Abstract
We performed an observational study with very-low-birth weight infants (VLBWI) ≤33 weeks of gestation born in centers of the German Neonatal Network (GNN; (total n = 8534, n = 6229 received probiotics). The primary objectives of our study were (a) to assess the effect of Lactobacillus acidophilus/Bifidobacterium infantis probiotics on growth in VLBWI during primary stay in hospital and (b) to determine whether this effect is modified by antibiotic exposure. In linear regression models the administration of probiotics was independently associated with improved weight gain [g/d; effect size B = 0.62 (95% CI: 0.37–0.87), p < 0.001], and higher growth rates for body length [(mm/d; B = 0.06 (95% CI: 0.04–0.08), p < 0.001] and head circumference [mm/d; B = 0.03, 95% CI: 0.02–0.04, p < 0.001]. This effect was pronounced in infants with postnatal exposure to antibiotics; i.e. weight gain [g/d; B = 0.66 (95% CI: 0.32–1), p < 0.001], growth rate body length [(mm/d; B = 0.09 (95% CI: 0.06–0.12), p < 0.001] and head circumference [mm/d; B = 0.04, 95% CI: 0.02–0.06, p < 0.001]. In the small subgroup that was available for analysis at 5-year-follow-up (with probiotics: n = 120 vs. without probiotics: n = 54) we noted a sustained effect of probiotics in infants who received postnatal antibiotics. Probiotics may improve growth in antibiotic-treated infants which needs to be confirmed in randomized-controlled trials.
Introduction
VLBWI are predisposed to early gut dysbiosis, which may increase the risk for acute, often fulminant complications such as sepsis or NEC. Gut dysbiosis may also lead to long lasting consequences, e.g. growth failure but also obesity and chronic inflammatory diseases1–4. Risk factors for gut dysbiosis in VLBWI include (a) prenatal administration of antibiotics to the mother leading to alteration of maternal microbiota composition, release of bacterial effectors and fetal antibiotic exposure, (b) Caesarean section, which prevents natural exposure to maternal bacteria, (c) perinatal infections, local or systemic inflammation and associated postnatal exposure to antibiotics. Probiotics may be a worthwhile treatment to foster the early microbiota establishment in a highly vulnerable population. They may have beneficial effects on growth, stabilization of the immunological homeostasis and thereby reduce the risk for infections and atopic disease3, 5. Studies on the therapeutic effects of probiotics in preterm infants have mainly focussed on short term endpoints, in particular NEC and sepsis. Several meta-analyses and systematic reviews including RCTs have concluded that prophylactic probiotics reduce the risk for NEC6, 7. In a large observational study in VLBW infants we have confirmed the association of Lactobacillus acidophilus and Bifidobacterium infantis probiotics with a reduced risk of NEC surgery8. This is in line with a recent analysis of the German NEO-KISS database indicating that the use of these dual-strain probiotics significantly reduced the risk of NEC9. Repa et al.10 reported the protective effect of Lactobacillus acidophilus and Bifidobacterium infantis on NEC in the subgroup of preterm infants exclusively fed with human milk, which was confirmed by a recent analysis from the Netherlands11. Despite these available data there is still uncertainty about the efficacy of probiotics. Recently, a large clinical trial involving 1315 infants ≤30 weeks of gestation found no clinical benefit of Bifidobacterium breve probotics for the risk of NEC12. The inconclusive results of well controlled trials have resulted in a very heterogenous incorporation of probiotics into clinical routine. While approximately 70% of VLBWI in Germany are prophylactically treated with probiotics8, most level III NICUs in the US are still reluctant to use probiotics as a clinical standard. It seems very likely that the inconsistency in probiotics efficacy is due to high variability in study protocols, including target populations, formulations – e.g. monostrain vs. multiple strains, and endpoints. In addition, the efficacy of probiotics could depend on the gut microbiota composition at baseline, i.e. before probiotics are started, which in turn depends on the history of antibiotic and pathogen exposure.
In order to improve strategies of prevention of dysbiosis and associated sequels including the use of probiotics, various endogenous and environmental influences need to be considered. This requires large, well-phenotyped cohorts, including subgroups with less exposure to antibiotics, i.e. VLBWI 28–32 weeks of gestation.. The primary objectives of our study were (a) to assess the effect of Lactobacillus acidophilus/Bifidobacterium infantis probiotics on growth in a large cohort of very- VLBWI (<33 weeks of gestation, n = 8534; subgroup 28–32 weeks, n = 5134) during primary stay in hospital and (b) to determine whether this effect is modified by ante- and postnatal antibiotic exposure.
Results
Lactobacillus acidophilus/Bifidobacterium infantis probiotics are associated with increased growth of VLBWI
Primary stay in hospital
The clinical characteristics of the cohort is outlined in Table 1 and supplemental Table 1. Mean duration of primary stay in hospital was 72 (median/25th–75th percentile ± SD: 65/48–88 ± 34) days. In univariate analyses, VLBWI, who received probiotics (n = 6229) had a higher growth rate than infants without probiotics (n = 2305). To address whether velocity differences represent catch-up growth in children starting out smaller rather than effects of probiotics, we performed linear regression analyses including gestational age, birth weight, gender, multiple birth and maternal descent. As outlined in Table 2, probiotics were associated with improved weight gain [g/d; effect size B = 0.62 (95% CI: 0.37–0.87), p < 0.001], and higher growth rates for body length [(mm/d; B = 0.06 (95% CI: 0.04–0.08), p < 0.001] and head circumference [mm/d; effect size B = 0.03, 95% CI: 0.02–0.04, p < 0.001].
Table 1.
Clinical characteristics according to prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics.
