Abstract
The clinician-patient relationship is asymmetric in the sense that clinicians and patients have different roles in the medical consultation. Yet, there are qualities of reciprocity and mutuality in many clinician-patient encounters, and we suggest that such reciprocity may be related to the phenomenon of empathy. Empathy is often defined as the capacity to place oneself in another’s position, but empathy may also be understood as a sequence of reciprocal turns-of talk, starting with the patient’s expression of emotion, followed by the perception, vicarious experience, and empathic response by the clinician. These patterns of reciprocity may also include the patient’s experience of and response to the clinician’s emotions. Researchers in different fields of research have studied how informal human interaction often is characterized by mutuality of lexical alignment and reciprocal adjustments, vocal synchrony, as well as synchrony of movements and psychophysiological processes. A number of studies have linked these measures of reciprocity and synchrony in clinical encounters to the subjective experience of empathy.
Keywords: communication, empathy, synchrony, reciprocal adjustments, linguistic alignment
Brief Introduction
The clinician–patient relationship is an asymmetric affair. The clinician has a number of instrumental tasks to fulfill, such as examining and treating the patient; whereas the patient comes to the conversation with a health-related concern—or 2 or 3. The roles are complementary, and the relationship is asymmetric. Yet, all clinicians will have experienced how the degree of asymmetry may change in certain consultations, in particular when patients express emotional concerns. Communication becomes more symmetrical and with a higher degree of mutuality. Such moments have often been described in the narrative literature on clinicians’ experiences, for instance, in terms of “connexion,” the special moments of intense feelings of compassion and reciprocal companionship with the patient, sometimes accompanied by physiological reactions such as wet eyes and chills.(1) The different roles of clinician and patient are still intact (or should be) in spite of high degree of emotional intensity, but the pattern of talk between patient and clinician may become more symmetrical and mutual.
In the present article, we shall relate this quality of reciprocity and mutuality to the phenomenon of empathy in 2 different ways. First, we will discuss definitions of empathy as a sequence of reciprocal turns of talk. Second, we will discuss recent research on how empathy relates to reciprocal adjustments and synchrony. Our main focus is on lexical alignment (an example of reciprocal adjustments); however, we will also touch on vocal, movement, and psychophysiological synchrony.
Empathy: From Capacity to Sequence to Synchrony to Reappraisal
Empathy is often defined as an individual capacity, as his/her capacity to place oneself in another’s position,(2) in “the other person’s shoes,” as the saying often goes. In the Webster online dictionary, “capacity” is replaced with “action.” Empathy is here defined as “the action of understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another.” (3) The word “action” points to empathy as a characteristic of an interpersonal event, in which one person, a listener, attempts to understand the thoughts and feelings of another person, a speaker. According to such standard dictionary definitions, empathy is understood in the framework of an asymmetric relationship between a listener and a speaker. One action for the listener is the perceptual component of empathy, to be aware of and sensitive to the emotions of the speaker, and as accurately as possible identify the emotion (emotional accuracy). The other component is the vicarious experience of the emotions the speaker expresses.
In clinical empathy, there is a third component of empathy not found in dictionary definitions. When the speaker’s (ie, the patient’s) emotions have been identified and (more or less) vicariously experienced, the listener (ie, the clinician) should somehow respond to the speaker to indicate that the message has been received, a response that clinicians are taught to enact in the face of patient emotions.(4)
In this way, empathy is a sequence, starting with the patient’s expression of emotion, followed by the perception, vicarious experience, and empathic response by the clinician. The sequence is exemplified in a small excerpt between a patient and a clinician below(5):
P: I have been feeling so down (patient’s expression of emotion)
C: and you are very anxious too (clinician’s response)
P: yes (patient’s response to the clinician’s response)
A sequential understanding of empathy is obviously not new in the literature. Definitions of empathy in terms of sequences have been suggested by a number of authors. In a much quoted paper, Barrett-Lennard suggested a model that includes 3 phases.(6) The model actually skips the patient's initial emotion and starts with the empathic resonance by the clinician in response to the patient as stage 1 (by the way, in his concept empathic resonation Barret-Lennard does not distinguish between the identification and vicarious experience of the patient’s original emotion). Phase 2 is the clinician’s attempt to convey his or her understanding and phase 3 is the patient’s actual reception and awareness of the clinician’s communication. Barrett-Lennard points out that when the process continues, phase 1 is again the core feature, and phases 2 and 3 may follow in a cyclical mode.
