Abstract
Purpose
Ukraine is home to Europe's worst HIV epidemic, overwhelmingly fueled by people who inject drugs who face harsh prison sentences. In Ukraine, HIV and other infectious diseases are concentrated in prisons, yet the magnitude of this problem had not been quantified. The purpose of this paper is to evaluate the systematic health survey of prisoners in the former Soviet Union (FSU).
Design/methodology/approach
Qualitative interviews were carried out with research and prison administrative staff to assess the barriers and facilitators to conducting a bio-behavioral survey in Ukrainian prisons.
Findings
Crucial barriers at the institutional, staff, and participant level require addressing by: first, ensuring Prison Department involvement at every stage; second, tackling pre-conceived attitudes about drug addiction and treatment among staff; and third, guaranteeing confidentiality for participants.
Originality/value
The burden of many diseases is higher than expected and much higher than in the community. Notwithstanding the challenges, scientifically rigorous bio-behavioral surveys are attainable in criminal justice systems in the FSU with collaboration and careful consideration of this specific context.
Keywords: Prisoners, Substance use disorders, Ukraine, Ethics, Health status, Implementation science research, Infectious diseases, Former Soviet Union
1. Introduction
Prisons globally house a disproportionate number of people who use drugs (PWUD) (Stover and Michels, 2010) and are high-risk environments for the spread of HIV and other blood-borne infections (Izenberg et al., 2014). With high-inmate turnover, this risk extends post-release when drug overdose is the leading cause of death (Merrall et al., 2010). Furthermore, this population transitions between the highly structured prison environment and the community, acting as bridges for the spread of the epidemic to the general population. Accordingly, the time during incarceration provides unique access to vulnerable populations that otherwise fall outside surveillance, prevention, and treatment services (Bridge et al., 2010). Accurate data from prisons is sparse and often unrepresentative due to numerous logistical constraints (Dolan et al., 2007; Vagenas et al., 2013; Altice et al., 2005; Azbel et al., 2013).
Community-based treatment, rather than incarceration, is effective and cost-effective, but for those incarcerated, periods of detainment should be leveraged to diagnose, treat, and prevent the further spread of disease. This is especially pertinent to the countries of the former Soviet Union (FSU), home to the fastest growing HIV epidemic, particularly driven by PWUD (Joint United Nations Programme on HIV/AIDS, 2010). Ukraine is home to Europe's worst HIV epidemic (Kruglov et al., 2008) with an estimated 360,000 HIV-infected persons (Ministry of Health of Ukraine, 2010a) and a similar number of people who inject drugs, nearly three-quarters of whom have been arrested (Jolley et al., 2012). Where the syndemic between HIV, substance use, and criminal justice is salient, prison-based surveillance may reliably estimate the scope of the problem to inform treatment and prevention activities. This report provides guidance on how to effectively conduct ethically and scientifically sound biosurveillance studies in order to assist future efforts in the FSU region, where such studies are virtually non-existent. We examine barriers and lessons learned to conducting bio-behavioral prison studies in Ukraine to help guide prevention efforts regionally (Bridge et al., 2010).
2. Methods
Setting
Ukraine, a lower middle-income country with a population of 45.2 million, has one of the highest worldwide incarceration rates with 321 per 100,000 population currently imprisoned (International Centre for Prison Studies King's College London, 2013). The State Penitentiary Service of Ukraine (SPSU), operated by the Ministry of Justice, oversees 145,189 prisoners (State Penitentiary Service of Ukraine, 2013). Voluntary HIV testing and antiretroviral therapy (ART) is statutorily required for prisoners, (United Nations Office on Drugs and Crime, 2012) but often falls short in practice (Ministry of Health of Ukraine, 2010b; Azbelet al., 2014). Obtaining objective information to inform implementation of evidence-based interventions requires collection of reliable data.
Bio-behavioral survey
We conducted a nationally representative bio-behavioral health survey of prisoners within six months of release. The operating procedures are based on similar seroprevalence surveys in prisons (Weild et al., 2000) and were agreed upon in collaboration with the SPSU. The procedure is presented in greater detail elsewhere (Azbel et al., 2013). Before study initiation, research assistants from local NGOs underwent a three-day training on the implementation of the protocol. The study was conducted in four national regions (north, south, west, and east) and participants were recruited from three types of facilities within each region (men's prisons for first-time offenders, repeat offenders, and women's prison) and weighted according to the number of prisoners within six months of release at each facility. A random-selection algorithm selected study participants from a list provided by SPSU of all prisoners with six months until their release into the community. After consent, participants underwent phlebotomy and completed a self-administered bio-behavioral survey using touchpad tablet computers in order to avoid bias and maintain confidentiality while guards remained present to ensure protection of research staff. Although literacy in Ukraine is 99 percent, research assistants read the survey in a private room to the participants who had difficulty reading.
