Abstract
Objectives
Acquiring communication and interpersonal skills is an important part of providing patient-centered care and improving patient satisfaction. This study explores whether residents' own values about patient communication can be influenced by training.
Methods
As part of service excellence, a three-hour communication skills training in AIDET™ (Acknowledge, Introduce, Duration, Explanation, Thank You) was delivered to first and second Post-Graduate Year (PGY) residents (n = 123). A survey was designed to measure the value of patient communication and administered pre/post communication skills training.
Results
Residents' scores about communication values improved significantly for all areas pre- to post-training for patient communication skills (p<0.04). After training, there was little difference by medical specialty, other than surgical specialties, which showed the greatest increase in valuing requesting permission (p=0.034). Gender was also not associated with differences in values, except men showed a greater increase in valuing sitting down (p=0.021) and introductions (p=0.005) than women who already valued these specific behaviors prior to training.
Conclusions
Residents value communication, and AIDET™ training is a useful tool to increase the values of good communication and interpersonal skills to enhance service excellence.
Keywords: communication, values, skills training, AIDET™
Introduction
Medical education has increasingly focused on the skill of doctor-patient communication since the 1970s.1 More recently, communication has been seen as a core competency by the Accreditation Council for Graduate Medical Education (ACGME). Communication between doctors and patients encompasses many domains including exchanging information with patients, teaming up with patients and their families, collaborating with other medical professionals, and delivering difficult news. The literature shows that an effective physician-patient partnership can have a positive impact on patient attitudes and expectations of care, can improve patient satisfaction, and can lower patient anxiety.2–7 Furthermore, higher patient psychosocial well-being has been positively associated with better patient adherence to treatment and improved clinical outcomes.8–10
Patient satisfaction is tied to good communication, and now is directly measured by questions on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey that hospitalized patients complete after discharge. Press Ganey, a national patient satisfaction vendor, includes five additional questions in the doctor communication domain. Studies have investigated how physicians are taught to communicate, but many have not included what behaviors are taught to improve patient communication.11 Furthermore, these studies contain a mismatch between the assessment instruments or procedures and the actual behaviors measured. Current models, such as The Four Habits Model, are now addressing these behavioral tasks and matching them to evaluations.12 In this training model, physicians are taught about communication skills in four broad categories: 1) Invest in the beginning, 2) Elicit the patient's perspective, 3) Demonstrate empathy, and 4) Invest in the end. There is now the Four Habits Coding Scheme, which is an instrument derived from this teaching model.13
The AIDET™ mnemonic was developed originally by the Studer Group as a template for improving physician communication with patients and now is widely applied across hospitals and trainings: Acknowledge (address each person in the room), Introduce (introducing yourself, role, specialty), Duration (setting expectations for the visit/procedure), Explanation (treatment and/or diagnosis), and Tank You (appreciation).14–16 The Doctor Communication, Attention, Respect, Expertise (CARE) Task Force is part of our institution's service excellence efforts and is charged with improving patients' satisfaction with their physicians. In 2012, the task force did a needs assessment of communication skills training using survey data from program directors. Less than 10 percent of program directors acknowledged training house staff in verbal and nonverbal communication skills. This reinforced the strategic plan to train all PGY1s and PGY2s who are often on the front line with patients. Training was developed to address these communication skills for house staff physicians to improve patient satisfaction. Training included didactics, large and small group discussions with faculty facilitators, video of good/bad doctor-patient communication, role play and audience response ratings with discussion. Previous research has shown that communication skills training increases self-efficacy up to three years later and increases performance up to a year later.12
Increasing residents' values of these communication skills, like self-efficacy, may be another determinant of utilization and retention of these skills with patients.
Methods
In 2013, as part of an institutional effort on value-based purchasing and service excellence, six three-hour communication skills training sessions in AIDET™ were delivered to mixed clinical specialty groups of PGY1s and PGY2s. IRB approved surveys (n=123) were collected before and after training to determine changes in participants' valuation of the specific communication skill. All residents were asked to complete the survey, but some arrived late and missed the pre-training survey.
