Abstract
The Proportional Responsibility for Integrated Metrics by Encounter (PRIME) model is a novel means of allocating patient experience scores based on the proportion of each physician's involvement in care. Secondary analysis was performed on Hospital Consumer Assessment of Healthcare Providers and Systems surveys from a tertiary care academic institution. The PRIME model was used to calculate specialty-level scores based on encounters during a hospitalization. Standard and PRIME scores for services with the most inpatient encounters were calculated. Hospital medicine had the most discharges and encounters. The standard model generated a score of 74.6, while the PRIME model yielded a score of 74.9. The standard model could not generate a score for anesthesiology due to the lack of returned surveys, but the PRIME model yielded a score of 84.2. The PRIME model provides a more equitable method for distributing satisfaction scores and can generate scores for specialties that the standard model cannot.
Keywords: HCAHPS, patient- and family-centered care, patient experience, patient satisfaction, value-based purchasing
Introduction
Patient- and family-centered care is increasingly being recognized as the approach to health care in the 21st century (1 –9). This national trend is affording patients and families a stronger voice in the care they receive. Value-based purchasing (VBP), the outcomes-focused reimbursement model implemented by the Centers for Medicare and Medicaid Services, has underscored the importance of this paradigm by financially incentivizing health care systems to optimize the patient experience (10). For fiscal years 2013 through 2015, the patient experience of care domain comprised 30% of the earnable VBP dollars (11 –13).
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey is the first standardized tool used nationally to assess patients’ perceptions of hospital care, enabling comparison of health care institutions (14). These data are now being publically reported (15). The VBP payment is based on institution-level scores, but it is difficult for organizations to enact targeted improvements without more detailed data. Some institutions have already attempted to assign survey scores at the clinical service level, often based on an individual clinician such as the discharging physician. While this and similar methodologies provide more granular data, the inherent limitation is that one survey score is assigned to only one service. Consulting services are neither given credit nor held accountable for their contributions to patient care and patient experience.
The purpose of this study was to develop an equitable paradigm to provide meaningful satisfaction data to all clinical services that contribute to a patient’s care. We refer to this as the Proportional Responsibility for Integrated Metrics by Encounter (PRIME) model. As the name implies, this model distributes scores in proportion to the number of patient–physician interactions during the hospitalization. This is accomplished by treating every patient–physician interaction during a hospitalization as a single encounter. A weighted score can then be calculated for every clinical service based on individual physician contributions to each patient’s care.
Methods
This study was conducted at an 830-bed, tertiary care academic medical center. The HCAHPS survey data from October 1, 2012, through September 30, 2013, were evaluated for discharged inpatients of age 19 years and older, reflecting our institution’s general definition of an adult versus pediatric patient. Only attending physician data were included. The medical staff office credentialing database was used to assign each physician to a clinical specialty. The system only allows a physician to be assigned to one specialty, so for those who practice in more than one, designation was done based on feedback from department chairs as to the physician’s principal clinical service. This study was approved by our institution’s research subjects review board.
The 3 standard questions listed under the Your Care From Doctors section of the HCAHPS survey were included in this study:
During this hospital stay, how often did doctors treat you with courtesy and respect?
During this hospital stay, how often did doctors listen carefully to you?
During this hospital stay, how often did doctors explain things in a way you could understand? (16).
Patients were given 4 options to choose from for each question: never, sometimes, usually, or always. Using the “top-box” approach, credit was only given for always responses; no credit was given for the other answers (15). Therefore, an individual survey could yield 1 of 4 possible composite scores: 100, 66.7, 33.3, or 0 if an always response was given for 3, 2, 1, or none of the questions, respectively.
Our survey vendor (Press Ganey®) provided returned satisfaction survey detail in a raw data file, listing every returned survey with patient answers to all questions. This included computation of select question categories and overall scores. Our organization’s standard process is to assign survey scores to clinical services based on the “attending of record.” This is determined by our health information management personnel using the discharging physician or service-specific algorithms.
