Abstract
The prominence of reciprocal understanding in patient–doctor empathic engagement implies that patient perception of clinician’s empathy has an important role in the assessment of the patient–clinician relationship. In response to a need for an assessment tool to measure patient’s views of clinician empathy, we developed a brief (5-item) instrument, the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE). This review article reports evidence in support of the validity and reliability of the JSPPPE.
Keywords: empathy, patient perceptions, Jefferson Scale, patient outcomes, validity, reliability
Introduction
Empathy has been described as one of the most frequently mentioned humanistic components of patient care (1), a royal road to treatment, a symbol of healthcare at its best (2), and an important component of professionalism in medicine (3). Research shows that empathic engagement in patient care is beneficial to the patient (eg, compliance, positive clinical outcomes, and fewer complications) (4[pp.189-201],5,6) and also serves as a buffer against professional stress and burnout (7), thereby benefitting clinicians’ well-being (8 -10). Research findings also suggest that empathic orientation in medical students is associated with positive personal qualities that are conducive to relationship building (eg, popularity, sociability, teamwork, and self-esteem) (4[pp.151-167],11 –14). Conversely, empathy deficit is predictive of negative personal attributes that are detrimental to the quality of interpersonal relationships and well-being (eg, aggression, hostility, burnout, and exhaustion) (4[pp.151-167],11 –14).
Definition
Despite the consensus among health professions researchers about the importance of empathy in patient care, there is less unanimity about its definition. There has been an ongoing debate about the definition of empathy as being a cognitive or emotional attribute, a behavior or an attitude, or a combination of these and other qualities (4[pp.3-16,71-81]). We defined empathy in the context of patient care “as a predominantly cognitive (rather than an affective or emotional) attribute that involves an understanding (rather than feeling) of experiences, concerns, and perspectives of the patient, combined with a capacity to communicate this understanding, and an intention to help” (4[p.74]). We developed the original framework for this definition approximately a decade and half ago after a comprehensive review of the literature (15,16) and especially by careful consideration of the factors in empathic engagement in patient care that could contribute to patient outcomes. We deliberately chose specific terms in this definition (eg, cognitive vs affective or emotional; understanding vs feeling) to make a distinction between empathy and sympathy (or between cognitive [or clinical] empathy and affective [or emotional] empathy [which is synonymous with sympathy in our view]). Such a distinction in the context of patient care is necessary because we maintain that cognitive empathy (or clinical empathy) and affective empathy (or sympathy) have different consequences in clinical outcomes (4,17,18).
In our definition of empathy, a key feature of “communication of understanding” implies that reciprocity between the clinician and patient is important and suggests that patient perceptions of clinicians’ empathy should be taken into consideration as an important dimension of empathic engagement. This was confirmed in a study that showed patients’ perceptions of clinicians’ empathy yielded the highest correlations with clinical outcomes, followed by observers’ ratings of clinicians’ empathy and finally by clinicians’ self-reported empathy (19).
We described elsewhere that reciprocity in patient–doctor empathic engagement can evoke interpersonal attunement, which in turn can lead to psycho-socio-bio-neurological responses (20). At the psychosocial level, interpersonal attunement lays the foundation for a trusting relationship, leading to a more accurate diagnosis and greater compliance (4,20). At the bioneurological level, patient–clinician attunement, according to the “perception–action” coupling theory, can lead to synchronized exchanges, inducing internal (eg, activation of prosocial endogenous hormones and the mirror neuron system, heart rate synchronization, and galvanic skin response) and external changes (eg, vocal and nonverbal mimicry, facial expression, imitation, and posture mirroring). All mechanisms associated with reciprocal attunement can lead to optimal clinical outcomes (4[pp.202, 239-240], 20).
