Abstract
Background
The effects of targeted neuromuscular training (TNMT) on movement biomechanics associated with the risk of anterior cruciate ligament (ACL) injuries are currently unknown.
Purpose/Hypotheses
To determine the effectiveness of TNMT specifically designed to increase trunk control and hip strength. The hypotheses were that (1) TNMT would decrease biomechanical and neuromuscular factors related to an increased ACL injury risk and (2) TNMT would decrease these biomechanical and neuromuscular factors to a greater extent in athletes identified as being at a high risk for future ACL injuries.
Study Design
Controlled laboratory study.
Methods
Female athletes who participated in jumping, cutting, and pivoting sports underwent 3-dimensional biomechanical testing before the season and after completing TNMT. During testing, athletes performed 3 different types of tasks: (1) drop vertical jump, (2) single-leg drop, and (3) single-leg cross drop. Analysis of covariance was used to examine the treatment effects of TNMT designed to enhance core and hip strength on biomechanical and neuromuscular characteristics. Differences were also evaluated by risk profile. Differences were considered statistically significant at P < .05.
Results
TNMT significantly increased hip external rotation moments and moment impulses, increased peak trunk flexion, and decreased peak trunk extension. Athletes with a high risk before the intervention (risk profile III) had a more significant treatment effect of TNMT than low-risk groups (risk profiles I and II).
Conclusion
TNMT significantly improved proximal biomechanics, including increased hip external rotation moments and moment impulses, increased peak trunk flexion, and decreased peak trunk extension. TNMT that focuses exclusively on proximal leg and trunk risk factors is not, however, adequate to induce significant changes in frontal-plane knee loading. Biomechanical changes varied across the risk profile groups, with higher risk groups exhibiting greater improvements in their biomechanics.
Keywords: anterior cruciate ligament, biomechanics, female athlete, neuromuscular training, risk profile
Proximal control of the knee joint has emerged in the literature as a crucial modifier of the anterior cruciate ligament (ACL) injury risk.34,35 Specifically, abnormal or insufficient control of the hip in the frontal and transverse planes during closed kinetic chain maneuvers directly affects alignment and load transmission through the knee.3,6,7,12 Hip internal rotation and adduction motions contribute to knee movement toward the midline, potentially leading to a valgus-like posture and an increased risk of injuries. Similarly, aberrant lateral trunk motion perturbs the center of mass and directly affects proximal knee loading.6 The effect of impaired proximal control is profound, as athletes with decreased trunk proprioception and postural stability are significantly more likely to suffer a future knee injury than those with good or normal measures for these values.34
There is strong evidence to support prevention programs as an effective means to reduce the ACL injury risk.24 Yet, the incidence of ACL reconstructions has continued to rise.9 Furthermore, the number of procedures being performed among patients under the age of 20 years, and among female athletes, is also increasing.9 This has prompted the recommendation that prevention programs should be targeted toward those who are most likely to sustain an ACL injury.9,16 The content of prevention programs has also come into question. Sadoghi et al24 performed a systematic review to evaluate the effectiveness of ACL injury prevention programs. Of 909 published studies, 9 met study inclusion criteria, which included that the number of ACL injuries was reported, a neuromuscular training program was applied, women were included as participants, a prospective controlled trial study design was employed, and attendance and compliance information for the neuromuscular training program was collected. The authors determined that, while injury prevention programs were an effective means to reduce the ACL injury risk, they were unable to identify the “best” training content.27 This was because of considerable heterogeneity of the included studies, with content including plyometrics, balance board exercises, video feedback, and education regarding positions to avoid during jump landing.2,5,10,19,22,23,25 While previous investigations have focused on knee motions and loads as risk factors, there is a need to address proximal factors, including the trunk and hip, that contribute to knee positions that result in ACL injuries.
Targeted neuromuscular training (TNMT) has been shown to effectively increase hip abduction strength in female athletes.16 Myer et al16 recruited 21 uninjured high school volleyball players for study participation. This included 7 players who served as control participants and 14 athletes who participated in a 10-week TNMT program designed to enhance trunk control and hip abduction strength. Outcome measures included changes in isokinetic hip abduction strength. Myer et al16 reported a 15% increase in hip abduction strength in the TNMT group, with no changes in strength for the control group. The authors concluded that improvement in hip abduction strength may improve the ability of female athletes to increase control of lower limb alignment and decrease knee loads resulting from increased trunk displacement during sports activities.16 The effect of TNMT on biomechanical and neuromuscular movement characteristics has not been evaluated. It is also unknown if there is a differential effect of TNMT on patients with distinct ACL injury risk profiles.
