Abstract
Steroid hormone receptors including estrogen receptors (ER) classically function as ligand-regulated transcription factors. However, estrogens also elicit cellular effects through binding to extra-nuclear ER (ERα, ERβ, and G protein-coupled ER or GPER) that are coupled to kinases. How extra-nuclear ER actions impact cardiac ischemia-reperfusion (I/R) injury is unknown. We treated ovariectomized wild-type female mice with estradiol (E2) or an estrogen-dendrimer conjugate (EDC), which selectively activates extra-nuclear ER, or vehicle interventions for two weeks. I/R injury was then evaluated in isolated Langendorff perfused hearts. Two weeks of treatment with E2 significantly decreased infarct size and improved post-ischemic contractile function. Similarly, EDC treatment significantly decreased infarct size and increased post-ischemic functional recovery compared to vehicle-treated hearts. EDC also caused an increase in myocardial protein S-nitrosylation, consistent with previous studies showing a role for this post-translational modification in cardioprotection. In further support of a role for S-nitrosylation, inhibition of nitric oxide synthase, but not soluble guanylyl cyclase blocks the EDC mediated protection. The administration of ICI182,780, which is an agonist of G-protein coupled estrogen receptor (GPER) and an antagonist of ERα and ERβ, did not result in protection; however, ICI182,780 significantly blocked EDC-mediated cardioprotection, indicating participation of ERα and/or ERβ. In studies determining the specific ER subtype and cellular target involved, EDC decreased infarct size and improved functional recovery in mice lacking ERα in cardiomyocytes. In contrast, protection was lost in mice deficient in endothelial cell ERα. Thus, extra-nuclear ERα activation in endothelium reduces cardiac I/R injury in mice, and this likely entails increased protein S-nitrosylation. Since EDC does not stimulate uterine growth, in the clinical setting EDC-like compounds may provide myocardial protection without undesired uterotrophic and cancer-promoting effects.
Keywords: cardiomyocyte, endothelium, estrogen receptor, nitric oxide signaling
Introduction
It is well established that pre-menopausal women have reduced incidence of cardiovascular disease (CVD) compared with men, but the incidence of CVD rises following menopause, suggesting a role for sex hormones in the reduction in CVD in pre-menopausal females [1, 2]. However, a large clinical trial, the Women’s Health Initiative (WHI) found that treating post-menopausal women with estrogen or estrogen plus progesterone was not beneficial [3, 4]. A recent update of the WHI examined different age groups and concluded that although conjugated equine estrogens had harmful effects on older women, there were some beneficial effects on myocardial infarction incidence in younger menopausal women [5]. The reasons for the age-dependent effects are unclear, [6, 7] and at least a portion of the current dilemmas regarding the clinical use of estrogen-based therapies resides in insufficient understanding of estrogen actions in the heart. Of note, the identity of the operative estrogen receptor(s) and the signaling mechanisms involved in estrogen-mediated protection against ischemia-reperfusion (I/R) injury are poorly understood. A better understanding of these processes could have important implications on the development of selective estrogen receptor modulators (SERMs) to provide beneficial effects of estrogen without unwanted uterotrophic and cancer-promoting effects [8, 9].
Estrogen signaling is mediated by estrogen binding to estrogen receptors (ER). There are two classic nuclear ER (ERα and ERβ) and a G-protein coupled receptor known as GPR30 or G-protein estrogen receptor (GPER). ERα and ERβ classically bind estrogen and translocate to the nucleus where they modulate transcription. ERα and ERβ also have extra-nuclear actions involving the activation of kinase signaling, leading to acute cellular responses as well as alterations in gene expression that occur via kinase activation [10–15]. On binding estrogen, GPER, localized at the plasma membrane, also activates signaling cascades [16–19].
Although it is well-recognized that estrogens have favorable impact on the severity of cardiac I/R injury, the role of extra-nuclear actions of estrogens and estrogen receptors in this protection is unknown. The goal of the present study was to determine how extra-nuclear estrogen actions impact cardiac I/R injury. This was accomplished using an estrogen-dendrimer conjugate (EDC) comprised of a non-degradable poly(amido)amine dendrimer to which estradiol molecules are linked by a stable covalent bond [20]. Previous studies have shown that EDC is excluded from the nucleus and it stimulates extra-nuclear ER signaling but is ineffective in modulating nuclear ER transcriptional activity, and the selectivity has been demonstrated both in cell culture and in vivo in mice [21]. We found that EDC treatment was as protective as estradiol and it significantly decreased infarct size and increased post-ischemic functional recovery compared to vehicle-treated hearts. We further showed that endothelial ERα, but not cardiomyocyte ERα was required for the protection.
Material and Methods
Animals
All animals were treated and cared for in accordance with the Guide for the Care and Use of Laboratory Animals [National Institutes of Health (NIH), Revised 2011], and protocols were approved by the Institutional Animal Care and Use Committee of the National Heart Lung and Blood Institute. Female C57BL/6J mice, obtained from Jackson Laboratories (Bar Harbor, ME), were bilaterally ovariectomized at 10 weeks of age and delivered to the laboratory at 11 weeks of age. Heterozygous C57BL/6 floxed ERα mice (flox\+) originally generated by S.A. Khan were kindly provided by L. Hahner and D. Clegg [22, 23]. Selective deletion of ERα from cardiac myocytes was accomplished using tamoxifen-inducible α-myosin heavy chain cre-transgenic mice (Mer-Cre-Mer, Jackson Laboratories, Bar Harbor, ME). In another group of mice the receptor was silenced in endothelial cells using vascular endothelial cadherin promoter-driven Cre mice (VECad-Cre) [24].
To generate cardiomyocyte-specific ERα knockout (cs-ERαKO) mice, mice heterozygous for the Exon 3-floxed ERα allele (flox\+) [23] were crossed to obtained homozygous mice for the floxed ERα alleles (flox\flox). Heterozygous flox\+ mice were also crossed with Mer-Cre-Mer mice, and cardiomyocyte-specific ERα knockouts were then generated by crossing cre\+, flox\+ mice with flox\flox mice. The presence of the cre transgene and the modified loxP alleles were verified by PCR of digested genomic DNA. For the cre transgene, the following PCR primers were used: reverse, 5α-AGGTGGACCTGATCATGGAG-3′ and forward, 5′-ATACCGGAGATCATGCAAGC-3′. We also used an internal positive control, performing PCR with the following primers: 5′-CTAGGCCACAGAATTGAAAGATCT-3 (forward) and 5′-GTAGGTGGAAATTCTAGCATCATCC-3 (reverse). The primers used for identifying the presence of the loxP site are as follows: 5′-TGGGTTGCCCGATAACAATAAC -3′ (forward) and 5-AAGAGATGTAGGGCGGGAAAAG-3′ (reverse). The expression of ERα in the hearts of Cre negative control cs-ERαWT mice and Cre positive cs-ERαKO mice was quantified by Western blotting using ERα specific antibody (sc-8005, Santa Cruz).
Mice with endothelial cell-specific deletion of ERα (es-ERαKO) were generated by crossing ERα floxed mice [23] with vascular endothelial cadherin promoter-driven Cre mice (VECad-Cre) [24]. In addition to genotyping done on tail-derived DNA, genotyping was performed on DNA isolated from intact versus endothelium-denuded aorta samples to evaluate effective ERα gene excision in the endothelium.
Minipump agent administration
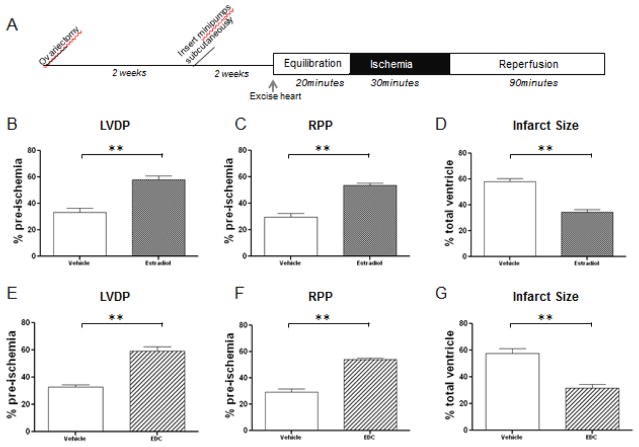
Two weeks after bilateral ovariectomy (OVX), micro-osmotic Alzet pumps (model 1002, DURECT Corporation, Cupertino, California) were implanted subcutaneously into female mice (Figure 1). Mice are anesthetized using 1–3% isoflurane given by inhalation through a vaporizer. Each pump delivered a constant dose (0.25 μl/hr) of vehicle, estradiol, EDC, or dendrimer. Six μg of estradiol or estradiol equivalents (for EDC) were dispensed daily. ICI 182,780 was infused as 2 mg/kg/day [25]. Following two weeks of treatment, hearts were excised for the I/R protocol (Figure 1A).
