Abstract
Physician involvement in service training initiatives can have a significant impact on the patient experience. This paper highlights some of the key components of what makes physician involvement in training engagements successful and includes anecdotes and data to support the findings.
Our service training program emerged from a desire to help clinic sections improve the patient experience. Our workshops contained customized materials that addressed service priority areas, as identified by patient satisfaction survey results, for individual clinic sections and included opportunities to practice the concepts introduced in each session. However, we were missing one key ingredient in the recipe for a successful training program — physician involvement.
This paper focuses on a best practice in which two physicians took an active role in creating, customizing and delivering service training for their clinic section and made a tremendous impact on their overall patient satisfaction scores and section morale.
In 2010, the department of Service Management with Emory Clinic in Atlanta, Georgia, recognized a need for internal service training initiatives focusing on service skill building (communication, empathy, problem solving, anticipating patient needs, etc.) as part of our plan to improve the patient experience. We realized that our existing service training offerings, though helpful as an introduction to service, were too general and broad in scope to meet the unique needs of individual outpatient clinics. In order to provide better resources for our clinic sections, we began to develop a new service training program. The goal was to educate and empower staff and physicians to create the ideal patient and family experience by utilizing customized, service-based training workshops. These workshops, led by training specialists, would address an individual clinic section's specific service challenges, provide tools and resources to educate it on patient satisfaction and ultimately provide a better experience for its patients.
Throughout the development of our program, we learned that section specific customization, as well as leadership involvement from both administrator and physician champions, was essential to the success of any training engagement. After months of trial and error developing our training program, we were able to clearly define our recipe for success (Figure 1).
Figure 1.
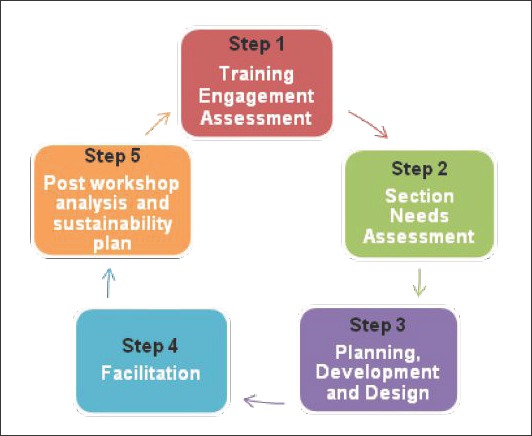
Training Engagement, Design and Development Model
Case Study/Best Practice
Perhaps the most beneficial training encounter that ultimately led to our “aha” moment and helped us further define our training process was our engagement with General Internal Medicine at our Midtown location (GIM@MOT). Prior to our workshop series with GIM@MOT, we were conducting service workshops exclusively for staff members (MAs, LPNs, nurses, patient services coordinators and clinic managers). Care providers (physicians, PAs and NPs) were not initially involved in our training programs. Our workshops were well regarded and effective, but there was a consistent theme that echoed from staff that “the workshops are helpful, but you should include care providers in the training.”
We understood that involving care providers in each training engagement would send the message that we are all in this together, positively impacting morale and sending a message of collaboration in the clinic section.
In February 2013, we were approached by two physicians from GIM@MOT with a request to conduct training sessions that included both staff and care providers. We were excited to break new ground with this project, hoping that a unified training effort would drive greater improvement in both patient satisfaction and staff morale. The physicians agreed that in order to make significant changes to their patient satisfaction scores, a true shift had to be adopted by everyone. They could no longer operate in silos; they had to work together.
GIM@MOT Training Process
Step 1: Training engagement assessment
Our training engagement with GIM@MOT began with an initial assessment to determine if it was a good candidate for a training commitment. We found that the organization had all of the necessary requirements: actively engaged leadership, a willingness to embrace change and specific, measurable patient satisfaction goals for improvement. The physician leaders and clinic manager were highly motivated to improve their patient satisfaction scores and wanted to provide resources for staff and care providers to improve the patient experience.