Assessment
To assess the barriers and facilitators to conducting the first ever representative bio-behavioral survey of a prison population in the FSU, individual interviews were conducted with the research coordinators, research assistants, and prison administrators before the start of research, mid-way through the study, and upon its completion. Each involved party qualitatively evaluated barriers and facilitators to the conduct of the research, with a subsequent discussion of possible solutions.
3. Results
Bio-behavioral survey
Table I summarizes the results of the bio-behavioral survey including the prevalence of HIV, hepatitis B and C, and syphilis among the study sample, including whether the participants were previously informed of their positive status. The results present higher prevalence of infectious diseases and SUDs than recorded elsewhere from official sources (Azbel et al., 2013). Figure 1 illustrates the gap in official SPSU statistics by comparing them to the data obtained from this study.
Table I. Bio-behavioral characteristics of study participants.
| Characteristic | No. (%) of participants |
|---|---|
| Sex | |
|
| |
| Female | 80 (20.1) |
| Ethnicity | |
| Russian | 290 (72.7) |
| Ukrainian | 91 (22.8) |
| Recidivists | 196 (48.8) |
| Region | |
| North | 104 (25.9) |
| South | 98 (24.4) |
| West | 97 (24.1) |
|
| |
| East | 102 (25.4) |
| Age in years, mean (SD) | 31.9 (8.4) |
| Poverty level | |
| Below poverty line | 242 (60.2) |
| Highest education level | |
| Elementary | 6 (1.5) |
| Some secondary | 82 (20.4) |
| Completed secondary | 271 (67.4) |
| Completed higher education | 34 (8.5) |
| Length of this incarceration, mean years (SD) | 2.5 (23.0) |
| Months until release, mean (SD) | 2.1 (1.7) |
| Number or lifetime arrests, mean (SD) | 5.4 (7.0) |
|
| |
| Major depressive disorder | 129 (32.9) |
| Alcohol use disorder | 224 (56.6) |
| Have injected drugs | |
| Yes | 193 (48.0) |
| No | 204 (51.4) |
| Infectious diseases | |
| HIV | 78 (19.4) |
| Previously informed of HIV + status | 37 (49.3) |
| Previously uninformed of HIV + status | 38 (50.7) |
| Mean CD4 count, cells/mL (SD) | 355 (251.8) |
| CD4 count under 250 cells/mL | 44 (56.4) |
| Hepatitis C | 241 (60.0) |
| Previously informed of Hepatitis C + status | 26 (10.8) |
| Previously uninformed of Hepatitis C + status | 215 (89.2) |
| Hepatitis B | 21 (5.2) |
|
| |
| Syphilis | 41 (10.0) |
| Previously informed of syphilis+status | 13 (31.7) |
| Previously uninformed of syphilis+status | 28 (68.3) |
| Illicit substance use in 30 days before arrest | |
|
| |
| Opioid use | 264 (65.7) |
| Amphetamine use | 85 (21.1) |
| Sedative use | 330 (82.1) |
| Polysubstance use | 127 (31.6) |
| Shared injection equipment | 104 (25.9) |
| More than 30 injections | 85 (21.1) |
Note: n = 402
Figure 1. Infectious disease and substance use disorders in the Ukrainian prison population according to official vs study statistics.