Measurement
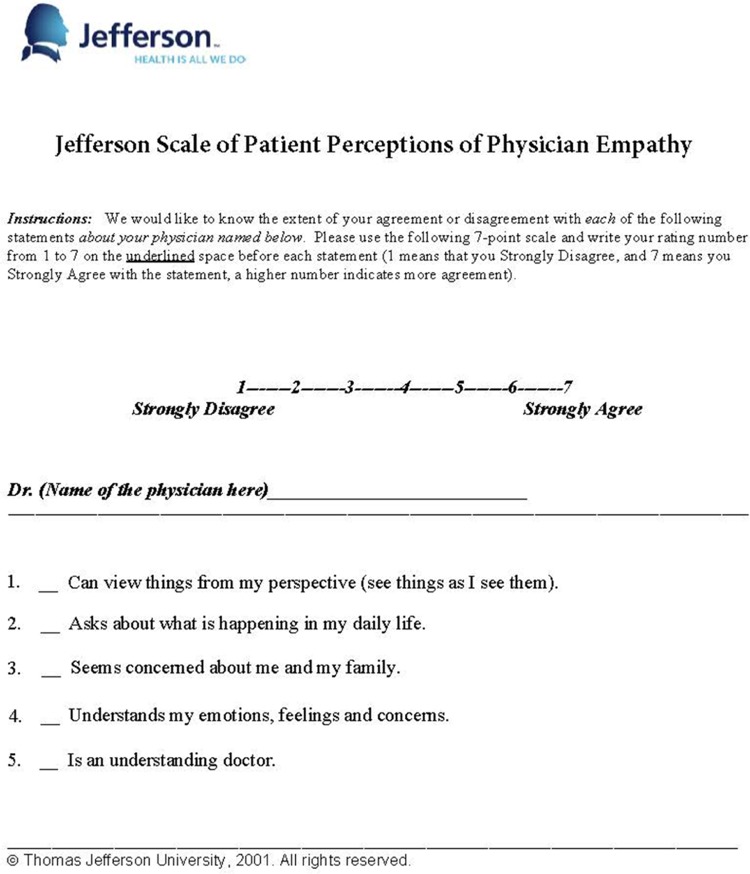
A valid and reliable instrument was needed for empirical research on patients’ perceptions of clinicians’ empathy. We developed a brief instrument (5-item), the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE), that can be completed by patients in a few minutes after a clinical encounter (see Appendix A). Each item is answered on a 7-point Likert-type scale (from Strongly Disagree = 1 to Strongly Agree = 7). The original intention was to measure patient perceptions of empathic engagement with a physician; however, the instrument can also be used to assess empathic engagement of other health-care providers such as nurses, dentists, pharmacists, clinical psychologists, clinical social workers, and so on. The JSPPPE has received broad national and international attention and has been translated into 10 languages (Danish, Finnish, French, German, Italian, Japanese, Persian or Farsi, Polish, Portuguese, and Romanian).
Face and Content Validity
The instrument was developed to be content specific and context relevant to assure its face and content validity. Face validity is determined by experts and nonexperts in judging the extent to which the items seem to be appropriate for measuring the concept purported to be measured (21). Content validity describes the extent to which a test measures a representative sample of subject matter relevant to the concept intended to be measured and is usually judged by experts (21). For example, a clinician’s concern regarding a patient/family is reflected in the following JSPPPE item: “[health-care provider’s name] seems concerned about me and my family.” Perspective taking, a major ingredient of empathy, is reflected in the following item: “[health-care provider’s name] can view things from my perspective.” The instrument was judged by nonexperts and experts to assure face validity and by experts only to confirm its content validity.
Item-Total Score Correlations
To examine the extent to which each item contributes to the total score, we examined corrected item-total score correlations of the JSPPPE (ie, correlations between each item score and the total score in which the corresponding item score was excluded). For example, in a study of 535 patients of family physicians (22) we found substantial item-total score correlations (>0.88). Similarly, large item-total score correlations (>0.77) were observed in another study with 225 patients (23).
Underlying Construct
Two exploratory factor-analytic studies showed that the JSPPPE is a unidimensional scale. For example, in an earlier study of 225 patient encounters (23), factor coefficients were greater than 0.72. In another study of 535 outpatients (22), factor coefficients were greater than 0.87. Thus, the scale seems to be saturated with only 1 underlying factor of “perceptions of clinician’s empathy.”
Criterion-Related Validity
Significant correlations between scores of a test and those of conceptually relevant measures are indicators of validity of the test. In a study of 225 patients (23), item scores as well as total scores of the JSPPPE yielded statistically significant correlations (P < .01) with scores on a patient rating form developed by the American Board of Internal Medicine (ABIM). The ABIM measure was developed as part of a comprehensive physician recertification process designed to assess doctor–patient relationships from patients’ perspectives (24). Correlations between item scores of the JSPPPE and scores of the ABIM patient rating form ranged from 0.70 to 0.54, with a median correlation of 0.67. Correlation between total score of the JSPPPE and total score of the ABIM patient rating form was 0.75 (23). These findings indicate the scores of the JSPPPE were significantly associated with patients’ evaluations of clinician’s communication skills, humanistic qualities, and professionalism as measured by the ABIM patient rating form (24).