| Clinical characteristics | All infants without probiotics | All infants with probiotics | p | 28–32 weeks without probiotics | 28–32 weeks with probiotics | p |
|---|---|---|---|---|---|---|
| No. of infants | 2305 | 6229 | 1596 | 3538 | ||
| Gestational age (weeks) | 29.0 (2.5) | 28.3 (2.3) | <0.001* | 30.3 (1.4) | 30.0 (1.3) | <0.001* |
| Body weight at birth (g) z-score | 1112 (297) −0.36/−0.36 (0.82) | 1032 (291) −0.31/−0.25 (0.84) | <0.001* 0.002* | 1251 (205) −0.44/−0.47 (0.74) | 1203 (221) −0.42/−0.42 (0.77) | <0.001* 0.09* |
| Head circumference at birth (cm) z-score | 26.1 (2.6) −0.41/−0.4 (0.77) | 25.5 (2.5) −0.41/−0.37 (0.78) | <0.001* 0.4* | 27.4 (1.6) −0.42/−0.42 (0.73) | 27.0 (1.6) −0.42/−0.37 (0.75) | <0.001* 0.9* |
| Body length at birth (cm) z-score | 37.1 (3.8) −0.26/−0.22 (0.8) | 36.2 (3.7) −0.23/−0.18 (0.81) | <0.001* 0.08* | 38.8 (2.6) −0.32/−0.29 (0.78) | 38.2 (2.8) −0.33/−0.24 (0.81) | <0.001* 0.6* |
| SGA | 12.7 | 12.1 | 0.4 | 11.4 | 11.9 | 0.7 |
| Female gender | 48.7 | 48.9 | 0.9 | 50.5 | 49.3 | 0.4 |
| Multiple birth | 34.8 | 35.2 | 0.7 | 37 | 38.3 | 0.4 |
| Caesarean section | 90.9 | 91.3 | 0.9 | 92 | 92.3 | 0.7 |
| Duration of stay (days) | 7035 | 7334 | <0.001* | 5319 | 5519 | 0.009* |
| Weight gain (g/d) | 23.1 (6.0) | 23.1 (5.6) | 0.4* | 24.5 (5.9) | 24.3 (5.8) | 0.05* |
| Growth velocity head (mm/d) | 1.02 (0.3) | 1.05 (0.3) | 0.01* | 1.04 (0.3) | 1.06 (0.3) | 0.3* |
| Growth velocity length (mm/d) | 1.37 (0.5) | 1.43 (0.5) | <0.001* | 1.39 (0.4) | 1.43 (0.4) | 0.007* |
Legend: Continuous variables are shown as mean (SD); z-scores are shown as mean/median (SD). Categorical variables are shown as percent. p-values were derived from Fisher’s exact test or Mann-Whitney-U test if indicated (*), SGA, small for gestational age (<10th percentile of birth weight adjusted to gestational age). Growth velocity and weight gain were calculated by differences between parameters at birth and respective measures at discharge/number of days (duration of stay).
Table 2.
Effect of probiotics on growth during primary stay in hospital.
| Variable | All infants (n = 8516) | 28–32 weeks (n = 5127) |
|---|---|---|
| Weight gain (g/d) | ||
| Effect of Probiotics | 0.62 | −0.05 |
| 95% CI; p | 0.37–0.87; <0.001 | −0.29–0.39; 0.8 |
| Adjusted R2 | 0.12 | 0.03 |
| Growth velocity body length (mm/d) | ||
| Effect of Probiotics | 0.06 | 0.03 |
| 95% CI; p | 0.04–0.08; <0.001 | −0.002–0.006; 0.06 |
| Adjusted R2 | 0.01 | 0.007 |
| Growth velocity head circumference (mm/d) | ||
| Effect of Probiotics | 0.03 | 0.006 |
| 95% CI | 0.02–0.04; <0.001 | −0.01–0.02; 0.5 |
| Adjusted R2 | 0.02 | 0.02 |
Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. The effect of probiotics on weight gain as g/d growth rates in mm/d is shown as B coefficient, 95% confidence interval and p-value. Adjusted R2 values indicate coefficients of determinations and adjust for the number of terms used in the model.
Subgroup of VLBWI born 28 0/7– 32 6/7 weeks
In the subgroup of infants ≥28 0/7 ≤ 32 6/7 gestational weeks probiotics significantly accelerated growth rate for body length (1.43 vs. 1.39 mm/d, p = 0.007; adjusted effect size B = 0.03, p = 0.06), while other growth parameters were not affected by probiotic use (Tables 1 and 2).
2-year-follow up
Based on the information retrieved from the parents with the standardized questionnaires13, infants who received probiotics in the early neonatal period (n = 813) were not different from infants without probiotics (n = 333) with regard to number of upper respiratory tract infections in the first 24 months of life or risk for atopic dermatitis. In VLBWI born 28–32 weeks of gestation (n = 724), we noted a potential risk reduction for the mean ( ± SD) number of episodes for upper airway infections in the first 24 months after discharge from primary stay in hospital (2.8 ± 2.4 vs. 3.2 ± 2.3, p = 0.02; Table 3).
Table 3.
Follow-up data according to prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics.
| Clinical characteristics | All infants Without probiotics | All infants with probiotics | p | 28–32 weeks without probiotics | 28–32 weeks with probiotics | p |
|---|---|---|---|---|---|---|
| No. of infants | 54 | 120 | 23 | 46 | ||
| Gestational age (weeks) | 27.5 (2.3) | 27.6 (2.3) | 0.9* | 29.7 (1.3) | 30.0 (1.4) | 0.5* |
| Body weight (g) at birth | 940290 | 964297 | 0.1* | 1157251 | 1202278 | 0.1* |
| Body weight (kg) at 5yr-F/U z-score | 16.9 (2.4) −0.93/−0.91 (1.03) | 18.0 (3.5) −0.43/−0.63 (1.4) | 0.08* 0.06* | 17.1 (2.9) −0.89/−1.19 (1.23) | 18.5 (3.1) −0.21/−0.52 (1.22) | 0.1* 0.06* |
| Head circumference (cm) at 5 yr F/U; z-score | 49.5 (2.1) −1.39 (−1.33, 1.73) | 50.2 (1.8) −0.71 (−0.0, 1.35) | 0.009* 0.006* | 50.1 (2.2) −0.94 (−1, 1.67) | 50.3 (1.6) −0.56/−0.69 (1.15) | 0.2* 0.2* |
| Body length (cm) at 5 yr F/U z-score | 108.7 (5.2) −0.56/−0.60 (1.08) | 110.3 (5.6) −0.21/−0.35 (1.13) | 0.09* 0.2* | 107.9 (6.1) −0.83/−0.51 (1.17) | 110.8 (5.8) −0.06/−0.35 (1.13) | 0.09* 0.05* |
| Episodes with upper respiratory tract infection at 2 yr F/U no. of infants [mean (SD) GA, weeks)] mean number of episodes (SD) | 333 [28.9 (2.5)] 3.0 (2.3) | 819 [28.3 (2.3)] 2.8 (2.3) | 0.1* | 228 [28.9 (2.5)] 3.2 (2.3) | 496 [28.9 (2.5)] 2.8 (2.4) | 0.02* |
| Atopic dermatitis at 2 yr F/U (%) | 10.3 | 13.5 | 0.3 | 9.8 | 12.7 | 0.3 |
Legend: Continuous variables are shown as mean (SD); z-scores are shown as mean/median (SD). Categorical variables are shown as percent. p-values were derived from Fisher’s exact test or Mann-Whitney-U test if indicated (*), SGA, small for gestational age (<10th percentile of birth weight adjusted to gestational age). Growth velocity and weight gain were calculated by differences between parameters at birth and respective measures at discharge/number of days (duration of stay).
5-year-follow-up
In the small subgroup that was available for analysis at 5-year-follow-up (with probiotics: n = 120 vs. without probiotics: n = 54) we noted a sustained effect of probiotics on growth for head circumference (Table 3) which was independent from gestational age, birth weight, gender, multiple birth and maternal descent (cm; effect size B = 0.77, 95% CI: 0.16–1.38, p = 0.01).