Figure 1.
Two-week treatment with estrogen and EDC improves functional recovery and infarct size. (A) I/R protocol following subcutaneous Alzet minipumps implantation in C57BL/6J. Mice were bilaterally ovariectomized at 10 weeks of age. After two weeks of recovery from the surgery, minipumps were implanted for drug treatments for two weeks. The hearts were then excised and cannulated to a Langendorff perfusion apparatus. For all the treatment groups, hearts were equilibrated for 20 minutes, subjected to 30 minutes of ischemia and reperfused for 90 minutes. (B–C) Recovery following two weeks of treatment with estradiol. Recoveries of heart functional parameters (LVDP and RPP) post-ischemia after two weeks of estradiol treatment were expressed as percentage of their pre-ischemic values. (D) To determine infarct size, hearts were perfused with 1% 2,3,5-triphenyltetrazoliumchloride (TTC) following reperfusion and ImageJ software was used to analyze the infarct size, which was expressed as the percentage of total area of cross-sectional slices (n=6 for each group, **, p<0.01). (E–F) Recovery following two weeks of treatment with EDC. Recoveries of heart functional parameters (LVDP and RPP) post-ischemia after two weeks of EDC treatment were expressed as percentage of their pre-ischemic values. (G) Infarct size was determined as described above (n=6 for each group, **, p<0.01).
I/R protocol, post-ischemic functional recovery, and infarct size determination
Female mice were anesthetized with sodium pentobarbital (50 mg/kg) and anticoagulated with heparin (1000 USP units/mL), injected directly into the inferior vena cava. Hearts were excised quickly and placed in ice-cold Krebs-Henseleit buffer (in mmol/L: 120 NaCl, 11 D-glucose, 25 NaHCO3, 1.75 CaCl2, 4.7 KCl, 1.2 MgSO4, and 1.2 KH2PO4). The aorta of the heart was then cannulated to a Langendorff perfusion apparatus. Once cannulated, the heart was retrograde perfused with Krebs-Henseleit buffer at a temperature of 37 °C and a constant pressure of 100 cm of water. Krebs-Henseleit buffer was oxygenated with 95% O2/5% CO2 and maintained at pH7.4. For all treatment groups, hearts were equilibrated for 20 minutes, subjected to 30 minutes of ischemia, and reperfused for 90 minutes. L-NAME (10 μM) and ODQ (10 μM) were added to the perfusate 10 minutes prior to ischemia and were present during ischemia and the first 30 minutes of reperfusion. To monitor functional recovery during the I/R protocol, a latex balloon connected to a pressure transducer was inserted into the left ventricle. Left ventricular developed pressure (LVDP) was recorded using a PowerLab system (ADInstruments, Colorado Springs, CO). Rate pressure product (RPP) was determined by multiplying LVDP by heart rate. Recoveries of post-ischemia LVDP and RPP were expressed as a percentage of the pre-ischemic values during equilibration. To determine infarct size, hearts were perfused with 1% 2,3,5-triphenyltetrazolium chloride (TTC) following reperfusion and then incubated in TTC for 30 minutes at 37 °C. Hearts were fixed in 10% formaldehyde, and infarct size was expressed as a percentage of total area of cross-sectional slices.
Identification of protein SNO with 2D CyDye-maleimide DIGE
Hearts were snap frozen in liquid nitrogen after 15 minutes of Langendorff perfusion. Total heart homogenates were then prepared in the dark to prevent the cleavage of S-nitrosothiols, as previously described by Sun et al. [26] Crude heart homogenate was obtained by grinding the heart into powder in liquid nitrogen and homogenizing in 1.5 mL buffer containing in mmol/L: 300 sucrose, 250 HEPES-NaOH pH7.8, 1 EDTA, 0.1 neocuproine, and an EDTA-free protease inhibitor tablet per 10 ml (Roche Diagnostics Corporation, Indianapolis, IN) added just before use. Protein concentrations of the total homogenates were determined using the Bradford assay.
To assess differences in protein fluorescence using two-dimensional DIGE, we used a modified biotin switch protocol [27] with CyDye maleimide mono-reactive sulfhydryl-reactive fluorescent dyes (GE Healthcare Life Sciences, Piscataway, NJ). We used three independent hearts for each group (dendrimer and EDC treated mice). Total heart homogenates (250 μg) were diluted in HEN buffer containing the following in mM: 250 HEPES-NaOH pH7.8, 1 EDTA, 0.1 neocuproine with 2% SDS and an EDTA-free protease inhibitor tablet per 10 ml. Samples were then incubated with 20 mM N-ethyl maleimide (NEM) for 20 minutes at 50°C to block free thiols. Acetone precipitations was used to remove NEM. Then, heart homogenates were resuspended in HEN buffer with 1% SDS, treated with 20 mM Na-ascorbate (Sigma) and finally labeled with CyDye maleimide mono-reactive sulfhydryl-reactive fluorescent dyes [28]. BSA was used as internal control. BSA (200 μg) was treated with GSNO, then equal amounts of GSNO-pretreated BSA were incubated with Na-ascorbate and labeled with each CyDye maleimide mono-reactive sulfhydryl-reactive fluorescent dye. Finally, BSA was added to each sample to standardize quantification of fold changes. Equal amounts of each sample were mixed and subjected to 2D DIGE. Isoelectric point focusing (pI 3 to 10) was completed on an Ettan IPGphor3 (GE Healthcare/Amersham Biosciences) and gel electrophoretic separation via 10–15% gradient SDS-PAGE (Jule, Milford, CT). After the 2D DIGE, each gel was scanned at the unique excitation/emission wave length of each dye using a Typhoon 9400 imager (GE Healthcare Life Sciences) at a resolution of 100 μm with the photomultiplier tube (PMT) for laser scanning of each dye set to obtain equal intensity for GSNO-treated BSA spot. The gels were then poststained overnight with SYPRO Ruby stain and scanned. The SYPRO Ruby staining is used to determine the level of protein associated with the CyDye labeled spots. Images of the same gel were analyzed using Progenesis Discovery Software (Nonlinear Dynamics, Newcastle on Tyne, UK). with intelligent noise correction algorithm. Spots with protein were chosen for identification by mass spectrometry if they showed a >1.5 fold difference in fluorescence intensity between treatment and control with a p-value of <0.05. The Ettan Spot Handling Workstation (GE Healthcare Life 147 Sciences) was used for automated extraction of the selected protein spots followed by in-gel trypsin digestion. After sample extraction from the Spot handling Workstation, each sample was manually desalted using Millipore C18 Ziptips (Millipore, Billerica, MA) following manufacturer’s procedures.