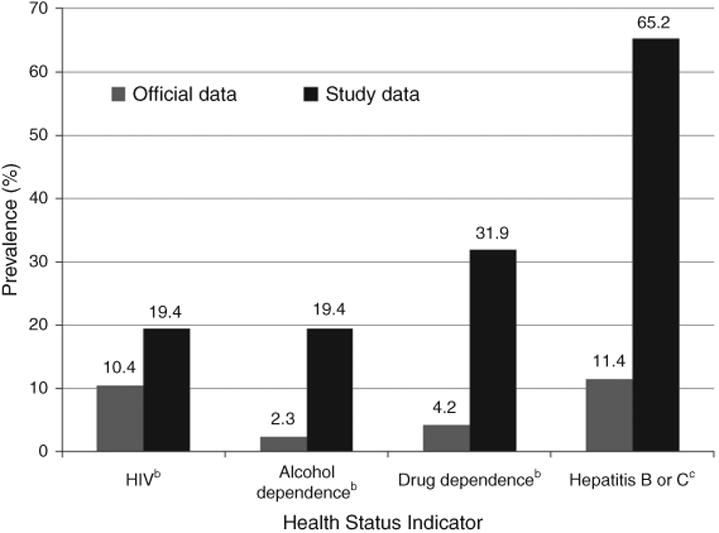
Notes: aAll prevalence data for 2011 among sentenced prisoners; bState Penitentiary Service of Ukraine, Department of Statistics; cThe study data are exclusively for Hepatits B and C whereas the official data are for all liver diseases. Ukrainian Institute of Sociological Research, “Potreby penitentsiarnoi systemy vdoskonalennia polityky z zapobihannia poshyrenniu VIL-infektsii” 2012
Assessment
Barriers and facilitators to implementing this study in the Ukrainian context were identified. Table II provides a list of the respondent-, staff-, and institutional-level factors that were highlighted by the research staff, along with solutions. These factors are further elaborated here.
Table II. Problems and solutions in avoiding bias introduction when surveying prisoners I.
| Problem | Situation | Bias | Solution | |
|---|---|---|---|---|
| Respondent-level factors | ||||
| Previously diagnosed prisoners | Prisoners with known HIV status would refuse HIV testing | Underestimates disease prevalence | We provided additional testing for several other conditions as well as reflex CD4 testing with provision of results and recommendations about treatment | |
| Disappearance for follow-up components of the study | Limited study to 2-3 days; insisted on follow-up irrespective of location within prison (isolation unit) or upon transfer | |||
| Phlebotomy logistical constraints | Venous access; secondary testing of CD4 | PWID may have poor venous access and excluding them underestimates blood-borne virus disease prevalence | Oral point-of-care testing as a back-up option (more costly); additional vial of blood for CD4 testing that could be used if HIV test was positive | |
| Confidentiality of participant data | Data collected included sensitive information about risk behaviors and infectious diseases | Concerns for potential breach of confidentiality which influence participation | Anonymous identifiers were assigned to link blood specimens to individual surveys | |
| Staff-level factors | ||||
| Interview privacy | The prison staff insisted on being present in the room for all interviews | May under-estimate risk behaviors | Negotiated with the prison department to place a guard right outside of the room in order to facilitate a private interview environment | |
| Bureaucratic restrictions surrounding testing and disease registration | Testing done for research cannot be used the medical establishment to “confirm” a disease. Patients sometimes had to be retested through official mechanisms in order to qualify for disease registration in order to receive treatment | |||
| Insistence on being informed of positive results from testing | Prisoners who do not want to be identified officially for any disease would refuse participation | All disease detection was promised not to be officially reported unless the prisoner signed a release-of-medical information to allow his/her status to be reported | ||
| Inquiring about sex and drug use behaviors | Prison officials wanted reports of any “illegal” behaviors reported during the incarceration | Underestimates prevalence of these stigmatizing behaviors | All data were collected anonymously using CASI and no “withinprison” risk behaviors were assessed | |
| Institutional-level factors | ||||
| Selection of sites | The prisons department wanted to control which of their sites was surveyed | May over- or under-estimate findings based on the type (e.g. addiction or HIV specialty prison), recidivists, gender, region of the country (known differences in HIV prevalence regionally) | We created a matrix of all the types of prisons that were operational and then stratified by factors that we anticipated would influence disease prevalence and randomly selected ones that met these criteria | |
| Selection of prisoners | The prisons department wanted to identify which prisoners they thought were appropriate for our study and would indicate that some were not “goodcharacters” for research. They also wanted to exclude anyone they already knew to have a diagnosis | May under-estimate disease prevalence if only “good” prisoners were allowed to participate | The prison created a comprehensive list of all prisoners who were within 6 months of release. Only after the full list was generated centrally did we assign each prisoner to a unique identifier and randomly selected from among this group. When “bad” characters showed up for the study and the prison guards said they were not appropriate, we still interviewed them | |
| Use of computers | Concerns about internet connection and cameras on the computer | Influences participation due to stigma; more stigmatized populations are likely to be more at risk | Computers were officially “approved” for entry, the cameras were disabled by research staff and confirmed by prison authorities and were also covered with tape | |
| Mandatory reporting of participant data | Sex- and drug-related behaviors that occur within prison are considered illegal and must be reported to prison authorities | Potential underestimation of risk behaviors | Drug and sexual risk-behavior questions referred to the pre-incarceration period to avoid having to report any behaviors in order to avoid punishment | |
Note: CASI, computer-assisted survey instrument
Respondent-level factors
Interviewing prisoners within prisons poses numerous unique challenges. In these restricted settings, all respondents must obey facility rules, which often include limited movement and continual supervision by authorities. Thus, obtaining transparent data must be balanced with maintaining a safe and secure environment. Confidentiality is central to this premise since researchers may be liable to report any “illegal” behaviors occurring within prison such as drug risk behaviors, obliging them to identify individual prisoners. To avoid this, study personnel and consent procedures remained independent from prison staff and all drug and sexual risk-behavior questions referred to the pre-incarceration period. Additionally, assigning an anonymous identifier linking blood specimens to individual surveys protected prisoners' confidentiality.
