Abstract
Introduction:
Patient satisfaction is of increasing importance in the delivery of quality healthcare and may influence provider reimbursement. The purpose of this study is to examine how patient wait time relates to their level of satisfaction and likelihood to recommend an orthopedic clinic to others.
Methods:
A retrospective analysis was performed on standardized new patient survey data collected at a single orthopedic clinic from June 2011 through October 2014.
Results:
A total of 3125 and 3151 responses were collected for satisfaction and likelihood to recommend the practice. The mean wait time was 27.3 ± 11.3 minutes. The likelihood of obtaining an “excellent” (odds ratio [OR]: 0.86, P = .01081) or “excellent/very good” (OR: 0.82, P = .0199) satisfaction demonstrated significant correlation with wait time in 15-minute intervals. The likelihood of obtaining an “agree” (OR: 0.9, P = .10575) and “strongly agree/agree” (OR: 0.85, P = .139) response to recommend the practice demonstrated no correlation during the same interval.
Conclusion:
Minimizing wait times in the orthopedic clinic may improve patient satisfaction but may not affect their likelihood of recommending the practice to others.
Keywords: patient satisfaction, outpatient clinic, orthopedics
Introduction
In today’s competitive market, patient satisfaction has become a topic of interest to both healthcare providers and third-party payers. In turn, maximizing a patient’s satisfaction has received more attention in the delivery of healthcare than ever before. Not only can it play a significant role in developing and maintaining a practice but it also serves as a potential means of determining how a provider is reimbursed for their services. Commonly cited factors affecting patient satisfaction in the literature include timely access to appointments, provider–patient relationships, academic versus private practice setting, overall wait times, and time spent with providers (1 –4). Several studies have shown a correlation between reduction in patient wait times and increased patient satisfaction in the outpatient clinic (5,6). However, there have been reports that show no such correlation (7,8), and rather the amount of time the provider spends with the patient may be a better predictor of patient satisfaction. Other investigators have found no significant correlation in patient satisfaction in the academic setting versus the nonacademic setting but have suggested that an academic setting is more likely to be recommended (1). To date, there have been no studies investigating the correlation between patient wait time and satisfaction specifically in the outpatient orthopedic clinic. We sought to determine whether such a correlation exists and, perhaps for a more practical application, assess its influence on the likelihood a patient may recommend the practice to their peers based on their experience.
Methods
We performed a retrospective analysis of cross-sectional data that are routinely collected for all patients in the outpatient orthopedic clinic at a single site of an institution. No specific patient identifiers were used during the study, and the United States Health Insurance Portability and Accountability Act regulations were followed throughout. Institutional review board approval was obtained for this study. All new patients at the senior author’s practice are asked to complete an electronic patient satisfaction survey at the conclusion of their visit. This information is subsequently stored in an Outcomes Based Electronic Research Database (OBERD), which can be evaluated by surgeon, clinic site, and time period. The survey questions evaluated in this study include:
Please rate your overall level of satisfaction with your Rothman Institute experience. Responses include excellent, very good, good, fair, and poor.
Based on my experience, I would recommend the Rothman Institute to my family, friends, and coworkers. Responses include strongly agree, agree, neither agree or disagree, disagree, and strongly disagree.
These questions were chosen as indicators of overall patient and practical satisfaction, that is, likelihood to recommend the practice. The OBERD database can be queried for satisfaction responses on a monthly time interval only.
Outpatient appointment time stamps are maintained in an electronic database, which include the scheduled appointment, patient arrival, and check-in, examination start, and departure times. For the purposes of this study, wait time was calculated using the time interval between the patient’s scheduled appointment and the time they entered the examination room. This study does not take into account time gained or lost for patients who arrive early or late for their appointments. Average wait time was calculated per month for each surgeon and compared to satisfaction results per month.
Wait time and patient satisfaction data were collected from June 2011, when the database began, until October 2014 in monthly intervals. The data used in this study represent those patient visits at 1 busy urban office location only and cover all orthopedic subspecialties. A single site was used in an effort to control for location, environment, and staff variability. Providers at the clinic include faculty only, although residents may assist some faculty in seeing patients. All providers at this urban office setting participate in the collected patient data. All new patients who submitted a completed survey during this time period were included in the study, whereas established patients were not. There were no exclusion criteria for new patients to the office who completed the satisfaction survey during the time period surveyed.
