Abstract
The goal of the current study was to examine the relationships between insight and both cognitive function and depression in schizophrenia and schizoaffective disorder, and to determine if there were similar relationships across diagnostic categories. We examined discrepancies between self and informant reports of function on the Specific levels of function scale as a metric of insight for interpersonal, social acceptance, work and activities. We examined two samples of individuals with schizophrenia and/or schizoaffective disorder (Ns of 188 and 67 respectively). In Sample 1, cognition was measured using the Dot Probe Expectancy Task. In Sample 2, cognition was measured by averaging several subtests from the MATRICS consensus cognitive battery, as well as additional measures of working memory. In both samples, depression was measured using the Brief Psychiatric Rating Scale. In both samples, we found significant relationships between worse cognition and overestimations of work function, as well as between higher depression levels and underestimation of interpersonal function. These relationships were specific to interpersonal and work function, with significantly stronger correlations with interpersonal and work function compared to the other areas of function. Similar results were found across diagnostic categories. These results have important implications for treatment planning, as they suggest the need to take into account depression and cognitive function when evaluating the patient's self-report of function, and highlight the utility of informant reports in evaluating function and treatment planning. Further, they add to the literature on the similarity across schizophrenia and schizoaffective disorder in a variety of pathological mechanisms.
Keywords: Insight, Psychosis, Depression, Cognition, Function, Interpersonal
1. Introduction
Schizophrenia is a debilitating psychiatric disorder associated with disruptions to work and educational function (Andreasen and Flaum, 1991). One frequent feature of schizophrenia is impairments in insight (Mintz et al., 2003), defined as awareness of one's psychiatric symptoms and level of functioning. Impaired insight in schizophrenia has been linked to higher rates of depression and more impaired cognition (Bowie et al., 2007), and may make it difficult for individuals with psychosis to accurately convey to clinicians and psychologists their level of function and thus to receive the medical and therapeutic attention that they need (Siu et al., 2015).
Schizophrenia is typically associated with cognitive impairments (Barch and Ceaser, 2012, Green, 1996, Green et al., 2004a), which in turn are associated with lower levels of social and occupational functioning (Gould et al., 2013). Gilleen and colleagues (Gilleen et al., 2016) suggested that good cognitive functioning is necessary, though not sufficient, for good insight into one's level of functioning. Importantly, individuals with schizophrenia who have poor cognitive function may overestimate their level of functioning (Bowie et al., 2007, Nair et al., 2014, Shad et al., 2006, Siu et al., 2015, Stratton et al., 2013), sometimes even to such an extreme that they will deny having a mental illness (Bedford and David, 2014).
Many individuals with schizophrenia also experience significant levels of depression (Avgustin, 2009, Bosanac and Castle, 2013), which is related to insight (Ampalam et al., 2012, Bowie et al., 2007, Gharabawi et al., 2007, Palmer et al., 2015). An extensive literature suggests that depressed people have a more realistic view, albeit often more negative, of themselves than non-depressed people (Soderstrom et al., 2011). This idea is termed “depressive realism” (Alloy and Abramson, 1979, Alloy and Abramson, 1988). An additional perspective is that patients who can comprehend more about how their illness negatively affects them (i.e., who have greater insight) become more depressed (Misdrahi et al., 2014, Palmer et al., 2015), a relationship termed the “insight paradox.” Both of these theories would suggest that depressed individuals with psychosis should have better insight. However, depression can also be associated with high levels of self-blaming and feelings of inadequacy and hopelessness (Zahn et al., 2015). Thus, depression may lead the individual to under estimate their level of function. Recent work by Harvey and colleagues is more consistent with the depressive realism or insight paradox hypotheses, showing that individuals with schizophrenia and schizoaffective disorder who were higher in self-reported depression were more accurate reporters as to their interpersonal, everyday activity, and vocational function (Harvey et al., 2016).
One important question not yet clearly addressed in the prior literature is the degree to which the relationships among insight, depression and cognition are similar among putatively different diagnostic categories among the schizophrenia spectrum disorders, such as schizophrenia versus schizoaffective disorder. There is some evidence that insight may be more intact among individuals with schizoaffective disorder versus schizophrenia (Birindelli et al., 2014, Wiffen et al., 2010), though recent work by Harvey and colleagues did not see evidence for greater insight among individuals with schizoaffective disorder (Harvey et al., 2016). There is also evidence for higher depression levels in schizoaffective disorder (e.g., Birindelli et al., 2014, Harvey et al., 2016, Woodberry et al., 2008). However, the level of cognitive impairment is similar across schizophrenia and schizoaffective disorder (Bora et al., 2009, Fiszdon et al., 2007, Owoso et al., 2013, Reichenberg et al., 2009). Several previous studies included both individuals with schizophrenia and schizoaffective disorder, and some studies explicitly controlled for diagnosis when examining such relationships (Onwuameze et al., 2016). However, no study has yet directly compared the magnitude of these interrelationships across schizophrenia and schizoaffective disorder.