Modification of the effect of probiotics on growth by antibiotic exposure
Antibiotic exposure
As depicted in Fig. 1, exposure to antibiotics is high across all gestational ages. Specifically, only 10.7% were never exposed to antenatal antibiotics or treated with postnatal antibiotics (stratum 1), 4.5% were exposed to antenatal antibiotics only (stratum 2), 38.2% had direct administration of postnatal antibiotics only (stratum 3), and 46.7% had exposure to both, ante- and postnatal antibiotics (stratum 4). Even in lower risk VLBWI, i.e. those with a gestational age of ≥28 0/7 ≤ 32 6/7 weeks, the percentage of infants who were not exposed to antibiotics was low (16.8%). In this subgroup, 6.6% had antenatal exposure only, 38.5% had postnatal treatment only and 36.5% were exposed to antibiotics before and after birth.
Figure 1.
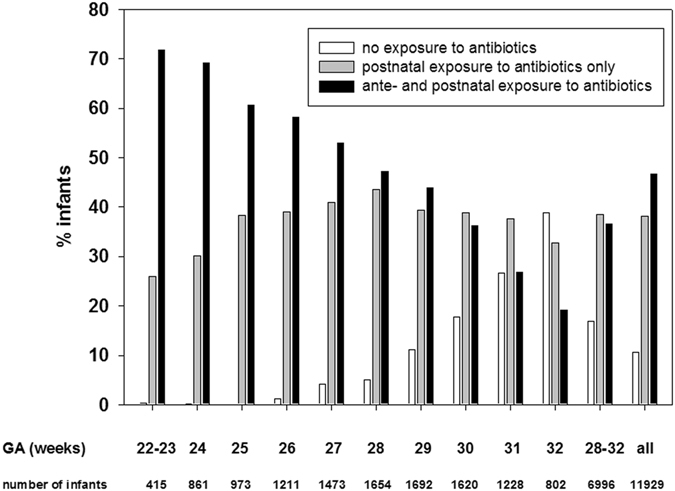
Exposure to antenatal and postnatal antibiotics according to gestational age. The figure describes the percentage of infants exposed to antenatal and/or postnatal antibiotics. A small percentage of infants was exposed to antenatal antibiotics but not to postnatal antibiotics (22–23 weeks: 1.4%, 24 weeks: 0.5%, 25 weeks: 0.8%; 26 weeks: 1.4%, 27 weeks: 2.0%; 28 weeks: 4.1%, 29 weeks: 5.6%; 30 weeks: 7.3%, 31 weeks: 9.4%; 32 weeks: 9.2%, 28–32 weeks: 6.6%; all: 4.5%).
Antibiotic classes
51.2% of mothers of VLBWI were exposed to antibiotics less than 5 days before preterm birth. Antenatal antibiotics were administered for several reasons, with preterm labour and suspected chorioamnionitis being the predominant causes. Cephalosporins and penicillins were used most frequently by the obstetricians (Supplemental Table 2). Neonatologist administered penicillins and aminoglycosides most often to VLBWI, while a significant number of infants was also exposed to second or third line antibiotics, such as glycopeptides (i.e. vancomycin) or carbapenems (Supplemental Table 3).
Within the four strata of antibiotic exposure, the percentage of infants supplemented with Lactobacillus acidophilus/Bifidobacterium infantis probiotics was different (68% without antenatal/postnatal exposure, 74% with antenatal exposure, 71% with postnatal exposure and 76.3% with both antenatal and postnatal exposure, p < 0.001).
Probiotic effect and modification by antibiotics
Antenatal antibiotics
Probiotics did not show a growth promoting effect in VLBWI, who were not exposed to antibiotics (stratum 1), or in VLBWI, who were exposed to antenatal antibiotics only (stratum 2, Table 4).
Table 4.
Antenatal antibiotics and effect of probiotics.
| Clinical characteristics | No antibiotics without probiotics | No antibiotics with probiotics | p | Antenatal antibiotics only without probiotics | Antenatal antibiotics only with probiotics | p |
|---|---|---|---|---|---|---|
| No. of infants | 295 | 628 | 103 | 293 | ||
| Gestational age (weeks) | 31.0 (1.3) | 30.4 (1.5) | <0.001 | 30.7 (1.4) | 29.8 (1.7) | <0.001 |
| Body weight at birth (g) z-score | 1277 (190) −0.7/−0.77 (0.67) | 1189 (221) −0.67/−0.74 (0.74) | <0.001 0.7 | 1300 (175) −0.49/−0.53, (0.67) | 1228 (224) −0.3/−0.28, (0.76) | 0.001 0.02 |
| Head circum-ference at birth (cm) z-score | 27.8 (1.5) −0.5/−0.47 (0.69) | 27.1 (1.7) −0.55/−0.49, (0.75) | <0.001 0.6 | 27.8 (1.4) −0.36/−0.37, (0.61) | 27.0 (1.7) −0.36/−0.29, (0.75) | <0.001 0.8 |
| Body length at birth (cm) z-score | 39.3 (3.4) −0.48/−0.48, (0.74) | 38.2 (2.7) −0.51/−0.5, (0.79) | <0.001 0.4 | 39.3 (2.2) −0.32/−0.24, (0.71) | 38.3 (2.8) −0.22/−0.21, (0.72) | 0.001 0.3 |
| Duration of stay (days) | 45 (13) | 49 (16) | 0.001 | 45 (13) | 49 (15) | 0.07 |
| Weight gain (g/d) | 26.2 (6.6) | 24.9 (57.1) | 0.01 | 26.1 (4.3) | 25.3 (14) | 0.001 |
| Growth velocity head (mm/d) | 1.10 (0.3) | 1.09 (0.3) | 0.8 | 1.08 (0.3) | 1.09 (0.3) | 0.8 |
| Growth velocity length (mm/d) | 1.49 (0.6) | 1.45 (0.5) | 0.3 | 1.34 (0.5) | 1.46 (0.6) | 0.08 |
Legend: Continuous variables are shown as mean (SD); z-scores are shown as mean/median (SD). Categorical variables are shown as percent. p-values were derived from Fisher’s exact test or Mann-Whitney-U test if indicated (*), SGA, small for gestational age (<10th percentile of birth weight adjusted to gestational age). Growth velocity and weight gain were calculated by differences between parameters at birth and respective measures at discharge/number of days (duration of stay).
Postnatal antibiotics
Probiotics accelerated growth in VLBWI with postnatal antibiotic exposure [stratum 3; with probiotics: n = 2272 vs. without probiotics: n = 900; mean HC ± SD (mm/d): 1.05 ± 0.3 vs. 1.01 ± 0.3, p < 0.001; mean BL ± SD (mm/d): 1.44 ± 0.4 vs. 1.35 ± 0.4, p < 0.001] and stratum 4 (Table 5; Fig. 2). As described in Table 6, probiotics were associated with improved growth rate in stratum 3 infants; i.e. weight gain [g/d; B = 0.66 (95% CI: 0.32–1), p < 0.001], growth rate body length [(mm/d; B = 0.09 (95% CI: 0.06–0.12), p < 0.001] and head circumference [mm/d; B = 0.04, 95% CI: 0.02–0.06, p < 0.001] and in stratum 4 infants (Figs 2 and 3).