Average wait times per month from June 2011 until October 2014 for each provider were compared to satisfaction survey results for the corresponding months and provider. Results were compared on a monthly basis as proportion of satisfaction results versus average wait time for that month, as satisfaction data can only be queried on a monthly basis in the OBERD system. Satisfaction data were collected as a function of “positive results” for each question. For question 1, level of overall satisfaction and tendency of “excellent” responses and of “excellent or very good responses” were evaluated. For question 2, likelihood to recommend the practice and tendency of “strongly agree” and of “strongly agree or agree” responses were evaluated.
A statistician performed a general linear-mixed statistical model with regression analysis at the institution using months as a term to account for multiple surgeons. This analysis was performed with respect to positive results as described above for each of the evaluated questions and wait times per monthly interval. This model allowed for the evaluation of a “positive response” with respect to wait time regardless of any trends that may have occurred over the calendar year. P values less than .05 were considered significant.
Results
Data were collected from a total of 22 orthopedic surgeons across all subspecialties including spine, joint replacement, shoulder and elbow, sports medicine, hand surgery, foot and ankle, trauma, and orthopedic oncology. The mean wait time for all new patients for all providers at the center city clinic from June 2011 through October 2014 was 27.3 (standard deviation: 11.3) minutes. The average monthly wait time ranged from 5 to 77.38 minutes. A total of 3125 responses were reviewed from June 2011 through October 2014 for question 1 and a total of 3151 responses for question 2. Average new patient survey compliance per month during this period was 14.4%, with a range of 8% to 20%. A general linear-mixed model with regression analysis was used to analyze survey results and corresponding average wait time per month.
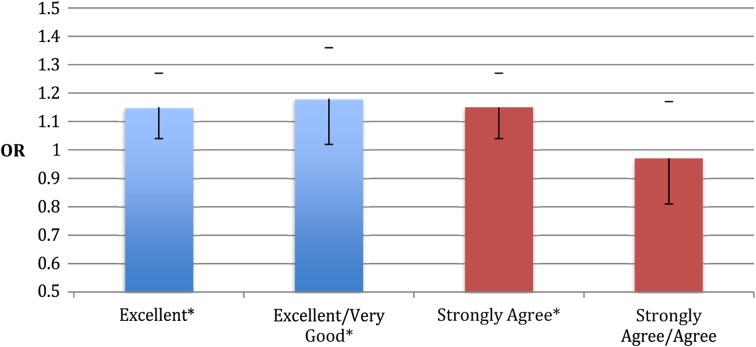
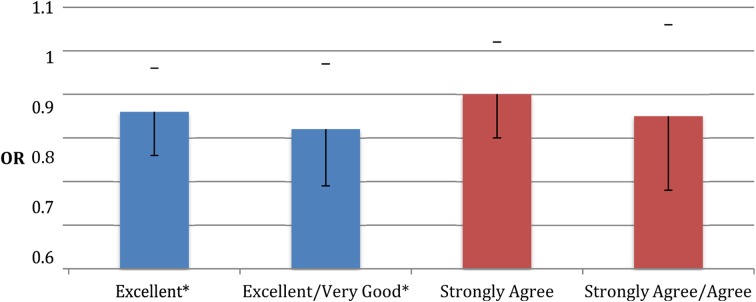
For question 1, there is a tendency for improved ratings over the time period surveyed. For excellent responses to the above question, odds ratio (OR) is 1.15 per year (95% confidence interval [CI]: 1.04-1.27; P = .00510). For an excellent or very good response, OR is 1.18 per year (95% CI: 1.02-1.36; P = .0239; Figure 1). Controlling for improvement over calendar time, ratings went down with increased wait times. For an excellent response, OR is 0.86 per 15 minutes of wait time (95% CI: 0.76-0.97; P = .01081). For an excellent or very good response, OR is 0.82 per 15 minutes of wait time (95% CI: 0.69-0.97; P = .0199; Table 1 and Figure 2).
Figure 1.
Odds ratio (OR) with corresponding 95% confidence interval (CI), as error bars, for obtaining an excellent and excellent or very good response to overall satisfaction per calendar year surveyed. Also shows OR with corresponding 95% CI, as error bars, for obtaining a strongly agree and strongly agree or agree response to likelihood to recommend the practice per calendar year surveyed. *P < .05 was considered significant.
Table 1.
Odds Ratio (OR), Confidence Interval (CI), and P Value for Receiving Excellent and Excellent or Very Good Responses to Overall Level of Satisfaction per Year Calendar Lime and per 15 Minutes of Wait Time.a
| Question 1 | OR | 95% CI | P Value |
|---|---|---|---|
| Calendar Year | |||
| Response | |||
| Excellent | 1.15 | 1.04-1.27 | .0051 |
| Excellent/very good | 1.18 | 1.02-1.36 | .0239 |
| 15-Minute Wait Time | |||
| Response | |||
| Excellent | 0.86 | 0.76-0.97 | .01081 |
| Excellent/very good | 0.82 | 0.69-0.97 | .0199 |
a P < .05 was considered significant.