Kane and colleagues (23) also found that scores of the JSPPPE were significantly (P < .01) correlated with patients’ ratings on the following selected items adapted from the Physicians’ Humanistic Behavior Questionnaire (25): “[this doctor] shows concerns for my feelings and needs, not just my physical status” (r = .86); “[this doctor] asks me how I feel about my problems” (r = .79); and “[this doctor] arranges for adequate privacy when examining or talking with me” (r = .61) (23). An inverse relationship was found between scores of the JSPPPE and responses to the following item: “[this doctor] is always in a hurry” (r = −.50). In addition, scores of the JSPPPE showed significant correlation with the following item selected from patients’ appraisal of physicians’ performance (26): “[this doctor] takes my wishes into account when making decisions” (r = .76) (23).
In a study of 535 patients (22), scores of the JSPPPE were substantially correlated with the following indicators of patient–clinician empathic relationships: “My doctor listens carefully to me” (r = .91); “My doctor really cares about me as a person” (r = .88); and indicators of interpersonal trust: “I would recommend my doctor to my family and friends” (r = .87); “I am satisfied that my doctor has been taking care of me” (r = .87); “My doctor spends sufficient time with me” (r = .80); and “I would like my doctor to be present in any medical emergency situation” (r = .77). Substantial correlation (r = .93) between scores of the JSPPPE and those of a validated measure of patient overall satisfaction with primary care physicians was also observed (27).
Also, higher scores on the JSPPPE were associated with patients’ compliance with their physicians’ recommendations (compliance rates >80%) for preventive care (eg, colonoscopy, mammogram for female, and the prostate-specific antigen (PSA) for male patients) (22). In a study of 248 third year medical students, scores on the JSPPPE assessed by 10 simulated patients in the objective structured clinical examination (OSCE) stations were significantly correlated (r = .87, P < .01) with the simulated patients’ global ratings of students’ empathy and support (28).
Reliability
The internal consistency (Cronbach coefficient α) of the JSPPPE was 0.48 in a study by Glaser and colleagues (29) and 0.58 in another study by Kane and colleagues (23). Although these reliability coefficients are relatively low, they can be considered satisfactory given that there are only 5 items in the instrument and insufficient visit time between patients and residents who were not primary care doctors. In a large scale study of 535 outpatients who were fairly familiar with their primary care doctors (defined as having at least 2 office visits with the doctor in the past 36 months and spending at least two-thirds of their total office visits with their identified primary care doctor), reliability coefficients were > 0.96 in male and female as well as younger and older patients (22). An alpha reliability coefficient of 0.91 was reported by Grosseman and colleagues (30) who used simulated patients in OSCE stations to assess empathy in internal medicine residents.
Correlation With Clinician’s Self-Reported Empathy
Associations between scores of the JSPPPE and self-reported clinician empathy have been examined in a few studies with mixed results. Clinicians’ self-reported empathy in these studies was measured by the Jefferson Scale of Empathy (JSE), a validated instrument developed specifically to measure clinicians’ empathy in the context of patient care (4,15,16). In one study with family medicine residents and their patients, a statistically significant correlation of 0.48 (P < .05) was found between scores of the JSPPPE and JSE (29). In another study of internal medicine residents and their patients (23), the correlation between residents’ scores on the JSE and patients’ scores on the JSPPPE did not reach conventional levels of statistical significance (r = .24, P = .22). It was observed in this study, however, that the scores of the JSPPPE for assessing residents were highly skewed toward the upper tail of the score distribution. Indeed, 78% of the residents received the highest possible scores on the JSPPPE, creating an extreme “ceiling effect” (23).
Berg and her colleagues (28) reported a statistically significant correlation of low magnitude (r = .19, P < .05) between medical students’ JSE scores and simulated patients’ ratings of students’ empathy (JSPPPE scores). In a study of 214 internal medicine and family medicine residents from 13 postgraduate programs at Drexel University College of Medicine using simulated patients in OSCE stations, negligible associations were observed between residents’ scores on the JSE and simulated patients’ ratings of residents’ empathy using the JSPPPE (30). One interpretation of the findings was that the poor associations between residents’ self-reported empathy and simulated patients’ assessments could be a contextual artifact due to the use of simulated versus real patients and short encounter times (30). It has been suggested that the link between patients’ perceptions and clinicians’ self-reported empathy could be strengthened by better training in how to communicate empathic understanding to patients (31). Empathic engagement requires a reasonable time to develop which cannot be fully formed in a short period of a single clinical encounter with simulated patients in OSCE situations (28,32).