The survey was developed by pairing AIDET™ behaviors such as introducing oneself when entering the room, as well as other behaviors such as sitting down with a patient with a five-point Likert scale response for how much the resident valued that behavior. (Figure 1.) The survey was developed internally by three of the authors (Kunkel, E., Braverman, A., Katona, A.) for the purpose of this study. It included demographics for PG year, specialty, gender and age. Eighteen items were rated very important, important, moderately important, of little importance, or unimportant. The ratings were converted to a 1 to 5 scale. No items were directly related to the AIDET™ mnemonic taught in the communication skills workshop. Two questions were related to No. 2 of the three-part physician initiative: sitting down to speak with the patient and asking, “What questions do you have for me?” The third part of the physician initiative related to use of AIDET™. Six additional items included both verbal and nonverbal communication skills. All items paralleled the audience response segment of the communication skills workshop. Participants were asked to name which item was most important for patient care and which item was least important for patient care. Heretofore, studies have measured the actual behaviors and not the residents' perception about the value of these behaviors.
Figure 1.
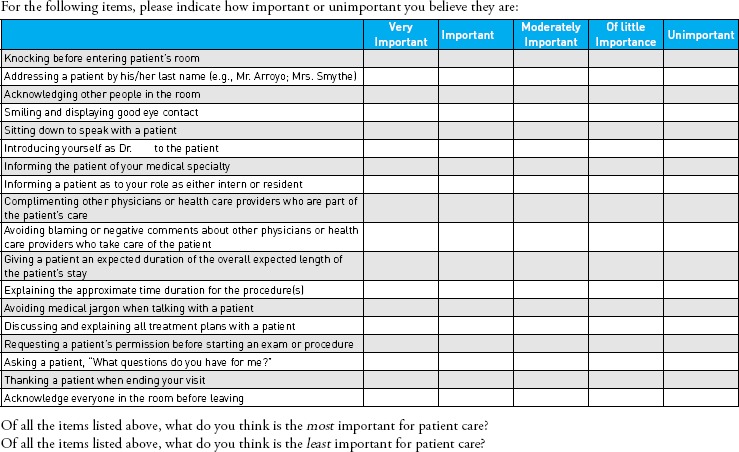
Values Questionnaire
Descriptive statistics were calculated for all collected items at both pre- and post-survey time points. Frequencies and percentages were reported for categorical items; means and standard deviations were reported for continuous items.
While the survey was administered in a pre-post format, there were no identifiers that matched the pre- and post-surveys, and there were different numbers of surveys collected pre and post (123 and 128, respectively). This was done to preserve resident confidentiality in the context of evaluating the impact of training. A pseudo ID was created based on sex, PGY, age and specialty. This allowed for unique identification of about 50 respondents and small clusters of the remaining respondents that ranged in size from two to six. This identifier was then used to represent clusters in generalized estimating equation models (GEE) with robust variance estimation. These models were used to estimate differences in scores overall, and differences in score change by sex, PGY and specialty.
HCAHPS and Press Ganey scores preceding and following communication skills training were compared to see if there were positive trends but were not calculated for statistical significance.
Results
Table 1 presents respondent characteristics at pre and post. Respondents were evenly divided by sex and averaged 28 years of age. Table 2 presents the change in residents' valuation of communication behaviors after skills training. Smaller values reflect a higher valuation of the communication or interpersonal skill being queried, e.g., a drop in score meant the physician endorsed a higher value for that particular skill after training. Scores for all questions declined significantly (p<0.04) for all questions between pre- and post-survey, indicating a higher valuation for all communication skills after training.
Table 1.