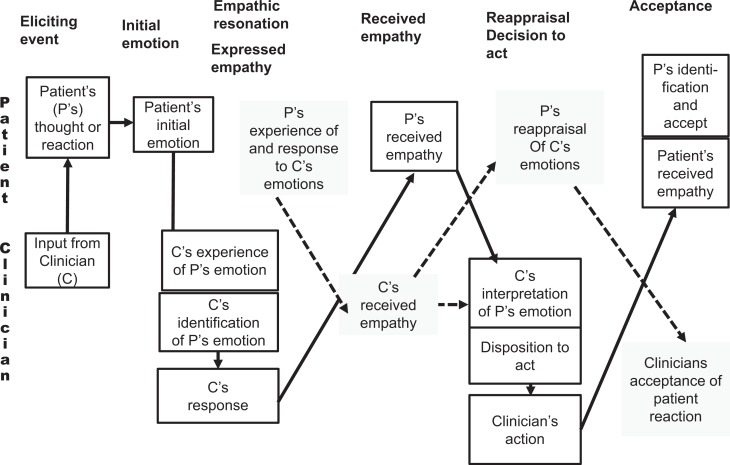
So far, we have analyzed empathy in terms of patient-initiated emotion and clinician-initiated response. But if the patient is sensitive and attentive; he or she may also observe the clinician’s empathic resonance before he explicitly responds. The patient may of course be absorbed in his or her own feelings and may miss the fact that the clinician too is also moved. Or he/she may identify the reaction, perhaps be moved by it and possibly even comment on it. This adds another level of reciprocity to the definition of empathy (see Figure 1).
Figure 1.
Model of patient–clinician empathy, including patient’s response to clinician’s emotions.
Some models add yet another phase in their understanding of empathy—that of the therapist’s helping behavior in response to the patient’s emotion. In Mercer’s model, clinical empathy involves the ability to (a) understand the patient’s situation, perspective, and feelings (and their attached meanings); (b) to communicate that understanding and check its accuracy; and (c) to act on that understanding with the patient in a helpful (therapeutic) way.(7) Although (a) and (b) somewhat corresponds to Barret-Lennard’s model of empathic resonance, (c) refers to the clinician’s judgment and action subsequent to achieving and communicating understanding the patient’s emotion. In this last phase of empathy, the patient’s expressed emotion not only serves as a cue for empathic resonance but also as a cue for professional helping behavior (eg, offer reassurance with information to counteract worrying). Now, it is the clinician (in the role of the speaker) who suggests a reappraisal of the patient’s concern which the patient (now in the role of the listener) will adjust to. If such clinician reappraisals are to be regarded as part of the empathic sequence, it is now up to the patient to resonate with the therapist’s appraisal of the event.
Figure 1 is a model of potential empathy. Whether the clinician has accurately perceived the patient’s emotions and actually felt a vicarious emotional resonance and acknowledged it is an empirical question. As resonance is achieved, the clinician can potentially move on to suggest context-dependent actions that reappraise the patient’s emotions and therefore set the stage for the patient to adjust to the clinician’s interpretation.
Our emphasis in the discussion of the empathy concept so far has been the reciprocity between the listener and speaker and the patient and clinician. Some researchers apply a slight different terminology and define empathy as a form of behavioral synchrony.(8) Synchrony: the term synchrony is used to refer to events that occur simultaneously. Thus, if there is a time lag between related events in an interaction, or if only 1 person exhibits a given behavior, there is a lack of synchrony. There is a growing literature on synchrony in psychotherapy.(9)
To summarize, empathy should not only—or primarily—be defined in terms of individual capacities but rather as a sequence of ongoing exchanges based on a high degree of reciprocity. One problem with this model is that it is difficult to measure the subjective feeling of received empathy during a consultation as that would interrupt the interaction. As a result, received empathy is most often measured post hoc after the encounter. Consequently, the role of reciprocal processes in empathy, at least in terms of the patient’s experience of received empathy, must be done by relating measures of reciprocal behaviors and synchronous events to post hoc measures of empathy, which is the topic of the rest of the present paper.