The PRIME Model
An encounter was defined as any face-to-face interaction between a patient and a physician. Physician notes in the electronic medical record (EMR; Epic) were used as proxies for encounters. A physician was given credit for only 1 encounter if multiple notes were documented by him or her on the same calendar date and every encounter was weighted equally. Clinicians who utilize the EMR have a role assigned in the system, such as (attending) physician, resident, or registered nurse. This information is stored in a discrete field, which enabled the data to be filtered. Physician notes were extracted using Crystal reports and exported to SAS® (SAS Version-9.3) to be merged with hospital administrative and patient satisfaction data. Provider specialties were then assigned after which PRIME scores were calculated.
Table 1 shows sample calculations for the PRIME model. First, the number of encounters an individual attending physician had with each patient for whom he or she had at least 1 encounter was counted (column C). The total number of encounters that patient had with all attending physicians during that hospitalization was then tallied (column D). These two numbers were used to calculate what we termed patient equivalents (PEs), the ratio of the individual attending’s encounters to all attending encounters for that hospitalization (column E = C/D). This is analogous to the full-time equivalents (FTEs) used in the business world to account for a unit of work responsibility. Next, the earned points were calculated. The earned points are the composite HCAHPS score for the physician questions multiplied by the PE (column G = E × F). Total possible points per survey were then determined by multiplying the PE by 100. The attending physician’s earned points and total possible points were then calculated for all surveys for which he or she had at least 1 patient encounter. This process was repeated for each physician within the given clinical specialty. Finally, the PRIME score for the service was calculated by dividing the sum of the earned points by the sum of the total possible points then multiplying by 100, (Σ column G)/(Σ column H) × 100.
Table 1.
Sample Calculations Using the PRIME Model.
| A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|
| Returned Survey # | Physician | Individual Physician’s Encounters | Total Physician Encounters | Patient Equivalents (C/D) | HCAHPS Composite Score | Earned Points (E × F) | Total Possible Points |
| 1 | Dr A | 7 | 22 | 0.318 | 100.0 | 31.8 | 31.8 |
| 2 | Dr A | 4 | 8 | 0.500 | 66.7 | 33.3 | 50.0 |
| 3 | Dr A | 2 | 16 | 0.125 | 100.0 | 12.5 | 12.5 |
| 4 | Dr A | 1 | 7 | 0.143 | 33.3 | 4.8 | 14.3 |
| 5 | Dr A | 3 | 52 | 0.058 | 0.0 | 0.0 | 5.8 |
| 6 | Dr B | 1 | 3 | 0.333 | 100.0 | 33.3 | 33.3 |
| 7 | Dr B | 6 | 35 | 0.171 | 100.0 | 17.1 | 17.1 |
| 8 | Dr C | 2 | 10 | 0.200 | 66.7 | 13.3 | 20.0 |
| 9 | Dr C | 3 | 17 | 0.176 | 100.0 | 17.6 | 17.6 |
| 10 | Dr C | 5 | 6 | 0.833 | 100.0 | 83.3 | 83.3 |
| Total | 247.0 | 285.7 | |||||
| PRIME Score: | 86.5 | ||||||
Abbreviations: HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems; PRIME, Proportional Responsibility for Integrated Metrics by Encounter.
Results
A total of 31 491 patients were discharged during the study period. Hospital medicine, cardiology, emergency medicine, anesthesiology, and nephrology were identified as the 5 clinical services with the most encounters. The standard model was used to attribute discharges to clinical services based on the attending of record at the time of discharge. Table 2 shows a comparison of our institution’s standard model and the PRIME model for these services.
Table 2.
Comparison of Standard and PRIME Models for Services With the Highest Volume of Physician Encounters.
| Service | Standard Model | PRIME Model | ||||
|---|---|---|---|---|---|---|
| Discharges | Returned Surveys | Score | Encounters | Returned Surveys | Score | |
| Hospital medicine | 6565 | 692 | 74.6 | 51,528 | 979 | 74.9 |
| Cardiology | 2245 | 482 | 83.8 | 22,742 | 732 | 83.1 |
| Emergency Medicine | 769 | 95 | 83.8 | 22,620 | 2033 | 75.0 |
| Anesthesiology | 10 | 0 | N/A | 21,480 | 1932 | 84.2 |
| Nephrology | 322 | 49 | 72.8 | 21,188 | 239 | 72.9 |
Abbreviations: N/A, not available; PRIME, Proportional Responsibility for Integrated Metrics by Encounter.