Table 5.
Postnatal antibiotics and effect probiotics.
| Clinical characteristics | Postnatal antibiotics only without probiotics | Postnatal antibiotics only with probiotics | p | Ante - and postnatal antibiotics without probiotics | Ante - and postnatal antibiotics with probiotics | p |
|---|---|---|---|---|---|---|
| No. of infants | 900 | 2272 | 918 | 2953 | ||
| Gestational age (weeks) | 29.0 (2.4) | 28.4 (2.2) | <0.001 | 28.2 (2.5) | 27.6 (2.3) | <0.001 |
| Body weight at birth (g) z-score | 1070 (306) −0.53/−0.57 (0.85) | 988 (293) −0.52/−0.5, (0.89) | <0.001 0.7 | 1090 (299) −0.07/−0.04, (0.74) | 1014 (290) −0.06/−0.02, (0.75) | <0.001 0.7 |
| Head circumference at birth (cm) z-score | 26.0 (2.6) −0.52/−0.5, (0.79) | 25.4 (2.4) −0.54/−0.5, (0.8) | <0.001 0.7 | 25.7 (2.6) −0.29/−0.26, (0.76) | 25.1 (2.6) −0.28/−0.25, (0.74) | <0.001 0.6 |
| Body length at birth (cm) z-score | 36.7 (3.9) −0.38/−0.33, (0.85) | 35.7 (3.8) −0.4/−0.33, (0.87) | <0.001 0.9 | 36.6 (3.9) −0.07/0 (0.73) | 35.8 (3.7) −0.04/−0.03, (0.72) | <0.001 0.4 |
| Duration of stay (days) | 72 (33) | 75 (33) | <0.001 | 77 (38) | 79 (35) | 0.003 |
| Weight gain (g/d), | 22.7 (5.4) | 22.9 (4.5) | 0.9 | 22.7 (5.9) | 22.8 (4.4) | 0.7 |
| Growth velocity head (mm/d) | 1.01 (0.2) | 1.05 (0.3) | <0.001 | 1.02 (0.3) | 1.04 (0.3) | 0.03 |
| Growth velocity length (mm/d) | 1.35 (0.4) | 1.44 (0.4) | <0.001 | 1.38 (0.5) | 1.42 (0.4) | 0.001 |
Legend: Continuous variables are shown as mean (SD); z-scores are shown as mean/median (SD). Categorical variables are shown as percent. p-values were derived from Fisher’s exact test or Mann-Whitney-U test if indicated (*), SGA, small for gestational age (<10th percentile of birth weight adjusted to gestational age). Growth velocity and weight gain were calculated by differences between parameters at birth and respective measures at discharge/number of days (duration of stay).
Figure 2.
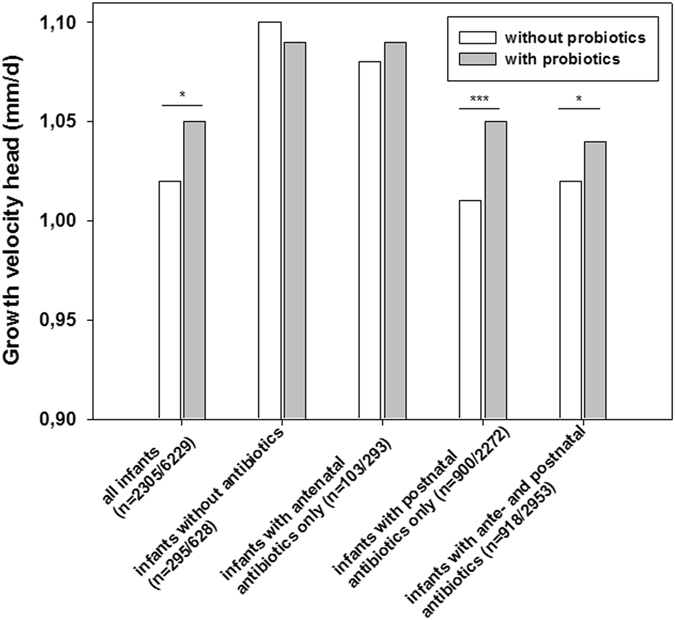
The effect of probiotics and modification by antibiotics on head circumference. The figure describes the effect of probiotics on growth velocity [difference of birth and discharge measures/number of days (duration of primary stay in hospital)] for head circumference. The effect is modified by exposure to antibiotics, the different strata are depicted on the x-axis. For each stratum, numbers of infants without probiotic treatment/with probiotic treatment are given. *p < 0.05, **p < 0.01, ***p < 0.001 (Fisher’s exact test, two-sided).
Table 6.
Effect of probiotics on growth during primary stay in hospital.
| Variable | No antibiotics (n = 919) | Antenatal antibiotics only (n = 396) | Postnatal antibiotics only (n = 3166) | Ante- and postnatal antibiotics (n = 3862) |
|---|---|---|---|---|
| Weight gain (g/d) | ||||
| Effect of Probiotics | −0.6 | −0.06 | 0.66 | 0.48 |
| 95% CI; p | −1.29 −0.15; 0.1 | −2.8–2.7; 0.9 | 0.32–1; p < 0.001 | 0.14–0.8; 0.005 |
| Adjusted R2 | 0.07 | 0.004 | 0.14 | 0.12 |
| Growth velocity body length (mm/d) | ||||
| Effect of Probiotics | −0.05 | 0.1 | 0.09 | 0.03 |
| 95% CI; p | −0.12–0.03; p = 0.2 | −0.04–0.24; 0.2 | 0.06–0.12; p < 0.001 | 0–0.06; 0.05 |
| Adjusted R2 | 0.001 | 0.009 | 0.012 | 0.004 |
| Growth velocity head circumference (mm/d) | ||||
| Effect of Probiotics | −0.02 | 0.014 | 0.04 | 0.02 |
| 95% CI;p | −0.07–0.02; 0.3 | −0.06–0.09; 0.7 | 0.02–0.06; p < 0.001 | 0.004–0.04; 0.02 |
| Adjusted R2 | 0.03 | 0.003 | 0.02 | 0.01 |
Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. The effect of probiotics on weight gain as g/d growth rates in mm/d is shown as B coefficient, 95% confidence interval and p-value. Adjusted R2 values indicate coefficients of determinations and adjust for the number of terms used in the model.
Figure 3.