Identification of protein SNO with SNO-resin assisted capture (RAC)
The SNO-RAC protocol was performed as described previously by Kohr et al [29]. All buffers were degassed to prevent oxidation of the resin. Total heart homogenates (1 mg) were diluted in HEN buffer with 2.5% SDS and an EDTA-free protease inhibitor tablet (Roche Diagnostics) and incubated with 50 mM NEM for 20 minutes at 50°C to block free thiol groups. NEM was removed with acetone precipitation for 30 minutes at 4°C. Samples were then resuspended in HEN buffer with 1% SDS (HENS). Thiopropyl sepharose (GE Healthcare, Piscataway, NJ) was rehydrated for 25 minutes in diethyl pyrocarbonate (DEPC) water, and then 25 μL of this slurry was added to a Handee Mini Spin Column (Pierce). The slurry was washed with 5×0.5 ml of DEPC water and 10×0.5 mL of HEN buffer. Samples were added to these columns along with 20 mM Na-ascorbate and rotated for 4 hours at room temperature. Resin-bound proteins were then washed with 8×0.5 mL of HENS buffer and 4×0.5 mL of HENS buffer diluted 1:10. Resin-bound proteins were then subjected to trypsin digestion (Promega, Madion, WI) overnight at 37°C with rotation in buffer containing in mM: 50 NH4HCO3 and 1 EDTA. The following day, samples were washed with 5×0.5 mL of HENS buffer diluted 1:10, 5×0.5 mL of 2 M NaCl, 5×0.5 mL of 80% acetonitrile/0.1% trifuoroacetic acid, and 5×0.5 mL of HEN buffer diluted 1:10. Trypsinized peptides were then eluted for 30 minutes at room temperature in elution buffer containing in mM: 20 DTT, 10 NH4HCO3, and 50% methanol. The resin was then washed with another volume of elution buffer and two volumes of DEPC water, and all fractions were combined and concentrated by SpeedVac (Thermo Fisher Scientific). Finally, samples were resuspended in 0.1% formic acid and cleaned with Millipore C18 Ziptips. (Millipore, Billerica, MA).
LC-MS/MS analysis on LTQ-Orbitrap Elite
Liquid chromatography-tandem mass spectrometry was performed using an Eksigent nanoLC-Ultra 1D plus system (Dublin, CA) coupled to an LTQ Orbitrap Elite mass spectrometer (Thermo Fisher Scientific, San Jose, CA) using CID fragmentation. Peptides were first loaded onto an Zorbax 300SB-C18 trap column (Agilent, Palo Alto, CA) at a flow rate of 6 μL/min for 6 min, and then separated on a reversed-phase PicoFrit analytical column (New Objective, Woburn, MA) using a short 15-min linear gradient of 5–40% acetonitrile in 0.1% formic acid at a flow rate of 250 nL/min. LTQ-Orbitrap Elite settings were as follows: spray voltage 1.5 kV; full MS mass range: m/z 300 to 2000. The LTQ-Orbitrap Elite was operated in a data-dependent mode; i.e., one MS1 high resolution (60,000) scan for precursor ions followed by six data-dependent MS2 scans for precursor ions above a threshold ion count of 500 with collision energy of 35%.
MASCOT database search
The raw file generated from the LTQ Orbitrap Elite was analyzed using Proteome Discoverer v1.3 software (Thermo Fisher Scientific, LLC) using our six-processor Mascot cluster at NIH (v.2.3) search engine. MS peptide tolerance was 20 ppm and MS/MS tolerance was 0.8 Da. The peptide confidence false discovery rate (FDR) was set to 1%. The positive identifications criteria were two or more unique peptides and the correct molecular mass.
Statistical Analysis
Results are expressed as mean ± SEM. Statistical significance was determined by Student t-test for comparison of two groups, by one-way ANOVA followed by a post-hoc Bonferroni test for the ICI182,780, L-NAME, and ODQ treatment studies, and by two-way ANOVA followed by a post-hoc Bonferroni test for the cs-ERα and es-ERα studies.
Results
Estrogen dendrimer conjugate (EDC) reduces ischemia-reperfusion injury
To determine the role of extra-nuclear estrogen receptors in cardioprotection, we compared protection mediated by estradiol with protection afforded by an EDC comprised of estradiol conjugated to a large, positively charged poly(amido)amine dendrimer via stable chemical linkages. Because of its inability to enter the nucleus,[20, 21] EDC selectively activates extra-nuclear ER. We ovariectomized (OVX) female mice and after two weeks we implanted subcutaneous minipumps, which delivered estradiol (6 μg of estradiol equivalents daily), vehicle, EDC (6 μg estradiol equivalents daily), or dendrimer for two weeks. Subsequently the heart was removed, perfused in Langendorff mode and subjected to I/R injury (Figure 1A). Hemodynamic parameters for the groups are shown in Table 1A. As shown in Figure 1B and 1C, after 30 minutes of ischemia and 90 minutes of reperfusion, hearts from estradiol-treated mice showed significantly greater post-ischemia recovery of left ventricular developed pressure and rate pressure product compared to pre-ischemic values. In addition, there was a significant decrease in infarct size with estradiol treatment (Figure 1D). Hearts from EDC-treated mice also showed an improvement in recovery of LVDP and RPP as compared with hearts from control dendrimer-treated mice (Figure 1E, 1F), and EDC treatment also decreased infarct size (Figure 1G). These results demonstrate that EDC afforded equal reduction in I/R injury compared to that seen with estradiol, indicating that the selective activation of extra-nuclear ER is sufficient to provide cardioprotection.
Table 1A.
Hemodynamic parameters wild type hearts
| Heart samples | Pre-ischemic equilibration | Post-ischemic reperfusion | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| (n) | Body weight (g) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | |
| Control | 6 | 21.7±1.0 | 2.2±0.1 | 364±14 | 114±4 | 1.8±0.1 | 325±19 | 38±4 |
| Estradiol | 6 | 22.8±0.3 | 2.4±0.2 | 381±24 | 124±8 | 1.9±0.2 | 353±19 | 71±3* |
| Dendrimer | 6 | 21.5±0.5 | 2.1±0.1 | 359±19 | 111±3 | 1.7±0.1 | 321±14 | 37±3 |
| EDC | 6 | 22.1±0.4 | 2.1±0.1 | 377±11 | 113±3 | 1.8±0.2 | 347±14 | 67±3* |
Values are mean ± SE; (n), number of hearts; FR, flow rate (ml/min); HR, heart rate (beats per min, bpm); LVDP, left ventricular developed pressure.
p<0.05, vs control or dendrimer.
EDC-related cardioprotection involves nitric oxide (NO) but not soluble guanylyl cyclase (sGC)
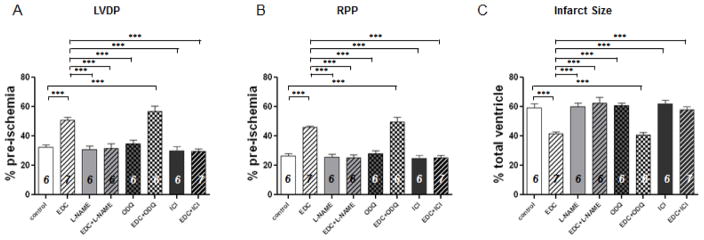
Because protection from cardiac I/R injury in females compared with males has been shown to be negated by L-NAME, an inhibitor of nitric oxide synthase (NOS),[30] we tested whether L-NAME alters the protection provided by activation with EDC. Female mice underwent bilateral OVX and treatment with EDC or dendrimer via minipumps for 2 weeks followed by assessment of I/R injury via the Langendorff perfusion in the absence and presence of L-NAME in the perfusate. Hemodynamic parameters are shown in Table 1B. As shown in Figure 2A–2C, post-ischemic contractile dysfunction was improved and infarct size was reduced following treatment with EDC, and this protection was blocked by the addition of L-NAME. We further tested whether NO activation of sGC was involved in the protection by pretreating the hearts with ODQ, an inhibitor of sGC. As shown in Figure 2A–2C, ODQ did not block the protection afforded by EDC. These cumulative results indicate that NO plays a key role in the cardioprotection provided by EDC, yet the activation of sGC is not necessary for the protection. The latter finding is consistent with the lack of a role for sGC in pre- and post-conditioning [31, 32].
Table 1B.
