Abstract
Background
Children exposed to multiple stressors are more likely to be overweight, but little is known about the mechanisms explaining this association.
Purpose
This cross-sectional study examined whether children exposed to multiple stressors had higher waist circumference, and whether this association was mediated through children’s television time.
Methods
Participants were 319 parent-child dyads. Children were 2–5 years old and had at least one overweight parent (BMI ≥ 25 kg/m2). Data were collected at baseline of a larger childhood obesity prevention study and included information on psychosocial stressors (e.g., parenting stress), demographic stressors (e.g., low income), children’s television time, and children’s waist circumference. Two cumulative risk scores were created by summing stressors in each domain (demographic and psychosocial). Mediation and moderated mediation analyses were conducted.
Results
Indirect effects of both cumulative risk scores on waist circumference through television time were not significant; however, moderated mediation analyses found significant moderation by gender. The indirect effects of both risk scores on waist circumference through television time were significant and positive for girls, but near-zero for boys.
Conclusions
Reducing television time should be explored as a strategy for buffering against the negative health effects of exposure to multiple stressors among girls. Longitudinal and intervention research is needed to confirm these results, and to identify mediating factors between cumulative risk and body weight among boys.
Keywords: Cumulative risk, stressors, family stress, environmental factors, childhood overweight, childhood obesity, body weight, waist circumference, television viewing, mediation, moderation, sex differences
More than 20% of children ages two to five in the United States are overweight or obese (1). Increasing attention is being paid to this age group (2,3), as evidence indicates that being overweight in early childhood increases a child’s risk of being an unhealthy weight later in life (4,5) and is associated with poor health outcomes and premature death in adulthood (6,7). Children’s home and family environments play a critical role in the development of obesity. Specifically, research indicates that a variety of psychosocial stressors in a child’s environment may increase his or her risk of becoming overweight, including parental stress (8–11) and household chaos or a lack of routines (12,13) among others. Additionally, children who have parents with certain demographic characteristics (e.g., a parent who is unmarried, has lower income, or has lower educational attainment) are also at greater risk for being an unhealthy weight (6,12,14).
Researchers typically assess how the aforementioned risk factors influence child outcomes independently of, or holding constant, other risk factors. However, risks often co-occur, and modeling risk factors independently may fail to capture the ways in which exposure to multiple, simultaneous risks affect health and development. For example, the child developmental and clinical psychological literatures suggest that some individual stressors may have only a marginal impact on behavior or health outcomes, but experiencing multiple stressors simultaneously can affect the child in ways a single risk factor did not (15,16). Moreover, a large body of evidence indicates that children exposed to several risk factors concurrently have significantly worse cognitive, social, and emotional outcomes than children exposed to just one risk factor (15). Accordingly, some researchers use ‘cumulative risk’ models that account for an accumulation of risks, rather than the presence or strength of any particular risk factor holding constant levels of other risk factors, when examining how environmental stressors influence childhood outcomes (15–17).
In spite of its potential relevance, very few studies have used the cumulative risk framework to study childhood weight outcomes (18–20). There has been even less attention to the factors that might mediate associations between cumulative risk and childhood weight, with only one study on this question to date: Evans et al. found that children exposed to greater cumulative risk at age nine exhibited larger increases in BMI at 13, and that this differential increase was mediated through children’s self-regulation abilities (19). To our knowledge, there are no other studies that examine the mediators between cumulative risk and weight outcomes, despite the potential for mediation analyses to identify potential targets for intervention.
The literature also suggests that children exposed to risks in more than one domain have worse outcomes than children exposed to risk in only one domain (15). Hence, some researchers have advocated for conceptualizing cumulative risk across different domains, and suggested several potential candidates for defining these domains of risk (15). In the developmental and child psychology literature, one categorization that has proven informative is to divide stressors into demographic risks (e.g., poverty, family structure, parental socioeconomic status) and psychosocial risks (e.g., parental stress, chaos in the home) (15,19,21,22). For example, the aforementioned study by Evans et al. (19) conceptualized cumulative risk as the total accumulation of stressors across three domains: sociodemographic (e.g., poverty), physical (e.g., substandard housing), and psychosocial (e.g., family turmoil). However, no studies have examined how risks across different domains influence young children’s weight outcomes.
The present study addresses these gaps in the literature by examining the association between children’s weight outcomes and cumulative risk exposure in two domains. Specifically, we examine risk factors in the psychosocial domain (i.e., chaos in the home, inconsistent parenting, low parenting sense of competence, parental stress, parental emotion dysregulation), and in the demographic domain (i.e., low family income, low parent education, parent unmarried/not living with a partner). Risk factors were selected based on previous studies linking these or similar factors to a broad range of adverse childhood outcomes, as well as evidence to suggest that this particular combination of risk factors may elevate the risk for child overweight in particular (9, 18–20, 23–27). We also test one potential pathway through which the accumulation of these stressors may impact children’s health, asking whether the effect of cumulative risk on weight outcomes is mediated through children’s television viewing. Previous research suggests that stressed parents may use television to occupy their children (28–30); in turn, TV viewing is known to be positively associated with excess weight in children (31). Thus, children in stressed households might watch more TV and, in turn, have worse weight outcomes. Because others have found differences between boys and girls in how television viewing affects weight outcomes (32–35), this study also examines the moderating role of sex using a moderated mediation model. We hypothesized that both cumulative psychosocial and cumulative demographic risk would be positively related to children’s weight outcomes, and that these associations would operate, at least in part, through the child’s television viewing. No specific predictions were made about how a child’s sex would influence the relationship between television viewing and weight outcomes.
Methods
This study used baseline data from the “My Parenting SOS” study (trial number NCT00998348), a 35-week obesity prevention intervention trial for families with preschool-age children (36). Study procedures were approved by the Institutional Review Board at the University of North Carolina, Chapel Hill.
Participants and Data Collection
Participants were English-speaking families (n = 319) with at least one child two to five years of age and at least one parent or guardian with a body mass index (BMI) greater than 25 kg/m2 (based on self-reported height and weight). Prior to randomization, parent-child dyads attended an in-person measurement event to complete baseline data collection. At these events, research staff collected children’s anthropometric measurements using standard protocols, and parents completed a series of self-administered questionnaires, providing information about their demographic characteristics, parenting practices, and children’s television time. At the end of the event, children were fit with an accelerometer to wear for one week.