The purpose of this study was to determine the effectiveness of TNMT specifically designed to increase trunk control and hip strength in female athletes playing high-risk sports. We hypothesized that this specialized training would decrease the magnitude of biomechanical and neuromuscular risk factors for an ACL injury. We also hypothesized that TNMT would decrease these biomechanical and neuromuscular factors to a greater extent among patients identified as high risk for future ACL injuries based on an algorithm that we have previously described.4
Methods
Participants
This was a repeated-measures, cluster randomized controlled trial. The initial cohort consisted of 624 uninjured female athletes from regional basketball, volleyball, and soccer teams (Figure 1). Participation requirements included no history of ACL injuries or knee surgery and no lower extremity injuries or low back pain in the year before study participation that required medical intervention. The study was approved by The Ohio State University institutional review board. Both participant and parental consent were obtained before study participation.
Figure 1.
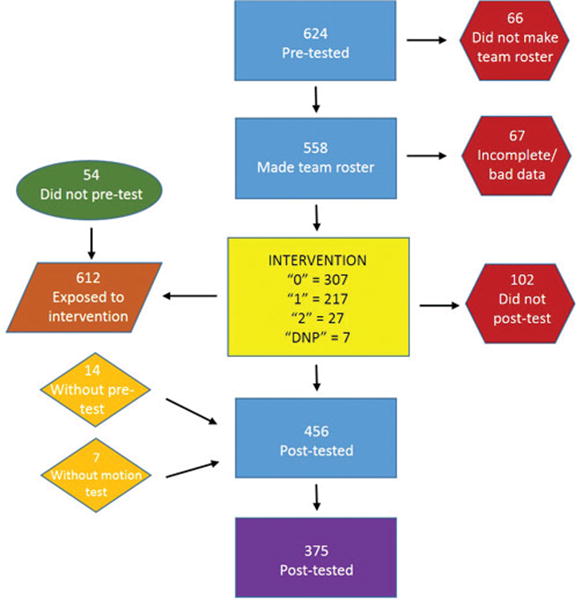
Flow diagram of testing and analysis. “0,” targeted neuromuscular training (TNMT); “1,” Sham speed training control group; “2,” Convenience control group whose team or coach did not comply with TNMT; “DNP,” individual athletes who did not participate in any intervention (did not make team) and were not included in the final analysis.
Procedures
Three-dimensional biomechanical testing was conducted before the athlete's competitive sports season and after completing the training protocol. All testing was performed in a single laboratory. Kinematic data were collected using a 10-camera motion capture system (Eagle Camera; Motion Analysis Corp) at 240 Hz. Kinetic data were collected at 1200 Hz from 2 force plates (AMTI) embedded into the floor and synchronized with motion data. Each participant was instrumented with 55 retro-reflective markers, after which a static trial with the participant positioned in an anatomic neutral position was performed. Subsequent kinematic measures were referenced in relation to this position.
During testing, athletes were asked to perform 3 different tasks from a 31-cm box: a drop vertical jump (DVJ), single-leg drop (SLD), and single-leg cross drop (SCD). For each task, 3 trials were performed. The SCD was performed by balancing on one foot and then dropping forward and medially off of the box and landing on the opposite leg. The SLD started in the same position on top of a 31-cm box, but participants were instructed to hop straight off the box and land on the same foot. During the DVJ, the participant dropped off the box with both feet leaving at the same time and immediately performed a maximum vertical jump upon landing. Tasks were performed in randomized order with the landing side further randomized within each movement.
Training
Teams were randomized into either a control or experimental group. Training volume was equivalent between groups, with each training session taking approximately 30 minutes to complete. Training took place both before the season and during the season 2 to 3 times weekly over a 10-week period. Training was performed in a team setting with an athletic trainer supervising exercise performance. The experimental group performed core neuromuscular training (TNMT). The TNMT plan was based on published reports and pilot work (Table 1)13,14,27 and has been reported to be potentially efficacious for reducing the ACL injury risk in female athletes.11,20,27,28 The overriding goal of TNMT was to include exercises that would increase lateral trunk control and decrease knee abduction moments (KAMs) and/or the ACL injury risk.6 Training exercises were divided into 5 phases, with a progression to the next phase dependent on the correct execution of each task. Exercises in the advanced phases progressed to techniques that initiated lateral trunk perturbations and forced the athlete to decelerate and control the trunk.13,14 Other published exercises that focused on decreasing lateral trunk motion and increasing hip abductor torque from TNMT programs designed to decrease KAMs were also utilized.17,18
Table 1. TNMT Exercise Progressiona.