Respondent Characteristics
| Pre | Post | |
|---|---|---|
| n(%) | n(%) | |
| Gender | ||
| Female | 60 (48.78) | 64 (50.00) |
| Male | 63 (51.22) | 64 (50.00) |
| PGY | ||
| 1 | 99 (79.20) | 101 (79.53) |
| 2 | 23 (18.40) | 24 (18.90) |
| 3 | 0 (0.00) | 0 (0.00) |
| 4 | 1 (0.80) | 0 (0.00) |
| 5 | 2 (1.60) | 2 (1.57) |
| 6 | 0 (0.00) | 0 (0.00) |
| Age | 125 | 127 |
| n; mean (sd) | 27.81 (2.59) | 27.76 (2.45) |
| Specialty | ||
| Neuro/Neurosurgery/Surgery | 9 (7.32) | 14 (11.11) |
| Pathology | 4 (3.25) | 3 (2.38) |
| Dermatology | 4 (3.25) | 4 (3.17) |
| PM&R | 5 (4.07) | 6 (3.97) |
| Internal/Sleep/Rehab/Medicine | 48 (39.02) | 47 (37.30) |
| Anesthesiology | 11 (8.94) | 9 (7.14) |
| Family Medicine | 8 (6.50) | 8 (6.35) |
| Orthopedics | 4 (3.25) | 4 (3.17) |
| Otolaryngology/Maxillofacial | 7 (5.69) | 8 (6.35) |
| OB/GYN | 8 (6.50) | 7 (5.56) |
| Psych | 7 (5.69) | 6 (4.76) |
| ENT | 1 (0.81) | 1 (0.79) |
| Radiation Oncology | 1 (0.81) | 1 (0.79) |
| Ophthalmology | 6 (4.88) | 8 (6.35) |
Table 2.
Overall Observed Scores and Differences
| Pre | Post | |||||
|---|---|---|---|---|---|---|
| n | mean (std dev) | n | mean (std dev) | Estimated Change (95% CI) | p-value | |
| Knocking before entering patient's room | 127 | 1.37 (0.55) | 128 | 1.20 (0.40) | –0.18 (–0.26, −0.09) | 0.000 |
| Addressing a patient by his/her last name | 127 | 1.43 (0.66) | 129 | 1.20 (0.44) | –0.23 (–0.34, −0.13) | 0.000 |
| Acknowledging other people in the room | 127 | 1.40 (0.57) | 129 | 1.22 (0.41) | –0.18 (–0.28, −0.08) | 0.000 |
| Smiling and displaying good eye contact | 126 | 1.18 (0.39) | 129 | 1.11 (0.31) | –0.07 (–0.13, −0.01) | 0.034 |
| Sitting down to speak with a patient | 127 | 1.86 (0.91) | 129 | 1.46 (0.68) | –0.41 (–0.54, −0.28) | 0.000 |
| Introducing yourself as Dr. | 127 | 1.74 (0.92) | 129 | 1.33 (0.58) | –0.42 (–0.57, −0.27) | 0.000 |
| Informing the patient of your medical specialty | 127 | 1.72 (0.91) | 128 | 1.34 (0.62) | –0.39 (–0.52, −0.26) | 0.000 |
| Informing a patient of your role as either intern or resident | 127 | 2.09 (0.98) | 129 | 1.50 (0.71) | –0.58 (–0.73, −0.44) | 0.000 |
| Complimenting other physicians or healthcare providers who take care of the patient | 127 | 2.24 (1.07) | 129 | 1.61 (0.79) | –0.63 (–0.79, −0.46) | 0.000 |
| Avoiding blaming or negative comments about other physicians or healthcare providers who take care of the patient | 126 | 1.40 (0.57) | 129 | 1.25 (0.47) | –0.15 (–0.25, −0.04) | 0.006 |
| Giving a patient an expected duration of the overall expected length of the patient's stay | 127 | 2.08 (0.89) | 129 | 1.43 (0.65) | –0.65 (–0.79, −0.50) | 0.000 |
| Explaining the approximate time duration for his/her procedure(s) | 117 | 1.89 (0.80) | 123 | 1.48 (0.59) | –0.41 (–0.57, −0.25) | 0.000 |
| Avoiding medical jargon when talking with a patient | 118 | 1.34 (0.54) | 123 | 1.17 (0.42) | –0.16 (–0.26, −0.06) | 0.001 |
| Discussing and explaining all treatment plans with patient | 118 | 1.36 (0.56) | 123 | 1.13 (0.36) | –0.22 (–0.31, −0.13) | 0.000 |
| Requesting patient's permission before starting an exam or procedure | 118 | 1.43 (0.61) | 123 | 1.22 (0.45) | –0.22 (–0.33, −0.10) | 0.000 |
| Asking a patient, “What question do you have for me?” | 118 | 1.31 (0.53) | 123 | 1.18 (0.41) | –0.12 (–0.20, −0.04) | 0.004 |
| Thanking a patient when ending your visit | 117 | 1.92 (1.02) | 123 | 1.54 (0.82) | –0.36 (–0.52, −0.20) | 0.000 |
| Acknowledge everyone in the room before leaving | 118 | 1.97 (0.92) | 123 | 1.53 (0.68) | –0.43 (–0.58, −0.28) | 0.000 |
In a comparison of male and female residents' valuation of communication behavior before and after training, there were two behaviors that showed significant differential change between males and females: sitting down to speak with a patient (p=0.021) and introducing oneself as Dr. ________ (p=0.005). With regard to sitting, females started with a lower pre score/higher valuation and had a smaller score change (1.62 and −0.25, respectively) than males, who started with a higher pre score/lower valuation and had a larger drop showing more improvement in their valuation score (2.1 and −0.55, respectively). A similar pattern is seen with the introduction question.