Measures
Anthropometrics
Trained research staff measured children’s standing height, weight, waist circumference, and skinfold thickness. Height was measured to the nearest 1/8 inch using a Shorr (Olney, MD) or Seca (Columbia, MD) measuring board. Weight was measured to the nearest 0.1 lb using a Seca 770 portable electronic scale (Columbia, MD). Waist circumference was measured to the nearest 0.1 cm using a Gulick II measuring tape. Triceps and subscapular skinfold thickness was measured to the nearest 1.0 mm using Lange calipers (Beta Technology, Inc., Columbia, MD). During measurements, staff recorded the child’s sex. These measures, along with parent-reported birthdate of the child, were used to calculate BMI, BMI percentile, and overweight status (defined as ≥ 85th percentile of BMI for age- and sex).
Demographics
Parent demographic questionnaires captured the respondent’s age, race/ethnicity, relationship to the child (mother, father, grandmother, etc.), educational attainment, total household income, and family structure. Due to small cell sizes, race responses were collapsed into either white or non-white; the non-white category included African American, Asian American/Pacific Islander, Native American, mixed race, other race, and Hispanic. Parent sex was derived from the respondent’s self-reported relationship to the child. Parents also reported their educational attainment from five categories (less than high school, high school or GED, some college or technical school, college graduate, and masters/doctoral degree) and total annual household income from three categories (less than $25,000; $25,000 to $50,000; and more than $50,000). Family structure was assessed by asking parents to indicate whether they were married/living with a partner, single/never married, or divorced/separated.
Parenting practices
Parent surveys incorporated several existing questionnaires to assess parenting practices. To reflect the psychosocial stressors commonly found to be predictors of child outcomes, five scales were extracted for this study: chaos in the home, inconsistent parenting, parenting confidence, parental stress, and parental emotion dysregulation. Model fit of all scales was examined in the study sample, at times necessitating slight modifications to the original scales.
Chaos in the home was measured with the Confusion, Hubbub, and Order Scale (CHAOS) (37). The scale consists of 15 true/false items about environmental chaos in the home and the use of routines. Responses were coded as 0 or 1, with 1 indicating greater chaos, and then summed for a total CHAOS score (possible range 0 to 15; Cronbach’s alpha = 0.82).
Inconsistent parenting was assessed with a scale from the Alabama Parenting Questionnaire – Preschool Revision (APQ-PR) (38). Items ask respondents to indicate how often (1–5, “never” to “always”) they typically engage in various parenting behaviors. The inconsistent parenting scale includes eight items such as, “The punishments you give your child depend on your mood.” Responses were summed to create a score for inconsistent parenting (range 8 to 40; Cronbach’s alpha = 0.79).
Parenting confidence was assessed with the Parenting Sense of Competence (PSOC) scale (39). This scale includes items related to parenting self-efficacy (e.g., “Being a parent is manageable, and any problems are easily solved”) and parenting satisfaction (e.g., ”Even though being a parent could be rewarding, I am frustrated now while my child is at his/her present age”). Responses were coded as 1 to 6 (“strongly disagree” to “strongly agree”), with reverse coding as appropriate. One item (“Being a parent makes me tense and anxious”) from the original scale was eliminated following the factor analysis. The remaining 15 items were summed to create a total parenting confidence score (range 15 to 90; Cronbach’s alpha = 0.85).
Parental stress was assessed using the Parenting Stress Index Short Form (PSI-SF) (40). The PSI-SF examines general parental distress, dysfunction in the parent-child relationship, and the respondents’ perception that they have a difficult-to-manage child. For example, respondents rate their agreement (1–5, “strongly disagree” to “strongly agree”) with statements such as “I often have the feeling that I cannot handle things very well.” Scores on the 36 items were summed to create a total score (range 36–180; Cronbach’s alpha = 0.93).
Finally, parental emotion dysregulation was assessed with the Difficulty in Emotion Regulation Scale (DERS) (41). For this scale, respondents indicate how often 36 statements apply to their life (1–5, ”almost never” to “almost always”). Scores on six domains (non-acceptance of emotional responses, difficulty engaging in goal-directed behavior, difficulty controlling impulses, lack of emotional awareness, limited access to emotion regulation strategies, and lack of emotional clarity) were summed to create the DERS total score (range 36–180; Cronbach’s alpha = 0.95).
Television viewing
Parent surveys included two items about their children’s television viewing habits. Following previous work (see [42] for a review), parents reported TV time separately for weekdays vs. weekends, answering two items regarding the total number of hours of television their child watched during the last five weekdays and during the last two weekend days. These variables were used to calculate average hours of TV viewing per day across the entire week. Values greater than 16 hours per day were deemed implausible (i.e., more than the number of hours most children are awake in a day) and, in the two cases in which this occurred (<1% of sample), responses were recoded as missing. Similar measures of television viewing time have been found in previous studies to be sufficiently reliable (42) and to be correlated with objective measures of TV time (e.g., videotaped observations of children’s television viewing; 43) and with viewing diaries (44).
Physical activity
Child physical activity was assessed using ActiGraph GT3X accelerometers (Fort Walton Beach, FL) programmed with a 15-second epoch. Children wore the monitors over the right hip for seven consecutive days during waking hours, except when in water. Children’s time in sedentary and moderate-to-vigorous physical activity was calculated using the cut-points developed by Evenson et al. (45).
Plan of Analysis
Following a common approach to calculating cumulative risk scores (15), we dichotomized all risk variables as present/absent. Clinical/standardized cutoffs were available for two scales: parenting confidence, for which we used an existing cut point (adjusted to reflect our use of 15 instead of 16 items) of 47 or lower to indicate low parenting confidence (46); and parenting stress, for which we used Abidin’s (38) cutoff of 90 or greater for ‘high’ parental stress. The remaining three psychosocial risk factors (chaos in the home, inconsistent parenting, and parental emotion dysregulation) have no published standardized cutoffs; for these variables, we followed previous literature (16,19,25,47) by applying quartile cut points. Specifically, observations were coded as “high risk” if they were in the top quartile of chaos in the home (CHAOS score ≥ 7.0), frequency of inconsistent parenting (inconsistent parenting score ≥ 20.0), and parental emotion dysregulation (DERS score ≥ 81.0). Variables incorporated into the demographic risk score included income, educational attainment, and marital status. Following others (19,20,23,25), we coded being unmarried or not living with a partner as ‘high risk.’ We coded as ‘high risk’ families with income less than $50,000, which reflects those living below the median income for the geographic area from which the sample was drawn (48). Finally, we considered those with educational attainment of ‘some college’ or less as having ‘low education,’ as this reflected approximately the lowest quartile in educational attainment in the sample (22.9% reported some college or less).