Our goal was to examine the relationships between insight and both cognitive function and depression in both schizophrenia and schizoaffective disorder. We used the discrepancies between self and a knowledgeable informant's report of function on the Specific Levels of Function (SLOF) scale as a metric of insight (Bowie et al., 2007, Corriveau and Sousa, 2013). We predicted that individuals with psychosis with more severe cognitive impairment would over-estimate their level of function (Bowie et al., 2007). Further, we wished to determine whether depression in schizophrenia would be associated with greater insight or with impaired insight. If impaired, we predicted that greater depression would lead patients to under-estimate their level of function (Siu et al., 2015). Lastly, we asked whether there were any significant differences between individuals with schizophrenia and schizoaffective disorder in these relationships.
2. Materials and methods
2.1. Participants
Participant data were taken from several samples recruited by the Cognitive Neuroscience Test Reliability and Clinical Applications for Schizophrenia Consortium (CNTRACS). The recruitment, assessment and inclusion/exclusion procedures both Sample 1 (a combination of two studies) (Henderson et al., 2012) (Strauss et al., 2013) and Sample 2 (Barch et al., 2017) are described in Supplemental materials. We examined only those participants who had informant rated functional status. This resulted in a total of 188 individuals with schizophrenia (N = 138) or schizoaffective disorder (N = 50) in Sample 1 and 67 in Sample 2 (35 schizophrenia, 32 schizoaffective).
2.2. Specific levels of functioning scale
The specific levels of functioning (SLOF) scale assess the level of functioning on four different subscales: interpersonal, social acceptance, activities, and work. Participants completed the SLOF during one of their testing sessions and provided the name of a knowledgeable informant. Study staff then either conducted a phone interview to obtain informant SLOF scores, or sent the informant a paper version with a stamped return envelope. The informant received $10 for completing the SLOF. We used the difference between self and informant SLOF reports as a proxy for insight (Figs. S1-S4 for histograms). A positive value meant that the patient rated themselves as doing better than the informant rated them. A negative value meant that the patient rated themselves as doing worse than the informant rated them.
2.3. Cognitive tasks
In Sample 1, the Dot Probe Expectancy (DPX) task was used to assess cognitive function, as described in (Henderson et al., 2012) and in Supplemental materials. The testing for Sample 2 did not include the DPX. Thus, instead we created an average cognition variable by combining the following tasks: 1) three subtests of the MATRICs consensus cognitive battery (Digit Symbol, Hopkins Verbal Learning (HVLT), and letter number sequencing (LNS)(Green et al., 2004b, Kern et al., 2008); 2) two versions of a running span working memory task (Broadway and Engle, 2010) (Supplemental materials); 3) two versions of a change detection working memory task (Supplemental materials); and 4) two versions of a change localization working memory task (Supplemental materials)(Gold et al., 2010, Gold et al., 2003). We z-scored (using the patient data) the primary dependent variable from each task and averaged them. This approach meant that we used different measures of cognition across samples, but provides greater evidence for generalizability across samples.
2.4. Diagnosis and clinical assessment
Diagnostic assessments were conducted or supervised by a master's level clinician using the Structured Clinical Interview for DSM-IV-Text Revision and the 24-item Brief Psychiatric Rating Scale (First et al., 2002, Ventura et al., 1993a, Ventura et al., 1993b). See Supplemental materials for details. We focused on the BPRS depression subscale (items 2, 3, 4 and 5; anxiety, depression, suicidality, and guilt) (Ventura et al., 1993b), but examined positive, negative, and disorganized symptoms as potential confounders in Supplemental materials.
2.5. Data processing and statistical analyses
We first examined the correlations between individual self-informant SLOF report discrepancy scores and BPRS depression and cognition measures separately for Samples 1 and 2. We used False Discovery Rate (FDR) to correct for the false positive rate (Benjamini and Yekutieli, 1995, Benjamini and Yekutieli, 2001). To better understand the source of the effects, we converted the dimensional scores into groups of over-estimators (+ 0.5 SD for the discrepancy score and greater), under-estimators (− 0.5 SD for the discrepancy score and lower) and accurate estimators (within + − 0.5 SD). This analysis was meant to characterize the pattern established by the primary dimensional analyses. To do so, we combined the two samples by Z-scoring all of the variables within each patient sample, as the number of participants in Sample 2 would lead to small Ns within subgroups. We used this combined sample to create the “groups” described above and to compare schizophrenia to schizoaffective disorder, so as to maximize power. We conducted regression analyses with diagnostic group, the discrepancy score, and the interaction between diagnosis and discrepancy score to predict either depression or cognition. In the Supplemental materials we report on analyses using residualized change scores to assess the relative contributions of self- versus informant-reports, as well as potential demographic or clinical confounders.