Ukraine, like many countries globally, administratively divides healthcare provision in prison from community healthcare structures. Thus, we chose to recruit participants about to re-enter the community because our research study could not guarantee that study participants would otherwise have full access to treatment in prison (despite assurances by the prison staff). Our rationale was that identifying new conditions in prisoners, as long as they were provided with the essential information about their condition and sites of referral, was possible just before their community release. Four participants, with CD4 counts under 100 cells/mL (far below the <350 cells/mL threshold for receiving ART), refused our referral for immediate prison-based medical care and ART, citing concerns about the perceived quality of prison-based healthcare and the fear of measures taken that would stigmatize them among other prisoners.
Only 24 (5.6 percent) of the 426 inmates randomly selected for consent declined participation, resulting in a high participation rate. At the end of the study, each participant received token compensation for their time (e.g. shaving supplies). After survey completion, most participants stated that compensation played no role in their participation, but that getting valid results and medical counseling and information external from prison staff about their health was a key motivating factor.
Staff-level factors
Oversight and training for research assistants and staff proved key to successfully completing the study. The research assistants underwent a three-day protocol and research ethics training supervised by coordinators. Because fieldwork lasted six months, however, it became clear that a single training at the start of the study was insufficient, so study coordinators provided continuous monitoring and ongoing training throughout the study, bringing to light important lessons learned along the way.
Despite having permission to operate the study from senior SPSU administrators, research assistants observed that staff attitudes in various geographical locations (especially in the east) interfered with study conduct. After completion of the study, all medical and non-medical, administrative and non-administrative staff in the 12 study facilities were surveyed and confirmed markedly negative attitudes toward substance users. For example, over three-quarters (68.5 percent) agreed that “modern society is too tolerant toward drug addicts” and similarly 71.3 percent agreed that “people who become addicted to opioids have only themselves to blame.” Of note, nearly half (42.5 percent) of prisoner participants self-reported substance use in the month prior to incarceration, suggesting that prison staff harbor negative feelings to a contingent to whom they have significant exposure. These attitudes were reflected in the administration of the study protocol. As an example, when prison staff was presented with a list of randomly selected study participants to approach for participation, those familiar with the prisoners would often express their desire to select those who were “well-behaved” and “clean” for study participation. Training was important in order to explain study procedures such as the necessity of random selection of participants to ensure a representative study sample. To meet this need, we conducted training meetings with prison staff before and during the study in order to keep them involved in the protocol and abreast of procedures.
Institutional-level factors
In a vertical prison bureaucracy, characteristic of the prison structures in the FSU, administrative approval is instrumental to receiving access to prison facilities. During the planning stages of the study, we learned that prison guards were required to remain in the room during interviews to “protect” research assistants. In order to respect patient privacy and ensure data collection accuracy, we created self-administered, computer-assisted structured interviews (CASI) that allowed participants to keep their responses confidential. Because electronic devices are not permitted in prison facilities, however, we ultimately agreed to allow the SPSU to remove all communication functionalities, thereby guaranteeing that they would be used exclusively for research purposes. For lower literate populations, however, CASI could be problematic and may require audio capabilities.
A second institutional hindrance was the need to receive written permission from the head of the SPSU for entry into each facility. These passes could not be prepared ahead of time and it was not possible to enter the prison without them. Securing them in a timely fashion required regular communication with the deputy of medicine at the SPSU. The parties involved in conducting the research had to establish congenial connections with the top-level bureaucrats and be flexible with last minute changes to the study schedule, which happened frequently.