Analyses were conducted in SAS Version 9.4 (SAS, Cary, NC). Descriptive statistics were run for individual items, derived scales, anthropometrics, and physical activity. No items or constructed scales had more than 5% of cases with missing data, with the exception of accelerometer measures, which were missing from approximately 12% (n = 41) of cases. To avoid a loss of power, physical activity and sedentary time were only included in sensitivity analyses (see below). We used multiple regression and mediation analyses to examine the relationship between cumulative risk scores, television viewing, and waist circumference. We used standard diagnostic procedures (e.g., examining plots of residuals, examining bivariate correlations, estimating variance inflation factors) to check regression assumptions (e.g., linearity, homoscedasticity, multicollinearity) and did not identify any violations. Models included both risk scores simultaneously. We also examined an interaction term between the two risk scores, but found no evidence of interaction, and thus final models did not retain this term. Child’s age and sex and parent’s age, race/ethnicity, and sex were controlled in all models.
Analyses proceeded in several steps. First, we used multivariate regression to examine whether either of the two cumulative risk scores (psychosocial risk and demographic risk) were related to waist circumference. We also examined the possibility that a single risk factor could drive the relationships between the cumulative risk scores and waist circumference by estimating regression models in which each risk factor was entered as a separate variable (rather than as part of the cumulative risk score) and modeled as a continuous variable when appropriate (i.e., using scale scores rather than dichotomized risk factors).
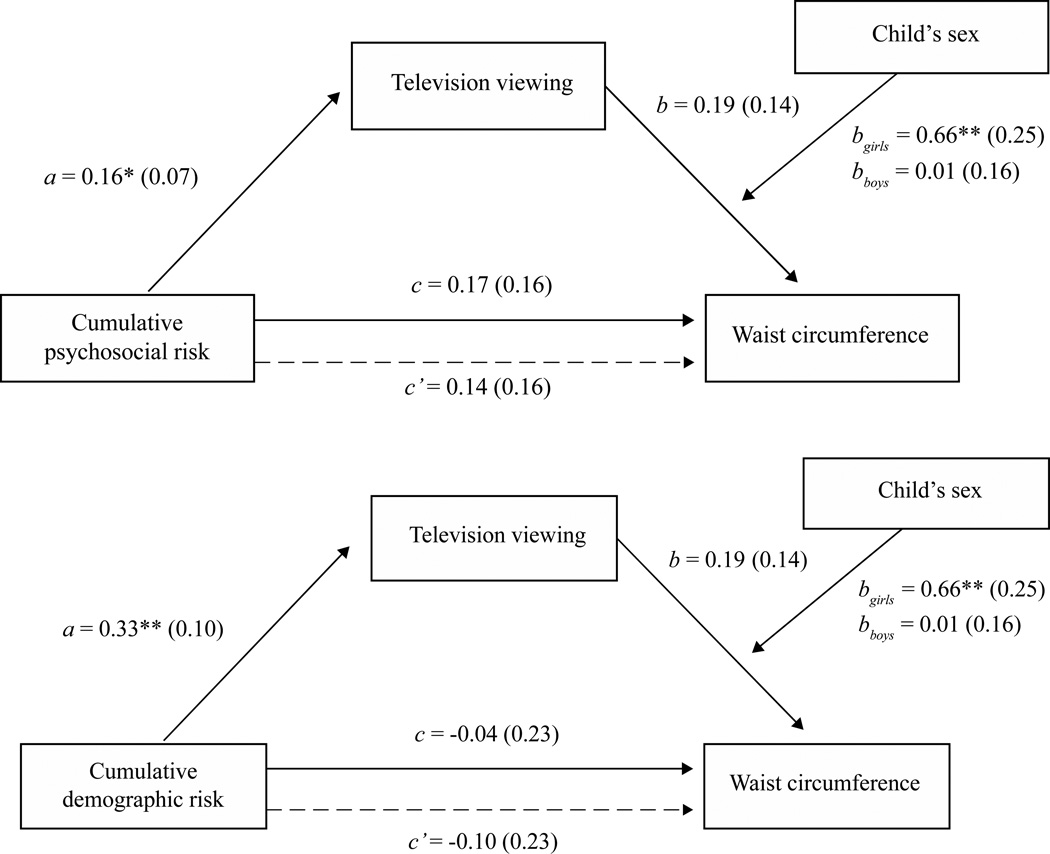
Next, we estimated mediation and moderated mediation models using the PROCESS macro for SAS (49). As described in detail elsewhere (49), methodologists now suggest that rather than relying on the ‘causal steps’ approach (50), researchers test mediation hypotheses by estimating the size of the indirect association using a set of regressions, and evaluating the statistical significance of the indirect association using bootstrapped confidence intervals. The indirect association between cumulative risk and waist circumference through television viewing is quantified as the product of the effect of cumulative risk on television viewing (a in Figure 1, both panels) and the effect of television viewing on waist circumference, controlling for cumulative risk (b in Figure 1, both panels). The indirect effect (a*b) is considered statistically significantly different from zero if the bootstrapped confidence interval for the product a*b does not contain zero. To examine indirect associations, we used model 4 in PROCESS with bias-corrected bootstrapped confidence intervals using 5,000 repetitions.
Figure 1.
Indirect effect of cumulative risk on waist circumference through television viewing. This figure shows the indirect effect of cumulative psychosocial risk on waist circumference through television viewing (top) and of cumulative demographic risk on waist circumference through television viewing (bottom). Unstandardized OLS coefficients (with standard errors in parentheses) are reported. a is the effect of cumulative risk on television viewing; b is the effect of television viewing on waist circumference, controlling for cumulative risk. bgirls and bboys indicate the effect of television on waist circumference for girls and boys, respectively, when this effect is allowed to vary by child’s sex. c is the effect of cumulative risk on waist circumference without including television viewing as a mediator. The dotted line and c’ denote the effect of cumulative risk on waist circumference when including television viewing as a mediator and allowing the effect of television to vary by child’s sex (i.e., a moderated mediation model).