3. Results
3.1. Sample 1
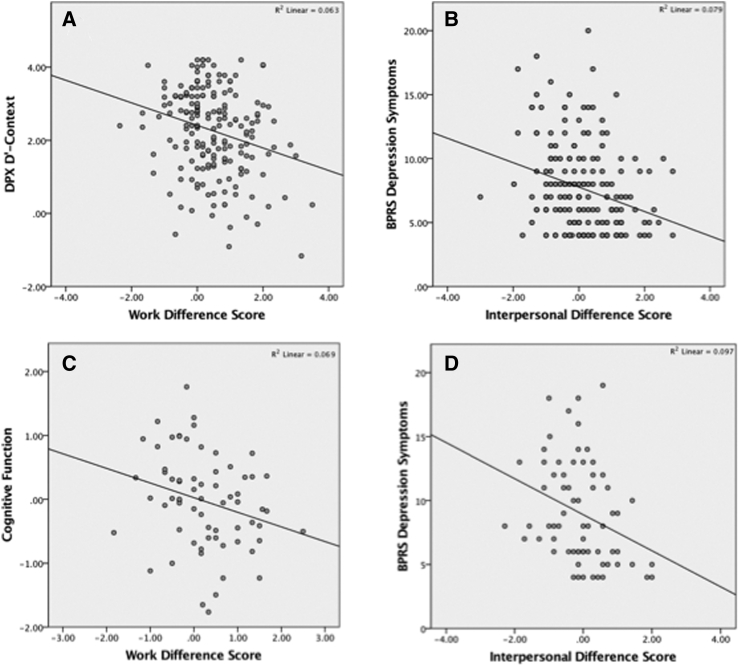
As shown in Table 1, performance on the DPX was significantly correlated with the work discrepancy score, which survived FDR correction. Further, using tests to compare dependent correlations (Meng et al., 1992), the work discrepancy score was significantly more correlated with DPX performance than the social acceptance (Z = − 3.07, p < 0.001), interpersonal (Z = − 2.28, p = 0.011), and activities (Z = − 3.27, p = 0.002) discrepancy scores. As shown in Fig. 1a, worse cognitive function was associated with the individual rating themselves as having better work function than they were rated by the informant.
Table 1.
Relationships between self-other discrepancy scores and depression and cognition.
| Activities discrepancy score |
Interpersonal discrepancy score |
Social acceptance discrepancy score |
Work discrepancy score |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | r | p | r | p | r | p | r | p |
| Sample 1 | ||||||||
| BPRS depression | − 0.13 | 0.08 | − 0.28 | < 0.001 | − 0.003 | 0.97 | − 0.18 | 0.013 |
| DPX | 0.02 | 0.82 | − 0.08 | 0.26 | 0.04 | 0.56 | − 0.25 | < 0.001 |
| Sample 2 | ||||||||
| BPRS depression | 0.15 | 0.11 | − 0.31 | 0.005 | − 0.007 | 0.48 | − 0.13 | 0.16 |
| Cognition composite | − 0.03 | 0.42 | − 0.24 | 0.025 | − 0.07 | 0.30 | − 0.26 | 0.016 |
*p < 0.05, **p < 0.01.
Fig. 1.
A) Relationship between work discrepancy score and DPX D′-context in Sample 1; B) Relationship between interpersonal discrepancy score and BPRS depression in Sample 1; C) Relationship between work discrepancy score and DPX D′-context in Sample 2; D) Relationship between interpersonal discrepancy score and BPRS depression in Sample 2.
BPRS depression was significantly correlated with the discrepancy scores for work and interpersonal function (Table 1), both of which survived FDR correction, but not with the scores for activities or social acceptance. Greater depression was associated with the individual rating themselves as having worse interpersonal function than they were rated by the informant (Fig. 1b). Interpersonal discrepancy scores were significantly more correlated with BPRS depression than both the social acceptance (Z = − 2.80, p = 0.002) and activities discrepancy scores (Z = − 1.92, p = 0.027), and the work discrepancy score was significantly more correlated with BPRS depression than the social acceptance discrepancy score (Z = − 1.87, p = 0.03).
3.2. Sample 2
In Sample 2, cognition was again negatively associated with both work and interpersonal discrepancy scores (Table 1 and Fig. 1c). These correlations also survived FDR correction (Table 1). For Sample 2, BPRS depression scores were again significantly associated with the interpersonal discrepancy score (Table 1 and Fig. 1d), a relationship that survived FDR correction. However, we did not see a significant correlation between BPRS depression and the work discrepancy score in Sample 2, though Fisher's r to Z transform analyses did not indicate a significant difference in the magnitude of the correlations across the two samples (rs of − 0.18 versus − 0.13 respectively, Z = 0.35, p = 0.36).