Lexical or Linguistic Alignment
A number of studies from the research tradition of conversation analysis (CA) have shown how talk in informal conversations is linked from turn to turn in a characteristic pattern of turn-taking between the conversational partners. Normatively, 1 person at a time talks and has the floor. In our example, the patient is the first speaker. When the clinician takes his or her turn to talk, it will most often connect to the first speaker’s turn in some way, for instance, by answering a question or making an explicit reference to what was just said.(10) In addition to the content, the second speaker’s turn will most often follow within an average of 200 ms with some variations among languages. Sometimes the turns overlap. In spite of overlaps and tiny gaps between turns, most often conversations run rather smoothly with a steady exchange of expressions between the conversational partners.(11)
In a paper named “Why is conversation so easy?” the Scottish language researchers Garrod and Pickering argue that one of the reasons why conversations run so smoothly is the fact that speakers apply largely automatic and unconscious processes of interactive alignment in the process of speaking and listening in conversations.(12) It is a process by which people adjust to one another’s behavior during ongoing interaction by making use of each other’s words, sounds, and grammatical forms. Scott, McGettigan, and Eisner point out how effective conversations heavily rely on smooth turn-taking routines characterized by lexical alignment.(13) Studies based on transcripts of dialogue contain numerous examples of lexical repetitions in adjacent turns.(14) Even pronunciation is found to converge with other participants in conversation.(15)
Few studies have investigated lexical alignment in clinical settings. A large part of conventional medical consultation may take the form of linked questions and answers known as adjacency pairs. During history taking in medical encounters communication is strongly under doctor control with turn-taking less dependent on repetitions and inferences. Studies from the CA tradition have found that medical questioning is often shaped by the principles of “optimization” and “recipient design,” which function to shape patients’ responses.(16) In a study of follow-up consultations in cancer care, Mellblom et al found examples of shifts between an asymmetrical, task-focused mode to more affiliative and facilitative communication, but they did not report the degree of interactive alignment in these encounters.(17)
In terms of synchrony in the lexical content of turns, Coulehan et al suggest reflecting the content of the patient’s statement as an empathic response.(18) The Empathic Communication Coding System (ECCS) also recognizes explicit recognition of the patient’s perspective as central to the communication of empathy.(19) In a study of physician’s responses to patients’ expressions of worry, only 6% of responses were categorized as empathic responses.(20) This particular study, however, also analyzed the subsequent responses of the physician. Most empathic responses were not only succeeded by biomedical enquiry but also by actions such as prescriptions or referrals, reassurance or change of topic.
The first study explicitly to measure phenomena such as lexical alignment in a clinical setting is a recent study by Lord et al.(21) In sessions with high empathy, language style synchrony, defined as the occurrence of both therapist and patient use of words in specific categories in adjacent talk-turn pairs, averaged over all talk turns, was higher across 11 language style categories. The authors concluded that synchrony in language style is related to empathy over and above the synchrony of content.
Vocal Synchrony
A number of studies have investigated qualities of the voice in interpersonal interaction. A frequently used measure is fundamental frequency (f0), which is a measure of the rate of the vibration of the vocal cords, which is highly correlated with perceived pitch. A number of studies using f0 in informal social interaction have found evidence of verbal alignment. Imel et al investigated vocally encoded arousal in motivational interview consultations and similarly found vocal synchrony.(22) The associations were stronger in consultations with high-empathy ratings.
In a similar study, Reich et al actually found a negative association between f0 and empathy ratings.(23) In this study, therapists were instructed to model pitch shifts behaviorally, encouraging clients to move in a different affective direction. Conscious manipulation of normally automatic behaviors may possibly explain this unexpected result.
Body Movement, Alignment, and Synchrony
The phenomenon of interactive alignment is not limited to verbal behavior. There is evidence that individuals in interpersonal interaction tend to adjust to one another’s posture and movements in an intricate dance of mirrored movements.
It has since long been suggested that reciprocal nonverbal, perceptual-motor mimicry may facilitate the smoothness and mutual positivity in face-to-face interaction and promote expression of affiliation with co-conversationalists.(24)
The alignment of body movements has also been studied in psychotherapy. In early experiments, therapists were instructed to synchronize their movements with patients. In consultations with high-synchrony ratings, therapists were rated more favorably than in consultation with a low degree of movement synchrony.