There was little difference by years of training with valuation scores; PGY2s had a greater valuation of asking a patient, “What questions do you have for me?” (p=0.01) after training, compared to trainees from other post-graduate years.
Table 3 shows surgical specialties had a significantly larger decrease in scores regarding asking a patient's permission before starting an exam or procedure (–0.44 vs −0.13, respectively, p=0.034), indicating that there was an increased valuation after training compared to nonsurgical specialties.
Table 3.
Observed Scores and Differences by Specialty
| Non-Surgical | Surgical | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||||
| n | mean (std dev) | n | mean (std dev) | Estimate Change (95% CI) | n | mean (std dev) | n | mean (std dev) | Estimate Change (95% CI) | p-value | |
| Knocking before entering patient's room | 87 | 1.34 (0.52) | 87 | 1.20 (0.40) | –0.15 (–0.23, −0.07) | 36 | 1.47 (0.61) | 38 | 1.21 (0.41) | –0.26 (–0.45, −0.07) | 0.292 |
| Addressing a patient by his/her last name | 87 | 1.43 (0.68) | 88 | 1.16 (0.40) | –0.27 (–0.38, −0.16) | 36 | 1.50 (0.65) | 38 | 1.29 (0.52) | –0.21 (–0.45, 0.03) | 0.687 |
| Acknowledging other people in the room | 87 | 1.34 (0.50) | 88 | 1.17 (0.38) | –0.17 (–0.28, −0.07) | 36 | 1.56 (0.69) | 38 | 1.34 (0.48) | –0.21 (–0.45, 0.03) | 0.792 |
| Smiling and displaying good eye contact | 86 | 1.16 (0.37) | 88 | 1.11 (0.32) | –0.04 (–0.12, 0.05) | 36 | 1.25 (0.44) | 38 | 1.11 (0.31) | –0.15 (–0.26, −0.05) | 0.087 |
| Sitting down to speak with a patient | 87 | 1.83 (0.90) | 88 | 1.43 (0.69) | –0.39 (–0.53, −0.24) | 36 | 1.97 (0.97) | 38 | 1.55 (0.69) | –0.47 (–0.75, −0.19) | 0.607 |
| Introducing yourself as Dr. | 87 | 1.57 (0.79) | 88 | 1.23 (0.52) | –0.35 (–0.50, −0.20) | 36 | 2.14 (1.05) | 38 | 1.55 (0.65) | –0.59 (–0.94, −0.24) | 0.210 |
| Informing the patient of your medical specialty | 87 | 1.67 (0.90) | 88 | 1.36 (0.66) | –0.32 (–0.47, −0.17) | 36 | 1.83 (0.91) | 37 | 1.30 (0.52) | –0.53 (–0.78, −0.29) | 0.140 |
| Informing a patient of your role as eitherintern or resident | 87 | 2.15 (1.02) | 88 | 1.53 (0.74) | –0.61 (–0.78, −0.45) | 36 | 1.97 (0.88) | 38 | 1.42 (0.64) | –0.53 (–0.83, −0.22) | 0.625 |
| Complimenting other physicians or healthcare providers who take care of the patient | 87 | 2.29 (1.07) | 88 | 1.64 (0.83) | –0.64 (–0.85, −0.43) | 36 | 2.17 (1.08) | 38 | 1.58 (0.72) | –0.60 (–0.88, −0.31) | 0.804 |
| Avoiding blaming or negative comments about other physicians or healthcare providers who take care of the patient | 87 | 1.43 (0.60) | 88 | 1.24 (0.43) | –0.19 (–0.31, −0.07) | 35 | 1.34 (0.48) | 38 | 1.29 (0.57) | –0.05 (–0.26, 0.16) | 0.272 |
| Giving a patient an expected duration of the overall expected length of the patient's stay | 87 | 2.09 (0.86) | 88 | 1.40 (0.62) | –0.70 (–0.86, −0.54) | 36 | 2.08 (0.97) | 38 | 1.55 (0.72) | –0.52 (–0.81, −0.23) | 0.295 |
| Explaining the approximate time duration for his/her procedure(s) | 79 | 1.82 (0.81) | 85 | 1.47 (0.59) | –0.35 (–0.54, −0.16) | 35 | 2.06 (0.76) | 36 | 1.53 (0.61) | –0.52 (–0.82, −0.22) | 0.351 |
| Avoiding medical jargon when talking with a patient | 80 | 1.30 (0.51) | 85 | 1.13 (0.40) | –0.17 (–0.29, −0.05) | 35 | 1.40 (0.55) | 36 | 1.25 (0.44) | –0.14 (–0.32, 0.04) | 0.801 |