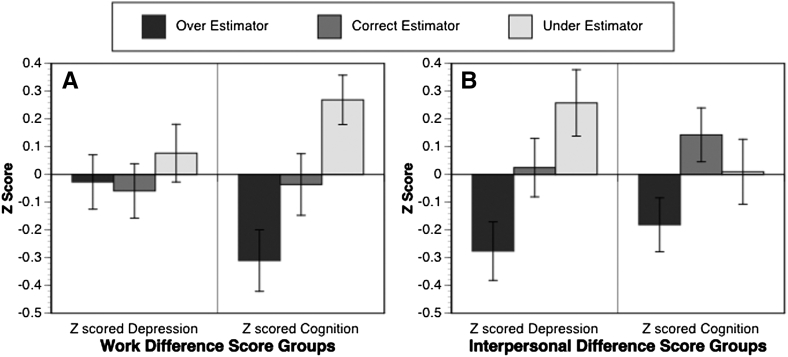
3.3. Categorical analysis
To better understand the nature of these associations, we examined relationships of the categorical self vs. informant groupings to the cognitive measures and BPRS depression. For the work discrepancy score groups, there were 71 over-estimators, 90 correct estimators, and 94 under-estimators. For the interpersonal discrepancy score groups, there were 81 over-estimators, 97 correct estimators and 77 under-estimators. For the work discrepancy score groups, there was a significant effect for cognition (F(2252) = 7.23, p = 0.001), but not for depression (F(2252) = 0.46, p = 0.63). As shown in Fig. 2a, post-hoc contrasts indicated that over-estimators had worse cognition scores than under-estimators (Cohen's D = 0.58, p < 0.001), with a trend to also have worse cognition than the correct estimators (Cohen's D = 0.27, p = 0.078). The correct estimators also had worse cognition than the under-estimators (Cohen's D = 0.30, p = 0.03). For the interpersonal discrepancy score groups (Fig. 2b), there was a significant effect for depression (F(2252) = 5.92, p = 0.003), but not for cognition (F(2252) = 2.36, p = 0.097). As shown in Fig. 2, posthoc contrasts indicated that under-estimators had higher depression scores than over-estimators (Cohen's D = 0.53, p = 0.001), but did not differ significantly from correct-estimators (Cohen's D = 0.23, p = 0.12). Correct estimators had greater depression than over-estimators (Cohen's D = 0.30, p = 0.042).
Fig. 2.
A) Graph illustrating the relationships of depression and cognitive function to groups defined by the magnitude of the self-informant interpersonal discrepancy score; B) Graph illustrating the relationships of depression and cognitive function to groups defined by the magnitude of the self-informant work discrepancy score.
3.4. Schizophrenia versus schizoaffective disorder
The diagnostic groups did not differ in age, gender, personal education, parental education, or cognitive function (Table 2). The individuals with schizoaffective disorder had higher BPRS depression and lower disorganization symptoms than those with schizophrenia, but did not differ in positive or negative symptoms (Table 2). The groups differed in both the interpersonal and work discrepancy scores, with more positive values in schizophrenia. The regression using the work discrepancy score to predict cognition indicated a main effect of work score (t = − 4.22, β = − 0.27, p < 0.001), but no main effect of diagnosis (t = − 0.94, β = − 0.06, p = 0.35), or interaction between diagnosis and work score (t = − 0.51, β = − 0.03, p = 0.61). Follow up correlations indicated that the work score and cognition were significantly correlated in both schizophrenia (r = − 0.23, p = 0.002) and schizoaffective disorder (r = − 0.31, p = 0.005). The regression using the interpersonal discrepancy score to predict BPRS depression also indicated a main effect of interpersonal score (t = − 2.76, β = − 0.20, p = 0.006), but no main effect of diagnosis (t = 0.61, β = 0.04, p = 0.54), or interaction (t = 0.44, β = 0.03, p = 0.66). Follow up correlations indicated that the interpersonal score and cognition were significantly correlated in schizophrenia (r = − 0.24, p = 0.001) but not schizoaffective disorder (r = − 0.14, p = 0.22).
Table 2.
Clinical and demographic characteristics of schizophrenia versus schizoaffective disorder.
| Schizophrenia (N = 173) |
Schizoaffective (N = 82) |
T-value | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Age | 38.6 | 12.0 | 40.9 | 11.0 | -1.48 | 0.14 |
| Gender (% male) | 64% | 52% | 3.2 | 0.07 | ||
| Patient years of school | 13.6 | 2.64 | 13.5 | 3.16 | 0.29 | 0.77 |
| Parent years of school | 14.7 | 3.1 | 14.3 | 3.33 | 0.84 | 0.40 |
| BPRS depression | 7.42 | 3.34 | 9.12 | 3.94 | − 3.57 | 0.001 |
| BPRS positive symptoms | 8.52 | 4.72 | 7.68 | 4.15 | 1.38 | 0.17 |
| BPRS negative symptoms | 7.41 | 2.95 | 6.69 | 2.64 | 1.87 | 0.06 |
| BPRS disorganization symptoms | 5.20 | 1.76 | 4.7 | 1.29 | 2.26 | 0.025 |
| Z-scored cognition | 0.0162 | 0.97 | − 0.0341 | 1.04 | 0.38 | 0.71 |
| Z-scored interpersonal discrepancy score | 0.1032 | 1.03 | − 0.2177 | 0.89 | 2.42 | 0.016 |
| Z-scored work discrepancy score | 0.0841 | 0.97 | − 0.1774 | 1.05 | 1.97 | 0.05 |
4. Discussion
The current study found a significant relationship between cognition and the discrepancy in self versus informant reports of work function for two independent samples, such that individuals who overestimated their work function had more impaired cognition. These findings are consistent with prior work that also found that patients who over-estimate their level of functioning tend to have lower levels of cognition (Siu et al., 2015). We found that the relationships between cognition and insight about work function was signifciantly stronger than the relationship between cognition and insight in regards to interpersonal, social acceptance or community activities. This suggests that cognitive function is particularly critical for a patient's understanding of their occupational or academic capabilities. However, as shown in supplemental analyses, we also found that the the magnitude of the discrepancy itself may not be as strongly related to cognition as the informant report itself when assessed using residualized change scores that are less dependent on baseline scores. This finding highlights the need for informant reports to evaluate work function levels in schizophrenia.