Hemodynamic parameters ICI182,780, L-NAME, and ODQ treatment
| Heart samples | Pre-ischemic equilibration | Post-ischemic reperfusion | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| (n) | Body weight (g) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | |
| Dendrimer | 6 | 23.5±0.4 | 2.4±0.1 | 399±25 | 121±5 | 1.8±0.1 | 319±17 | 39±3# |
| EDC | 7 | 24.0±1.1 | 2.3±0.1 | 366±11 | 121±7 | 1.8±0.1 | 337±12 | 61±3* |
| L-NAME | 6 | 25.8±0.5 | 2.2±0.1 | 359±11 | 124±10 | 1.6±0.1 | 299±9 | 38±3# |
| EDC + L-NAME | 6 | 26.0±0.8 | 2.1±0.1 | 364±16 | 141±8 | 1.5±0.1 | 291±14 | 44±4# |
| ODQ | 6 | 24.8±0.5 | 2.2±0.1 | 351±14 | 138±8 | 1.7±0.1 | 293±7 | 48±4# |
| ODQ + EDC | 6 | 24.6±0.5 | 2.2±0.1 | 383±9 | 141±5 | 1.7±0.1 | 334±13 | 77±5*,& |
| ICI182,780 | 6 | 25.0±1.0 | 2.3±0.1 | 392±18 | 144±4 | 1.8±0.1 | 328±16 | 43±4# |
| EDC + ICI182,780 | 7 | 23.8±0.5 | 2.2±0.1 | 402±10 | 142±6 | 1.7±0.1 | 347±17 | 42±3# |
Values are mean ± SE; (n), number of hearts; FR, flow rate (ml/min); HR, heart rate (beats per min, bpm); LVDP, left ventricular developed pressure.
p<0.05, vs dendrimer;
p<0.05 vs EDC;
p<0.05 vs ODQ.
Figure 2. Pharmacological inhibition of nitric oxide synthase or ERα/ERβ blocks the improved functional recovery by EDC treatment in ovariectomized wild type mice.
(A–B) Post-ischemic recoveries of heart functional parameters (LVDP and RPP) in ovariectomized mice treated with L-NAME (a selective inhibitor of nitric oxide synthase), ODQ (an inhibitor of soluble guanylyl cyclase) or ICI182,780 (a selective inhibitor of ERα and ERβ and an activator of GPER were expressed as percentage of their pre-ischemic values. (C) Infarct size was determines as described in Figure 1D. Numbers inside each bar represent the number of mice used for each group, ***, p<0.0001.
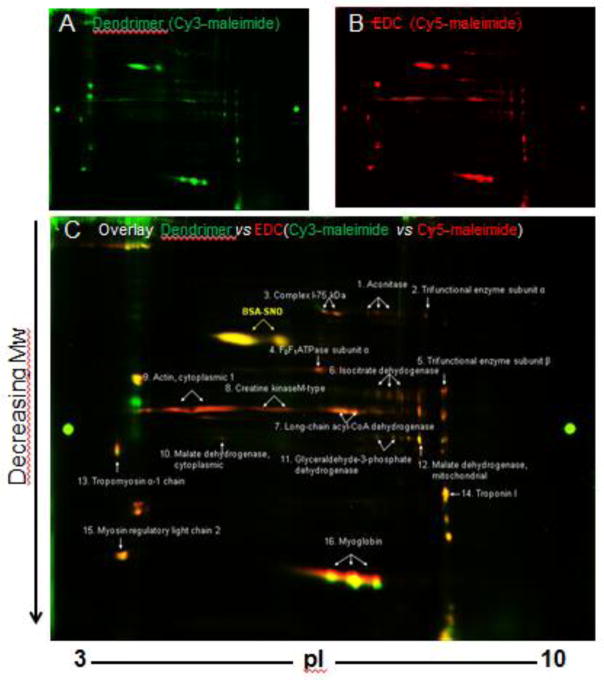
Having determined that EDC-mediated cardiac protection is dependent on NO but independent of sGC activation, we examined whether two weeks of EDC administration alters protein SNO in the heart. After EDC and dendrimer treatment, protein SNO was measured in total heart homogenates by a modified biotin switch method based on CyDye-maleimide mono-reactive fluorescence dyes and 2D DIGE proteomics analysis. Figure 3 shows representative images of SNO in dendrimer control- (Figure 3A) and EDC-treated hearts (Figure 3B): S-nitrosylated proteins in the dendrimer group are labeled by Cy3-malemide (green) and S-nitrosylated proteins in the EDC group are labeled with Cy5-maleimide (red). In the overlay (Figure 3C), a red spot indicates an increased levels of protein SNO in EDC-treated samples and a green spot indicates an increased levels of protein SNO in dendrimer-treated versus EDC-treated samples, which corresponds with a relative decrease in the abundance of protein SNO with EDC administration. The data in the gels were analyzed using Progenesis software and proteins that showed a significant increase in SNO in EDC-treated mice as compared to the dendrimer samples (greater than a 1.5 fold change) were extracted and identified by mass spectrometry. Sixteen proteins (Table 2) showed a significant increase in protein SNO following EDC treatment compared to dendrimer control treatment. To confirm that EDC treatment leads to an increase in SNO, we also performed SNO-RAC studies. As shown in Supplemental Online Tables 1 and 2, with SNO-RAC we found that EDC leads to an increase in SNO as assessed by SNO-RAC as 66 of the 96 peptides identified showed an increase with EDC treatment.
Figure 3.
Two-week EDC treatment leads to protein S-nitrosation changes identified by 2D CyDye-maleimide DIGE. Representative 2D CyDye-maleimide DIGE gel electrophoresis from three independent experiments. (A) Dendrimer treated group were labeled with Cy3-malemide (green) and (B) EDC treated group with Cy5-maleimide (red). (C) Overlay of S-nitrosation in EDC or vehicle treated heart.
Table 2.
Increased SNO proteins in EDC-treated ovariectomized hearts by 2D CyDye-maleimide DIGE
| Spots # | Protein Name | Protein ID | Score | Coverage | Unique peptides | #PSM | Mw (KDa) | Cal. pI | SNO level (EDC vs Vehicle) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Aconitase | Q99KI0 | 4001.3 | 36.4 | 26 | 185 | 85.4 | 7.93 | 2.6 ± 0.5 |
| 2 | Trifunctional enzyme subunit α | Q8BMS1 | 17735.8 | 37.2 | 35 | 606 | 82.6 | 9.14 | 2.9 ± 0.6 |
| 3 | Complex I-75 kDa subunit | Q91VD9 | 914.9 | 22.4 | 17 | 48 | 79.7 | 5.72 | 1.9 ± 0.4 |
| 4 | F0F1 ATPase subunit α | Q03265 | 4805.4 | 34.0 | 23 | 197 | 59.7 | 9.19 | 2.7 ± 0.7 |
| 5 | Trifunctional enzyme subunit β | Q99JY0 | 6171.2 | 42.5 | 33 | 269 | 51.4 | 9.38 | 3.0 ± 0.9 |
| 6 | Isocitrate dehydrogenase [NADP], mitochondrial | P54071 | 5577.3 | 35.0 | 17 | 208 | 50.9 | 8.69 | 2.0 ± 0.4 |
| 7 | Long-chain specific acyl-CoA dehydrogenase | P51174 | 12935.2 | 38.1 | 16 | 368 | 47.9 | 8.31 | 1.8 ± 0.3 |
| 8 | Creatine kinase M- type | P07310 | 3746.1 | 38.3 | 18 | 170 | 43.0 | 7.06 | 2.5 ± 0.6 |
| 9 | Actin, cytoplasmic 1 | P60710 | 6797.4 | 28.8 | 13 | 252 | 41.7 | 5.48 | 2.7 ± 0.4 |
| 10 | Malate dehydrogenase, cytoplasmic | P14152 | 1728.2 | 29.9 | 10 | 122 | 36.5 | 6.58 | 3.1 ± 0.9 |
| 11 | Glyceraldehyde-3- phosphate dehydrogenase | P16858 | 4175.6 | 28.2 | 10 | 126 | 35.8 | 8.25 | 1.6 ± 0.2 |
| 12 | Malate dehydrogenase, mitochondrial | P08249 | 2069.1 | 42.0 | 14 | 84 | 35.6 | 8.68 | 1.5 ± 0.1 |
| 13 | Tropomyosin α-1 chain | P58771 | 6608.5 | 62.7 | 18 | 258 | 32.7 | 4.74 | 1.9 ± 0.3 |
| 14 | Troponin I, cardiac muscle | P48787 | 7350.7 | 55.0 | 20 | 312 | 24.2 | 9.55 | 1.6 ± 0.3 |
| 15 | Myosin regulatory light chain 2, cardiac isoform | P51667 | 3353.0 | 52.4 | 11 | 185 | 22.4 | 5.10 | 1.7 ± 0.3 |
| 16 | Myoglobin | P04247 | 4315.6 | 57.1 | 13 | 122 | 17.1 | 7.62 | 1.7 ± 0.2 |
Note: Positive identifications from three independent experiments consisted of two peptides or more with the highest MS/MS score and a correct molecular mass position.