| Discussing and explaining all treatment plans with patient | 80 | 1.33 (0.55) | 85 | 1.14 (0.38) | –0.18 (–0.28, −0.09) | 35 | 1.40 (0.55) | 36 | 1.11 (0.32) | –0.30 (–0.48, −0.11) | 0.281 |
| Requesting patient's permission before starting an exam or procedure | 80 | 1.34 (0.53) | 85 | 1.21 (0.47) | –0.13 (–0.24, −0.02) | 35 | 1.66 (0.73) | 36 | 1.22 (0.42) | –0.44 (–0.71, −0.17) | 0.034 |
| Asking a patient, “What questions do you have for me?” | 80 | 1.31 (0.54) | 85 | 1.19 (0.42) | –0.12 (–0.22, −0.02) | 35 | 1.29 (0.52) | 36 | 1.17 (0.38) | –0.11 (–0.27, 0.05) | 0.892 |
| Thanking a patient when ending your visit | 80 | 1.90 (1.05) | 85 | 1.51 (0.84) | –0.37 (–0.55, −0.19) | 34 | 2.00 (0.95) | 36 | 1.67 (0.79) | –0.33 (–0.66, 0.00) | 0.860 |
| Acknowledge everyone in the room before leaving | 80 | 1.91 (0.93) | 85 | 1.46 (0.63) | –0.45 (–0.61, −0.28) | 35 | 2.14 (0.91) | 36 | 1.69 (0.79) | –0.43 (–0.77, −0.10) | 0.935 |
Table 4 presents changes in both HCAHPS and Press Ganey scores preceding and following communication skills training and reflects a positive increase in patient satisfaction. The HCAHPS doctor communication domain increased from 79.9 to 80.8. The Press Ganey doctor communication domain increased from 87.8 to 88.6 (from 52nd to 64th national percentile). These domains trended in an upward direction from before to after training.
Table 4.
Integrated HCAHPS/PG Survey (all specialties)
| April – June 2013* | July – September 2013** | October – December 2013** | January – March 2014*** | |
|---|---|---|---|---|
| Domain: Item | Percent of always | |||
| HCAHPS Doctor Communication Domain: | 79.9 | 80.4 | 80.1 | 80.8 |
| During this hospital stay, how often did doctors treat you with courtesy and respect? | 85.7 | 87.3 | 86.3 | 87.1 |
| During this hospital stay, how often did doctors listen carefully to you? | 78.7 | 78 | 78.4 | 78.8 |
| During this hospital stay, how often did doctors explain things in a way you could understand? | 75.3 | 75.9 | 75.7 | 76.5 |
| PG Doctor Communication Domain: | 87.8 (52nd)† | 87.8 (52nd)† | 88.2 (53rd)† | 88.6 (64th)† |
| The doctor spent enough time with me | 82.8 (42nd) | 82.9 (42nd) | 83.3 (42nd) | 83.9 (54th) |
| The doctor demonstrated interest in my questions and concerns | 87 (49th) | 87.1 (49th) | 87.4 (50th) | 87.8 (59th) |
| The doctor made sure I was well-informed about my care | 86.4 (49th) | 86.4 (49th) | 86.9 (52nd) | 87.4 (63rd) |
| The doctor was polite and friendly | 90.3 (53rd) | 90.5 (53rd) | 90.7 (52nd) | 91.1 (63rd) |
| Overall, the doctor was experienced and skilled | 93.4 (69th) | 93.2 (69th) | 93.4 (66th) | 93.8 (78th) |
Pre-training;
Training September – October;
Post-Training
Percent of always response/national percentile
HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) PG (Press Ganey)
Discussion
Across specialties, medical residents highly value all aspects of communication and interpersonal skills with patients.9,12 Teaching communication skills, therefore, falls on receptive ears and is congruent with already established values. According to the Kalamazoo report from 2002, residents' values mirror attending physicians' valuation of these skills.17 Our use of attending physicians at the training may have reinforced the valuation of these skills. The recent focus on physician communication skills appears to resonate with already held values, as training moved all scores to a more positive valuation.