| Exercise | Published Studies |
|---|---|
| Lateral jump | Hewett et al,5 |
| Mandelbaum et al10 | |
| Hop-hold | Hewett et al5 |
| BOSU single-knee hold | Myer et al16 |
| Single-leg lateral Airex hop-hold | Myklebust et al,21 |
| Petersen et al23 | |
| Tuck jump | Hewett et al5 |
| Lunge jump | Hewett et al5 |
| Walking lunge | Mandelbaum et al10 |
| BOSU single-leg pelvic bridge | Mandelbaum et al10 |
| Table lateral crunch | Myer et al16 |
| Table double crunch | Myklebust et al,21 |
| Petersen et al23 | |
| Back hyperextension with ball reach | Myer et al16 |
| Single-leg 90° hop-hold | Myklebust et al,21 |
| Petersen et al23 |
The full targeted neuromuscular training (TNMT) and control intervention plans are outlined in detail in the cited references.
The control group performed sagittal plane–only resistive running drills using rubber resistance bands designed solely to enhance sprint speed.15 Five phases were utilized to facilitate progressions designed to improve the athletes' straight-line sprinting speed and match the progressive nature of the investigational protocol by increasing the duration and resistance level with each phase. All running drills in each phase were progressive in nature and developed from prior investigations that showed increased sprint speed in female athletes who participated in the protocol.15,18
Data Management
The average of the 3 trials performed for each task was used for analysis. The interval of interest was the initial landing phase of each jump. Marker trajectories and force plate data used for the calculation of joint moments were filtered with a bidirectional low-pass fourth-order Butterworth digital filter (12-Hz cutoff frequency). Force plate data used in calculating the peak ground-reaction force were additionally filtered with a bidirectional low-pass fourth-order Butter-worth digital filter (100-Hz cutoff frequency). The hip joint center was determined using a validated anthropometricsbased calculation.1 Euler angles were used to describe lower extremity motions, and joint moments were calculated using inverse dynamics (C-Motion Inc; MathWorks Inc).
Statistical Analysis
Changes after training in biomechanical measures of interest were evaluated between the TNMT and control groups using analysis of covariance and adjusted for preintervention values and sports teams. Differences were considered statistically significant at P < .05. In our previous work using latent profile analysis (LPA), 467 athletes were characterized by the risk (low, medium, and high) for future ACL injuries based on biomechanical landing data. Athletes who were classified as medium and high risk had a significantly higher knee adduction moment compared with those classified as low risk.4 We further explored the interaction between training treatment group and risk profile and conducted analyses stratified by risk profile as appropriate. Statistical testing was performed with SAS version 9.3 (SAS Institute).
Results
Of 624 athletes who completed pretesting, 66 did not make their team's roster, and 67 were excluded secondary to unusable or incomplete data. A total of 456 athletes completed the training intervention, and 375 who had biomechanical data available both before and after training were included in the current analysis (Figure 1 and Table 2). Of the 370 athletes, 54 (15%), 262 (71%), and 51 (14%) had risk profiles of I (low), II (moderate), and III (high), respectively, based on the baseline data (3 did not have a risk profile because of missing data in specific biomechanical variables used to define the risk profiles).
Table 2. Pretesting Characteristics of Participants Included in Intention-to-Treat Analysisa.
| Characteristics | Overall (n = 375) | TNMT (n = 222) | Control (n = 148) |
|---|---|---|---|
| Age, y | 13.9 ± 1.7 | 14.0 ± 1.7 | 13.8 ± 1.8 |
| Height, cm | 160.0 ± 8.4 | 160.7 ± 8.7 | 160.1 ± 8.0 |
| Weight, kg | 55.0 ± 12.2 | 54.1 ± 12.0 | 55.4 ± 12.5 |
| Body mass index, kg/m2 | 21.1 ± 3.6 | 20.8 ± 3.5 | 21.5 ± 3.8 |
Values are reported as mean ± SD. TNMT, targeted neuromuscular training.
After training, changes in maximum trunk flexion and extension angles during the SCD were significantly different between the TNMT and control groups (P < .05). Maximum trunk flexion angles had an increase of 2.80 in the TNMT group, compared to a decrease of 4.84 in the control group (P < .01) (Table 3). Maximum trunk extension angles were significantly lower in the TNMT group after training compared with a significant increase in the control group (Table 3).