* p<0.05; ** p<0.01.
Finally, we examined whether the relationship between television viewing and waist circumference was moderated by child’s sex. To test for moderation, we regressed waist circumference on cumulative risk, television time, covariates (including child’s sex), and an interaction between television viewing and child’s sex. The interaction term allowed the effect of television time on waist circumference to vary with child’s sex. Next, we estimated a moderated mediation model using PROCESS model 14 to examine whether the indirect effect of cumulative risk on waist circumference through television viewing was significantly moderated by child’s sex. We computed the conditional indirect effects and simple slopes at each level of the moderator (i.e., for girls and for boys) using PROCESS and PROC GLM, respectively.
We ran four sensitivity analyses to check the robustness of the results. First, several of our risk factors lacked standardized or clinical cutoffs to establish who was at “high risk.” In these cases, we assigned risk scores using statistical cutoffs (e.g., riskiest quartile was assigned to “high risk” category) or logical thresholds (e.g., children with an unmarried parent were assigned to “high risk” category). To examine whether results were sensitive to using these particular cut-points to assign risk scores, we created revised ordinal cumulative psychosocial and demographic risk scores using alternative thresholds to dichotomize each risk factor. Specifically, we used tertile cutoffs (i.e., riskiest one-third of the sample assigned to the “high risk” category) for the risk factors for which we initially used quartile cut-points (CHAOS, inconsistent parenting, parenting sense of competence, parenting stress, and emotion dysregulation), an alternative definition of low-income (<$25,000/year in annual household income, instead of <$50,000 in the initial specification), and an alternative specification of low educational attainment (high school degree or less, compared to some college or less in the initial specification). We then re-ran the mediation and moderated mediation models using these alternative cut points for creating the ordinal cumulative psychosocial and cumulative demographic risk scores. Second, we repeated the original mediation and moderated mediation analyses after including children’s sedentary time and moderate-to-vigorous physical activity time as covariates. Third, we repeated the original mediation and moderated mediation analysis, using the original cut points for risk scores, but this time examining children’s BMI percentile instead of waist circumference as the outcome variable.
Additionally, while there is a long tradition in the cumulative risk literature of dichotomizing risk factors and summing these dichotomous variables to produce an ordinal cumulative risk score and using this ordinal variable in regression analysis, there are also drawbacks to this approach, and some recommend specifying continuously-scaled cumulative risk scores when possible (24). Thus, in our fourth sensitivity analysis, we conducted the mediation and moderated mediation analyses with waist circumference as the outcome and using continuously-scaled composite risk scores (rather than ordinal cumulative risk scores) as the key independent variables. We created the composite cumulative psychosocial risk scores by standardizing responses on the five psychosocial risk variables and summing these z-scores. Our composite cumulative demographic risk variable follows Fiese and colleagues (20) in assigning a score of +1 to those who are unmarried (indicating higher risk) and -1 to those who are married, and sums this value with standardized scores for the household income and educational attainment variables.
Results
Sample Characteristics
A total of 319 parent-child dyads provided data. About 13.8% of the sample (n=44) had missing data on one or more items and were dropped from analysis to allow for consistent samples across models. Children were, on average, 42.27 months old (SD = 9.85) (Table 1). About half (49.09%) of child participants were female, while 93.1% parent participants were female. About half of parents (52.36%) self-identified as white; the remaining 47.64% identified as non-white. Of those who identified as non-white (n = 131), 81.68% (n = 107) identified as Black or African American, 6.87% (n = 9) identified as Asian American/Pacific Islander, 2.29% (n = 3) identified as Native American, 7.63% (n = 10) identified as mixed race, and 1.53% (n = 2) identified as ‘Other’ (data not shown in Table). Parents had an average age of 34.96 years (SD = 6.02). About two-fifths of parent respondents had completed a college degree (42.91%), with another 34.18% completing an advanced degree. About 12.00% of families earned $25,000 or less per year, and another 24.00% had total annual household incomes between $25,000 and $50,000. Just over three-quarters (78.18%) were married or living with a partner.
Table 1.
Sample characteristics (n=275)
| N (%) or Mean (SD) | |
|---|---|
| Child Characteristics | |
| Age (months) | 42.27 (9.85) |
| Female | 135 (49.09%) |
| Anthropometrics | |
| Body mass index (BMI) percentile | 58.76 (28.70) |
| Overweight or obese (≥85th percentile BMI) | 71 (25.82%) |
| Waist circumference (cm) | 49.79 (3.57) |
| Parent and Household Characteristics | |
| Female | 256 (93.09%) |
| Age (years) | 34.96 (6.02) |
| Race/ethnicity | |
| White | 144 (52.36%) |
| Non-whitea | 131 (47.64%) |
| Educational attainment | |
| High school or less | 12 (4.36%) |
| Some college | 51 (18.55%) |
| College graduate | 118 (42.91%) |
| More than college | 94 (34.18%) |
| Total household income | |
| Less than $25,000 | 33 (12.0%) |
| $25,000 to $50,00 | 66 (24.00%) |
| More than $50,000 | 176 (64.00%) |
| Family structure | |
| Married/living with a partner | 215 (78.18%) |
| Single/never married | 41 (14.91%) |
| Divorced/separated | 19 (6.91%) |
Includes Black/African American, Hispanic/Latino, Asian American/Pacific Islander, Native American, and Mixed race.
Risk Scores
Children were exposed to an average of 1.29 psychosocial risk factors (SD =1.49; range 0–6) (Table 2). About one-fifth (21.45%) of children were exposed to one psychosocial risk factor, 17.09% to two risk factors, 10.91% to three risk factors, and 8.36% to 4 or more risk factors. On average, children experienced 0.81 demographic risk factors (SD = 1.05, range 0–3). Over half (56.00%) of the sample was exposed to no demographic risk factors. However, there was still sufficient variability in cumulative demographic risk, with 18.18% being exposed to one risk factor, 14.91% to two risk factors, and 10.91% to three risk factors.
Table 2.