Studies by Ramseyer and Tschacher indicate that movement synchrony was associated with more positive emotion and served as a predictor of symptom reduction.(25,26)
Psychophysiological Synchrony
Physiological concordance in interpersonal interaction has been investigated in a number of studies, and the implications for the clinician–patient relations have been suggested.(27) However, only a few empirical studies so far have investigated on psychophysiological synchrony in medical consultations. In an early study, Robinson et al measured electrodermal activity (EDA) of both therapists and simulated patients in arranged consultations.(28) They found a significant relationship between subjective empathy scores and phasic, but not tonic, EDA activity.
In another EDA study, an association was found between physiological concordance of EDA and patients’ report of received empathy.(29) In another study, the same investigators found an association between EDA activation and social–emotional responses as measured by Bales Interaction Coding system.(30) Similar findings were reported by Messina et al who found a significant positive correlation between empathy, as perceived by standardized patient actors, and physiological measures.(31)
Summary and Conclusion
In this brief review, we have presented evidence that informal human interaction is characterized by mutuality of lexical alignment, reciprocal adjustments, synchrony of movements, and psychophysiological processes. A body of research links these measures of mutuality in clinical encounters to the subjective experience of empathy.
An obvious chicken and egg question here is whether the feeling of mutual understanding is a consequence of ongoing adjustments in verbal behavior, movement synchrony and psychophysiological arousal. Or, is it the experience of mutual understanding which leads to synchronous processes in the body? And to what extent is either of these phenomena related to explicit talk about emotion in both clinician and patient? We hope the present article has shed some light on these complicated relationships and may serve as inspiration for further research on empathy in clinical interaction.
Author Biographies
Arnstein Finset, PhD, is a professor of Behavioral Sciences in Medicine, University of Oslo and Editor-in-Chief of Patient Education and Counseling. He is a clinical psychologist with a background in rehabilitation and neuropsychology. He has published widely in clinical communication research and clinical health psychology.
Knut Ørnes, MD, is currently a doctoral student at the Centre for Medical Ethics, Institute of Health and Society, University of Oslo.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research and/or authorship of this article.
References
- 1. Matthews DA, Suchman AL, Branch WT., Jr Making ‘connexions’: enhancing the therapeutic potential of patient-clinician relationships. Ann Internal Med. 1993;118:973–7. [DOI] [PubMed] [Google Scholar]
- 2. Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med. 1998;73:403–7. [DOI] [PubMed] [Google Scholar]
- 3. Shapiro J. Perspective: does medical education promote professional alexithymia? A call for attending to the emotions of patients and self in medical training. Acad Med. 2011;86:326–32. [DOI] [PubMed] [Google Scholar]
- 4. Halpern J. What is clinical empathy? J Gen Intern Med. 2003;18:670–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wynn R, Wynn M. Empathy as an interactionally achieved phenomenon in psychotherapy. Characteristics of some conversational resources. J Pragmatics. 2006;38:1385–97. doi:10.1016/j.pragma.2005.09.008. [Google Scholar]
- 6. Barrett-Lennard GT. The empathy cycle: refinement of a nuclear concept. J Couns Psychol. 1981;28:91–100. doi:10.1037//0022-0167.28.2.91. [Google Scholar]
- 7. Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;P52(suppl):S9–S12. [PMC free article] [PubMed] [Google Scholar]
- 8. Behrend A, Müller S, Dziobek I. Moving in and out of synchrony: A concept for a new intervention fostering empathy through interactional movement and dance. Arts Psychother. 2012;39:107–116. doi:10.1016/j.aip.2012.02.003. [Google Scholar]
- 9. Koole SL, Tschacher W. Synchrony in psychotherapy: A review and an integrative framework for the therapeutic alliance. Font Psychol. 2016;7:862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Drew P. Turn design In: Sidnell J, Stivers T, eds. The Handbook of Conversation Analysis. Chichester: Wiley-Blackwell; 2013:131–49 [Google Scholar]