ERα/β, not GPER mediate the cardioprotection
To distinguish whether GPER or one of the classical ER is responsible for the cardioprotection provided by EDC, we performed studies with ICI182,780, a selective inhibitor of both ERα and ERβ and an activator of GPER [33–35]. Female mice underwent bilateral OVX and ICI182,780 (2 mg/kg/day) [25] was administered with and without EDC via minipumps for 2 weeks followed by assessment of I/R injury via the Langendorff model. As shown in Figure 2A–2C, ICI182,780 alone did not affect LVDP, RPP or infarct size. Alternatively, the protection of both function and infarct size reduction afforded by EDC was blocked by concurrent administration of ICI182,780. These results reveal that GPER does not mediate EDC-related cardioprotection, and that instead ERα and/or ER are involved.
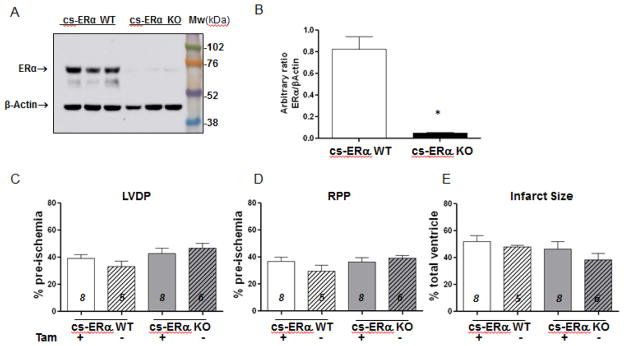
EDC-related cardioprotection is not mediated by cardiac ERα
A recent study, which reported the presence of ERα and a lack of ERβ expression in cardiomyocytes [36] prompted us to initially focus on ERα. This was accomplished by generating a tamoxifen-inducible cardiomyocyte-specific ERα knock out mouse (cs-ERαKO), as detailed in the Material and Method section. In addition to genotyping the mice by PCR, we confirmed the deletion of ERα by Western blotting of total heart homogenate using an anti-ERα antibody (Figure 4A and 4B). Five days of tamoxifen intraperitoneal injections (20 mg/kg) effectively reduced ERα protein expression in the hearts of cs-ERαKO mice (Figure 4A and 4B).
Figure 4. Cardiomyocyte-specific ERα knock-out mice generation.
(A) Anti-ERα Western Blot. Three samples for each group, cs-ERα WT and KO mouse heart total homogenates were loaded in the same gel and were probed with anti-ERα antibody. The amount of protein per well was checked by probing the membrane with anti-β-actin antibody. (B) Densitometry analysis show the ratio between the densitometric values of the ERα bands and those bands detected with the anti-β-actin antibody. (C–D) Post-ischemic recoveries of heart functional parameters (LVDP and RPP) in ovariectomized cs-ERα WT and KO mice treated with tamoxifen (Tam) for five days were expressed as percentage of their pre-ischemic values. (E) Infarct size was determined as described in Figure 1D. Numbers inside each bar represent the number of mice used for each group, *, p=0.0023.
Before comparing findings in the mice expressing versus lacking ERα in cardiomyocytes (cs-ERαWT and cs-ERαKO, respectively), we first investigated whether tamoxifen treatment affects cardiac function or infarct severity in our model. After ovariectomy, Cre positive (cs-ERαKO) and Cre negative control floxed mice (cs-ERαWT) were treated for five days with 20 mg/kg tamoxifen (by intraperitoneal injection). After two weeks the heart was removed and I/R injury was assessed. We found no changes in cardiac function or infarct size following I/R injury with the administration of tamoxifen (Figure 4C), demonstrating that the treatment is not affecting cardiac function in our model. Hemodynamic parameters are provided in Table 1C.
Table 1C.
Hemodynamic parameters following tamoxifen treatment
| Heart samples | Pre-ischemic equilibration | Post-ischemic reperfusion | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| (n) | Body weight (g) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | |
| cs-ERαWT +Tam | 8 | 24±1 | 2.1±0.2 | 352±22 | 140±6 | 2.0±0.4 | 322±17 | 56±6 |
| cs-ERαWT | 5 | 26±2 | 2.5±0.2 | 366±20 | 142±10 | 1.7±0.1 | 326±21 | 46±5 |
| cs-ERαKO +Tam | 8 | 24±1 | 2.6±0.2 | 395±10 | 144±7 | 1.8±0.1 | 337±13 | 62±7 |
| cs-ERαKO | 6 | 23±1 | 2.7±0.3 | 352±19 | 131±8 | 1.8±0.1 | 317±30 | 61±6 |
Values are mean ± SE; (n), number of hearts; FR, flow rate (ml/min); HR, heart rate (beats per min, bpm); LVDP, left ventricular developed pressure.
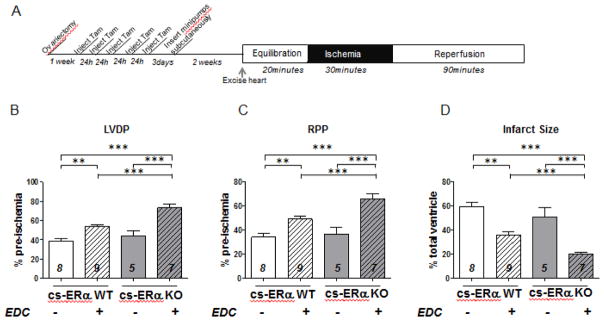
We then employed these mice to interrogate the role of cardiomyocyte ERα in EDC-related cardioprotection. Cre positive (cs-ERαKO) and Cre negative floxed control mice (cs-ERαWT) were ovariectomized at 10 weeks of age. After a week of recovery, the animals were injected with tamoxifen every 24 hours for 5 days. Minipumps were then inserted subcutaneously for 2 weeks of treatment with EDC or dendrimer as a control (Figure 5A). Hemodynamic parameters are given in Table 1D. As expected, in OVX Cre negative (cs-ERαWT) mice, EDC treatment improved cardiac function and decreased infarct size after 30 min of ischemia and 90 min of reperfusion (Figure 5B–5D). In Cre positive (cs-ERαKO) mice EDC was also protective compared to dendrimer control, suggesting that cardiomyocyte ERα is not required for EDC-mediated protection. Interestingly, we found that the protection afforded by EDC treatment was actually greater in OVX Cre positive cs-ERαKO mice than in OVX Cre negative control cs-ERα WT mice, suggesting the loss of cardiomyocyte ERα might enhance the cardioprotection provided by extra-nuclear ER activation.
Figure 5.
Treatment for two weeks with EDC improves functional recovery and infarct size in cardiomyocyte-specific ERα knock out mice. (A) I/R protocol following subcutaneous Alzet minipumps implantation in cs-ERα KO and WT mice. Mice were bilaterally ovariectomized at 10 weeks of age. After 1 week of recovery from the ovariectomy surgery, tamoxifen was injected intraperitoneally daily for five days, and after two days minipumps were implanted for drug treatments for two weeks. (B–C) Post-ischemic recoveries of heart functional parameters (LVDP and RPP) after two weeks of EDC or dendrimer vehicle treatment were expressed as percentage of their pre-ischemic values. (D) Infarct size was determined as described in Figure 1D. Numbers inside each bar represent the number of mice used for each group, **, p<0.001; ***p<0.0001.
Table 1D.
Hemodynamic parameters EDC treatment in csERagr;-WT and cs-ERα-KO
| Heart samples | Pre-ischemic equilibration | Post-ischemic/End of reperfusion | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| (n) | Body weight (g) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | |
| cs-ERαWT | 8 | 24±1 | 2.4±0.3 | 376±25 | 144±11 | 1.7±0.1 | 328±17 | 57±6# |
| cs-ERαWT + EDC | 9 | 23±1 | 2.9±0.3 | 377±17 | 143±6 | 1.9±0.1 | 339±9 | 77±4 |
| cs-ERαKO | 5 | 21±1 | 2.5±0.2 | 388±23 | 148±10 | 1.8±0.1 | 325±20 | 67±9# |
| cs-ERαKO + EDC | 7 | 22±1 | 2.8±0.3 | 375±24 | 135±9 | 1.8±0.1 | 336±20 | 98±7 |
Values are mean ± SE; (n), number of hearts; FR, flow rate (ml/min); HR, heart rate (beats per min, bpm); LVDP, left ventricular developed pressure.
p<0.05 vs the same genotype + EDC.