Psychosocial and demographic risk exposure (n =275)
| N (%) or Mean (SD) | |
|---|---|
| Psychosocial Risk Exposure | |
| Individual psychosocial risk factor exposure | |
| Confusion, Hubbub, and Order Scale total score | 4.36 (3.32) |
| Alabama Parenting Questionnaire Preschool Revision inconsistent parenting subscale | 17.34 (4.25) |
| Parenting Sense of Competence total score | 63.02 (11.69) |
| Parenting Stress Index Short Form total score | 75.08 (19.74) |
| Difficulty in Emotion Regulation Scale total score | 67.21 (19.90) |
| Cumulative psychosocial risk exposure | |
| Cumulative psychosocial risk score | 1.29 (1.49) |
| Psychosocial risk factors experienced | |
| 0 | 116 (42.18%) |
| 1 | 59 (21.45%) |
| 2 | 47 (17.09%) |
| 3 | 30 (10.91%) |
| 4 or more | 23 (8.36%) |
| Demographic Risk Exposure | |
| Individual demographic risk factor exposure | |
| Low household income (< 50k/year) | 99 (36.00%) |
| Low education (some college or less) | 63 (22.91%) |
| Unmarried / not living with partner | 60 (21.82%) |
| Cumulative demographic risk exposure | |
| Cumulative demographic risk score | 0.81 (1.05) |
| Demographic risk factors experienced | |
| 0 | 154 (56.00%) |
| 1 | 50 (18.18%) |
| 2 | 41 (14.91%) |
| 3 | 30 (10.91%) |
Cumulative Risk Exposure and Waist Circumference
Regression analyses indicated that a child’s exposure to cumulative psychosocial risk was positively but not significantly related to their waist circumference (unstandardized coefficient = 0.17, p = 0.28; c in Figure 1, top panel), while cumulative demographic risk did not show a strong relationship (unstandardized coefficient = −0.04, p = 0.86; c in Figure 1, bottom panel). The only covariate from this model significantly related to waist circumference was child’s age (unstandardized coefficient = 0.14, p <0.001). In the regression models with each risk factor entered separately, no individual risk factor explained a significant portion of the variance in waist circumference (all p’s > 0.10; results not shown).
Mediating Effect of Television Viewing
In the simple mediation model, we found that children exposed to more psychosocial risk factors tended to watch more hours of television per day (unstandardized coefficient = 0.16, p = 0.02; a in Figure 1, top panel). Similarly, children exposed to more demographic risk factors also watched more hours of television per day (unstandardized coefficient = 0.33, p = 0.001, a in Figure 1, bottom panel). In turn, children who watched more hours of television per day had higher waist circumferences (unstandardized coefficient = 0.19, b in Figure 1, both panels), though this relationship did not reach statistical significance (p = 0.17). The product of these two paths, a*b, is the indirect effect of cumulative risk on waist circumference through television viewing. For cumulative psychosocial risk, this indirect effect was 0.16 * 0.19 = 0.030 and was not significantly different from zero at the 95% confidence level (95% CI: −0.005, 0.097). A child exposed to one additional psychosocial risk factor would be predicted to watch an additional 0.16 hours of television per day, which in turn is predicted to increase waist circumference by 0.030 cm. For cumulative demographic risk, the indirect effect was 0.33 * 0.19 = 0.063 and was again was not significantly different from zero (95% CI: −0.013, 0.166). A child with one additional demographic risk factor is predicted to watch an average of 0.33 additional hours of television a day, which in turn is predicted to increase the child’s waist circumference by 0.063 cm.
Moderating Role of Sex
Child’s sex significantly moderated the relationship between TV viewing and waist circumference (unstandardized coefficient on the interaction term = 0.65, p = 0.03). For girls, watching an additional hour of television is expected to increase waist circumference by 0.66 cm (p = 0.009; bgirls in Figure 1, both panels), while for boys, an additional hour of television is associated with a near-zero increase in waist circumference (0.01 cm, p = 0.95, bboys in Figure 1, both panels) (coefficients were estimated using PROC GLM as βTV + βTV*family = 0.0098 + 0.6482*female; where female is coded as 1 for girls and 0 for boys).
Additionally, moderated mediation analyses indicated that the indirect association a*b was moderated by the child’s sex. Hayes’s Index of Moderated Mediation (51), which reflects the difference between the indirect effect for girls and the indirect effect for boys, was significantly different from zero for both cumulative psychosocial risk (Index = 0.11; 95% CI: 0.02, 0.28) and cumulative demographic risk (Index = 0.21, 95% CI: 0.03, 0.49). Quantifying the indirect effects (a*b) for each sex also revealed the conditional nature of these associations. For girls, the indirect effect of cumulative psychosocial risk on waist circumference through television time was positive and statistically significant (point estimate: 0.11, 95% CI: 0.02, 0.28); for boys, the effect was close to zero and not statistically significant (point estimate: 0.002, 95% CI: −0.07, 0.05). Likewise, the indirect effect of cumulative demographic risk was positive and significant for girls (point estimate: 0.21; 95% CI: 0.06, 0.47), but non-significant for boys (point estimate: 0.003; 95% CI: −0.15, 0.08).
Sensitivity Analyses
All four sensitivity analyses confirmed the pattern of results (see Supplemental Tables 1–4 for detailed results). In the first sensitivity analysis using alternative thresholds for dichotomizing risk variables, we found a significant positive indirect effect of the cumulative risk scores through television time on waist circumference for girls (indicated by positive point estimates for both psychosocial and demographic risk variables and 95% CI’s that did not contain 0), and non-significant indirect effects for boys (indicated by 95% CI’s crossing 0). Likewise, in the second sensitivity analysis, we obtained similar results (positive and statistically significant indirect effects for girls for both psychosocial and demographic cumulative risk scores, and non-significant indirect effects for boys) when controlling for children’s sedentary time and moderate-to-vigorous physical activity time. We again found this pattern of results in the third sensitivity analysis using children’s BMI percentile as the outcome variable in place of waist circumference. Finally, when examining the cumulative risk scores as continuous rather than ordinal variables, we again found a positive and statistically significant indirect effects of both risk variables on waist circumference through television time for girls, but nearly zero and non-significant indirect effects among boys.