In both samples, higher depressive symptoms were significantly related to patients under-estimating their interpersonal function. The finding of a significant relationship between depression and underestimating one's interpersonal function is consistent with prior work in schizophrenia (Palmer et al., 2015) and with prior work showing that people with depressive symptoms often have a negative self-bias (Zahn et al., 2015). Further, we found that although depression levels were related to the patient's own report of interpersonal function, the discrepancy scores continued to relate to depression even when we used residualized change scores, as described in supplemental analyses. This finding suggests that depression is related to the actual magnitude of the discrepancy between informant- and self-report, as well as to the patient's self-evaluation of their interpersonal function. Our findings differ somewhat from those of Harvey and colleagues, who found that greater depression in psychotic individuals was associated with more accurate self-assessment, but did not find evidence for underestimation of function in the most depressed individuals (Harvey et al., 2016). It is possible that the differences across these studies are related to the method of depression assessment. Harvey and colleagues used self-report on the Beck Depression Inventory, while we used clinician ratings on the Brief Psychiatric Rating Scale. It would be important in future work to collect both types of assessment in the same individuals to determine whether they show differential relationships to insight.
As has been seen in some prior work (Birindelli et al., 2014, Wiffen et al., 2010), though not all (Harvey et al., 2016), we found that individuals with schizophrenia and schizoaffective disorder had different levels of insight. On average, there were no significant differences in the self-versus informant report for either interpersonal or work function in schizophrenia. However, the individuals with schizoaffective disorder provided significantly lower evaluations of their interpersonal function compared to informant. Further, the individuals with schizoaffective disorder had higher depression levels than the individuals with schizophrenia, consistent with prior work (e.g., Birindelli et al., 2014, Woodberry et al., 2008). However, the two diagnostic groups did not differ in cognitive function, again consistent with prior work (Bora et al., 2009, Fiszdon et al., 2007, Owoso et al., 2013, Reichenberg et al., 2009). Importantly, the relationships between the interpersonal discrepancy score and depression did not differ as a function of diagnostic group and were significant in each group independently. There was a significant correlation between the interpersonal discrepancy score and BPRS depression in schizophrenia, and this correlation was in the same direction in the schizoaffective group, though not significant. These results add to the literature suggesting that both schizophrenia and schizoaffective disorder should be considered on the same continuum of psychosis, and point to the interrelationship across insight, depression, and cognitive function across diagnostic categories.
4.1. Limitations and future directions
Our participants were medicated and it would be important in future work to understand whether medication status influenced the relationship between self and informant reported function. In addition, this study was cross-sectional and thus we could not address the causal relationship between either depression and cognition and insight. It will also be important to determine whether we see similar findings in other clinical groups to determine if these relationships are unique to psychosis. Lastly, asking more than one informant may provide an even a better representation of the patient's level of function. However, it can be difficult to engage even one informant, making the use of multiple informants challenging.
5. Conclusion
The current study provides further evidence that both depression and cognitive function are related to insight in schizophrenia, as measured by discrepancies between self and informant reports. Importantly, both of these findings replicated across two independent samples and across schizophrenia and schizoaffective disorder. These results suggest that a patient's level of cognitive function should be considered when evaluating their reports of occupational or academic function, or in when evaluating the feasibility of successfully starting new occupational pursuits. They also suggest that depression level should be considered when evaluating a patient's report of interpersonal function. These results also suggest that it may be particularly important to obtain an informant's perspective on the patient's function when they either have low levels of cognitive function or high levels of depression to most realistically evaluate what they are capable of and when they may need further support or intervention.
Funding body agreements and policies
Funding for this study was provided by NIMH ROI1s MH084840 (DMB), MH084826 (CSC), MH084821 (JMG), MH084861 (AWM) and MH084828 (SMS).
Contributors
Authors JE & DMB had full access to all study data and take responsibility for the integrity of the data and accuracy of the data analysis. JE and DMB performed the data analysis. JE and DMB drafted the initial manuscript. All authors developed the study concept and design and aided in interpretation and provided critical revisions. All authors approved the final version of the paper for submission.