In addition to the ability to gauge empathic communication, several other factors could explain the weak associations observed in the aforementioned studies. For example, empathic engagement in patient care is a complex phenomenon that may not be fully captured by simulated patients in simulated situations where the participants are unwilling to suspend disbelief because of unrealistic clinical encounters and artificial role playing games by both simulated patients and clinician in training (33,34). The OSCE in an “artificial environment” of clinical encounter often involves a “mutual pretense” that can influence trainees’ behavior as well as the simulated patients’ assessments of trainees (33,34). In addition, there are some confounding factors (eg, gender, race, and ethnicity) that may be at play. For example, students’ ethnic background (white vs Asian American) was found to influence simulated patients’ assessments of empathic engagement in clinical encounters in OSCE stations (33). In a multi-institutional study by Berg and colleagues (35), inconsistencies were observed between simulated patients’ assessments (using JSPPPE scores) and students’ self-reported empathy (using JSE scores) (36). The inconsistencies were explained by significant interaction effects of gender and ethnicity (white, African American, Asian/Pacific Islander) of the simulated patients as well as the medical students (36).
Concluding Remarks
Based on the notion that patient’s understanding of clinician empathy is important in understanding clinical outcomes, we developed the JSPPPE to measure clinicians’ empathic engagement as viewed by patients. Brevity and simplicity of the instrument, plus evidence in support of its psychometrics, bolster our confidence in this measure. The JSPPPE has implications for the assessment of clinical outcomes and for evaluating the quality of clinicians’ interpersonal skills as experienced by patients. More research is needed to reaffirm the psychometrics of the JSPPPE in different groups of patients (inpatient and outpatient with a variety of disease conditions), in different groups of clinicians, in a variety of health professional disciplines, specialties, and settings, and in different cultures and demographic compositions.
Acknowledgment
The authors would like to thank Dorissa Bolinski for her editorial help.
Author Biographies
Mohammadreza Hojat is a research professor in the Department of Psychiatry and Human Behavior and director of the Jefferson Longitudinal Study, the Center for Research in Medical Education and Health Care, Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, Pennsylvania, USA.
Jennifer DeSantis is a senior research analyst at the Center for Research in Medical Education and Health Care, Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia. She provides research support and manages analytic services for the Jefferson Scale of Empathy.
Joseph S Gonnella is distinguished professor of medicine, emeritus dean, and founder of the Center for Research in Medical Education and Health Care, Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, Pennsylvania, USA.
Appendix A
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported in part by funding from the Noguchi Medical Research Institute in Tokyo, Japan.
References
- 1. Linn LS, DiMatteo MR, Cope DW, Robbins A. Measuring physicians’ humanistic attitudes, values, and behavior. Med Care. 1987;25:504–15. [DOI] [PubMed] [Google Scholar]
- 2. Larson EB, Yao X. Clinical empathy as emotional labor in patient-physician relationship. JAMA. 2005;293:1100–6. [DOI] [PubMed] [Google Scholar]
- 3. Veloski J, Hojat M. Measuring specific elements of professionalism: empathy, teamwork, and lifelong learning In: Stern DT, ed. Measuring Medical Professionalism. Oxford, UK: Oxford University Press; 2006:117–145. [Google Scholar]
- 4. Hojat M. Empathy in Health Professions Education and Patient Care. New York, NY: Springer International; 2016. [Google Scholar]
- 5. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes in diabetic patients. Acad Med. 2011;86:359–64. [DOI] [PubMed] [Google Scholar]
- 6. Del Canale S, Louis DZ, Maio V, Wang X, Rossi G, Hojat M, et al. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87:1243–9. [DOI] [PubMed] [Google Scholar]
- 7. Sullivan P. Pay more attention to your health, physicians warned. CMAJ. 1990;142:1309–10. [PMC free article] [PubMed] [Google Scholar]
- 8. Shamasundar MRC. Reflections: understanding empathy and related phenomena. AM J Psychother. 1999;53:232–45. [DOI] [PubMed] [Google Scholar]
- 9. Hyyppa M, Kronholm E, Mattler C. Mental well-being of good sleepers in a random population sample. Br J Med Psychol. 1991;64:25–34. [DOI] [PubMed] [Google Scholar]