Table 3. Change (Before to After Intervention) in Selected Variables by Treatment Groupa.
| Variable | TNMT | Control | P Value |
|---|---|---|---|
| Maximum trunk flexion angle, deg | |||
| SCD | |||
| All risk profiles | –2.80 (1.08) | 4.84 (1.67) | <.01 |
| Risk profile Ib | –2.11 (1.91) | 3.71 (1.68) | |
| Risk profile II | –1.20 (1.64) | 2.72 (2.43) | .33 |
| Risk profile III | –4.66 (1.99) | 8.23 (2.70) | .01 |
| Maximum trunk extension angle, deg | |||
| SCD | |||
| All risk profiles | –3.29 (1.23) | 6.18 (1.90) | <.01 |
| Risk profile Ib | –2.11 (2.10) | 5.36 (2.02) | |
| Risk profile II | –1.59 (1.92) | 3.69 (2.84) | .26 |
| Risk profile III | –4.10 (2.61) | 9.09 (3.53) | .03 |
| Hip external rotation moment, Nm/kg | |||
| SLD | |||
| All risk profiles | –2.52 (0.78) | 1.54 (1.19) | .03 |
| Risk profile Ib | –1.05 (0.71) | –1.96 (0.99) | |
| Risk profile II | –3.82 (1.39) | 3.13 (2.05) | .04 |
| Risk profile III | –0.49 (2.03) | –1.21 (2.80) | .87 |
| Hip external rotation moment impulse during first 10% of landing phase, Nm/kgs | |||
| SLD | |||
| All risk profiles | –0.03 (0.02) | 0.10 (0.04) | .02 |
| Risk profile Ii | –0.01 (0.02) | 0.08 (0.03) | |
| Risk profile II | –0.01 (0.04) | 0.04 (0.06) | .59 |
| Risk profile III | –0.06 (0.07) | 0.21 (0.09) | .08 |
Values are reported as least squares mean (standard error). Negative values for change in maximum trunk flexion angle, hip external rotation moment, hip external rotation moment impulse imply an increase in the measure, while negative values for change in maximum trunk extension angle imply a decrease. P values are for comparison between the treatment groups. SCD, single-leg cross drop; SLD, single-leg drop; TNMT, targeted neuromuscular training.
Values are reported as raw mean (standard error) because of the sample size.
After training, changes in the hip external rotation moment during the SLD were significantly different between the TNMT and control groups (P = .03): there was a significant increase in the TNMT group compared with a decrease in the control group (Table 3). Changes in the hip external rotation moment impulse during the SLD were also significantly different between the TNMT and control groups (P = .02): there was an increase of 0.03 in the TNMT group compared with a decrease of 0.10 in the control group (Table 3).
There were no significant differences in KAM changes between the TNMT and control groups during the SCD (mean [SE], 0.85 [1.37] Nm and –2.27 [2.12] Nm, respectively; P = .36) or the DVJ (mean [SE], 0.72 [1.31] Nm and 0.64 [0.02] Nm, respectively; P = .98). A priori, we did not examine the KAM during the SLD. There were also no differences between the groups for any other variables of interest during the DVJ (P > .05).
We also analyzed the treatment effects in these biomechanical measures by LPA (risk profiles II and III; risk profile I was not analyzed because the sample size was too small in the control group [n = 15]). During the SCD, athletes with the highest risk profile (III) showed overall greater beneficial changes with TNMT than those with lower risk profiles (I and II). Among the high-risk athletes, there was a significant treatment effect on the maximum trunk flexion angle (TNMT: mean [SE] increase, 4.66° [1.99°]; control: mean [SE] decrease, 8.23° [2.70°]; P = .01) and the maximum trunk extension angle (TNMT: mean [SE] decrease, 4.10° [2.61°]; control: mean [SE] increase, 9.09° [3.53°]; P = .03) during the SCD. In addition, the treatment effect was borderline significant in the highest risk profile group for the hip external rotation moment impulse during the SLD in the TNMT and control groups (mean [SE], –0.06 [0.07] Nm/kgs and 0.21 [0.09] Nm/kg-s, respectively; P = .08). However, there were no significant treatment effects in the highest risk profile group during the SLD for the hip external rotation moment in the TNMT and control groups (mean [SE], –0.49 [2.03] Nm/kg and –1.21 [2.80] Nm/kg, respectively; P = .87).
There were also no significant effects in the KAM when analyzed by risk profile.
