Abstract
Purpose
The results from Radiation Therapy Oncology Group (RTOG) 0617, a dose escalation trial that compared treatment with 60 Gy versus 74 Gy for patients with stage III non-small cell lung cancer (NSCLC), suggested that in these patients, the heart dose from radiation therapy correlates with survival. In particular, the study noted that patients with a high heart V5 and V30 had a poorer overall survival; however, the exact cause of this correlation is not known. We hypothesize that heart dose may be a surrogate for mediastinal nodal involvement, which has prognostic value in NSCLC. This study evaluates the relationship between heart dose and involvement of mediastinal lymph nodes in patients with stage III NSCLC treated with radiation therapy.
Methods and materials
A total of 56 patients were identified and treated with definitive radiation therapy from 2007 to 2014. The heart was recontoured for every patient by a single physician, per the RTOG 1106 contouring atlas. We assessed lymph node station involvement using pretreatment data, and nodal coverage was confirmed on plan review.
Results
Mean heart dose was found to be significantly higher in patients with multinodal station and level 7 involvement. On Spearman's rank correlation, level 7 was significantly associated with all heart parameters tested (P < .001). Patients who had 2 or more lymph node stations involved were found to have significantly higher heart doses for all parameters tested when compared with those who had only one station involved or no nodal involvement.
Conclusions
Our findings suggest that heart dose may be a surrogate for other prognostic factors in stage III NSCLC rather than an independent predictor of outcome.
Summary.
The intention of this study was to establish a relationship between mediastinal lymph node involvement and heart dose in patients treated with definitive radiation therapy for stage III non-small cell lung cancer. In our cohort of patients, we showed that heart dose was correlated with both multistation and subcarinal nodal involvement; therefore, heart dose may be a surrogate for the extent of nodal involvement rather than an independent predictor of survival.
Introduction
The results of Radiation Therapy Oncology Group (RTOG) 0617, a randomized phase III trial that evaluated both dose escalation and the use of cetuximab in addition to concurrent chemoradiation in the treatment of unresectable stage III non-small cell lung cancer (NSCLC), were recently published and showed a detriment with higher doses of radiation therapy and no benefit to the addition of treatment with cetuximab.1 On dosimetric evaluation, heart dose was unexpectedly found to be a negative predictor of survival. It currently is unclear whether this is a causal or associative relationship (ie, is heart dose the cause of increased mortality or a surrogate for another poor prognostic factor).
Mediastinal lymph node involvement in NSCLC is a prognostic indicator of poor outcomes compared with patients with an earlier stage of NSCLC. Multiple surgical series have shown that multistation nodal disease, subcarinal lymph node involvement (level 7 lymph nodes) in particular, confers an especially poor prognosis. Iwasaki et al2 examined 142 patients with T1-3 N2 NSCLC who underwent an attempted curative resection and concluded that surgery for these patients might be acceptable if subcarinal lymph node metastasis is absent because of a 0% 5-year overall survival (OS) for patients with subcarinal involvement. Similarly, Watanabe et al.3 examined 199 patients with N2 NSCLC and found that patients with single-level metastases had a significantly better survival rate than those with multilevel metastases. The researchers also noted that subcarinal nodal involvement had an unfavorable effect in the case of single-level metastasis.3 The prognostic value of mediastinal nodal stations and extent of involvement have been supported by multiple other surgical series as well.4, 5, 6
The clinical impact of the extent and location of mediastinal lymph node involvement on the survival of patients with T1–4 N2–3 M0 stage III NSCLC treated with definitive chemoradiation or definitive radiation therapy alone has also been explored.7 A series of 106 patients from the University of Pennsylvania found that subcarinal nodal involvement was a significant negative predictor of OS on multivariable analysis.
Anatomically, the subcarinal nodes are located caudally to the carina of the trachea, around the superior edge of the heart. Therefore, we propose to investigate the relationship between radiation dose to the heart and mediastinal nodal involvement to investigate a possible correlation between the two, which could explain the association between heart dose and survival.
Methods and materials
In an institutional review board–approved study, we reviewed an institutional database and identified 56 patients who were diagnosed with stage IIIA/B NSCLC treated definitively with radiation at our institution between 2007 and 2014. A total of 50 patients were treated with definitive chemoradiation therapy, and 6 patients were treated with radiation therapy alone. Patients who were treated with concurrent chemotherapy primarily received either a combination of cisplatin and etoposide or carboplatin and paclitaxel. The median radiation therapy dose was 66 Gy delivered in 1.8 Gy fractions (range, 59.4-73.8 Gy; delivered in 1.8-2 Gy fractions). Doses were selected at the discretion of the treating physician, and all patients were treated prior to the publication of the results of RTOG 0617. In all patients, radiation was targeted to gross disease only without elective nodal coverage. Thirty-three patients (59%) were treated using 3-dimensional conformal therapy, and 23 patients (41%) were treated using intensity modulated radiation therapy.