Hospitalists had the most discharges and the most encounters, yielding standard and PRIME scores of 74.6 and 74.9, respectively. Cardiology had the second largest number of discharges, less than half as many as hospital medicine. Emergency medicine physicians discharged 769 inpatients and had the third largest number of encounters. Anesthesiologists discharged only 10 patients during the study period. No surveys were returned by these patients, so no standard score could be calculated. However, they had 21 480 inpatient encounters, the fourth highest in the institution, with 1932 returned surveys. This enabled a PRIME score of 84.2 to be calculated. Nephrology had the fifth largest volume of patients discharged from their service. Statistical comparison of the standard versus PRIME scores was not performed due to the markedly different methodologies used to derive them.
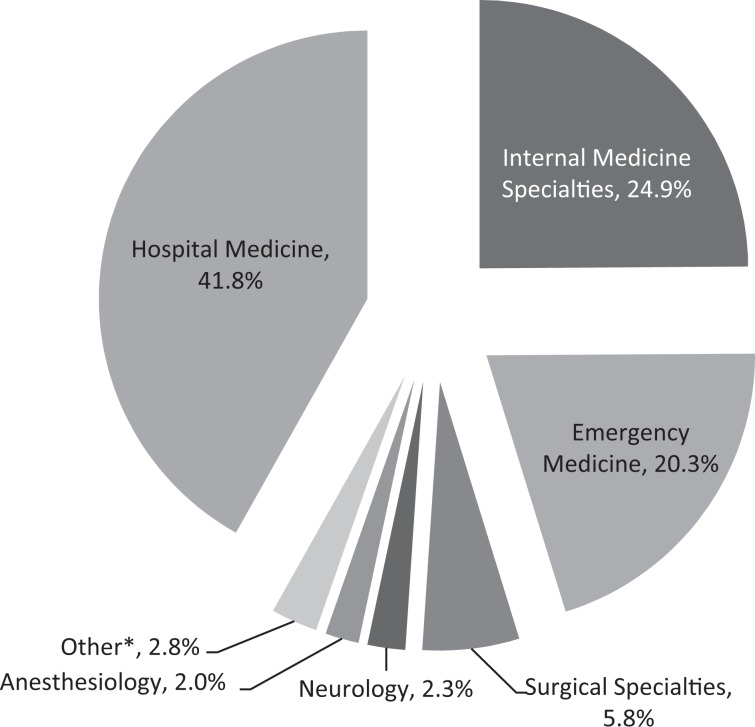
Figure 1 shows the breakdown of encounters by clinical service for inpatients discharged by hospital medicine. The 6565 patients discharged had a total of 34 977 encounters with an attending physician. Hospitalists comprised 14 637 (41.8%) of these encounters. Other internal medicine specialties contributed 8708 (24.9%) of the encounters, and emergency medicine physicians contributed 7112 (20.3%) of the encounters. Surgical specialties, neurology, and anesthesiology comprised 2037 (5.8%), 796 (2.3%), and 707 (2.0%) of the encounters, respectively. Eight hundred seventy-one (2.5%) encounters were distributed among a host of medical and surgical specialties; each individually contributed less than 1% of the total. An additional 109 (0.31%) of the encounters were not assigned to a specific service primarily due to physicians not having a specialty listed in the medical staff database.
Figure 1.
Proportion of physician encounters by specialty for patients discharged by a hospitalist (n = 34 977). *Other includes the following specialties: dermatology, family practice, obstetrics/gynecology, imaging sciences, pathology, pediatric specialties, psychiatry, and unassigned.
Discussion
The PRIME model provides an equitable methodology to allocate patient satisfaction scores. It holds every physician who contributes to the patient experience accountable for the care he or she provides. Unlike a standard model that assigns one survey score to one service based on an individual physician, the PRIME model enables the many physicians, including consultants, who share in patient care responsibility to be allotted an appropriate proportion of the survey score.