Step 2: Section needs assessment
In order to select the most relevant, service-related topics, we analyzed all patient satisfaction data sources available to us — patient satisfaction mean scores and rankings, priority index reports, patient comments collected through the Press Ganey Medical Practice Survey and patient complaint trends via our incident reporting system. For a three-week period, we conducted department observations, shadowed staff and collected staff opinion survey results. We used patient satisfaction survey results as a marker for improvement. During our assessment phase, GIM@MOT was ranked in the 11th percentile (as compared to its Press Ganey General Internal Medicine benchmark group). Based on the analysis of all quantitative and qualitative data, we chose the service workshop themes of sensitivity to patient needs, defining unique steps of great service and creating lasting impressions.
Step 3: Planning, development and design
Our development sessions began in March 2013 with the planning team (service trainers, physician champions, nurse manager, clinic manager and service ambassador). We met biweekly for one hour to develop our training plan and content for each service workshop. With physician champion input and direct involvement, we modified existing material to create a robust and relevant workshop series, ensuring the workshops addressed GIM@MOT's specific service opportunities. A heavy emphasis was placed on interactive activities and role-playing to support the concepts presented. The initial task was to establish a goal by using its Press Ganey percentile ranking as a metric. The organization specifically focused on moving from the 11th percentile (as compared to its General Internal Medicine Benchmark Group) to the 60th percentile by the end of the calendar year. It further supported this initiative by soliciting staff input and creating a department vision statement. With our end goal established and collective buy-in established, we were prepared to conduct a series of workshops designed to be informative, engaging and targeted at specific improvement goals.
Figure 2.
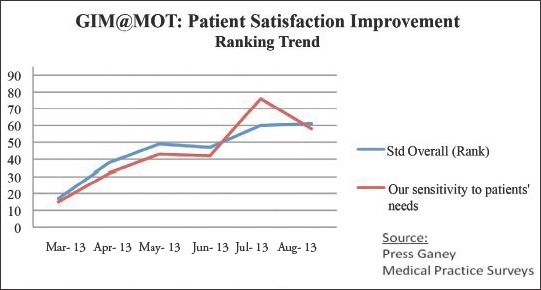
Patient Satisfaction Improvement Ranking Trends for “Overall” and “Sensitivity to Patients' Needs” survey questions for a 6 month period
Figure 3.
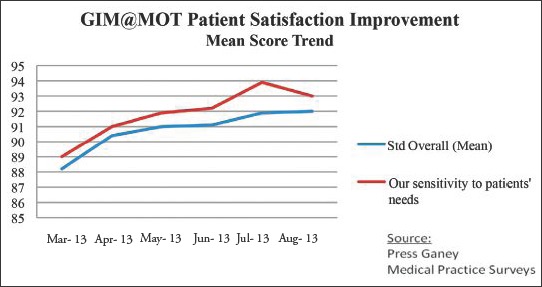
Patient Satisfaction Improvement Mean Score Trend for “Overall” and “ Sensitivity to Patients' Needs” survey questions for a six-month period
Figure 4.
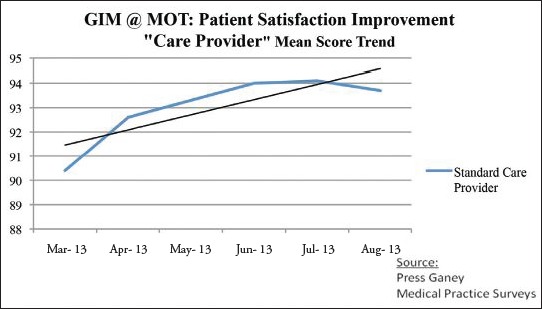
Patient Satisfaction Improvement Mean Score Trend for “Care Provider” survey questions for a six-month period
Step 4: Workshop facilitation
It was challenging to find time in busy clinic schedules to bring everyone together for each one-hour workshop. To ensure all staff and care providers were able to attend these required sessions, the clinic manager created four teams, with approximately seven members on each. Each team included representatives from every job role in the practice. For example, the Blue Team consisted of one MA, two patient service coordinators, two physicians, one nurse manager and one nurse. We conducted each workshop twice per month, with two teams at each session. The workshops were structured to devote the majority of time to practicing the concepts presented during the workshop. Typically, one of our physician champions introduced the workshop theme and delivered a motivating message to set the tone for the session. The remainder of the workshop agenda was 20 percent lecture, 50 percent interactive activities such as role-playing, problem-solving sessions and small group discussions, and 30 percent evaluation and participant feedback.