4. Discussion
The data presented as a result of this survey illustrates how scientifically rigorous assessments drastically differ from official statistics which should be interpreted cautiously. This study highlights the urgent need and feasibility of such assessments. As part of the implementation process, international stakeholders from other FSU countries (e.g. Azerbaijan and Kyrgyzstan) have since conducted parallel studies, which document similar disparities in official vs actual statistics (data forthcoming). The experiences garnered from this health survey, with some modifications, are transferable to other countries in Eastern Europe and Central Asia which have HIV epidemics among PWUD, severe sentencing for drug-related crimes, and structurally similar prison systems. Currently, this study's protocol is being adapted for replication in the prisons of Central Asia.
These findings demonstrate that accurate data can in some instances result in significant changes in prison settings. The bio-behavioral study provided motivation to use best evidence to transition to routine HIV testing and evidence-based interventions such as opioid substitution therapy (OST). Despite evidence that OST with methadone and buprenorphine is effective in criminal justice settings (Haig, 2003; Smith-Rohrberg et al., 2004; Stallwitz and Stover, 2007; Wickersham et al., 2013) and its availability in the community for over ten years, it has not been implemented in Ukrainian prisons. After presenting key findings to local NGOs, international authorities, and government officials, however, the SPSU decided to introduce and pilot test evidence-based therapies as part of the implementation science framework. The first steps to introducing OST into the criminal justice setting were taken by passing into law in October 2012 legislation ensuring the continuity of OST for those enrolled in community programs who are arrested. The recent political destabilization stalled OST introduction in prisons, but this process has now been resurrected after the October 2015 parliamentary elections.
Receiving feedback from each of the parties involved and adjusting operating procedures throughout the course of the study helped tackle deterrents to its successful conduct. The hurdles to conducting ethical and scientifically rigorous research within prisons in the FSU can be overcome with dialogue and culturally sensitive planning. This requires a delicate balance between honoring the stringent rules of these institutions and upholding scientific ethics in an environment that breeds significant challenges to providing healthcare.
Ethics statement
This Institutional Review Boards at the Ukrainian Institute on Public Health Policy and the Yale University School of Medicine approved the study. Further safety assurances were provided by the Office for Human Research Protections (OHRP) in accordance with the 45 CFR 46.305(c) “Prisoner Research Certification” requirement. Participants provided their written informed consent to take part in the study.
Acknowledgments
This research was supported by grants from the National Institute on Drug Abuse for research (R01 DA029910, Altice, PI) and career development (K24 DA017072, Altice, PI). The authors have declared that no conflicts of interest exist.
Contributor Information
Lyuba Azbel, The Ukrainian Institute on Public Health Policy, Kyiv, Ukraine and Department of Internal Medicine, Section of Infectious Diseases, AIDS Program, Yale University, New Haven, Connecticut, USA.
Yevgeny Grishaev, The Ukrainian Institute on Public Health Policy, Kyiv, Ukraine.
Jeffrey A. Wickersham, The Department of Internal Medicine, Section of Infectious Diseases, AIDS Program, Yale University, New Haven, Connecticut, USA
Olena Chernova, The Ukrainian Institute on Public Health Policy, Kyiv, Ukraine and Department of Internal Medicine, Section of Infectious Diseases, AIDS Program, Yale University, New Haven, Connecticut, USA.
Sergey Dvoryak, The Ukrainian Institute on Public Health Policy, Kyiv, Ukraine.
Maxim Polonsky, The Ukrainian Institute on Public Health Policy, Kyiv, Ukraine and Department of Internal Medicine, Section of Infectious Diseases, AIDS Program, Yale University, New Haven, Connecticut, USA.
Frederick L. Altice, The Department of Internal Medicine, Section of Infectious Diseases, AIDS Program, Yale University, New Haven, Connecticut, USA and Division of Epidemiology of Microbial Diseases, School of Public Health, Yale University, New Haven, Connecticut, USA
References
- Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. Journal of Urban Health. 2005;82(2):312–26. doi: 10.1093/jurban/jti055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. Plos One. 2013;8(3):e59643. doi: 10.1371/journal.pone.0059643. Article Number. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Correlates of HIV infection and being unaware of HIV status among soon-to-be-released Ukrainian prisoners. Journal of the International AIDS Society. 2014;17:19005. doi: 10.7448/IAS.17.1.19005. September, Article Number. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge J, Lazarus JV, Atun R. HIV epidemics and prevention responses in Asia and Eastern Europe: lessons to be learned? AIDS. 2010;24(S3):S86–94. doi: 10.1097/01.aids.0000390094.91176.d8. [DOI] [PubMed] [Google Scholar]
- Dolan K, Kite B, Black E, Aceijas C, Stimson GV Reference Group on Hiv Aids Prevention Care Among Injecting Drug Users in Developing Transitional Countries. HIV in prison in low-income and middle-income countries. The Lancet Infectious Diseases. 2007;7:32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- Haig T. Randomized controlled trial proves effectiveness of methadone maintenance treatment in prison. Can HIV AIDS Policy Law Review. 2003;8(3):48. [PubMed] [Google Scholar]
- International Centre for Prison Studies King's College London. World prison brief. [accessed March 30, 2013];2013 available at: www.prisonstudies.org/info/worldbrief/wpb_country.php?country=168.