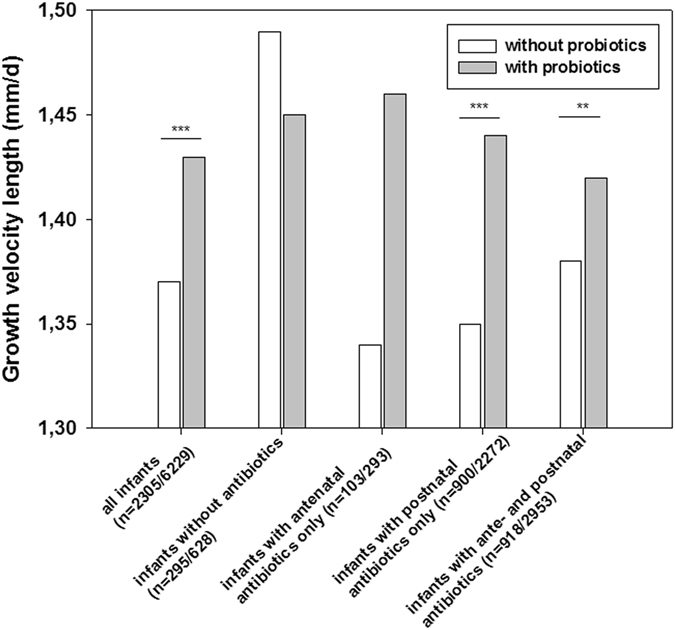
The effect of probiotics and modification by antibiotics on body length. The figure describes the effect of probiotics on growth velocity [difference of birth and discharge measures/number of days (duration of primary stay in hospital)] for body length. The effect is modified by exposure to antibiotics, the different strata are depicted on the x-axis. For each stratum, numbers of infants without probiotic treatment/with probiotic treatment are given. *p < 0.05, **p < 0.01, ***p < 0.001 (Fisher’s exact test, two-sided).
At 2 year follow-up, stratum 3 infants with postnatal antibiotic exposure only seem to have a benefit from neonatal probiotic use with regard to a potential risk reduction for the mean ( ± SD) number of episodes for upper airway infections (2.6 ± 2.1 vs. 3.1 ± 2.6, p = 0.01; Table 7) during the first 24 months after discharge from hospital. The risk for atopic dermatitis was not affected. All other strata of antibiotic exposure did not benefit from probiotics.
Table 7.
Follow-up data of infants exposed to postnatal antibiotics according to prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics.
| Clinical characteristics | Postnatal exposure to antibiotics Without probiotics | Postnatal exposure to antibiotics with probiotics | p | Ante- and postnatal exposure to antibiotics without probiotics | Ante- and postnatal exposure to antibiotics with probiotics | p |
|---|---|---|---|---|---|---|
| No. of infants | 19 | 46 | 29 | 61 | ||
| Gestational age (weeks) | 27.2 (2.3) | 27.9 (2.1) | 0.9* | 27.2 (2.1) | 26.9 (2.1) | 0.8* |
| Body weight (g) at birth | 787 (258) | 926 (272) | <0.001* | 976 (262) | 928 (290) | 0.1* |
| Body weight (kg) at 5yr-F/U z-score | 15.8 (2.0); −1.46/−1.62 (0.84) | 18.2 (4.2) −0.31/−0.67 (1.74) | 0.008* 0.003* | 17.6 (2.4) −0.54/−0.66 (1.01) | 17.8 (3.1) −0.55/−0.59 (1.3) | 1.0* 0.9* |
| Head circumference (cm) at 5 yr F/U, z-score | 48.9 (1.4) 1.68/−1.75 (1.19) | 49.9 (1.8) −0.83/−0.54 (1.32) | 0.01* 0.01* | 49.9 (2.5) −1.32/−1.04 (2.07) | 50.4 (1.9) −0.72/−0.77 (1.42) | 0.3* 0.3* |
| Body length (cm) at 5 yr F/U z-score | 107.0 (6.0) −0.91/−1.1 (1.27) | 110.0 (6.0) −0.2/−0.71 (1.25) | 0.06* 0.07* | 109.7 (4.3) −0.31/−0.11 (0.83) | 110.1 (5.3) −0.23/−0.21 (1.06) | 0.8* 0.9* |
| Episodes with upper respiratory tract infection at 2 yr F/U, no. of infants [mean (SD) GA, weeks)] mean number of episodes (SD) | 134 [28.7 (2.5)] 3.1 (2.6) | 318 [28.4 (2.3)] 2.6 (2.1) | 0.01* | 138 [28.2 (2.5)] 2.8 (2.3) | 406 [27.6 (2.3)] 2.8 (2.3) | 0.8* |
| Atopic dermatitis at 2 yr F/U (%) | 9.2 | 13.6 | 0.1 | 12.7 | 13.8 | 0.3 |
Legend: Continuous variables are shown as mean (SD); z-scores are shown as mean/median (SD). Categorical variables are shown as percent. p-values were derived from Fisher’s exact test or Mann-Whitney-U test if indicated (*), SGA, small for gestational age (<10th percentile of birth weight adjusted to gestational age). Growth velocity and weight gain were calculated by differences between parameters at birth and respective measures at discharge/number of days (duration of stay).
At 5-year-follow-up, the effect of probiotics on weight gain/growth was solely persistant in stratum 3 infants [with probiotics: n = 46; without probiotics: n = 19; mean body weight (BW) ± SD (kg): 18.2 ± 4.2 vs. 15.8 ± 2.0, p = 0.008; mean HC ± SD (cm): 49.9 ± 1.8 vs. 48.9 ± 1.8, p = 0.01; mean BL ± SD (cm): 110.0 ± 6.0 vs. 107.0 ± 6.0, p = 0.06, Table 6]. This was confirmed after adjustment for confounding variables (Table 8).
Table 8.
Effect of probiotics on growth parameters at 5 years of age.
| Variable | all (n = 151) | Postnatal antibiotics only (n = 59) | Ante- and postnatal antibiotics (n = 74) |
|---|---|---|---|
| Body weight | |||
| Effect of Probiotics | 1.2 | 3.3 | 0.1 |
| 95% CI; p | 0.1–2.3; 0.04 | 1.13–5.43; 0.003 | −1.7–1.5; 0.9 |
| Adjusted R2 | 0.06 | 0.16 | 0.11 |
| Body length (cm) | |||
| Effect of Probiotics | 1.59 | 4.4 | 0.4 |
| 95% CI; p | −0.3–3.4; 0.09 | 0.97–7.8; 0.01 | −2–2.8; 0.7 |
| Adjusted R2 | 0.1 | 0.2 | 0.15 |
| Head circumference (cm) | |||
| Effect of Probiotics | 0.77 | 0.91 | 0.7 |
| 95% CI; p | 0.16–1.38; 0.01 0.23 | 0.43–1.79; 0.04 | −0.3–1.7; 0.2 |
| Adjusted R2 | 0.29 | 0.22 | |
Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. Linear regression analysis included gestational age per week, birth weight in 100 g steps, gender, multiple birth, maternal descent and exposure to Bifidobacterium infantis/Lactobacillus acidophilus probiotics. The effect of probiotics on weight gain as g/d growth rates in mm/d is shown as B coefficient, 95% confidence interval and p-value. Adjusted R2 values indicate coefficients of determinations and adjust for the number of terms used in the model.