Conflict of interest
JE has no conflicts to report. CSC has received research grants from the National Institutes of Health (NIH), the Brain and Behavior Foundation, the Burroughs Wellcome foundation, GlaxoSmithKline, and the Robert Wood Johnson Foundation and has been an external consultant for Lilly, Merck, Pfizer, Roche, and Servier. JMG has received grants from National Institutes of Health (NIH), receives royalty payments from Brief Assessment of Cognition in Schizophrenia, and has acted as a consultant to Amgen, AstraZeneca, GlaxoSmithKline, Hoffman LaRoche, Merck, Pfizer, and Solvay. AWM has received research grants from the National Institutes of Health (NIH) and the Brain & Behavior Research Foundation. JDR has received research grants from the National Institutes of Health (NIH), the Brain & Behavior Research Foundation, the EJLB Foundation, and the Robert Wood Johnson Foundation. SMS has received research grants from the National Institutes of Mental Health (NIMH), The Brain & Behavior Research Foundation, the van Ameringen Foundation, the Jacob and Valeria Langaloth Foundation, the New England Research Institutes, the New York State Office of Mental Health, the New Jersey Division of Mental Health and Addiction Services, Janssen Pharmaceuticals, AstraZeneca, and Pfizer. MES has no conflicts to report. DMB has received grants from the Brain & Behavior Research Foundation and the National Institutes of Health (NIH), and is a consultant for Pfizer, Amgen, Upsher-Smith and Takeda on studies related to the treatment of negative symptoms in schizophrenia.
Acknowledgements
The authors would like to thank the participants in this study, who gave generously of their time.
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.scog.2017.04.001.
Contributor Information
Julia Ermel, Email: juliaermel@wustl.edu.
Cameron S. Carter, Email: cscarter@ucdavis.edu.
James M. Gold, Email: JGOLD@mprc.umaryland.edu.
Angus W. MacDonald, III, Email: angus@umn.edu.
J. Daniel Ragland, Email: jdragland@ucdavis.edu.
Steven M. Silverstein, Email: steven.silverstein@rutgers.edu.
Milton E. Strauss, Email: milton.strauss@gmail.com.
Deanna M. Barch, Email: dbarch@wustl.edu.
Appendix A. Supplementary data
Supplementary material
References
- Alloy L.B., Abramson L.Y. Judgment of contingency in depressed and nondepressed students: sadder but wiser? J. Exp. Psychol. Gen. 1979;108:441–485. doi: 10.1037//0096-3445.108.4.441. [DOI] [PubMed] [Google Scholar]
- Alloy L.B., Abramson L.Y. Deprssive realism: four theoretical perspectives. In: Alloy L.B., editor. Cognitive Processes in Depression. Guildford Press; New York: 1988. pp. 223–265. [Google Scholar]
- Ampalam P., Deepthi R., Vadaparty P. Schizophrenia – insight, depression: a correlation study. Indian J. Psychol. Med. 2012;34(1):44–48. doi: 10.4103/0253-7176.96158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen N.C., Flaum M. Schizophrenia: the characteristic symptoms. Schizophr. Bull. 1991;17(1):27–49. doi: 10.1093/schbul/17.1.27. [DOI] [PubMed] [Google Scholar]
- Avgustin B. Depression in schizophrenia - literature overview. Psychiatr. Danub. 2009;21(Suppl. 1):93–97. [PubMed] [Google Scholar]
- Barch D.M., Ceaser A.E. Cognition in schizophrenia: core psychological and neural mechanisms. Trends Cogn. Sci. 2012;16:27–34. doi: 10.1016/j.tics.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch D.M., Carter C.S., Gold J.M., Johnson S.L., Kring A.M., MacDonald A.W., III, Pizzagalli D., Ragland D., Silverstein S.M., Strauss M.E. Explicit and implicit reinforcement learning across the psychosis spectrum. J. Abnorm. Psychol. 2017 doi: 10.1037/abn0000259. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedford N.J., David A.S. Denial of illness in schizophrenia as a disturbance of self-reflection, self-perception and insight. Schizophr. Res. 2014;152(1):89–96. doi: 10.1016/j.schres.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Benjamini Y., Yekutieli D. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. 1995;57:289–300. [Google Scholar]
- Benjamini Y., Yekutieli D. The control of the false discovery rate: a practical and powerful approach to multiple testing. Ann. Stat. 2001;29(4):1165–1188. [Google Scholar]
- Birindelli N., Montemagni C., Crivelli B., Bava I., Mancini I., Rocca P. Cognitive functioning and insight in schizophrenia and in schizoaffective disorder. Riv. Psichiatr. 2014;49(2):77–83. doi: 10.1708/1461.16143. [DOI] [PubMed] [Google Scholar]