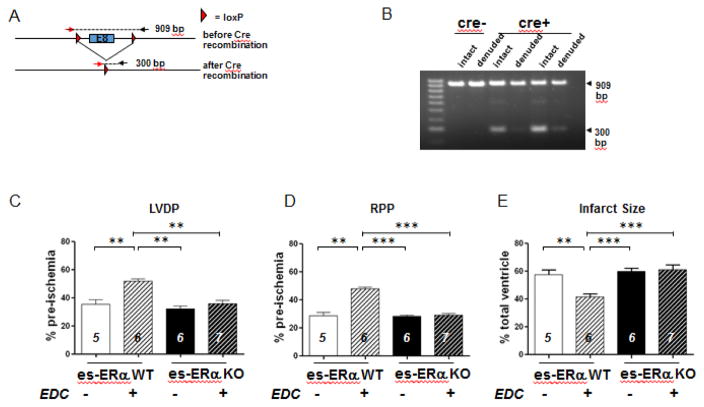
EDC mediated protection is lost in endothelial specific ERα knockout mice
Recognizing that the EDC-related cardioprotection is NO-dependent, and knowing that the activation of non-nuclear ERα in endothelium stimulates the production of NO by eNOS, [21] we next investigated the potential role of endothelial ERα in EDC-related cardioprotection. Endothelial cell-specific ERα knock out mice (es-ERαKO) were generated, and the selective loss of the receptor in endothelium was confirmed (Figure 6A–6B). Endothelial cell Cre positive (es-ERαKO) and Cre negative control floxed mice (es-ERαWT) were ovariectomized at 10 weeks of age, and after a week of recovery, minipumps were inserted subcutaneously for 2 weeks of treatment with EDC or dendrimer as a vehicle control. Hemodynamic parameters are given in Table 1E. Predictably EDC treatment in OVX Cre negative es-ERαWT mice improved cardiac function and decreased myocardial injury after 30 min of ischemia and 90 min of reperfusion (Figure 6C–6E). However, EDC-related protection in both cardiac contractility and infarct size was blocked in Cre positive (es-ERαKO) mice lacking endothelial cell ERα. These findings indicate that ERα in endothelium is required for EDC-mediated protection of the myocardium. As EDC treatment leads to an increase in SNO (see Figure 3), we tested whether the EDC-induced increase in SNO is mediated by es-ERα. As shown in online supplemental Figure 1, the increase in SNO observed with EDC treatment in es-ERαWT was largely ablated in es-ERαKO hearts.
Figure 6. EDC mediated protection is blocked in mice with endothelial specific loss of ERα.
Characterization of ERα expression in ERαfl/fl;VECad-Cre mice. (A–B) To evaluate effective gene excision in the endothelium, genotyping was performed on DNA isolated from intact versus endothelium-denuded aorta samples from ERαfl/fl and ERαfl/fl;VECad-Cre mice. PCR with a single primer set yielded products that were 909 bp versus 300 bp in size before versus after Cre-mediated recombination, respectively. Whereas samples from either intact or endothelium-denuded ERαfl/fl mice yielded only a 909 bp product (Lanes 1,2), samples from ERαfl/fl;VECad-Cre mice yielded both 909 bp and 300 bp products, with far less 300 bp product following endothelial denudation. (C–D) Endothelial specific ERα-KO mice were bilaterally ovariectomized at 10 weeks of age. After 1 week of recovery minipumps were implanted for drug treatments for two weeks. Post-ischemic recoveries of heart functional parameters (LVDP and RPP) after two weeks of EDC or dendrimer vehicle treatment were expressed as percentage of their pre-ischemic values. (E) Infarct size was determined as described in Figure 1D. Numbers inside each bar represent the number of mice used for each group, **, p<0.001; ***p<0.0001.
Table 1E.
Hemodynamic parameters EDC treatment in esERα-WT and -KO
| Heart samples | Pre-ischemic equilibration | Post-ischemic/End of reperfusion | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| (n) | Body weight (g) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | FR (ml/min) | HR (bpm) | LVDP (cmH2O) | |
| es-ERαWT | 5 | 23±0.3 | 2.2±0.1 | 365±5.3 | 138±3 | 1.7±0.1 | 294±9 | 49±4# |
| es-ERαWT + EDC | 6 | 22±0.5 | 2.2±0.1 | 355±17 | 121±9 | 1.6±0.01 | 329±21 | 62±4 |
| es-ERαKO | 6 | 23±0.8 | 2.0±0.1 | 344±16 | 129±8 | 1.6±0.1 | 302±6 | 41±2 |
| es-ERαKO + EDC | 7 | 23±0.5 | 2.1±0.1 | 375±11 | 125±7 | 1.6±0.1 | 304±13 | 47±4 |
Values are mean ± SE; (n), number of hearts; FR, flow rate (ml/min); HR, heart rate (beats per min, bpm); LVDP, left ventricular developed pressure.
p<0.05 vs the same genotype + EDC.
Discussion
Seeking to better understand the basis of estrogen-mediated protection against cardiac I/R injury, the present work demonstrates that 2 weeks of treatment of OVX mice with EDC reduces infarct size and post-ischemic functional impairment in mice. The extent of protection afforded by EDC mirrors that obtained with equimolar estradiol treatment. We also demonstrate that treatment with EDC leads to an increase in NO/SNO signaling in the heart, as indicated by an increase in SNO levels of cardiac specific proteins in the EDC-treated hearts. Many of the cardiac proteins displaying increased SNO following EDC treatment are similar to those that we previously found to be S-nitrosated in female hearts and with cardioprotection [37–39]. These included aconitase, the 75 KDa subunit of mitochondrial Complex I, the α-subunit of mitochondrial FoF1-ATPase, creatine kinase, and malate dehydrogenase. We and other have previously shown that SNO of key proteins before and during ischemia, such as FoF1-ATPase and Complex I, can play an important role in cardioprotection [26, 40]. We previously measured the occupancy of SNO in cardioprotection and showed that for many of these proteins SNO occupancy was in an appropriate range, especially given the labile nature of SNO. The inhibition of EDC-related protection with L-NAME together with the maintenance of protection despite sGC inhibition, indicate that NO/SNO-dependent mechanisms underlie the reduction in infarct size in heart.
We further investigated which ER mediates the cardioprotection provided by EDC. The administration of ICI182,780, which is a GPER agonist and an ERα and ERβ antagonist, did not affect cardiac function or infarct size, indicating that GPER is not likely participating in the beneficial impact of EDC. However, the EDC-related reduction in infarct size and in cardiac functional impairment was ablated if the mice were treated with ICI182,780, indicating participation of ERα or ERβ. This finding is consistent with the prior observation in rabbits that ICI182,780 attenuates the cardioprotection provided by estradiol [41]. ICI182,780, which is also known as Fulvestrant, is used in the treatment of hormone receptor-positive breast cancer [42–44]. The observed loss of protection with the addition of Fulvestrant may have implications for cardioprotection in women treated with the agent.
Having observed an increase in cardiomyocyte SNO with EDC and a reversal of the beneficial actions of EDC with ICI182,780, the role of cardiomyocyte ERα was determined. Using mice with global deletion of ERα (ERα-Neo-KO) [45] we previously reported that global deletion of ERα did not block I/R injury that was observed in females [46]. However, the ERα-Neo-KO mouse encodes ER splice variants, and it was reported that the estradiol mediated increase in NO production in the endothelial cells was maintained in the ERα-Neo-KO, but not in the ERα-Δ2-KO which has complete loss of ERα [47]. Because cardioprotection in females is dependent on NO signaling, we therefore reconsidered the role of ERα in cardioprotection. The recent report that ERα but not ERβ is abundantly expressed in cardiomyocytes, [36] further supported studying the role of cardiomyocyte ERα. The cardioprotective effects of EDC were not attenuated by selective deletion of cardiomyocyte ERα. This finding is consistent with a recent study of isolated cardiomyocytes reporting that in those cells ERα is primarily localized in the nucleus and not capable of activating MAPK kinase or PI3 kinase-related signaling [36]. Surprisingly, we observed that cardiomyocyte-specific loss of ERα resulted in enhanced cardioprotection by EDC. The finding suggests that cardiomyocyte ERα activation by EDC might be detrimental.