- Izenberg JM, Bachireddy C, Wickersham JA, Soule M, Kiriazova T, Dvoriak S, Altice FL. Within-prison drug injection among HIV-infected Ukrainian prisoners: prevalence and correlates of an extremely high-risk behaviour. International Journal of Drug Policy. 2014;25(5):845–52. doi: 10.1016/j.drugpo.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on Hiv/Aids. Global report: UNAIDS report on the global AIDS epidemic 2010. UNAIDS; Geneva: 2010. [Google Scholar]
- Jolley E, Rhodes T, Platt L, Hope V, Latypov A, Donoghoe M, Wilson D. HIV among people who inject drugs in Central and Eastern Europe and Central Asia: a systematic review with implications for policy. BMJ Open. 2012;2(5):e001465. doi: 10.1136/bmjopen-2012-001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruglov YV, Kobyshcha YV, Salyuk T, Varetska O, Shakarishvili A, Saldanha VP. The most severe HIV epidemic in Europe: Ukraine's national HIV prevalence estimates for 2007. Sexually Transmitted Infections. 2008;84(S1):i37–i41. doi: 10.1136/sti.2008.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, Hutchinson SJ, Bird SM. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–54. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health of Ukraine. Ukraine: national report on monitoring progress towards the ANGASS declaration of commitment on HIV/AIDS. Kyiv, Reporting period. 2010a January 2008-December 2009. [Google Scholar]
- Ministry of Health of Ukraine. Ukraine: national report on monitoring progress towards the UNGASS declaration of commitment on HIV/AIDS. Kyiv, Reporting period. 2010b January 2008-December 2009. [Google Scholar]
- Smith-Rohrberg D, Bruce RD, Altice FL. Review of corrections-based therapy for opiate-dependent patients: implications for buprenorphine treatment among correctional populations. Journal of Drug Issues. 2004;34:451–80. [Google Scholar]
- Stallwitz A, Stover H. The impact of substitution treatment in prisons - a literature review. International Journal of Drug Policy. 2007;186:464–74. doi: 10.1016/j.drugpo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- State Penitentiary Service of Ukraine. State Penitentiary Service of Ukraine statistics. [accessed March 30, 2013];2013 available at: www.kvs.gov.ua/peniten/control/main/uk/publish/article/628075.
- Stover H, Michels II. Drug use and opioid substitution treatment for prisoners. Harm Reduction Journal. 2010;7(17) doi: 10.1186/1477-7517-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. Potreby penitentsiarnoi systemy shchodo zapobihannia poshyrenniu VIL-infektsii. United Nations Office on Drugs and Crime; Kyiv: 2012. [Google Scholar]
- Vagenas P, Azbel L, Polonsky M, Kerimi N, Mamyrov M, Dvoryak S, Altice FL. A review of medical and substance use co-morbidities in Central Asian prisons: implications for HIV prevention and treatment. Drug Alcohol Depend. 2013;132(S1):S25–31. doi: 10.1016/j.drugalcdep.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weild AR, Gill ON, Bennett D, Livingstone SJ, Parry JV, Curran L. Prevalence of HIV, hepatitis B, and hepatitis C antibodies in prisoners in England and Wales: a national survey. Commun Disease and Public Health. 2000;3(2):121–6. [PubMed] [Google Scholar]
- Wickersham JA, Marcus R, Kamarulzaman A, Zahari MM, Altice FL. Implementing methadone maintenance treatment in prisons in Malaysia. The Bulletin of the World Health Organanization. 2013;91(2):124–9. doi: 10.2471/BLT.12.109132. [DOI] [PMC free article] [PubMed] [Google Scholar]