Discussion
The present study provides evidence for utilizing trunk- and hip-focused neuromuscular training programs to reduce bio-mechanical and neuromuscular risk factors associated with first-time ACL injuries. The mechanisms underlying the effectiveness of TNMT as an element of ACL injury prevention programs have been shown, including changes in trunk and hip kinematics and kinetics. Exclusively addressing proximal factors with the TNMT program did not, however, result in significant changes in frontal-plane knee loading. The study also suggests that the greatest effect of TNMT programs may be observed among patients who are at the greatest risk for future injuries.
The present study provides an evidence-based rationale for trunk- and hip-focused neuromuscular training programs. Changes in frontal-plane hip kinematics were more than twice as great as the effects of previously described plyometric and balance training programs.26 We are unaware of previous investigations that describe changes in trunk kinematics after an ACL injury prevention program. Trunk displacement has been shown to increase the risk of knee, knee ligament, and ACL injuries with a high sensitivity and specificity in female athletes.34 Greater torso lean and trunk rotation toward the support leg are related to increasing external knee abduction loads.35 Thus, controlled activities that elicit trunk motion toward the support leg may help athletes learn better control of these risky knee loads, which may not be completely avoidable during high-level sports activities.2 Neuromuscular control of the hip is required to control frontal-plane trunk and pelvis motion. The external hip abduction moment created by the ground-reaction force moving lateral to the center of the femoral head is counterbalanced internally by hip adductor torque to adduct the pelvis and move the trunk toward the midline.33 Poor neuromuscular control of the posterior and lateral hip musculature may affect the generation of optimal net hip joint moments required to control hip motion upon landing. Therefore, exercises that promote large hip extension and external rotation moments should elicit powerful contractions of the target musculature including hip extensors, abductors, and external rotators.2 Although weakness of these muscle groups may not be strongly related to frontal-plane hip and knee mechanics,29,32 recent evidence links muscle activation deficits to poor control of the lower extremities.30,31
TNMT is a composite of published exercises that were derived or adapted for all progressions. Consequently, there is overlap with previously published ACL injury prevention programs. The effectiveness of the Fédération Internationale de Football Association (FIFA) 111 program in preventing lower extremity injuries among soccer athletes has been documented.8,22 The FIFA 111 program is composed of running, strength, plyometric, and balance exercises that are performed during a team warm-up and supervised by a team coach. There are 3 performance levels for each exercise, and correct lower extremity and trunk alignment cues are emphasized through verbal instruction. All drills are performed on the soccer field, and the only additional equipment necessary is cones. Finally, the FIFA 111 program was developed specifically to prevent injuries among soccer athletes. In contrast, TNMT does not include running drills. Each exercise has 5 levels of performance to provide a paradigm that accommodates beginner to advanced abilities. In this study, exercises were performed as part of the team warm-up and supervised by an athletic trainer. We believe that this level of supervision and feedback is critical to ensure correct lower extremity and trunk alignment, particularly for patients classified as high risk. TNMT is not sport specific but is generalizable to athletes who participate in jumping, cutting, and pivoting sports. Finally, TNMT utilizes equipment that provides an unstable base of support, introducing an advanced challenge to core control and lower extremity alignment. We are unaware, however, of studies that have evaluated the effects of the FIFA 111 program on biomechanical and neu-romuscular characteristics. Future studies will be necessary to compare and contrast the effects of the 2 training programs on biomechanical and neuromuscular characteristics as well as injury rates.
There are limitations to this study. The purpose of the study was to investigate the biomechanical and neuromus-cular effects of TNMT. The effect of training on the incidence of ACL injuries was not evaluated. A clinical trial will be necessary to assess if the changes in trunk and hip movement patterns after TNMT impact injury rates. We were not able to examine the treatment effects among participants with risk profile I (low) because of the limited number of participants in one of the treatment groups. The comparative effectiveness of TNMT was not evaluated. Future studies comparing the effects of distinct training interventions on biomechanical and neuromuscular characteristics, as well as injury rates, will enhance ACL injury prevention strategies. Finally, the delineation of risk groups was performed by assessing 3-dimensional movement pat-terns.4 It will be necessary to develop a clinical equivalent of the screening examination to integrate risk classification as a widespread strategy for ACL injury prevention.