Because EDC-related cardioprotection is NO-dependent, and non-nuclear ERα activation in endothelium stimulates eNOS to generate NO, [21] we investigated the role of endothelia ERα in cardioprotection. We found that EDC-related cardioprotection is absent in mice lacking endothelial ERα, which is consistent with previous studies showing that endothelial ERα is needed for estradiol protection against I/R injury [48]. In contrast to prior work, the present studies demonstrate the critical involvement of extra-nuclear processes mediated by ERα in endothelium for the first time. The present study further shows that the protection afforded by es-ERα results in an increase in SNO in the heart. In prior investigations the global deletion or inhibition of ERβ prevented estradiol-induced cardioprotection, [37, 46, 49–51], suggesting an additional requirement for ERβ in the cardioprotection. However, the earlier findings with ERβ loss-of-function are potentially explained by a decrease in ERα in the endothelium because it has been previously shown that ERβ promotes endothelial cell ERα expression [52]. Although these data clearly demonstrate an important role for endothelial ERα, they do not exclude a potential role for ERβ, as previous studies have suggested a role for ER [51]. In addition, we cannot exclude the possibility that loss of endothelial ERα affects the biopermeability and biodistribution of EDC, for example if ERα participates in transcytosis or elimination of EDC.
From a clinical perspective, it is worthwhile noting that EDC and related molecules with selective action on non-nuclear ER may have therapeutic advantages over estradiol or other forms of estrogens. Whereas the latter agents impact the reproductive tract and promote estrogen-response cancer cell growth, the former do not [21, 53]. Interestingly, the non-nuclear receptor selectivity of EDC is related to the physical exclusion of the nanoparticle from the nucleus, [20] and the selectivity of pathway preferential estrogens is likely due to their low binding affinity for ERs [53]. As such, there are options for ligand characteristics that can be modified to preferentially activate non-nuclear versus nuclear ER, and now we know that the former mechanism of action is entirely sufficient to afford myocardial protection.
In summary, the present findings reveal that extra-nuclear ER activation initiated by EDC treatment leads to a reduction in infarct size and improved cardiac function following I/R. We also demonstrate that EDC treatment leads to an increase in the SNO of cardiac proteins that have previously been found to undergo SNO in other models of cardioprotection. Furthermore, we show that the cardioprotection afforded by EDC is not mediated by cardiomyocyte ERα, and that instead it occurs through endothelial cell ERα activation. These observations provide important new mechanistic insights into estrogen-related cardioprotection. These data suggest that EDC or similar selective estrogen receptor modulators (SERMs) can provide beneficial effects on the cardiovascular system without detrimental effects such as proliferation of the breast and uterus, or of cancer cells in these tissues. EDC does not promote uterine or breast cancer growth; however, we cannot exclude the possibility that EDC could also reduce cell death pathways in cancer cells analogous to its activation of cardioprotective pathways in heart. These data, suggest that compounds which selectively activate plasma membrane ER signaling could be developed as therapeutic agents [21].
Supplementary Material
Hightlights.
Non-nuclear estrogen receptor activation with EDC reduces ischemia-reperfusion injury
EDC mediated protection does not depend on cardiac estrogen receptor-alpha
EDC mediated protection requires endothelial estrogen receptor-alpha
EDC mediated protection increases S-nitrosylation of cardiac proteins
Acknowledgments
Sources of Funding
This work was supported by National Heart Lung and Blood Institutes Intramural funds (EM) and by grants from the National Institutes of Health (R01 HL087564 to PWS, R01 DK015556 to JAK and PWS, and P50 AT006268 to BSK).
We thank the NHLBI/NIH Animal Surgery and Resources Core for their assistance.
Non-standard Abbreviations and Acronyms
- CVD
Cardiovascular disease
- EDC
Estradiol-dendrimer conjugate
- eNOS
Endothelial nitric oxide synthase
- ER
Estrogen receptor
- GPER
G protein-coupled estrogen receptor
- GPR30
Orphan G-protein coupled receptor
- I/R
Ischemia/Reperfusion
- LVDP
Left ventricular developed pressure
- OVX
Ovariectomy
- RPP
Rate pressure product
- SERMs
selective estrogen receptor modulators
- SNO
S-nitrosylation
- TTC
2,3,5-triphenyltetrazolium chloride
- WHI
Women’s Health Initiative
Footnotes
Conflict of Interest: None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science. 2005;308:1583–7. doi: 10.1126/science.1112062. [DOI] [PubMed] [Google Scholar]
- 2.Barrett-Connor E, Bush TL. Estrogen and coronary heart disease in women. Jama. 1991;265:1861–7. [PubMed] [Google Scholar]
- 3.Hodis HN, Mack WJ, Azen SP, Lobo RA, Shoupe D, Mahrer PR, et al. Hormone therapy and the progression of coronary-artery atherosclerosis in postmenopausal women. The New England journal of medicine. 2003;349:535–45. doi: 10.1056/NEJMoa030830. [DOI] [PubMed] [Google Scholar]
- 4.Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II) Jama. 2002;288:49–57. doi: 10.1001/jama.288.1.49. [DOI] [PubMed] [Google Scholar]
- 5.Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310:1353–68. doi: 10.1001/jama.2013.278040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurney EP, Nachtigall MJ, Nachtigall LE, Naftolin F. The Women’s Health Initiative trial and related studies: 10 years later: a clinician’s view. The Journal of steroid biochemistry and molecular biology. 2014;142:4–11. doi: 10.1016/j.jsbmb.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Lobo RA. Where are we 10 years after the Women’s Health Initiative? The Journal of clinical endocrinology and metabolism. 2013;98:1771–80. doi: 10.1210/jc.2012-4070. [DOI] [PubMed] [Google Scholar]
- 8.Conner P. Breast response to menopausal hormone therapy--aspects on proliferation, apoptosis and mammographic density. Ann Med. 2007;39:28–41. doi: 10.1080/07853890601039842. [DOI] [PubMed] [Google Scholar]
- 9.Grady D, Gebretsadik T, Kerlikowske K, Ernster V, Petitti D. Hormone replacement therapy and endometrial cancer risk: a meta-analysis. Obstetrics and gynecology. 1995;85:304–13. doi: 10.1016/0029-7844(94)00383-O. [DOI] [PubMed] [Google Scholar]
- 10.Meyer MR, Haas E, Barton M. Gender differences of cardiovascular disease: new perspectives for estrogen receptor signaling. Hypertension. 2006;47:1019–26. doi: 10.1161/01.HYP.0000223064.62762.0b. [DOI] [PubMed] [Google Scholar]
- 11.Murphy E. Estrogen signaling and cardiovascular disease. Circulation research. 2011;109:687–96. doi: 10.1161/CIRCRESAHA.110.236687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madak-Erdogan Z, Kieser KJ, Kim SH, Komm B, Katzenellenbogen JA, Katzenellenbogen BS. Nuclear and extranuclear pathway inputs in the regulation of global gene expression by estrogen receptors. Molecular endocrinology. 2008;22:2116–27. doi: 10.1210/me.2008-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menazza S, Murphy E. The Expanding Complexity of Estrogen Receptor Signaling in the Cardiovascular System. Circulation research. 2016;118:994–1007. doi: 10.1161/CIRCRESAHA.115.305376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Q, Chambliss K, Umetani M, Mineo C, Shaul PW. Non-nuclear estrogen receptor signaling in the endothelium. The Journal of biological chemistry. 2011;286:14737–43. doi: 10.1074/jbc.R110.191791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chambliss KL, Yuhanna IS, Anderson RG, Mendelsohn ME, Shaul PW. ERbeta has nongenomic action in caveolae. Molecular endocrinology. 2002;16:938–46. doi: 10.1210/mend.16.5.0827. [DOI] [PubMed] [Google Scholar]