- Bora E., Yucel M., Pantelis C. Cognitive functioning in schizophrenia, schizoaffective disorder and affective psychoses: meta-analytic study. Br. J. Psychiatry. 2009;195(6):475–482. doi: 10.1192/bjp.bp.108.055731. [DOI] [PubMed] [Google Scholar]
- Bosanac P., Castle D.J. Schizophrenia and depression. Med. J. Aust. 2013;199(6 Suppl):S36–S39. doi: 10.5694/mja12.10516. [DOI] [PubMed] [Google Scholar]
- Bowie C.R., Twamley E.W., Anderson H., Halpern B., Patterson T.L., Harvey P.D. Self-assessment of functional status in schizophrenia. J. Psychiatr. Res. 2007;41(12):1012–1018. doi: 10.1016/j.jpsychires.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadway J.M., Engle R.W. Validating running memory span: measurement of working memory capacity and links with fluid intelligence. Behav. Res. Methods. 2010;42(2):563–570. doi: 10.3758/BRM.42.2.563. [DOI] [PubMed] [Google Scholar]
- Corriveau D.P., Sousa S. Levels of recovery scale (LORS): psychometric properties of a new instrument to assess psychotic symptoms and patient awareness. Psychol. Rep. 2013;113(2):435–440. doi: 10.2466/03.07.02.PR0.113x20z0. [DOI] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Miriam G., Williams J.B.W. Biometrics Research. New York State Psychiatric Institute; New York: 2002. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition (SCID-I/P) [Google Scholar]
- Fiszdon J.M., Richardson R., Greig T., Bell M.D. A comparison of basic and social cognition between schizophrenia and schizoaffective disorder. Schizophr. Res. 2007;91(1–3):117–121. doi: 10.1016/j.schres.2006.12.012. [DOI] [PubMed] [Google Scholar]
- Gharabawi G., Bossie C., Turkoz I., Kujawa M., Mahmoud R., Simpson G. The impact of insight on functioning in patients with schizophrenia or schizoaffective disorder receiving risperidone long-acting injectable. J. Nerv. Ment. Dis. 2007;195(12):976–982. doi: 10.1097/NMD.0b013e31815c1982. [DOI] [PubMed] [Google Scholar]
- Gilleen J., David A., Greenwood K. Self-reflection and set-shifting mediate awareness in cognitively preserved schizophrenia patients. Cogn. Neuropsychiatry. 2016;21(3):185–196. doi: 10.1080/13546805.2016.1167031. [DOI] [PubMed] [Google Scholar]
- Gold J.M., Wilk C.M., McMahon R.P., Buchanan R.W., Luck S.J. Working memory for visual features and conjunctions in schizophrenia. J. Abnorm. Psychol. 2003;112(1):61–71. [PubMed] [Google Scholar]
- Gold J.M., Hahn B., Zhang W.W., Robinson B.M., Kappenman E.S., Beck V.M., Luck S.J. Reduced capacity but spared precision and maintenance of working memory representations in schizophrenia. Arch. Gen. Psychiatry. 2010;67(6):570–577. doi: 10.1001/archgenpsychiatry.2010.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould F., Sabbag S., Durand D., Patterson T.L., Harvey P.D. Self-assessment of functional ability in schizophrenia: milestone achievement and its relationship to accuracy of self-evaluation. Psychiatry Res. 2013;207(1–2):19–24. doi: 10.1016/j.psychres.2013.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M.F. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatr. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green M.F., Kern R.S., Heaton R.K. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr. Res. 2004;72(1):41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Green M.F., Nuechterlein K.H., Gold J.M., Barch D.M., Cohen J., Essock S., Fenton W.S., Frese F., Goldberg T.E., Heaton R.K., Keefe R.S., Kern R.S., Kraemer H., Stover E., Weinberger D.R., Zalcman S., Marder S.R. Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol. Psychiatry. 2004;56(5):301–307. doi: 10.1016/j.biopsych.2004.06.023. [DOI] [PubMed] [Google Scholar]
- Harvey P.D., Twamley E.W., Pinkham A.E., Depp C.A., Patterson T.L. Depression in schizophrenia: associations with cognition, functional capacity, everyday functioning, and self-assessment. Schizophr. Bull. 2016 doi: 10.1093/schbul/sbw103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson D., Poppe A.B., Barch D.M., Carter C.S., Gold J.M., Ragland J.D., Silverstein S.M., Strauss M.E., MacDonald A.W., 3rd Optimization of a goal maintenance task for use in clinical applications. Schizophr. Bull. 2012;38(1):104–113. doi: 10.1093/schbul/sbr172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern R.S., Nuechterlein K.H., Green M.F., Baade L.E., Fenton W.S., Gold J.M., Keefe R.S., Mesholam-Gately R., Mintz J., Seidman L.J., Stover E., Marder S.R. The MATRICS consensus cognitive battery, part 2: co-norming and standardization. Am. J. Psychiatry. 2008;165(2):214–220. doi: 10.1176/appi.ajp.2007.07010043. [DOI] [PubMed] [Google Scholar]