Discussion
In a large population-based cohort study we demonstrated that supplementation with Lactobacillus acidophilus/Bifidobacterium infantis probiotics improved growth of VLBWI during primary stay in hospital. This effect is most pronounced in infants with postnatal exposure to antibiotics. Given the limitations of an epidemiological analysis our data are hypothesis-generating. Administration of dual-strain probiotics may improve the metabolism of VLBWI and therefore considered as medical intervention that can target the microbiota-host interplay at the beginning of life, with potentially long-lasting impact on individual health.
Microbial patterns of initial colonisation of the intestine are important for growth of the newborn as they support the gut integrity, nutrient absorption as well as metabolic and endocrine functions (fat deposition, leptin and insulin levels; ref. 14. Bioactive compounds are known to stimulate the immune system, to support the infant’s growth and to facilitate the selective colonization of apparently protective bacterial species such as Bifidobacteria and Lactobacilli 15, 16.
Preterm birth, however, is associated with particular challenges to the development of the delicate host-microbe mutualism including mode of delivery, immature immunity, exposure to antibotics as well as feeding strategies. In the complex situation of preterm infants, probiotics may have a positive effect on infant´s growth. This assumption is based on animal models that reported improved weight gain in poultry that received probiotic supplement17. The beneficial effects of probiotics on metabolism may be mediated by the production of enzymes for fermentation of non-digestible dietary residues, energy recovery in the form of short-chain fatty acids, absorption of electrolytes and iron, synthesis of vitamins and conversion of pro-drugs to active metabolites. Furthermore, probiotics may help to repress potentially virulent bacteria by competition for compounds18. It is important to note, that the host dictates many of the conditions under which different bacteria of the microbiota compete. Thus it remains an important research question how the host’s genotype and the environmental factors interact to establish eubiosis or dysbiosis in the gut.
Clinical trials on the effect of probiotics on neonatal growth parameters are scarce. Term infants who are not nourished with human milk might have improved growth when formula is supplemented with Bifidobacterium lactis19. In preterm infants observational studies suggested a potential relationship between the diversity of the intestinal microbiota and weight gain in VLBWI20. A small scale study from Japan including 91 VLBWI suggested that supplementation with Bifidobacterium breve might improve gastrointestinal tolerance and weight gain21. So far, randomised trials which studied weight gain as main outcome failed to demonstrate a beneficial effect of probiotics22. Just recently, the PREMAPRO study performed by Hays et al.23 randomly assigned 199 preterm infants to receive daily supplementation over 4–6 weeks with placebo or three groups receiving probiotics - Bifidobacterium lactis or Bifidobacterium longum, or both. At the end of the supplementation period, no significant differences were seen for body weight, length, and head circumference.
Our large scale data point to a specific role of probiotics in the context of antibiotic exposure. In our setting, >85% infants are exposed to ante- and/or postnatal antibiotics. Even in the subgroup of infants with lower risk (28–32 weeks of gestation) treatment rate was >75%. Interestingly, infants who were not exposed to antibiotics or only exposed to antenatal antibiotics did not benefit from supplementation with probiotics.
Our primary observation is that antibiotic-treated VLBWI benefit from probiotics. In mature, established microbiota antibiotic treatment is unlikely to result in persistent changes24. In contrast, the developing infant gut microbiota of preterm infants is highly dynamic and susceptible to disruption by antibiotic exposure4, 25. For example, macrolide use in 2–7 year-old Finnish children is associated with a long-lasting shift in microbiota composition and metabolism26. Antibiotic treatment of newborns causes a reduced prevalence of Clostridia, whereas the gut of untreated infants was more likely to be colonized with Escherichia coli and S. aureus 27. Gibson et al. recently28 noted that antibiotic treatments in VLBWI are associated with widespread collateral microbiome impact by enrichment of antibiotic resistance genes that have no known activity against the specific antibiotic driver. With high-resolution microbiota sequencing, the gut dysbiosis in preterm infants mediated by antibiotics may be characterized by four aspects: loss of keystone taxa, loss of diversity, shifts in metabolic capacity, and blooms of pathogens4. We hypothesize that probiotics may prevent or attenuate the adverse effects of antibiotics on gut communities thereby stabilizing gut integrity and improving absorption of nutrients. This effect might be sustainable on weight, body length and head circumference at the age of 5 years, at least in the subgroup of infants who were treated with postnatal antibiotics. This aspect would be highly beneficial to preterm infants who are prone to growth failure as compared to term infants; i.e. the antibiotic-treated subgroup of infants who benefitted most from probiotic supplementation had still impaired growth at 5 years of age; mean weight: 18 kg = 2 kg <50th percentile, mean body length 110 cm = 3 cm <50th percentile, mean head circumference: 50 cm = 1 cm <50th percentile as compared to KiGGS data; 13). A single small RCT on the effect of Bifidobacterium lactis Bb12 demonstrated that in antibiotic-treated infants, probiotic supplementation resulted in a higher body weight, lower fecal pH, lower fecal calprotectin and higher fecal IgA levels as compared with placebo29, therefore supporting our finding of improved growth parameters in antibiotic-treated infants supplemented with probiotics. Secondly, we hypothesize that probiotics prevent low-grade chronic inflammation3, 5. This chronic inflammation is usually associated with higher energy consumption and predisposing to growth failure. On the other hand, probiotics may have beneficial effects on the crosstalk between metabolism and developing immune system which is is not yet understood. Antibiotic-treated infants in our setting have a lower rate of upper respiratory tract infections during infancy when supplemented with probiotics after birth. This needs to be confirmed in large-scale studies.
Our approach has several limitations. We present data of an observational study which may be biased by several confounding variables including center-specific effects and uneven number of VLBWI who were not treated with probiotics. In addition to that, the subgroup of infants with follow-up data at 5 years is small yet (as GNN has started enrolment in 2009 with available data on probiotic use in 2010). The sample size of the follow-up cohort is not sufficient to draw warrant conclusions. Secondly, probiotics were more often given to infants <28 weeks of age. A part of the effects on growth may be more related to catch-up growth of extremely preterm infants rather than a pure probiotic effect. This may explain why duration of stay in hospital might be shorter for infants without probiotics, despite enhanced weight gain in the probiotics group. Thirdly, the administration of probiotics for 28 days in capsules is a pragmatical way but still arbitrary and variable among study centers. Finally, duration of primary stay in hospital was highly variable (median 65 days, 25th–75th percentile: 48–88 days) which implies variability in observational time and outcome measures for growth. In conclusion, large randomized-controlled trials and animal models are needed to clarify the efficacy and mechanism of probiotics for preventing long-term health problems of preterm infants, i.e. infections and growth failure. Furthermore, the effect of probiotics may vary depending on the species and the strains/mix of microorganisms employed as well as the feeding strategies (human milk vs. formula) used in different centers. Deep sequencing technology may enable to discover new probiotic formulations to guide preventive strategies against dysbiosis30.
