number of unanswered questions about the veracity of the data and the reliability of the process.
Our findings will have profound and important implications for the fairness of the VBP model as it relates to the HCAHPS component and for hospitals that treat patients with a higher-than-average severity of illness. Without valid and appropriate risk adjustment of the HCAHPS data, large academic medical centers will paradoxically be penalized for treating the sickest patients in our society.
Providers and hospitals have an important responsibility to provide high-quality service standards to their patients in addition to providing high-quality and safe medical care. Driving toward patient centeredness and focusing on the patient experience is the right thing to do for patients, and hospitals and providers should be held accountable for their performance. The initiative to link value-based performance to financial incentives is a credible tool to drive improvement, accountability and transparency, and if we are to make a meaningful impact on improving the delivery of care in the United States, this model must be protected and strengthened. We believe this analysis demonstrates that there are additional factors that impact an individual hospitals performance on HCAHPS scores, and that this information will help make the process of adjustment more credible, reliable and fair.
References
- 1.Centers for Medicare & Medicaid Services, Baltimore, MD. “Fact Sheet Final Rule for First Year of Hospital Value-Based Purchasing Program.” Accessed Dec. 8, 2011. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html
- 2.Centers for Medicare & Medicaid Services, Baltimore, MD: Accessed Dec. 8, 2011. http://www.hcahpsonline.org. [Google Scholar]
- 3.Centers for Medicare & Medicaid Services, Baltimore, MD: “HCAHPS fact sheet.” Accessed Dec. 8, 2011. Updated August 2013. http://www.hcahpsonline.org/files/August_2013_HCAHPS_Fact_Sheet3.pdf [Google Scholar]
- 4.Centers for Medicare & Medicaid Services, Baltimore, MD. “Mode and Patient-mix Adjustment of the CAHPS® Hospital Survey (HCAHPS).” Accessed Dec.8, 2011. http://www.hcahpsonline.org/files/Final%20Draft%20Description%20of%20HCAHPS%20Mode%20and%20PMA%20with%20bottom%20box%20modedoc%20April%2030,%202008.pdf
- 5.3M, St. Paul, MN: Accessed Dec 8, 2011. http://solutions.3m.com/wps/portal/3M/en_US/Health-Information-Systems/HIS/Products-and-Services/Products-List-A-Z/APR-DRG-Software/ [Google Scholar]
- 6.Centers for Medicare & Medicaid Services, Baltimore, MD. “Patient-mix Coefficients for September 2009 Publicly Reported HCAHPS Results.” Accessed Dec. 8, 2011. http://www.hcahpsonline.org/files/September%202009%20%20PMA%20Web%20Document%2007-13-2009.pdf [Google Scholar]
- 7.Centers for Medicare & Medicaid Services, Baltimore, MD. “Patient-mix Coefficients for September 2010 Publicly Reported HCAHPS Results.” Accessed Dec. 8, 2011. http://www.hcahpsonline.org/files/September%202010%20PMA%20Web%20Document%207-12-2010.pdf
- 8.Centers for Medicare & Medicaid Services, Baltimore, MD. “Patient-mix Coefficients for October 2011 Publicly Reported HCAHPS Results.” Accessed Dec. 8, 2011. http://www.hcahpsonline.org/files/October%202011%20PMA%20Web%20Document%20.pdf
- 9.Elliott Marc N. Zaslavsky Alan M. Goldstein Elizabeth et al. Effects of survey mode, patient mix, and nonresponse on CAHPS Hospital Survey scores. Health Services Research 2009; 44: 501–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moody's Investors Service. “U.S. Not-for-Profit Hospital Medians Show Resiliency against Industry Headwinds But Challenges Still Support Negative Outlook.” Special Comment Aug. 30 2011. [Google Scholar]