Communication skills are also correlated with patient care and safety. Miscommunication between physicians and patients is the most common cause of medical errors and is responsible for more than 60 percent of sentinel events that lead to increased mortality or injury among hospitalized patients.18–19 Communication skills contribute to patient satisfaction as measured by patients' survey ratings under value-based purchasing and whether patients choose specific health care providers.12 With revenue dollars now at risk, hospitals are increasingly incentivized to train their physicians to provide excellent communication with patients. Research has shown that patient perceptions and values can be influenced by physician behavior, e.g., a patient significantly overestimates the time a physician spends with her when the physician is seated.20 Training residents with these communication skills contributes to the likelihood that behavioral changes will be made. If these skills are valued, there is a higher opportunity for the skills to be utilized and/or retained.21 As seen in the psychological theory, Bandura has shown that behavior will change with self-reinforcement.22 Another theory takes this further and suggests that the evaluation of consequences also leads to behavior change.23 Being instructed to change a behavior that is not perceived to be of value is unlikely to be as effective as making a behavior change because the resident intrinsically values that change.
In 1999 and 2002, two conferences brought attention to the high valuation of communication skills and identified the need for better education and evaluation of medical professionals.17 Five ways were identified to evaluate communication and interpersonal skills. In a study of 33 surgical residents and 16 attending surgeons, participants rated communication as very important in the successful care of patients despite attending surgeons reporting that they did not give feedback on communication skills.24 Providing specific skills training can, therefore, improve this proficiency and can be effectively measured. Absent from these studies and conferences was an exploration of whether these skills are equally valued by training physicians.
Training physicians involves education about value-based purchasing, which necessitates the understanding of how communication and interpersonal skills are an integral part of patient care. Resident physicians bring their own independent valuation of these skills and, if training increases this valuation, the opportunity for good communication skills and greater patient satisfaction is enhanced. This increased satisfaction improved hospital value-based purchasing scores and often can improve quality, safety and patient satisfaction.15 When put into practice, patient-centered communication constitutes an important indicator of quality care and contributes to a better patient experience and improved health outcomes.25–27
Physicians come to AIDET™ training with different levels of valuation of these skills despite all indications that these skills are of overall value. For example, initially, women valued a formal introduction prior to training more than men. During the course of their training, female physicians voiced having had the experience of being mistaken for a nurse, some other health professional, or support staff. This may predispose women to valuing a formal introduction and clarification of their role for patients. Most sessions had meaningful dialogue regarding the role of transitioning from a medical student to a PGY1/2 physician, as well as the use of “doctor” versus an introduction using the resident's first name. Feedback from this training led to a rollout of “doctor” identification tags for all physicians.
Female physicians valued sitting down with patients more than their male colleagues before training (as had been seen in previous research).28 Although physicians appear to value sitting down, studies have shown few actually do sit down and, in one study, less than 10 percent actually sat with patients when being observed.29 Other research has shown that sitting with a patient can have a significant positive impact on patient satisfaction and provider-patient rapport.30
AIDET™ training teaches the skills of a formal introduction and reinforces the value of role clarification so that patients understand clearly who their physicians are. Our training also taught the value of sitting down to our residents. Physicians who initially did not value sitting as highly as others were the ones to see the most change in that value after training. The finding that surgical house staff increased their valuation of requesting a patient's permission before starting an exam or procedure may reflect that they are in a procedural specialty. Increased differences between medical and surgical specialties might have been found with more senior house staff who have better consolidated their professional clinical specialty identities.