- 10. Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:763 doi:10.3389/fpsyg.2016.00763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hojat M, Zuckerman M, Gonnella JS, Mangione S, Nasca TJ, Vergare M, et al. Empathy in medical students as related to specialty interest, personality, and perceptions of mother and father. Personality and Individual Differences. 2005;39:1205–15. [Google Scholar]
- 12. Hojat M, Bianco JA, Mann D, Massello D, Calabrese LH. Overlap between empathy, teamwork, and integrative approach to patient care. Med Teach. 2015;37:755–8. [DOI] [PubMed] [Google Scholar]
- 13. Hojat M, Michalec B, Veloski J, Tykocinski ML. Can empathy, other personality attributes, and level of positive social influence in medical school identify potential leaders in medicine? Acad Med. 2015;90:505–10. [DOI] [PubMed] [Google Scholar]
- 14. Pohl CA, Hojat M, Arnold L. Peer nominations as related to academic attainment, empathy, and specialty interest. Acad Med. 2011;86:747–51. [DOI] [PubMed] [Google Scholar]
- 15. Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educational and Psychological Measurement. 2001;61:349–65. [Google Scholar]
- 16. Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9. [DOI] [PubMed] [Google Scholar]
- 17. Hojat M, Spandorfer J, Louis DZ, Gonnella JS. Empathic and sympathetic orientations toward patient care: conceptualization, measurement, and psychometrics. Acad Med. 2011;86:989–95. [DOI] [PubMed] [Google Scholar]
- 18. Nightingale SD, Yarnold PR, Greenberg MS. Sympathy, empathy, and physician resource utilization. J Gen Intern Med. 1991;6:420–3. [PubMed] [Google Scholar]
- 19. Bohart AC, Elliot R, Greenberg LS, Watson JC. Empathy In: Norcross JC, ed. Psychotherapy Relationships That Work: Therapist Contributions and Responsiveness to Patients. Oxford, UK: Oxford University Press; 2002:89–108. [Google Scholar]
- 20. Hojat M, Louis DZ, Maio V, Gonnella JS. Empathy and health care quality. Am J Med Qual. 2013;28:6–7. doi:10.1177/1062860612464731. [DOI] [PubMed] [Google Scholar]
- 21. VandenBos GR, ed. APA dictionary of psychology. Washington, DC: American Psychological Association, 2007. [Google Scholar]
- 22. Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ. 2010;1:83–7. [Google Scholar]
- 23. Kane GC, Gotto JL, Mangione S, West S, Hojat M. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48:81–6. [PMC free article] [PubMed] [Google Scholar]
- 24. Lipner RS, Blank LL, Leas BF, Fortna GS. The value of patient and peer ratings in recertification. Acad Med. 2002;77:s64–6. [DOI] [PubMed] [Google Scholar]
- 25. Weaver MJ, Ow CL, Walker DJ, Degenhardt EF. A questionnaire for patients’ evaluations of their physicians’ humanistic behaviors. J Gen Intern Med. 1993;8:135–9. [DOI] [PubMed] [Google Scholar]
- 26. Matthews DA, Feinstein AR. A new instrument for patients’ rating of physician performance in hospital setting. J Gen Intern Med. 1989;4:14–22. [DOI] [PubMed] [Google Scholar]
- 27. Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. A brief instrument to measure patient’s overall satisfaction with primary care physicians. Fam Med. 2011;43:412–7. [PubMed] [Google Scholar]
- 28. Berg K, Majdan JF, Berg D, Veloski J, Hojat M. A comparison of medical students’ self-reported empathy with simulated patients’ assessment of the students’ empathy. Med Teach. 2011;33:388–91. [DOI] [PubMed] [Google Scholar]
- 29. Glaser K, Markham FW, Adler HM, McManus PR, Hojat M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit. 2007;13:CR291–4. [PubMed] [Google Scholar]
- 30. Grosseman S, Novack DH, Duke P, Mennin S, Rosenzweig S, Davis TJ, et al. Residents’ and standardized patients’ perspectives on empathy: issues of agreement. Patient Educ Couns. 2014;96:22–8. [DOI] [PubMed] [Google Scholar]
- 31. Free NK, Green BL, Grace MC, Chernus LA, Whitman RM. Empathy and outcome in brief focal dynamic therapy. Am J Psychiatry. 1985;142:917–21. [DOI] [PubMed] [Google Scholar]
- 32. Newble D. Techniques for measuring clinical competence: objective structured clinical examinations. Med Educ. 2004;38:100–203. [DOI] [PubMed] [Google Scholar]
- 33. Berg K, Berg D, Majdan J, Veloski J, Hojat M. Medical students’ self-reported empathy and simulated patients’ assessments of student empathy: an analysis by gender and ethnicity. Acad Med. 2011;86:984–8. [DOI] [PubMed] [Google Scholar]
- 34. Henry SG. Playing doctors. JAMA. 2005;294:2138–9. [DOI] [PubMed] [Google Scholar]
- 35. Berg K, Blatt B, Lopreiato J, Jung J, Schaeffer A, Heil D, et al. Standardized patient assessment of medical student empathy: ethnicity and gender effects in a multi-institutional study. Acad Med. 2015;90:105–11. [DOI] [PubMed] [Google Scholar]