- Meng X., Rosenthal R., Rubin D.B. Comparing correlated correlation coefficients. Psychol. Bull. 1992;111:172–175. [Google Scholar]
- Mintz A.R., Dobson K.S., Romney D.M. Insight in schizophrenia: a meta-analysis. Schizophr. Res. 2003;61(1):75–88. doi: 10.1016/s0920-9964(02)00316-x. [DOI] [PubMed] [Google Scholar]
- Misdrahi D., Denard S., Swendsen J., Jaussent I., Courtet P. Depression in schizophrenia: the influence of the different dimensions of insight. Psychiatry Res. 2014;216(1):12–16. doi: 10.1016/j.psychres.2014.01.039. [DOI] [PubMed] [Google Scholar]
- Nair A., Palmer E.C., Aleman A., David A.S. Relationship between cognition, clinical and cognitive insight in psychotic disorders: a review and meta-analysis. Schizophr. Res. 2014;152(1):191–200. doi: 10.1016/j.schres.2013.11.033. [DOI] [PubMed] [Google Scholar]
- Onwuameze O.E., Uga A., Paradiso S. Longitudinal assessment of clinical risk factors for depression in schizophrenia spectrum disorders. Ann. Clin. Psychiatry. 2016;28(3):167–174. [PubMed] [Google Scholar]
- Owoso A., Carter C.S., Gold J.M., MacDonald A.W., 3rd, Ragland J.D., Silverstein S.M., Strauss M.E., Barch D.M. Cognition in schizophrenia and schizo-affective disorder: impairments that are more similar than different. Psychol. Med. 2013;43(12):2535–2545. doi: 10.1017/S0033291713000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer E.C., Gilleen J., David A.S. The relationship between cognitive insight and depression in psychosis and schizophrenia: a review and meta-analysis. Schizophr. Res. 2015;166(1–3):261–268. doi: 10.1016/j.schres.2015.05.032. [DOI] [PubMed] [Google Scholar]
- Reichenberg A., Harvey P.D., Bowie C.R., Mojtabai R., Rabinowitz J., Heaton R.K., Bromet E. Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr. Bull. 2009;35(5):1022–1029. doi: 10.1093/schbul/sbn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shad M.U., Tamminga C.A., Cullum M., Haas G.L., Keshavan M.S. Insight and frontal cortical function in schizophrenia: a review. Schizophr. Res. 2006;86(1–3):54–70. doi: 10.1016/j.schres.2006.06.006. [DOI] [PubMed] [Google Scholar]
- Siu C.O., Harvey P.D., Agid O., Waye M., Brambilla C., Choi W.K., Remington G. Insight and subjective measures of quality of life in chronic schizophrenia. Schizophr. Res. Cogn. 2015;2(3):127–132. doi: 10.1016/j.scog.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderstrom N.C., Davalos D.B., Vazquez S.M. Metacognition and depressive realism: evidence for the level-of-depression account. Cogn. Neuropsychiatry. 2011;16(5):461–472. doi: 10.1080/13546805.2011.557921. [DOI] [PubMed] [Google Scholar]
- Stratton J., Yanos P.T., Lysaker P. Insight, neurocognition, and schizophrenia: predictive value of the Wisconsin card sorting test. Schizophr. Res. Treatment. 2013;2013:696125. doi: 10.1155/2013/696125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss M.E., McLouth C.J., Barch D.M., Carter C.S., Gold J.M., Luck S.J., Macdonald A.W., 3rd, Ragland J.D., Ranganath C., Keane B.P., Silverstein S.M. Temporal stability and moderating effects of age and sex on cntracs task performance. Schizophr. Bull. 2013 doi: 10.1093/schbul/sbt089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J., Green M.F., Shaner A., Liberman R.P. Training and quality assurance on the brief psychiatric rating scale: the “drift busters”. Int. J. Methods Psychiatr. Res. 1993;3:221–226. [Google Scholar]
- Ventura J., Lukoff D., Nuechterlein K.H., Liberman R.P., Green M.F., Shaner A. Brief psychiatric rating scale (BPRS) exanded version: scales, anchor points, and administration manual. Int. J. Psychiatr. Methods. 1993;3:227–243. [Google Scholar]
- Wiffen B.D., Rabinowitz J., Fleischhacker W.W., David A.S. Insight: demographic differences and associations with one-year outcome in schizophrenia and schizoaffective disorder. Clin. Schizophr. Relat. Psychoses. 2010;4(3):169–175. [PubMed] [Google Scholar]
- Woodberry K.A., Giuliano A.J., Seidman L.J. Premorbid IQ in schizophrenia: a meta-analytic review. Am. J. Psychiatry. 2008;165(5):579–587. doi: 10.1176/appi.ajp.2008.07081242. [DOI] [PubMed] [Google Scholar]
- Zahn R., Lythe K.E., Gethin J.A., Green S., Deakin J.F., Young A.H., Moll J. The role of self-blame and worthlessness in the psychopathology of major depressive disorder. J. Affect. Disord. 2015;186:337–341. doi: 10.1016/j.jad.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material