As shown in Figure 1, more than half of the encounters with patients discharged by a hospitalist were provided by other specialists. The standard model attributes the effect of these interactions to one clinical service, whereas the PRIME model distributes them across all specialties involved.
Our EMR allowed us to extract physician documentation based on role which could then be linked to survey and hospital administrative data. As more and more health care organizations transition to new, upgraded EMR systems, they should be able to implement similar processes to generate PRIME scores. Tracking individual patient–physician encounters through the EMR offers the ability to provide meaningful data to clinical services that discharge few or no patients but have important roles in patient care. These data can then be used to identify gaps and focus on performance improvement activities. For specialties such as anesthesiology that have a large number of patient encounters but discharge relatively few patients, a standard model offered no ability to determine a score. However, the PRIME model enabled a score to be calculated. This will become increasingly important, as health care reimbursement becomes more dependent on outcome measures and institutions seek to identify factors that influence patient experience scores (10,17 –20).
The PRIME model offers additional opportunities. It is not limited to use with the HCAHPS survey. It could be used with other patient experience survey tools. It is not limited to inpatient metrics. For example, it can be applied in the emergency department where “treat and release” patient satisfaction scores are often attributed solely to emergency medicine physicians. The PRIME model can provide data for the many consulting services who also contribute to patient care in this setting. It is not limited to attending physicians. Scores can be calculated for other health care providers, such as residents and nurse practitioners. Analogous data can be generated for nurses using HCAHPS questions under the Your Care From Nurses section. The PRIME model is not limited to satisfaction data. Quality metrics, such as hospital-acquired conditions, could also be proportionately allotted using this paradigm. The PRIME model could be used to assign scores to individual physicians, a step in the calculations, but would have to be done very judiciously. This is a further level of granularity for which the HCAHPS survey was not originally designed.
This study has limitations. The HCAHPS data were analyzed and reviewed for clinical services at 1 tertiary care academic institution. Our findings may not be generalizable to other settings. Interpretation of PRIME scores must be done with caution, as benchmarks are currently based on the standard model and may not be applicable. The PRIME model needs to be applied at other health care organizations to further assess its utility and to establish national benchmarks for comparison of clinical services across institutions. The PRIME scores need to be shared with physicians, incorporated into performance improvement activities, and tracked over time to assess the impact of having such service-specific data.
The service-level scores produced by the standard and PRIME models were derived from the same HCAHPS data but were generated by 2 distinctly different methodological approaches: single assignment versus weighted attribution, respectively. As such, they represent different measures. Statistical comparison therefore did not seem appropriate. Notes were used as proxies for encounters. A physician was only given credit for one encounter even if multiple notes were written on the same calendar date, and a physician might not have documented every patient encounter or cosigned each trainee’s note every day. This would result in a lower proportion of the overall experience attributed to him or her. All types of encounters were given equal weight, but some physician encounters may have more impact on the overall patient experience than others. For example, the initial encounter with the primary team or the final encounter on the day of discharge might have more of an influence on the overall patient experience than day 8 of a 2-week admission. The PRIME model did not account for the amount of time an attending spent with a patient. However, quantity does not necessarily equal quality. A patient may have a very positive experience during a brief encounter or a negative experience during a longer encounter.
Of the 769 inpatient discharges attributed to emergency medicine, 39 (5.1%) were discharged by a single physician who also worked on another clinical service. Because he could only be assigned to 1 specialty in our system, these discharges were ascribed to emergency medicine. Finally, our survey vendor only sent HCAHPS surveys to 50% of eligible discharged patients. However, every patient has an equal chance of receiving a survey, so sampling bias should be minimized.
Conclusion
The PRIME model enables patient satisfaction scores, and potentially other quality metrics, to be equitably distributed across all physicians involved in patient care. These data can be leveraged by health care organizations to help improve performance. The PRIME model promotes team-based care by holding each member of the team accountable for his or her role and influence on the overall patient experience. Everyone becomes responsible for his or her contribution to patient care, and every encounter counts.