Figure 2.
Odds ratio with corresponding 95% confidence interval (CI), as error bars, for excellent and excellent or very good response to overall satisfaction per 15 minutes of additional wait time. Also shows OR with corresponding 95% CI, as error bars, for strongly agree and strongly agree or agree responses to likelihood to recommend the practice per 15 minutes of additional wait time. *P < .05 was considered significant.
For question 2, there was a mixed association with ratings over the time period surveyed. For a strongly agree response, there is a significant improvement over calendar year (OR: 1.15 per year; 95% CI: 1.04-1.27; P = .00695). For a strongly agree or agree response, there was no association with calendar time (OR: 0.97 per calendar year; 95% CI: 0.81-1.17; P = .783; Figure 1). The association between wait time and likelihood to recommend the practice was also mixed. For a strongly agree response to question 2, there was a borderline association with wait time (OR: 0.90 per 15 minutes of wait time; 95% CI: 0.80-1.02; P = .10575). For a strongly agree or agree response, there was no association with wait time (OR: 0.85 per 15 minutes of wait time; 95% CI: 0.68-1.06; P = .139; Table 2 and Figure 2).
Table 2.
Odds Ratio (OR), Confidence Interval (CI), and P Value for Receiving Strongly Agree and Strongly Agree or Agree Responses for Likelihood to Recommend the Practice per Year Calendar Time and per 15 Minutes Wait Time.a
| Question 2 | OR | 95% CI | P Value |
|---|---|---|---|
| Calendar Year | |||
| Response | |||
| Strongly agree | 1.15 | 1.04-1.27 | .00695 |
| Strongly agree/agree | 0.97 | 0.81-1.17 | .783 |
| 15-Minute Wait Time | |||
| Response | OR | ||
| Strongly agree | 0.9 | 0.8-1.02 | .10575 |
| Strongly agree/agree | 0.85 | 0.68-1.06 | .139 |
a P < .05 was considered significant.
Discussion
In today’s changing healthcare market, patient satisfaction is of increasing importance in the delivery of quality healthcare. Insurance companies, including the Centers for Medicare and Medicaid Services, are placing a greater emphasis on patient satisfaction and are offering reimbursement incentives to hospitals based on the quality of care provided. Although largely subjective, patient satisfaction surveys play a critical role in the measurement of quality care (9). Surveys offer a means of quantifying patient satisfaction and the many factors that may contribute. Recognition of these factors is crucial to the delivery of quality healthcare.
Wait time is a commonly cited factor affecting patient satisfaction in the outpatient setting (2 –4,6,7,8,10). This study evaluated the average monthly wait times for 22 providers and the corresponding monthly satisfaction survey results for new patients in a single outpatient orthopedic clinic from June 2011 through October 2014. Specifically, we focused on the overall patient satisfaction by asking patients to rate their experience and their likelihood to recommend the practice.
For overall patient satisfaction, we found a significant reduction in both excellent and excellent/very good responses occurred for every 15 minutes of additional wait time experienced, as measured from the scheduled appointment time to the time the patient entered the examination room. On the contrary, we found that the likelihood for a patient to subsequently recommend the practice was not affected in this regard. Based on these data, we conclude that an additional 15 minutes of wait time may negatively affect a patient’s overall satisfaction with their experience but not necessarily their likelihood to recommend the practice to their peers. A possible explanation is that although the patient was less satisfied with their individual experience, they did not believe this to be indicative of the practice overall. On a similar note, decreased wait times did not necessarily translate into an increased likelihood of recommendation.
For overall patient satisfaction, there was a significant improvement in responses per year surveyed for both excellent and excellent or very good responses. For likelihood to recommend the practice, there was a significant improvement in strongly agree responses per year surveyed. These results may indicate an improvement in factors, other than wait time, that influence patient satisfaction and the likelihood to recommend the practice. These factors can only be hypothesized but may include improved patient–physician relationship, interaction with staff, ease of appointment scheduling, and recognition of the practice. Our data suggest that it is important for any practice to quantify their overall patient satisfaction and contributing factors so that they can continue to improve the quality of care they provide.