Methods
Observational study
The German Neonatal Network (GNN) studies the long-term effects of genetic, clinical, and social risk factors as well as center specific treatment strategies in very-low-birth weight infants (VLBWI) born in 54 neonatal intensive care units in Germany (1st of April 2009 until 31st of December 2015, n = 11929 enrolled infants). Herein we performed an observational, population-based study with VLBWI enrolled in the first days after birth. The inclusion criteria for this study were as follows: birth weight <1500 g and gestational age >22 0/7 and ≤32 6/7 weeks, written informed consent of pareets or legal representatives and discharge to home environment Exclusion criteria were lethal malformations, e.g. trisomy 13 and trisomy 18. After recruitment by the attending physicians, a predefined GNN data set (supplemental information), including treatment parameter and outcome data, was recorded by completion of case record files. After discharge, data sheets were sent to the GNN center in Lübeck. A physician trained in neonatology or a study nurse evaluated the data quality by annual on site monitoring of the data sets. Data on the use of Lactobacillus acidophilus/Bifidobacterium infantis (Infloran®, one capsule containing 109 L. acidophilus and 109 B. infantis) probiotics were documented from 1st of September 2010 until 31st of December 2015 (n = 8534) at 48 study sites. We included subgroup analyses as follows:
VLBWI born at 28 0/7–32 6/7 gestational weeks (n = 5134)
All VLBWI without exposure to antibiotics (stratum 1, n = 923)
All VLBWI with exposure to antenatal antibiotics only (stratum 2, n = 396)
All VLBWI with postnatal antibiotic treatment only (stratum 3, n = 3172)
All VLBWI with antenatal and postnatal antibiotic treatment (stratum 4, n = 3871).
The primary objectives of our study were (a) to assess the effect of prophylactic Lactobacillus acidophilus/Bifidobacterium infantis probiotics on growth in very-low-birth-weight infants (VLBWI) during primary stay in hospital and (b) to determine whether this effect is modified by ante- and postnatal antibiotic exposure. This study was not nested within a clinical trial.
Follow-up analysis
24-month-follow-up
For the 24-month-follow-up, parents of surviving infants enrolled in GNN received a voluntary questionnaire (according to the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) from Robert Koch Institute, Germany including data on sociodemographic characteristics, vaccine preventable diseases, and illnesses such as infections and atopic disease; www.rki.de)13. Prevalence calculations of infections were based on the question: “Has your child ever had the following infectious illnesses…?” Possible parental responses were “yes”/”no”/”don’t know”. The parent questionnaire collected data on the following infections after discharge from primary stay in hospital: cold/flu-like infection, tonsillitis, herpesvirus infection, bronchitis (not when asthma was present), gastrointestinal infection, cystitis and/or urethritis, purulent conjunctivitis (bacterial conjunctivitis).
5-year-follow-up
For the 5-year follow-up infants were examined by the GNN study team (physician trained in neonatology and 2 study nurses). Growth parameters (body length, body weight, head circumference) and systolic/diastolic blood pressure levels were determined with standardized measurements. The motor and cognitive development was assessed through the following tests: Movement Assessment Battery for Children (M-ABC) and Wechsler Preschool and Primary Scale of Intelligence – Third Edition; WPPSI I–III). A hearing test (tone audiometry), visual test and lung function testing (spirometry) were also performed.
Definitions
Probiotic use was defined as prophylactic administration of Lactobacillus acidophilus/Bifidobacterium infantis to VLBWI. Probiotic use was as follows: 41/48 centers used probiotics prophylactically. 38/41 centers administered probiotics to all VLBWI, 3 centers restricted probiotic use to infants with a birth weight <1000 g. All centers started probiotics (1 capsule/day) on day 1–3 of life and continued treatment for 28 days or until full enteral feeds (150 ml/kg) were reached.
Antenatal exposure to antibiotic therapy was defined as antenatal antibiotic treatment of mothers of VLBWI (percentage of neonates whose mothers got any dose of antibiotics within 5 days before birth)).
Postnatal exposure to antibiotic therapy was defined as antibiotic treatment of VLBWI (percentage of neonates who got any direct dose of antibiotics after birth; denomination: number of infants enrolled in GNN who were discharged home). Indirect exposure (for example by human milk) was not considered.
Growth velocity was defined of growth (head circumference or body length) in mm/day (difference of the parameter at birth and at discharge/number of days in hospital).
Statistical analysis
Data analysis was performed using the SPSS 22.0 data analysis package (Munich, Germany). Hypotheses were evaluated with two-sided tests including Fisher’s exact test and Mann-Whitney U test. A p value < 0.05 was considered as statistically significant for two-sided tests, Bonferroni corrections were made for multiple comparisons. Z-scores were calculated for birth weight, length and head circumference according to Voigt et al.31 and for anthropometric parameters according to Kromeyer-Hauschild et al.32 To determine potential associations between administration of probiotics and growth rates we conducted linear regression analyses with known confounding variables, i.e. gestational age per week, birth weight in 100 g steps, gender, multiple birth and maternal descent. Effect size and 95% confidence intervals (CI) were calculated. A p-value of <0.05 was considered statistically significant. For primary and subgroup analyses, we used a uniform dataset with available data for all metric parameters. Missing data were not included.
Ethics
The study including all experimental protocols was approved by the local committee on research in human subjects of the University of Lübeck (08–022; 03.12.2010) and the local ethical committees at the other study centers. Informed consent was obtained from all subjects. All methods were carried out in accordance with relevant guidelines and regulations, specifically: the Declaration of Helsinki, the current revision of ICH Topic E6, the Guidelines for Good Clinical Practice, and the Guidelines of the Council for International Organization of Medical Sciences, the WHO (“Proposed International Guidelines For Biomedical Research Involving Human Subjects”).
Electronic supplementary material
Acknowledgements
The writing group for this article acknowledges the contributions of all other members of the Geman Neonatal Network. We are grateful to the infants, parents and health care providers who supported our study. The German Neonatal Network is funded by the German Ministry for Education and Research (BMBF-grant-No: 01ER0805 and 01ER1501). The sponsor had no role in the study design, performance of the study and the preparation of manuscript.