For radiographic evaluation of mediastinal lymph node involvement, we reviewed pretreatment positron emission tomography-computed tomography (CT) scans, which were available for all but 2 patients. For the 3 patients without positron emission tomography-CT scans, pretreatment diagnostic CT scans and radiation treatment-planning CT scans were used. Thirty-seven patients also underwent surgical staging of the mediastinum. All dosimetric plans were reviewed to confirm the planning target volume coverage of the recorded involved nodal stations, and all patients had their heart volume recontoured by a single physician (J.Z.) per the RTOG 1106 contouring atlas.
The primary endpoint of this study was to demonstrate an association between the extent and location of involved and treated mediastinal lymph nodes and the radiation dose that the heart received. Multistation nodal involvement was considered as involvement of 2 or more stations of levels 1 to 9. The Spearman's rank correlation was performed to test the association of both any mediastinal lymph node involvement and individual lymph node station (2-10) involvement on heart V5 Gy, V40 Gy, V50 Gy, and mean heart dose.
All statistical analyses were performed using OriginPro 9.1 (OriginLab Corporation, Northhamptom, MA).
Results
Patient characteristics are listed in Table 1. The median age of patients who were treated was 64.3 years (range, 38.4-85.9). Fifty-two of 56 patients (92.8%) were determined to have involvement of at least one of station 1 to 9 lymph nodes. Of these patients, 34 had subcarinal involvement and 43 had multistation nodal involvement. For those with multistation nodal involvement, the median number of lymph node stations involved was 3 (range, 2-9).
Table 1.
Patient characteristics
| Characteristics | All Patients (N = 56) |
|---|---|
| Median age, y (range) | 64.3 (38.4-85.9) |
| Sex | |
| Male | 32 |
| Female | 24 |
| Histology | |
| Adenocarcinoma | 30 |
| Squamous cell | 16 |
| Non-small cell lung cancer, not otherwise specified | 10 |
| Stage | |
| IIIA | 30 |
| IIIB | 26 |
| Median radiation therapy dose, Gy (range) | 66 (59.4-73.8) |
| Treatment technique | |
| Three-dimensional conformal | 33 |
| Intensity modulated radiation therapy | 23 |
| Concurrent systemic therapy | |
| Yes | 50 |
| No | 6 |
| Lymph node station 1-9 involvement | |
| Yes | 52 |
| No | 4 |
| Multinodal station involvement | |
| Yes | 43 |
| No | 13 |
| Subcarinal involvement | |
| Yes | 34 |
| No | 22 |
Individual nodal stations
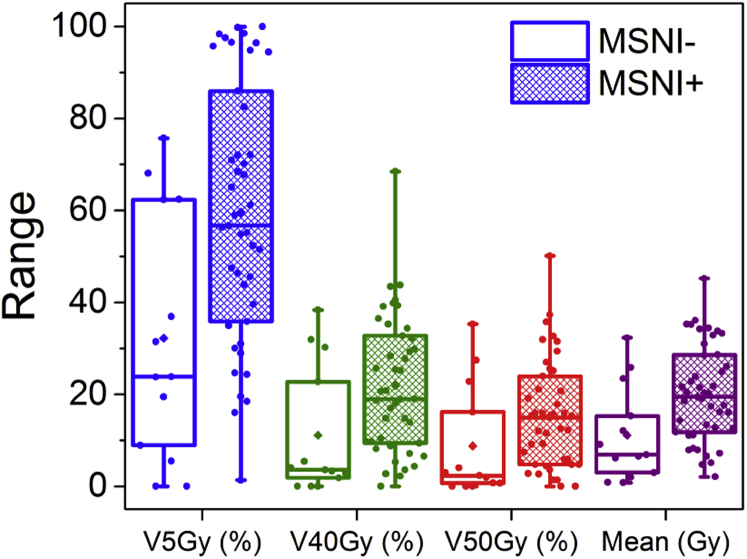
Results from the Spearman's rank correlation are shown in Table 2. When evaluating the interaction between individual lymph node stations and heart dose, level 7 involvement was associated with a higher dose to the heart in all parameters that were examined, including mean heart dose, V5 Gy, V40 Gy, and V50 Gy (P < .001 for all parameters). Level 9 involvement was significantly associated with a higher mean heart dose (P = .043), V5 Gy (P = .021), and V40 Gy (P = .0214), but not V50 Gy. Level 4L involvement was associated with higher V40 Gy (P = .031). Figure 1 and Table 3 show the distribution and median values in patients with and without level 7 involvement and the associated levels of significance. The remainder of the lymph node stations did not significantly affect any of the tested heart dose parameters.