Discussion
Findings revealed that cumulative exposure to multiple risk factors in the psychosocial domain was positively (though not significantly) related to child waist circumference, while risks in the demographic domain were not strongly directly related to waist circumference. Our finding of a positive relationship between psychosocial risk and waist circumference is consistent with the handful of existing studies examining exposure to multiple risk factors and child weight outcomes (18–20). Our study extends these previous findings by investigating cumulative risk in very young children. To our knowledge, no other studies have examined childhood weight outcomes and cumulative demographic risk independently of other risk domains. We are also among the first to examine potential mechanisms linking cumulative risk to waist circumference. In the moderated mediation analyses, we found that children’s television time, a modifiable behavior, was a significant mediator of the relationship between cumulative risk exposure and child’s waist circumference among girls.
There are several mechanisms through which watching more television might be linked to excess weight. Some hypothesize that viewing television while eating may distract children from physiological satiety cues that would normally help them regulate their food intake; lack of attention to satiety cues may, in turn, increase caloric consumption (31). Others note that television viewing exposes children to more food advertisements, which increases children’s demand for these (typically unhealthy) food items. For example, longitudinal mediation studies have found that watching more television is associated with greater increases in BMI in part via increased consumption of the unhealthy foods commonly advertised on television (52).
Our moderated mediation analyses also revealed moderation by sex. Specifically, increased television time was significantly associated with higher waist circumference in girls only; for boys, the relationship was close to zero and not significant. In moderated mediation models, the indirect effects of both cumulative risk scores on waist circumference through television time were also conditional on the child’s sex. Others have examined sex as a moderator for the relationship between television time and weight, with some studies finding that television time is more strongly related to weight outcomes in girls than in boys (as ours did) (33,34,53), but at least one other study finding a stronger relationship among boys (35). It is not clear what accounts for these sex differences. It is possible that the mechanisms through which television influences weight operate differently in boys and girls. For example, perhaps preschool girls are more distracted by television (and thus less attentive to satiety cues) than boys, though this hypothesis has not yet been tested. It is also possible that girls and boys are exposed to different amounts or types of ads, or that girls respond differently than boys even to the same advertisements. For example, girls may have higher neural activation in response to food stimuli (54). Future research should explore the factors that might account for the differential relationship by sex between television time and weight outcomes. Studies might also examine other forms of screen time, such as using handheld devices like smartphones and tablets, particularly as these devices become increasingly common (55).
Our findings suggest that for preschool-aged girls experiencing multiple risk factors, reducing television time may be a successful obesity prevention strategy. We found that a one-hour reduction in television time was associated with a 0.64 cm reduction in waist circumference among girls. Television viewing is a modifiable behavior that has been successfully targeted by previous obesity prevention interventions (56,57). A benefit of using the cumulative risk model is that it can help identify children most in need of such interventions. Indeed, in the present study, no individual risk factor explained a significant amount of variance in children’s waist circumference. Instead, only the accumulation of multiple risks was associated with higher waist circumference, suggesting the interventionists must consider cumulative risk to identify children at greatest risk for overweight.
In contrast to previous work studying cumulative risk and weight outcomes in children (18–20), our study used waist circumference, rather than BMI or BMI-based weight categories (i.e., overweight/obese vs. healthy weight) as the primary outcome measure. While BMI is often used to assess weight outcomes, it does not perfectly detect unhealthy weight status in children (58) or adults (59). Additionally, BMI does not capture how fat is distributed in the body. Because central adiposity tends to be a better predictor of chronic health conditions than peripheral adiposity, some have argued that waist circumference, which helps quantify abdominal fatness, may be a more useful public health indicator than BMI (60–63). Previous work has indeed found that higher waist circumference is associated with disease risk factors and poor health outcomes in both children and adults (64–67). A strength of our study was examining this important indicator of unhealthy weight status.
As with all research, this study has limitations. First, we used cross-sectional data, which precludes establishing the direction of associations. That said, it may be less likely that child waist circumference or television time cause the sociodemographic or psychological risk factors we assessed. Still, the link between television time and overweight could plausibly be reciprocal: television time might cause children to become overweight, and children who become overweight might also choose to watch more television. Longitudinal and intervention studies that help families reduce key stressors would help to clarify the direction of the relationships studied here, and have the potential to improve child health outcomes. Another limitation is that all dyads in the study were participants in an obesity prevention intervention study, and, to be eligible, children needed to have at least one overweight parent at home. Having one or more overweight parent is a strong risk factor for childhood overweight (68) and, therefore, this eligibility criterion focused the study on an important population of children, we cannot say with certainty the results would generalize to children with normal weight parents. Third, participants in our sample had a relatively high socioeconomic status: more than half had annual household income greater than $50,000 and three-quarters had a college or advanced degree. As such, similar to our caution regarding parent overweight, our findings may not generalize to children raised in more socioeconomically diverse and/or lower SES families. That said, many children experienced cumulative psychosocial risk factors within this sample, and those that did also tended to have higher waist circumference. This highlights the importance of examining and intervening on a broad range of risk factors for childhood overweight, including parent- and household-level psychosocial risks such as household chaos, negative parenting practices, and parental stress, which are likely to vary within and between families regardless of SES.
Several strengths are also worth noting. We obtained objective anthropometric measures, and thus avoided the possibility of biased self-reporting of weight outcomes. Our results were also highly robust to a variety of sensitivity analyses: the pattern of results was maintained when controlling for accelerometer-measured physical activity and sedentary time, when using other outcome measures for childhood unhealthy weight, and when using several alternative specifications for creating the cumulative risk variables. We are also among the first to examine potential mediators between cumulative risk and child health outcomes. This information is important to understand as the public health community continues to search for new intervention strategies, particularly given that many childhood obesity prevention interventions to date have had only modest success (69). Psychosocial stressors and television time are both potentially malleable by public health interventions; intervening on these factors could help mitigate the negative effects of cumulative risk exposure on children’s weight outcomes.
Conclusions
This study suggests that exposure to multiple psychosocial risk factors is positively associated with worse weight outcomes in preschool-aged children (though the association is only moderate in magnitude), while demographic risk factor exposure is not directly related to waist circumference. For girls, the relationship between cumulative risk and waist circumference is mediated through time spent watching television. The results suggest that researchers and practitioners could benefit from considering the accumulation of risk factors when identifying children most vulnerable to excess weight gain. Households experiencing multiple psychosocial stressors (e.g., high parental stress, low parental sense of competence, high degrees of household chaos) may be particularly important to reach. Interventions will likely need to help parents address these stressors as part of any effort to help children achieve healthier weight outcomes. Additionally, reducing children’s television time may help buffer against the negative effects of these stressors, at least among girls. Future research should clarify whether these are causal relationships, as well as identify what accounts for the association between cumulative psychosocial risk and weight outcomes in boys.