- 11. Finset A. Talk-in-interaction and neuropsychological processes. Scand J Psychol. 2014;55:212–18. [DOI] [PubMed] [Google Scholar]
- 12. Garrod S, Pickering MJ. Why is conversation so easy? Trends Cogn Sci. 2004;8:8–11. doi:10.1016/j.tics.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 13. Scott SK, McGettigan C, Eisner F. A little more conversation, a little less action—candidate roles for the motor cortex in speech perception. Nat Rev Neurosci. 2009;10:295–302. doi:10.1038/nrn2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tannen D. Talking Voices: Repetition, Dialogue, and Imagery in Conversational Discourse. New York: Cambridge University Press; 2007. [Google Scholar]
- 15. Pardo JS. On phonetic convergence during conversational interaction. J Acoust Soc Am. 2006;119:2382–93. doi:10.1121/1.2178720. [DOI] [PubMed] [Google Scholar]
- 16. Heritage J, Maynard DW. Introduction: Analyzing interaction between doctors and patients in primary care encounters In: Heritage J, Maynard DW, eds. Communication in Medical Care: Interaction Between Primary Care Physicians and Patients. New York: Cambridge University Press; 2006:1–21. [Google Scholar]
- 17. Mellblom AV, Korsvold L, Ruud E, Lie HC, Loge JH, Finset A. Sequences of talk about emotional concerns in follow-up consultations with adolescent childhood cancer survivors. Patient Educ Couns. 2016;99:77–84. doi: 10.1016/j.pec.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 18. Coulehan JL, Platt FW, Egener B, Frankel R, Lin CT, Lown B, et al. “Let me see if I have this right…”: words that help build empathy. Ann Intern Med. 2001;135:221–7. [DOI] [PubMed] [Google Scholar]
- 19. Bylund CL, Makoul G. Empathic communication and gender in the physician–patient encounter. Patient Educ Couns. 2002;48:207–16. [DOI] [PubMed] [Google Scholar]
- 20. Epstein RM, Hadee T, Carroll J. Could this be something serious? J General Intern Med. 2007;22:1731–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lord SP, Sheng E, Imel ZE, Baer J, Atkins DC. More than reflections: empathy in motivational interviewing includes language style synchrony between therapist and client. Behav Ther. 2015;46:296–303. doi10.1016/j.beth.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Imel ZE, Barco JS, Brown HJ, Baucom BR, Baer JS, Kircher JC, et al. The association of therapist empathy and synchrony in vocally encoded arousal. J Couns Psychol. 2014;61:146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reich CM, Berman JS, Dale R, Levitt H. Vocal synchrony in psychotherapy. J Soc Clin Psychol. 2014;33:481–94. doi:10.1521/jscp.2014.33.5.481. [Google Scholar]
- 24. Chartrand TL, Bargh JA. The chameleon effect: the perception-behavior link and social interaction. J Pers Soc Psychol. 1999;76:893–910. doi:10.1037/0022-3514.76.6.893. [DOI] [PubMed] [Google Scholar]
- 25. Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol. 2011;79:284–95. doi:10.1037/a0023419. [DOI] [PubMed] [Google Scholar]
- 26. Tschacher W, Rees GM, Ramseyer F. Nonverbal synchrony and affect in dyadic interactions. Front Psychol. 2014;5:1323 doi:10.3389/fpsyg.2014.01323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Coutinho JF, Silva PO, Decety J. Neurosciences, empathy, and healthy interpersonal relationships: recent findings and implications for counseling psychology. J Couns Psychol. 2014;61:541–8. [DOI] [PubMed] [Google Scholar]
- 28. Robinson JW, Herman A, Kaplan BJ. Autonomic responses correlate with counselor-client empathy. J Couns Psychol. 1982;29:195–8. doi:10.1037//0022-0167.29.2.195. [Google Scholar]
- 29. Marci CD, Orr SP. The effect of emotional distance on psychophysiologic concordance and perceived empathy between patient and interviewer. Appl Psychophysiol Biofeedback. 2006;31:115–28. doi:10.1007/s10484-006-9008-4. [DOI] [PubMed] [Google Scholar]
- 30. Marci CD, Ham J, Moran E, Orr SP. Physiologic correlates of perceived therapist empathy and social-emotional process during psychotherapy. J Nerv Ment Dis. 2007;195:103–11. doi:10.1097/01.nmd.0000253731.71025.fc. [DOI] [PubMed] [Google Scholar]
- 31. Messina I, Palmieri A, Sambin M, Kleinbub JR, Voci A, Calvo V. Somatic underpinnings of perceived empathy: the importance of psychotherapy training. Psychother Res. 2013;23:169–77. doi:10.1080/10503307.2012.748940. [DOI] [PubMed] [Google Scholar]