The communication skills that were reported to be more highly valued after training may have contributed to the increase of inpatient satisfaction scores as measured by HCAHPS and Press Ganey inpatient satisfaction survey. Although there is no way to be certain that the AIDET™ training was directly responsible for the increase in patient satisfaction scores, this training of all house staff was the only hospitalwide intervention that was made with physicians during this time period.
There are several limitations to this study. Although resident surveys were anonymous, there were many attendings who were involved in the training. The desire to please those attendings by demonstrating increased values for the skills taught may have masked actual valuation of those skills. The training emphasized that these skills were valued by the hospital leadership and faculty, and this also may have had a biasing effect rather than a personal intrinsic change in valuation. The study could benefit from follow-up with the residents to see whether the valuation of the communication and interpersonal skills translated to behavioral changes with the implementation of these skills. Follow-up would create an opportunity to see whether the valuation of communication skills was sustained over time. Another limitation of the study was due to the choice of statistical analysis which involved assumptions that could contribute to differences in sensitivity analyses.
The challenge of teaching communication involves both how to train and how to measure these skills. Future research must focus on what specific skills are being taught and measured, and if the resident also values the skill being taught. Focusing on the value of the skill, along with the specific skill, promises to be an important part of changing that behavior and fulfills the ACGME core competency for developing communication and interpersonal skills with patients. Self-evaluation of this kind, done with pre/post surveys and audience response systems also can be used as part of the required 360° resident evaluations.
Conclusions
Residents appear to intrinsically value communication skills, but training in communication and interpersonal skills, such as AIDET™, increases the perceived value of these skills. We believe that increased value contributes to the implementation of these skills. Gender, specialty, and surgical versus nonsurgical specialty do not appear to play a major role in how residents view and value communication skills.
References
- 1.Hulsman RL Ros WJG Winnubst JAM Bensing JM. Teaching clinically experienced physicians communication skills. A review of evaluation studies. Medical Education 1999; 33:655–668. [DOI] [PubMed] [Google Scholar]
- 2.Peck BM Ubel PA Roter DL Goold Dorr S Asch DA Jeffreys AS Mtstat Grambow SC Tulsky JA. Do unmet expectations for specific tests, referrals and new medications reduce patients' satisfaction? J Gen Intern Med. 2004;19(11):1080–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bowling A Rowe G Lambert N Waddington M Mahtani KR Kenten C Howe A Francus SA. The measurement of patients' expectations for health care: A review and psychometric testing of a measure of patients' expectations. Health Technol Assess. 2012;16(30):i–xii, 1–509. [DOI] [PubMed] [Google Scholar]
- 4.Stempniak M. The patient experience: Taking it to the next level. Press Ganey; 2013. [PubMed] [Google Scholar]
- 5.Porter M Lee T. The strategy that will fix health care. Harvard Business Review. 2013;91(10):50–70.23898735 [Google Scholar]
- 6.Hagerty RG Butow PN Ellis PM Dimitry S Tattersall MH. Communicating prognosis in cancer care: A systematic review of the literature. Ann Oncol. 2005;16(7):1005–1053. [DOI] [PubMed] [Google Scholar]
- 7.Turnberg L. Improving communication between doctors and patients. London: Royal College of Physicians; 1997. [PMC free article] [PubMed] [Google Scholar]
- 8.Jha AK Orav EJ Zheng J Epstein AM. Patients' perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–1931. [DOI] [PubMed] [Google Scholar]
- 9.Harmon G Lefante J Krousel-Wood M. Overcoming barriers: The role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310–315. [DOI] [PubMed] [Google Scholar]
- 10.Hojat M Louis DZ Markham FW Wender R Rabinowitz C Gonnella JS. Physicians' empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–364. [DOI] [PubMed] [Google Scholar]