Supplementary Material
Acknowledgments
This research was supported in part by a grant from the National Heart, Lung, and Blood Institute (R01 HL 091093). The project was conducted out of the Center for Health Promotion and Disease Prevention, a Prevention Research Center funded through a cooperative agreement with the Centers for Disease Control and Prevention (U48-DP005017). The findings and conclusions in this journal article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Birch LL, Parker L, Burns A, editors. Early Childhood Obesity Prevention Policies. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 3.Larson N, Ward DS, Neelon Benjamin S, Story M. Research Synthesis: Preventing Obesity among Preschool Children. Princeton, NJ: Robert Wood Johnson Foundation; 2011. [Accessed June 28, 2016]. http://files.eric.ed.gov/fulltext/ED541796.pdf. [Google Scholar]
- 4.Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nader PR, O’Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 6.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23(s2) doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 7.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 8.Koch F-S, Sepa A, Ludvigsson J. Psychological stress and obesity. J Pediatr. 2008;153(6):839–844.e3. doi: 10.1016/j.jpeds.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12(5):e54–e63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- 10.Stenhammar C, Olsson G, Bahmanyar S, et al. Family stress and BMI in young children. Acta Pædiatrica. 2010;99(8):1205–1212. doi: 10.1111/j.1651-2227.2010.01776.x. [DOI] [PubMed] [Google Scholar]
- 11.Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15(1):126–126. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 12.Anderson S, Whitaker RC. Household routines and obesity in US preschool-aged children. Pediatrics. 2010;125(3):420–428. doi: 10.1542/peds.2009-0417. [DOI] [PubMed] [Google Scholar]
- 13.Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. Ann Am Acad Pol Soc Sci. 2008;615(1):11–37. [Google Scholar]
- 14.Chen AY, Escarce JJ. Family structure and childhood obesity, Early Childhood Longitudinal Study - Kindergarten Cohort. Prev Chronic Dis. 2010;7(3):A50. [PMC free article] [PubMed] [Google Scholar]
- 15.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 16.Appleyard K, Egeland B, van Dulmen MHM, Alan Sroufe L. When more is not better: The role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46(3):235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- 17.Jones DJ, Forehand R, Brody G, Armistead L. Psychosocial adjustment of African American children in single-mother families: A test of three risk models. J Marriage Fam. 2002;64(1):105–115. [Google Scholar]
- 18.Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative social risk and obesity in early childhood. Pediatrics. 2012;129(5):e1173–e1179. doi: 10.1542/peds.2011-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans GW, Fuller-Rowell TE, Doan SN. Childhood cumulative risk and obesity: The mediating role of self-regulatory ability. Pediatrics. 2012;129(1):e68–e73. doi: 10.1542/peds.2010-3647. [DOI] [PubMed] [Google Scholar]
- 20.Fiese BH, Hammons A, Grigsby-Toussaint D. Family mealtimes: A contextual approach to understanding childhood obesity. Obes Fam Life Course. 2012;10(4):365–374. doi: 10.1016/j.ehb.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Dev. 2002;73(4):1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- 22.Furstenberg FF. Managing to Make It: Urban Families and Adolescent Success. Chicago, IL: University of Chicago Press; 1999. [Google Scholar]
- 23.Garasky S, Stewart SD, Gundersen C, Lohman BJ, Eisenmann JC. Family stressors and child obesity. Soc Sci Res. 2009;38(4):755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 25.Bagley EJ, El-Sheikh M. Familial risk moderates the association between sleep and zBMI in children. J Pediatr Psychol. 2013;38(7):775–784. doi: 10.1093/jpepsy/jst031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans GW, Kim P. Childhood poverty and health: Cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18(11):953–957. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- 27.Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and Body Mass Index trajectories through young adulthood. Am J Public Health. 2010;100(12):2507–2512. doi: 10.2105/AJPH.2009.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans CA, Jordan AB, Horner J. Only two hours?: A qualitative study of the challenges parents perceive in restricting child television time. J Fam Issues. 2011;32(9):1223–1244. [Google Scholar]
- 29.Jordan AB, Hersey JC, McDivitt JA, Heitzler CD. Reducing children’s television-viewing time: A qualitative study of parents and their children. Pediatrics. 2006;118(5):e1303–e1310. doi: 10.1542/peds.2006-0732. [DOI] [PubMed] [Google Scholar]
- 30.Chowhan J, Stewart JM. While mothers work do children shirk? determinants of youth obesity. Appl Econ Perspect Policy. 2014;36(2):287–308. [Google Scholar]
- 31.Marshall SJ, Biddle SJH, Gorely T, Cameron N, Murdey I. Relationships between media use, body fatness and physical activity in children and youth: A meta-analysis. Int J Obes. 2004;28(10):1238–1246. doi: 10.1038/sj.ijo.0802706. [DOI] [PubMed] [Google Scholar]
- 32.Chernin A. The Effects of Food Marketing on Children’s Preferences: Testing the Moderating Roles of Age and Gender. Ann Am Acad Pol Soc Sci. 2008;615(1):101–118. [Google Scholar]
- 33.Lazarou C, Soteriades ES. Children’s physical activity, TV watching and obesity in Cyprus: the CYKIDS study. Eur J Public Health. 2010;20(1):70–77. doi: 10.1093/eurpub/ckp093. [DOI] [PubMed] [Google Scholar]
- 34.Crespo C, Smit E, Troiano R, Bartlett SJ, Macera C, Andersen R. Television watching, energy intake, and obesity in US children: Results from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2001;155(3):360–365. doi: 10.1001/archpedi.155.3.360. [DOI] [PubMed] [Google Scholar]
- 35.Prentice-Dunn H, Prentice-Dunn S. Physical activity, sedentary behavior, and childhood obesity: A review of cross-sectional studies. Psychol Health Med. 2012;17(3):255. doi: 10.1080/13548506.2011.608806. [DOI] [PubMed] [Google Scholar]