Author Contributions
Each author listed on the manuscript has seen and approved the submission of this version of the manuscript and takes full responsibility for the manuscript. C.H. and W.G. conceptualized and designed the study, carried out the initial data analyses, supervised and coordinated the data collection, drafted the initial manuscript, and approved the final manuscript as submitted. J.P., J.B., J.S., P.H., M.Z., D.V., C.G., S.G., D.F., J.R., E.H. supported the study design and the development of data collection instruments coordinated and supervised data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-06161-8
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shaw AG, et al. Late-Onset bloodstream infection and perturbed maturation of the gastrointestinal microbiota in premature infants. PLoS ONE. 2015;10:e0132923. doi: 10.1371/journal.pone.0132923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Backhed F. Programming of host metabolism by the gut microbiota. Ann. Nutr. Metab. 2011;58(Suppl 2):44–52. doi: 10.1159/000328042. [DOI] [PubMed] [Google Scholar]
- 3.Logan AC, Jacka FN, Prescott SL. Immune-Microbiota Interactions: Dysbiosis as a Global Health Issue. Curr. Allergy Asthma Rep. 2016;16:13. doi: 10.1007/s11882-015-0590-5. [DOI] [PubMed] [Google Scholar]
- 4.Vangay P, Ward T, Gerber JS, Knights D. Antibiotics, pediatric dysbiosis, and disease. Cell Host Microbe. 2015;17:553e64. doi: 10.1016/j.chom.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson CC, Ownby DR. Allergies and Asthma: Do Atopic Disorders Result from Inadequate Immune Homeostasis arising from Infant Gut Dysbiosis? Expert Rev. Clin. Immunol. 2016;7:1–10. doi: 10.1586/1744666X.2016.1139452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AlFaleh K, Anabrees J. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Evid. Based Child Health. 2014;9:584e671. doi: 10.1002/ebch.1976. [DOI] [PubMed] [Google Scholar]
- 7.Olsen R, Greisen G, Schrøder M, Brok J. Prophylactic Probiotics for Preterm Infants: A Systematic Review and Meta-Analysis of Observational Studies. Neonatology. 2016;109:105–12. doi: 10.1159/000441274. [DOI] [PubMed] [Google Scholar]
- 8.Härtel C, et al. Prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics and outcome in very low birth weight infants. J. Pediatr. 2014;165:285–289. doi: 10.1016/j.jpeds.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 9.Denkel LA, et al. Protective Effect of Dual-Strain Probiotics in Preterm Infants: A Multi-Center Time Series Analysis. PLoS One. 2016;11:e0158136. doi: 10.1371/journal.pone.0158136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Repa A, et al. Probiotics (Lactobacillus acidophilus and Bifidobacterium infantis) prevent NEC in VLBW infants fed breast milk but not formula. Pediatr. Res. 2015;77:381–8. doi: 10.1038/pr.2014.192. [DOI] [PubMed] [Google Scholar]
- 11.Samuels N, et al. Necrotising enterocolitis and mortality in preterm infants after introduction of probiotics: a quasi-experimental study. Sci. Rep. 2016;6:31643. doi: 10.1038/srep31643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costeloe K, et al. Probiotics in Preterm Infants Study Collaborative Group. Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet. 2016;387:649–60. doi: 10.1016/S0140-6736(15)01027-2. [DOI] [PubMed] [Google Scholar]
- 13.Schmitz R, Poethko-Müller C, Reiter S, Schlaud M. Vaccination status and health in children and adolescents: findings of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Dtsch. Arztebl. Int. 2011;108:99–104. doi: 10.3238/arztebl.2011.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bäckhed F, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci. USA. 2004;101:15718e23. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zivkovic AM, German JB, Lebrilla CB, Mills DA. Human milk glycobiome and its impact on the infant gastrointestinal microbiota. Proc. Natl. Acad. Sci. USA. 2011;108(Suppl 1):4653–8. doi: 10.1073/pnas.1000083107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Underwood MA, German JB, Lebrilla CB, Mills DA. Bifidobacterium longum subspecies infantis: champion colonizer of the infant gut. Pediatr. Res. 2015;77:229–35. doi: 10.1038/pr.2014.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Angelakis E, Raoult D. The increase of lactobacillus species in the gut flora of newborn broiler chicks and ducks is associated with weight gain. PLoS One. 2010;5:e10463. doi: 10.1371/journal.pone.0010463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singhi SC, Kumar S. Probiotics in the critically ill children. F1000 Res. 2016;407:1–11. doi: 10.12688/f1000research.7630.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steenhout PG, Rochat F, Hager C. The effect of Bifidobacterium lactis on the growth of infants: a pooled analysis of randomized controlled studies. Ann. Nutr. Metab. 2009;55:334e40. doi: 10.1159/000248992. [DOI] [PubMed] [Google Scholar]
- 20.Jacquot A, et al. Dynamics and clinical evolution of bacterial gut microflora in extremely premature patients. J. Pediatr. 2011;158:390e6. doi: 10.1016/j.jpeds.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 21.Kitajima H, et al. Early administration of bifidobacterium breve to preterm infants: randomised controlled trial. Arch. Dis. Child Fetal Neonatal Ed. 1997;76:F101e7. doi: 10.1136/fn.76.2.F101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sari FN, et al. Do oral probiotics affect growth and neurodevelopmental outcomes in very low-birth-weight preterm infants? Am. J. Perinatol. 2012;29:579e86. doi: 10.1055/s-0032-1311981. [DOI] [PubMed] [Google Scholar]
- 23.Hays S, et al. Probiotics and growth in preterm infants: A randomized controlled trial, PREMAPRO study. Clin. Nutr. 2016;35:802–11. doi: 10.1016/j.clnu.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6:e280. doi: 10.1371/journal.pbio.0060280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gibson MK, Crofts TS, Dantas G. Antibiotics and the developing infant gut microbiota and resistome. Curr. Opin. Microbiol. 2015;27:51–6. doi: 10.1016/j.mib.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Korpela K, et al. Intestinal microbiome is related to lifetime antibiotic use in Finnish pre-school children. Nat. Commun. 2016;7:10410. doi: 10.1038/ncomms10410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adlerberth I, et al. Reduced enterobacterial and increased staphylococcal colonization of the infantile bowel: an effect of hygienic lifestyle? Pediatr. Res. 2006;59:96e101. doi: 10.1203/01.pdr.0000191137.12774.b2. [DOI] [PubMed] [Google Scholar]
- 28.Gibson MK, et al. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat. Microbiol. 2016;1:16024. doi: 10.1038/nmicrobiol.2016.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohan R, et al. Effects of Bifidobacterium lactis Bb12 supplementation on body weight, fecal pH, acetate, lactate, calprotectin, and IgA in preterm infants. Pediatr Res. 2008;64:418e22. doi: 10.1203/PDR.0b013e318181b7fa. [DOI] [PubMed] [Google Scholar]
- 30.Groer MW, et al. Development of the preterm infant gut microbiome: a research priority. Microbiome. 2014;2:38. doi: 10.1186/2049-2618-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Voigt M, et al. Analyse des Neugeborenenkollektivs der Jahre 1995–1997 der Bundesrepublik Deutschland. 11. Mitteilung: Unterschiede im somatischen Entwicklungsstand Neugeborener unter Berücksichtigung des Herkunftslandes der Mutter. Geburtsh. Frauenheilk. 2006;66:391–9. doi: 10.1055/s-2006-924032. [DOI] [Google Scholar]
- 32.Kromeyer-Hauschild K, et al. Perzentile für den Body-Mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschr Kinderheilk. 2001;149:807–18. doi: 10.1007/s001120170107. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