Table 2.
Association of mean heart dose, V5 Gy, V40 Gy, and V50 Gy with nodal station involvement
| Mean Heart Dose Rho | V5 Gy (%) Rho | V40 Gy (%) Rho | V50 Gy (%) Rho | |
|---|---|---|---|---|
| 2R | −0.116 | −0.116 | −0.102 | −0.0786 |
| 2L | −0.104 | −0.182 | 0.0181 | 0.0072 |
| 3 | −0.0153 | −0.0153 | 0.0181 | 0.0209 |
| 4R | 0.0228 | 0.0541 | −0.00481 | −0.0373 |
| 4L | 0.204 | 0.141 | 0.288a | 0.225 |
| 5 | −0.0391 | −0.122 | 0.0269 | 0.044 |
| 6 | 0.141 | 0.165 | 0.153 | 0.147 |
| 7 | 0.534a | 0.518a | 0.534a | 0.487a |
| 8 | 0.199 | 0.219 | 0.15 | 0.143 |
| 9 | 0.272a | 0.307a | 0.307a | 0.155 |
| 10R | 0.143 | 0.208 | 0.0911 | 0.0511 |
| 10L | 0.179 | 0.144 | 0.201 | 0.216 |
Statistically significant.
Figure 1.
Box and whiskers plot, showing the distribution of values for mean hart dose, V5 Gy, V40 Gy, and V50 Gy in patients with and without level 7 nodal involvement. Differences in median values reached statistical significance for all parameters tested.
Table 3.
Median values for mean heart dose, V5 Gy, V40 Gy, and V50 Gy for patients with and without level 7 nodal involvement
| Level 7+ | Level 7− | MNSI+ | MNSI− | |
|---|---|---|---|---|
| Mean Dose (Gy) | 21.6 | 7.5a | 19.5 | 6.9b |
| V5 Gy (%) | 66.4 | 27.4a | 56.7 | 23.8b |
| V40 Gy (%) | 25.3 | 3.8a | 19 | 3.6c |
| V50 Gy (%) | 15.8 | 2.8a | 14.9 | 2.3b |
MSNI, multi-station nodal involvement.
P ≤ .001, and with and without MSNI.
P ≤ .05.
P ≤ .01.
Multistation nodal involvement
Patients who had 2 or more lymph node stations involved were found to have significantly higher heart doses for all parameters that were tested when compared with those who had only one station involved or no nodal involvement. The mean heart dose was reduced from 19.5 to 6.9 Gy (P = .005), V5 Gy from 56.7% to 23.8% (P = .005), V40 Gy from 19.0% to 3.6% (P = .009), and V50 Gy from 14.9% to 2.3% (P = .03). Figure 2 and Table 3 show the distribution of and median values in patients with and without multistation nodal involvement and the associated levels of significance.
Figure 2.
Box and whiskers plot, showing the distribution of values for mean hart dose, V5 Gy, V40 Gy, and V50 Gy in patients with and without multistation nodal involvement. Differences in median values reached statistical significance for all parameters tested.
Survival
After a median follow-up of 14.9 months (range, 2.6-123.2 months), the median OS for the entire cohort was 20.5 months. The estimated 2-year OS rate was 44.3 months.
Discussion
In RTOG 0617, one of the reported findings in the multivariate analysis was that heart V5 and V30 significantly increased the risk of death.1 However, neither acute nor late cardiac toxicities were specifically followed and therefore were not reported. Furthermore, heart doses were not compared between the standard and high dose groups. In older studies that used less conformal techniques and adequate dosing, such as RTOG 9410, grade 3 or greater acute and toxicities were noted to be 5% or less in all arms of patients, with only one death related to a cardiac event noted.8 Another study by Schytte et al,9 which retrospectively evaluated heart dose and toxicity for consecutive patients treated with definitive radiation therapy for NSCLC, found no correlation between mean heart dose to the entire heart, left ventricle, or both ventricles and cardiac events or survival. These studies suggest that although heart dose may be important, it may not be cardiac toxicity that is driving survival in this patient population.