- 36.Ward DS, Vaughn AE, Bangdiwala KI, et al. Integrating a family-focused approach into child obesity prevention: Rationale and design for the My Parenting SOS study randomized control trial. BMC Public Health. 2011;11:431. doi: 10.1186/1471-2458-11-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matheny AP, Jr, Wachs TD, Ludwig JL, Phillips K. Bringing order out of chaos: Psychometric characteristics of the Confusion, Hubbub, And Order scale. J Appl Dev Psychol. 1995;16(3):429–444. [Google Scholar]
- 38.Clerkin SM, Halperin JM, Marks DJ, Policaro KL. Psychometric Properties of the Alabama Parenting Questionnaire–Preschool Revision. J Clin Child Adolesc Psychol. 2007;36(1):19–28. doi: 10.1080/15374410709336565. [DOI] [PubMed] [Google Scholar]
- 39.Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol. 1989;18(2):167–175. [Google Scholar]
- 40.Abidin RR. Parenting Stress Index:(Short Form) Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- 41.Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004;26(1):41–54. [Google Scholar]
- 42.Bryant MJ, Lucove JC, Evenson KR, Marshall S. Measurement of television viewing in children and adolescents: A systematic review. Obes Rev. 2007;8(3):197–209. doi: 10.1111/j.1467-789X.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- 43.Borzekowski DLG, Robinson TN. Viewing the viewers: Ten video cases of children’s television viewing behaviors. J Broadcast Electron Media. 1999;43(4):506–528. [Google Scholar]
- 44.Anderson DR, Field DE, Collins PA, Lorch EP, Nathan JG. Estimates of young children’s time with television: A methodological comparison of parent reports with time-lapse video home observation. Child Dev. 1985:1345–1357. doi: 10.1111/j.1467-8624.1985.tb00202.x. [DOI] [PubMed] [Google Scholar]
- 45.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 46.Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol. 1989;18(2):167–175. [Google Scholar]
- 47.Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and Body Mass Index trajectories through young adulthood. Am J Public Health. 2010;100(12):2507–2512. doi: 10.2105/AJPH.2009.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.U.S. Census Bureau. North Carolina: State & County QuickFacts; [Google Scholar]
- 49.Hayes, Andrew F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013. [Google Scholar]
- 50.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 51.Hayes, Andrew F. An index and test of linear moderated mediation. Multivar Behav Res. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- 52.Sonneville KR, Gortmaker SL. Total energy intake, adolescent discretionary behaviors and the energy gap. Int J Obes. 32(S6):S19–S27. doi: 10.1038/ijo.2008.203. [DOI] [PubMed] [Google Scholar]
- 53.Heelan KA, Eisenmann JC. Physical activity, media time, and body composition in young children. J Phys Act Health. 2006;3(2):200. doi: 10.1123/jpah.3.2.200. [DOI] [PubMed] [Google Scholar]
- 54.Uher R, Treasure J, Heining M, Brammer MJ, Campbell IC. Cerebral processing of food-related stimuli: Effects of fasting and gender. Behav Brain Res. 2006;169(1):111–119. doi: 10.1016/j.bbr.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 55.Hill DA Nusheen Reid Chassiakos, Yolanda (Linda) Cross, Corinn Hutchinson, Jeffrey Levine, Alanna Boyd, Rhea Mendelson, Robert Moreno, Megan Swanson, Wendy Sue., editors. Media and young minds. Pediatrics. 2016;138(5) doi: 10.1542/peds.2016-2591. [DOI] [PubMed] [Google Scholar]
- 56.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial of the effects of reducing television viewing and computer use on Body Mass Index in young children. Arch Pediatr Adolesc Med. 2008;162(3):239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robinson TN. Reducing children’s television viewing to prevent obesity: A randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 58.Javed A, Jumean M, Murad MH, et al. Diagnostic performance of Body Mass Index to identify obesity as defined by body adiposity in children and adolescents: A systematic review and meta-analysis. Pediatr Obes. 2015;10(3):234–244. doi: 10.1111/ijpo.242. [DOI] [PubMed] [Google Scholar]
- 59.Okorodudu DO, Jumean MF, Montori VM, et al. Diagnostic performance of Body Mass Index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int J Obes. 2010;34(5):791–799. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 60.McCarthy HD. Body fat measurements in children as predictors for the metabolic syndrome: Focus on waist circumference. Proc Nutr Soc. 2006;65(04):385–392. doi: 10.1017/s0029665106005143. [DOI] [PubMed] [Google Scholar]
- 61.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not Body Mass Index explains obesity-related health risk. Am J Clin Nutr. 2004;79(3):379–384. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 62.Dobbelsteyn CJ, Joffres MR, MacLean DR, Flowerdew G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors: The Canadian Heart Health Surveys. Int J Obes Relat Metab Disord. 2001;25(5):652–661. doi: 10.1038/sj.ijo.0801582. [DOI] [PubMed] [Google Scholar]
- 63.Savva SC. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than Body Mass Index. Int J Obes. 2000;24(11):1453–1458. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 64.Bassali R, Waller JL, Gower B, Allison J, Davis CL. Utility of waist circumference percentile for risk evaluation in obese children. Int J Pediatr Obes. 2010;5(1):97–101. doi: 10.3109/17477160903111722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hirschler V, Aranda C, Calcagno M, Maccalini G, Jadzinsky M. Can waist circumference identify children with the metabolic syndrome? Arch Pediatr Adolesc Med. 2005;159(8):740–744. doi: 10.1001/archpedi.159.8.740. [DOI] [PubMed] [Google Scholar]
- 66.Gopinath B, Baur LA, Garnett S, Pfund N, Burlutsky G, Mitchell P. Body Mass Index and waist circumference Are associated with blood pressure in preschool-aged children. Ann Epidemiol. 2011;21(5):351–357. doi: 10.1016/j.annepidem.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 67.Moreno LA, Pineda I, Rodriguez G, Fleta J, Sarria A, Bueno M. Waist circumference for the screening of the metabolic syndrome in children. Acta Paediatr Oslo Nor 1992. 2002;91(12):1307–1312. doi: 10.1080/08035250216112. [DOI] [PubMed] [Google Scholar]
- 68.Flores G, Lin H. Factors predicting severe childhood obesity in kindergarteners. Int J Obes. 2013;37(1):31–39. doi: 10.1038/ijo.2012.168. [DOI] [PubMed] [Google Scholar]
- 69.Thomas H. Obesity prevention programs for children and youth: Why are their results so modest? Health Educ Res. 2006;21(6):783–795. doi: 10.1093/her/cyl143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.