In analyzing our data, the following limitations should be considered: an average survey response rate of 14.4%, lack of direct association between an individual patient’s wait time and their survey response, and our measurement of wait time. Similar studies have shown a comparable patient survey response rate of 21% to 28% (1 –3), while some have been as high as 60% (7). Lasek et al evaluated the effects of nonresponse bias on patient survey results. They concluded the differences in overall satisfaction between responders and nonresponders may be relatively small and the nonresponder bias minimal (11). This study did not allow for direct comparison of wait times and corresponding survey results for an individual patient. Data used were evaluated from 2 separate databases containing routinely collected data: one of appointment time stamps and one of patient survey results. These databases were evaluated by new patients on a monthly basis for each individual provider, as patient satisfaction data are collected and stored on a per-month interval. This allowed for a monthly evaluation of average wait times and patient survey results for that month for each provider. We believe the strength of our survey lies in the volume of data and time period surveyed. Additionally, our data span numerous orthopedic specialties and therefore minimizes the potential influence of a specific subset of orthopedic patients who may generally be less satisfied as a group. Given these data, we are able to conclude that reducing average wait times correlates with increased patient satisfaction scores. Finally, we measured wait time from time of scheduled appointment to time in the examination room. This does not take into account patient’s arriving early or late and corresponding change in wait time experienced by the patient. We believed it was important to use a standardized scheduled appointment time as this is the time a patient can reasonably be expected to be seen by a physician regardless of their arrival time. Furthermore, we do not account for additional wait time in the examination room before physician evaluation and only considered wait time spent in the waiting room.
By reducing the average time spent in the waiting room by 15 minutes, you can expect to increase overall patient satisfaction. We acknowledge that there are likely several other factors that contribute to patient satisfaction that were not evaluated. Further investigation is necessary to determine other factors affecting patient satisfaction. This study suggests a strong correlation between patient wait times and overall satisfaction in the outpatient orthopedic clinic.
Author Biographies
Tyler M Kreitz, MD, is an Orthopaedic Surgery Resident at Thomas Jefferson University Hospital.
Brian S Winters, MD, is a board certified Orthopaedic Surgeon and Foot and Ankle Specialist at the Rothman Institute.
David I Pedowitz, MD, is a board certified Orthopaedic Surgeon and Foot and Ankle Specialist at the Rothman Institute.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Boss EF, Thompson RE. Patient satisfaction in otolaryngology: can academic institutions compete? Laryngoscope. 2012;122(5):1000–9. [DOI] [PubMed] [Google Scholar]
- 2. Famiglietti RM, Neal EC, Edwards TJ, Allen PK, Buchholz TA. Determinants of patient satisfaction during receipt of radiation therapy. Int J Radiat Oncol Biol Phys. 2013;87(1):148–52. [DOI] [PubMed] [Google Scholar]
- 3. McMullen M, Netland PA. Wait time as a driver of overall patient satisfaction in an ophthalmology clinic. Clin Ophthalmol. 2013;7:1655–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Prentice JC, Davies ML, Pizer SD. Which outpatient wait-time measures are related to patient satisfaction? Am J Med Qual. 2014;29(3):227–35. [DOI] [PubMed] [Google Scholar]
- 5. Billing K, Newland H, Selva D. Improving patient satisfaction through information provision. Clin Experiment Ophthalmol. 2007;35(5):439–47. [DOI] [PubMed] [Google Scholar]
- 6. Zopf D, Joseph AW, Thorne MC. Patient and family satisfaction in a pediatric otolaryngology clinic. Int J Pediatr Otorhinolaryngol. 2012;76(9):1339–42. [DOI] [PubMed] [Google Scholar]
- 7. Dang BN, Westbrook RA, Rodriguez-Barradas MC, Giordano TP. Identifying drivers of overall satisfaction in patients receiving HIV primary care: a cross-sectional study. PLoS One. 2012;7(8):e42980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trentman TL, Cornidez EG, Wilshusen LL, Chang YH, Seamans DP, Rosenfeld DM, et al. Patient satisfaction in an academic chronic pain clinic. Pain Pract. 2013;13(5):372–9. [DOI] [PubMed] [Google Scholar]
- 9. Hospital Inpatient Value-Based Purchasing Program. Centers for Medicare & Medicaid Services web site; 2011. Retrieved from: http://www.gpo.gov/fdsys/pkg/FR-2011-05- 06/pdf/2011-10568.pdf. Accessed March 16, 2014.
- 10. Anderson RT, Camacho FT, Balkrishnan R. Willing to wait? The influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lasek RJ, Barkley W, Harper DL, Rosenthal GE. An evaluation of the impact of nonresponse bias on patient satisfaction surveys. Med Care. 1997;35(6): 646–52. [DOI] [PubMed] [Google Scholar]