In patients who undergo definitive radiation therapy with or without chemotherapy, Fernandes et al7 also found that subcarinal nodal involvement may be one of the most important factors driving survival in patients with stage III NSCLC. In this study, 106 patients were divided into 4 categories on the basis of the location of lymph node involvement. In patients with stage IIIA disease, even though no difference in local control was seen, there was a significant reduction in 2-year survival and distant failure rates observed among those with subcarinal involvement compared with patients without subcarinal involvement (24.1% vs. 52.6%, P = .016 and 28.4% vs. 61.2%, P = .043, respectively).
Further subgroup analysis beyond the correlation of location and extent of mediastinal lymph node involvement and heart dose in our patient population was limited because of the number of patients included in the analysis and the relatively short follow-up period. Therefore, the overall number of events did not allow for an analysis of the effect of heart dose on survival or other endpoints, such as local control or toxicity. Additionally, due to the retrospective nature of this study, our patient population was fairly heterogeneous with regard to work up, follow-up, treated dose, radiation treatment technique, and systemic therapy, and these differences may potentially have confounded the results.
In our study, we showed that both location and extent of mediastinal lymph node involvement correlates with heart dose on a number of dosimetric parameters. Because of the small number of patients in our cohort and a relatively short follow-up, we did not have adequate patient numbers to evaluate survival as a function of heart dose or nodal station involvement. However, our results suggest that heart dose may be a surrogate for extent and location of mediastinal nodal involvement rather than an independent predictor of survival. Further prospective analysis with larger patient numbers and longer follow-up will be required to validate our findings and assess whether heart dose is an independent predictor of survival in patients with locally advanced NSCLC.
References
- 1.Bradley J.D., Paulus R., Komaki R., Masters G., Blumenschein G., Schild S. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): A randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015;16:187–199. doi: 10.1016/S1470-2045(14)71207-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iwasaki A., Shirakusa T., Miyoshi T., Hamada T., Enatsu S., Maekawa S. Prognostic significance of subcarinal station in non-small cell lung cancer with T1-3 N2 disease. Thorac Cardiovasc Surg. 2006;54:42–46. doi: 10.1055/s-2005-865828. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe Y., Hayashi Y., Shimizu J., Oda M., Iwa T. Mediastinal nodal involvement and the prognosis of non-small cell lung cancer. Chest. 1991;100:422–428. doi: 10.1378/chest.100.2.422. [DOI] [PubMed] [Google Scholar]
- 4.Okada M., Tsubota N., Yoshimura M., Miyamoto Y., Matsuoka H. Prognosis of completely resected pN2 non-small cell lung carcinomas: What is the significant node that affects survival? J Thorac Cardiovasc Surg. 1999;118:270–275. doi: 10.1016/S0022-5223(99)70217-5. [DOI] [PubMed] [Google Scholar]
- 5.Lee J.G., Lee C.Y., Park I.K., Kim D.J., Cho S.H., Kim K.D. The prognostic significance of multiple station N2 in patients with surgically resected stage IIIA N2 non-small cell lung cancer. J Korean Med Sci. 2008;23:604–608. doi: 10.3346/jkms.2008.23.4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Misthos P., Sepsas E., Kokotsakis J., Skottis I., Lioulias A. The significance of one-station N2 disease in the prognosis of patients with nonsmall-cell lung cancer. Ann Thorac Surg. 2008;86:1626–1630. doi: 10.1016/j.athoracsur.2008.07.076. [DOI] [PubMed] [Google Scholar]
- 7.Fernandes A.T., Mitra N., Xanthopoulos E., Evans T., Stevenson J., Langer C. The impact of extent and location of mediastinal lymph node involvement on survival in Stage III non-small cell lung cancer patients treated with definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2012;83:340–347. doi: 10.1016/j.ijrobp.2011.05.070. [DOI] [PubMed] [Google Scholar]
- 8.Curran W.J., Jr., Paulus R., Langer C.J., Komaki R., Lee J.S., Hauser S. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: Randomized phase III trial RTOG 9410. J Natl Cancer Inst. 2011;103:1452–1460. doi: 10.1093/jnci/djr325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schytte T., Hansen O., Stolberg-Rohr T., Brink C. Cardiac toxicity and radiation dose to the heart in definitive treated non-small cell lung cancer. Acta Oncol. 2010;49:1058–1060. doi: 10.3109/0284186X.2010.504736. [DOI] [PubMed] [Google Scholar]