Author Biographies
Michael S Leonard is the Associate Chief Quality Officer for the University of Rochester Medical Center. He is also the Chief Quality Officer and the Chief Experience Officer for its Golisano Children's Hospital. He is a practicing pediatric hospitalist and an associate professor of pediatrics and public health sciences.
Brenda Foster is a Data Analyst and Programmer in the University of Rochester Medical Center's Office of Clinical Practice Evaluation.
Eric A Biondi is the Performance Improvement Officer for the Golisano Children's Hospital at the University of Rochester Medical Center. He is a practicing pediatric hospitalist and an assistant professor of pediatrics.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Institute of Medicine. Crossing the Quality Chasm: A New Helath System for the 21st Century Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2. Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006;296(23):2848–51. [DOI] [PubMed] [Google Scholar]
- 3. Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1. [DOI] [PubMed] [Google Scholar]
- 4. Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit. Care Med. 2007;35(2):605–22. [DOI] [PubMed] [Google Scholar]
- 5. Committee on Hospital Care and Institute for Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404. [DOI] [PubMed] [Google Scholar]
- 6. Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006;141(1):86–92. [DOI] [PubMed] [Google Scholar]
- 7. Weinstein JN, Clay K, Morgan TS. Informed patient choice: patient-centered valuing of surgical risks and benefits. Health Aff. 2007;26(3):726–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. JABFM. 2011;24(3):229–39. [DOI] [PubMed] [Google Scholar]
- 9. Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff. 2010;29(8):1489–95. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Medicare & Medicaid Services. Frequently asked questions: Hospital value- based purchasing program; 2012. [cited 2014 Jun 11]. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/Downloads/FY-2013-Program-Frequently-Asked-Questions-about-Hospital-VBP-3-9-12.pdf.
- 11. Centers for Medicare & Medicaid Services. Open door forum: Hospital value-based purchasing. Fiscal year 2013 overview for beneficiaries, providers and stakeholders; 2011. [cited 2014 Jun 10]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/downloads/HospVBP_ODF_072711.pdf.
- 12. Centers for Medicare & Medicaid Services. National provider call: Hospital value-based purchasing. Fiscal year 2014 overview for beneficiaries, providers and stakeholders; 2012. [cited 2014 Jun 10]. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/Downloads/NPCSlides071112.pdf.
- 13. Centers for Medicare & Medicaid Services. National provider call: hospital value- based purchasing. Fiscal year 2015 overview for beneficiaries, providers and stakeholders; 2013. [cited 2014 Jun 10]. Available from: http://www.cms.gov/Outreach-andEducation/Outreach/NPC/Downloads/HospVBP_FY15_NPC_Final_03052013_508.pdf.
- 14. Centers for Medicare & Medicaid Services. CAHPS Hospital Survey (HCAHPS) Quality Assurance Guidelines Version 9.0 Baltimore, MD: Centers for Medicare & Medicaid Services; 2014. [Google Scholar]
- 15. Centers for Medicare & Medicaid Services. Hospital Compare. [cited 2014 Jun 9]. Available from: www.medicare.gov/hospitalcompare.
- 16. HCAHPS Survey; 2014. [cited 2014 Jun 10]. Available from: http://www.hcahpsonline.org/files/HCAHPS%20V9.0%20Appendix%20A%20%20Mail%20Survey%20Materials%20%28English%29%20March%202014.pdf.
- 17. Zusman EE. HCAHPS replaces Press Ganey survey as quality measure for patient hospital experience. Neurosurgery. 2012;71(2): N21–4. [DOI] [PubMed] [Google Scholar]
- 18. Stein SM, Day M, Karia R, Hutzler L, Bosco JA., 3rd Patients’ perceptions of care are associated with quality of hospital care: a survey of 4605 hospitals. Am J Med Qual. 2015;30(4):382–8. [DOI] [PubMed] [Google Scholar]
- 19. Anhang Price R, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tevis SE, Kennedy GD. Patient satisfaction: does surgical volume matter? J Surg Res. 2015;196(1):124–9. [DOI] [PMC free article] [PubMed] [Google Scholar]