- 11.Cegala DJ Broz Lenzmeier S. Physician communication skills training: A review of theoretical backgrounds, objectives and skills. Med Educ. 2002. Nov;36(11):1004–16. [DOI] [PubMed] [Google Scholar]
- 12.Gulbrandsen P Jensen BF Finset A Blanch-Hartigan D. Long-term effect of communication training on the relationship between physicians' self-efficacy and performance. Patient Educ Couns. 2013. May;91(2):180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krupat E Frankel R Stein T Irish J. The Four Habits Coding Scheme: Validation of an instrument to assess clinicians' communication behavior. Patient Educ Couns. 2006. Jul;62(1):38–45. [DOI] [PubMed] [Google Scholar]
- 14.Katona A Kunkel E Arfaa J Weinstein S Skidmore C. Methodology for Delivering Feedback to Neurology House Staff on Communication Skills Using AIDET™ (Acknowledge, Introduce, Duration, Explanation, Thank You). Neurology, 2014; 82 (10): Supplement P1328. [Google Scholar]
- 15.Studer Q Robinson B Cook K. The HCAHPS handbook: Hardwire your hospital for success. Gulf Breeze, FL: Fire Starter Publishing; 2010. [Google Scholar]
- 16.Studer Q. Results that Last: Hardwiring behaviors that will Take Your Company to the Top. John Wiley and Sons, Inc.: Hoboken, NJ; 285–292. [Google Scholar]
- 17.Duffy FD Gordon GH Whelan G Cole-Kelly K Frankel R, PhD Buffton N Lofton S Wallace M Goode L Langdon L, All Participants in the American Academy on Physician and Patient's Conferenceon Education and Evaluation of Competence in Communication and Interpersonal Skills. Assessing Competence in Communication and Interpersonal Skills: The Kalamazoo II Report. Academic Medicine 2004; 79(6): 495–707. [DOI] [PubMed] [Google Scholar]
- 18.Baptist Leadership Group. The HCAHPS imperative for creating a patient-centered experience. Baptist Leadership Group; 2001. [Google Scholar]
- 19.National Research Council. Rapporteur roundtable on health literacy. In: Measures of health literacy: Workshop summary. Washington DC: The National Academies Press; 2009:100–120. [Google Scholar]
- 20.Johnson RL Sadosty AT Weaver AL Goyal DG. To sit or not to sit? Annals Emergency Med 2008. 51(2):188–193e2. [DOI] [PubMed] [Google Scholar]
- 21.Simon KM. Self-evaluation reactions: The role of personal valuation in the activity. Cognitive Therapy & Research 1979;3(1):111–116. [Google Scholar]
- 22.Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes 1991. 50(2): 248–287. [Google Scholar]
- 23.Masters John C Santrock John W. Studies in the self-regulation of behavior: Effects of contingent cognitive and affective events. Developmental Psychology 1976. Vol 12(4): 334–348. [Google Scholar]
- 24.Hutul OA Carpenter RO Tarpley JL Lomis KD. Missed opportunities: A descriptive assessment of teaching and attitudes regarding communication skills in a surgical residency. Curr Surg 2006; 63(6): 401–409. [DOI] [PubMed] [Google Scholar]
- 25.Arora NK Weaver KE Clayman ML Oakley-Girvan I Potosky AL. Physicians' decision- making style and psychosocial outcomes among cancer survivors. Patient Educ Couns. 2009;77(3):404–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong LM Visser MR Lammes FB van Der Velden J Kuenen BC de Haes JC. Effect of providing cancer patients with the audiotaped initial consultation on satisfaction, recall, and quality of life: A randomized, double-blind study. J Clin Oncol. 2000;18(16):3052–3060. [DOI] [PubMed] [Google Scholar]
- 27.Street RL Jr Makoul G Arora NK Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. [DOI] [PubMed] [Google Scholar]
- 28.Tackett S Tad-Y D Rios R Kisuule F Wright S. Appraising the Practice of Etiquette-Based Medicine in the Inpatient Setting. Gen Intern Med. 2013. Jul;28(7):908–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Block L Hutzler L Habicht R Wu AW Desai SV Silva Novello K Niessen T Oliver N Feldman L. Do internal medicine interns practice etiquette-based communication? A critical look at the inpatient encounter. J Hosp Med 2013;8(11):631–4. [DOI] [PubMed] [Google Scholar]
- 30.Swayden KJ Anderson KK Connelly LM Moran JS McMachon JK Arnold PM. Effect of sitting vs. standing on perception of provider time at bedside: A pilot study. Patient Educ Couns. 2012. Feb;86(2):166–71. [DOI] [PubMed] [Google Scholar]