Conclusion
The findings of this study provide greater understanding of the interaction between biomechanical and neuromuscular risks underlying the mechanics of an ACL injury and specific risk factors, which may help to predict risks. Combined with findings in our previous work,4 the clustering of biomechanical and neuromuscular risk factors associated with increased KAMs (and thus an increased risk for ACL injuries) also successfully delineates those young female athletes who will preferentially benefit from preventive, core stability–based intervention protocols. The study results suggest that training that addresses proximal factors alone is not adequate to address frontal-plane knee loading. These findings also demonstrate the clinical significance of LPA to determine which female participants most benefit from TNMT. The findings also demonstrate that those young athletes undergoing and completing pubertal maturation are most likely to benefit from this training.
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: The authors acknowledge funding support from National Institutes of Health/NIAMS Grants R21AR065068-01A1, U01AR 067997, and R21AR069873.
The authors acknowledge Kim, Chris, Staci, and Dai, as well as the Boone County School District.
References
- 1.Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23(6):617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- 2.Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777–792. doi: 10.2519/jospt.2013.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford KR, Myer GD, Hewett TE. Longitudinal effects of maturation on lower extremity joint stiffness in adolescent athletes. Am J Sports Med. 2010;38(9):1829–1837. doi: 10.1177/0363546510367425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD. Utilization of ACL injury biomechanical and neuromuscular risk profile analysis to determine the effectiveness of neuromuscular training. Am J Sports Med. 2016;44(12):3146–3151. doi: 10.1177/0363546516656373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 6.Hewett TE, Myer GD. The mechanistic connection between the trunk, hip, knee, and anterior cruciate ligament injury. Exerc Sport Sci Rev. 2011;39(4):161–166. doi: 10.1097/JES.0b013e3182297439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 8.Junge A, Lamprecht M, Stamm H, et al. Countrywide campaign to prevent soccer injuries in Swiss amateur players. Am J Sports Med. 2011;39(1):57–63. doi: 10.1177/0363546510377424. [DOI] [PubMed] [Google Scholar]
- 9.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 10.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 11.McCambridge TM, Myer GD. STOP anterior cruciate ligament injuries. Orthopedics. 2013;33(1) [Google Scholar]
- 12.Mendiguchia J, Ford KR, Quatman CE, Alentorn-Geli E, Hewett TE. Sex differences in proximal control of the knee joint. Sports Med. 2011;41(7):541–557. doi: 10.2165/11589140-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42(7):614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neu-romuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27(3):425–448, ix. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myer GD, Ford KR, Brent JL, Divine JG, Hewett TE. Predictors of sprint start speed: the effects of resistive ground-based vs. inclined treadmill training. J Strength Cond Res. 2007;21(3):831–836. doi: 10.1519/R-20886.1. [DOI] [PubMed] [Google Scholar]
- 16.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in”high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in low-risk” athletes. BMC Muscu-loskelet Disord. 2007;8:39–45. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 19.Myer GD, Stroube BW, DiCesare CA, et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. Am J Sports Med. 2013;41(3):669–677. doi: 10.1177/0363546512472977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203–215. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Myklebust G, Skjolberg A, Bahr R. ACL injury incidence in female handball 10 years after the Norwegian ACL prevention study: important lessons learned. Br J Sports Med. 2013;47(8):476–479. doi: 10.1136/bjsports-2012-091862. [DOI] [PubMed] [Google Scholar]
- 23.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2006;125(9):614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 24.Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94(9):769–776. doi: 10.2106/JBJS.K.00467. [DOI] [PubMed] [Google Scholar]
- 25.Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. doi: 10.1136/bmj.a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football: a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 27.Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714–723. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46(14):979–988. doi: 10.1136/bjsports-2011-090895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Willson JD, Davis IS. Lower extremity strength and mechanics during jumping in women with patellofemoral pain. J Sport Rehabil. 2009;18(1):76–90. doi: 10.1123/jsr.18.1.76. [DOI] [PubMed] [Google Scholar]
- 30.Willson JD, Kernozek TW, Arndt RL, Reznichek DA, Scott Straker J. Gluteal muscle activation during running in females with and without patellofemoral pain syndrome. Clin Biomech. 2011;26(7):735–740. doi: 10.1016/j.clinbiomech.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 31.Willson JD, Petrowitz I, Butler RJ, Kernozek TW. Male and female gluteal muscle activity and lower extremity kinematics during running. Clin Biomech. 2012;27(10):1052–1057. doi: 10.1016/j.clinbiomech.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 32.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41(9):625–632. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 33.Winter DA. Biomechanics and Motor Control of Human Movement. 3rd. New York: John Wiley & Sons; 2005. [Google Scholar]
- 34.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 35.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective study. Am J Sports Med. 2007;35(3):368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]