All workshops were delivered during a period of four months, starting in May and concluding in August. Thus, the training series was aptly titled “Summer of Satisfaction.”
Step 5: Post workshop analysis and sustainability plan
The “Summer of Satisfaction” training engagement yielded impressive results. We began with our Press Ganey goal of reaching the 60th percentile by teaching specific strategies to impact the patient experience. The leadership team also chose to track mean score progress on the “Sensitivity to Patient's Needs” question, a high-priority question impacting the overall score (Press Ganey Associates, Inc. (2013). Medical Practice Survey. South Bend, IN: Author). As the training engagement progressed, we saw a significant increase in mean scores and rankings for those selected areas.
A unique discovery
As this was the first training engagement where we had the benefit of physician involvement in the creation of customized content, we were excited to see upward movement in Press Ganey “Care Provider” scores, as well. (Press Ganey Associates, Inc. (2013). Medical Practice Survey. South Bend, IN: Author). In addition to providing input for the workshop content, the physician champions highly encouraged their colleagues to be active participants in the sessions. Their concerted efforts seemed to make a positive impact on “Care Provider” mean scores, something we had not previously experienced with past training engagements.
This improvement was not solely represented in patient satisfaction scores but was also visible in changes to physician behavior. For example, one physician shared with us how she implemented changes to her clinic processes as a result of the workshop series. She stated that in the past, she chose not to see late patients, fearing that it would push her schedule further behind, but has now realized that the stress and chaos that ensued negatively impacted her patients and staff. As she began to work late patients into her schedule, she was surprised by the reduction in stress and resulting lack of negative impact on her clinic schedule. Her participation in the workshop series and willingness to change her own behavior inspired a renewed eagerness to improve patient and staff satisfaction.
Sustainability plan: Booster shots
In order to maintain the positive momentum generated through the “Summer of Satisfaction,” we conducted follow-up workshops two months after the conclusion of the workshop series. We named these follow-up sessions “booster shots,” during which we reviewed concepts previously introduced over the summer and introduced new service skills to promote learning. We also supplied our physician champions with an extensive list of group activities, designed for staff meetings, and daily huddles (quick group meetings) to sustain the enthusiasm for improving the patient experience.
Training engagement outcomes
The entire department's increased awareness of service priorities, coupled with specific strategies for service improvement, team building and physician involvement in the design process, created a lasting positive effect on department morale and on the patient experience. By the end of our training engagement, GIM@MOT not only reached its goal of scoring in the 60th percentile in patient satisfaction ranking, it did it three months ahead of schedule. It also saw significant improvement in “Sensitivity to Patients Needs,” “Care Provider” and “Overall” mean scores during this period of focused attention to patient satisfaction. The success of this training engagement was largely attributed to the leadership, enthusiasm and involvement of our physician champions. They were a critical part of the content design team and actively supported and reinforced the service messages presented. They did not make excuses for low patient satisfaction scores and poor department morale. Instead, they took responsibility for their own patient satisfaction scores, established service goals and led by example. Their participation set the tone for the department and helped to drive change. We were excited to have collaborated with this team and have improved our training process as result. We are now approaching each training engagement differently, requesting physician involvement in content design and delivery, hoping to replicate these positive results.