- 16.Revankar CM, Cimino DF, Sklar LA, Arterburn JB, Prossnitz ER. A transmembrane intracellular estrogen receptor mediates rapid cell signaling. Science. 2005;307:1625–30. doi: 10.1126/science.1106943. [DOI] [PubMed] [Google Scholar]
- 17.Filardo EJ, Quinn JA, Bland KI, Frackelton AR., Jr Estrogen-induced activation of Erk-1 and Erk-2 requires the G protein-coupled receptor homolog, GPR30, and occurs via trans-activation of the epidermal growth factor receptor through release of HB-EGF. Molecular endocrinology. 2000;14:1649–60. doi: 10.1210/mend.14.10.0532. [DOI] [PubMed] [Google Scholar]
- 18.Haas E, Meyer MR, Schurr U, Bhattacharya I, Minotti R, Nguyen HH, et al. Differential effects of 17beta-estradiol on function and expression of estrogen receptor alpha, estrogen receptor beta, and GPR30 in arteries and veins of patients with atherosclerosis. Hypertension. 2007;49:1358–63. doi: 10.1161/HYPERTENSIONAHA.107.089995. [DOI] [PubMed] [Google Scholar]
- 19.Funakoshi T, Yanai A, Shinoda K, Kawano MM, Mizukami Y. G protein-coupled receptor 30 is an estrogen receptor in the plasma membrane. Biochemical and biophysical research communications. 2006;346:904–10. doi: 10.1016/j.bbrc.2006.05.191. [DOI] [PubMed] [Google Scholar]
- 20.Harrington WR, Kim SH, Funk CC, Madak-Erdogan Z, Schiff R, Katzenellenbogen JA, et al. Estrogen dendrimer conjugates that preferentially activate extranuclear, nongenomic versus genomic pathways of estrogen action. Molecular endocrinology. 2006;20:491–502. doi: 10.1210/me.2005-0186. [DOI] [PubMed] [Google Scholar]
- 21.Chambliss KL, Wu Q, Oltmann S, Konaniah ES, Umetani M, Korach KS, et al. Non-nuclear estrogen receptor alpha signaling promotes cardiovascular protection but not uterine or breast cancer growth in mice. The Journal of clinical investigation. 2010;120:2319–30. doi: 10.1172/JCI38291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu Y, Nedungadi TP, Zhu L, Sobhani N, Irani BG, Davis KE, et al. Distinct hypothalamic neurons mediate estrogenic effects on energy homeostasis and reproduction. Cell Metab. 2011;14:453–65. doi: 10.1016/j.cmet.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Y, Manka D, Wagner KU, Khan SA. Estrogen receptor-alpha expression in the mammary epithelium is required for ductal and alveolar morphogenesis in mice. Proc Natl Acad Sci U S A. 2007;104:14718–23. doi: 10.1073/pnas.0706933104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alva JA, Zovein AC, Monvoisin A, Murphy T, Salazar A, Harvey NL, et al. VE-Cadherin-Cre-recombinase transgenic mouse: a tool for lineage analysis and gene deletion in endothelial cells. Dev Dyn. 2006;235:759–67. doi: 10.1002/dvdy.20643. [DOI] [PubMed] [Google Scholar]
- 25.Xue B, Pamidimukkala J, Lubahn DB, Hay M. Estrogen receptor-alpha mediates estrogen protection from angiotensin II-induced hypertension in conscious female mice. American journal of physiology Heart and circulatory physiology. 2007;292:H1770–6. doi: 10.1152/ajpheart.01011.2005. [DOI] [PubMed] [Google Scholar]
- 26.Sun J, Morgan M, Shen RF, Steenbergen C, Murphy E. Preconditioning results in S-nitrosylation of proteins involved in regulation of mitochondrial energetics and calcium transport. Circulation research. 2007;101:1155–63. doi: 10.1161/CIRCRESAHA.107.155879. [DOI] [PubMed] [Google Scholar]
- 27.Jaffrey SR, Snyder SH. The biotin switch method for the detection of S-nitrosylated proteins. Sci STKE. 2001;2001:pl1. doi: 10.1126/stke.2001.86.pl1. [DOI] [PubMed] [Google Scholar]
- 28.Tong G, Aponte AM, Kohr MJ, Steenbergen C, Murphy E, Sun J. Postconditioning leads to an increase in protein S-nitrosylation. American journal of physiology Heart and circulatory physiology. 2014;306:H825–32. doi: 10.1152/ajpheart.00660.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kohr MJ, Sun J, Aponte A, Wang G, Gucek M, Murphy E, et al. Simultaneous measurement of protein oxidation and S-nitrosylation during preconditioning and ischemia/reperfusion injury with resin-assisted capture. Circulation research. 2011;108:418–26. doi: 10.1161/CIRCRESAHA.110.232173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun J, Picht E, Ginsburg KS, Bers DM, Steenbergen C, Murphy E. Hypercontractile female hearts exhibit increased S-nitrosylation of the L-type Ca2+ channel alpha1 subunit and reduced ischemia/reperfusion injury. Circulation research. 2006;98:403–11. doi: 10.1161/01.RES.0000202707.79018.0a. [DOI] [PubMed] [Google Scholar]
- 31.Sun J, Aponte AM, Kohr MJ, Tong G, Steenbergen C, Murphy E. Essential role of nitric oxide in acute ischemic preconditioning: S-nitros(yl)ation versus sGC/cGMP/PKG signaling? Free radical biology & medicine. 2013;54:105–12. doi: 10.1016/j.freeradbiomed.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Methner C, Lukowski R, Grube K, Loga F, Smith RA, Murphy MP, et al. Protection through postconditioning or a mitochondria-targeted S-nitrosothiol is unaffected by cardiomyocyte-selective ablation of protein kinase G. Basic research in cardiology. 2013;108:337. doi: 10.1007/s00395-013-0337-1. [DOI] [PubMed] [Google Scholar]
- 33.Chen Y, Li Z, He Y, Shang D, Pan J, Wang H, et al. Estrogen and pure antiestrogen fulvestrant (ICI 182 780) augment cell-matrigel adhesion of MCF-7 breast cancer cells through a novel G protein coupled estrogen receptor (GPR30)-to-calpain signaling axis. Toxicology and applied pharmacology. 2014;275:176–81. doi: 10.1016/j.taap.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Filardo EJ, Quinn JA, Frackelton AR, Jr, Bland KI. Estrogen action via the G protein-coupled receptor, GPR30: stimulation of adenylyl cyclase and cAMP-mediated attenuation of the epidermal growth factor receptor-to-MAPK signaling axis. Molecular endocrinology. 2002;16:70–84. doi: 10.1210/mend.16.1.0758. [DOI] [PubMed] [Google Scholar]
- 35.Prossnitz ER, Arterburn JB. International Union of Basic and Clinical Pharmacology. XCVII. G Protein-Coupled Estrogen Receptor and Its Pharmacologic Modulators. Pharmacological reviews. 2015;67:505–40. doi: 10.1124/pr.114.009712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pugach EK, Blenck CL, Dragavon JM, Langer SJ, Leinwand LA. Estrogen receptor profiling and activity in cardiac myocytes. Molecular and cellular endocrinology. 2016;431:62–70. doi: 10.1016/j.mce.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin J, Steenbergen C, Murphy E, Sun J. Estrogen receptor-beta activation results in S-nitrosylation of proteins involved in cardioprotection. Circulation. 2009;120:245–54. doi: 10.1161/CIRCULATIONAHA.109.868729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deschamps AM, Murphy E. Activation of a novel estrogen receptor, GPER, is cardioprotective in male and female rats. American journal of physiology Heart and circulatory physiology. 2009;297:H1806–13. doi: 10.1152/ajpheart.00283.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nuedling S, Karas RH, Mendelsohn ME, Katzenellenbogen JA, Katzenellenbogen BS, Meyer R, et al. Activation of estrogen receptor beta is a prerequisite for estrogen-dependent upregulation of nitric oxide synthases in neonatal rat cardiac myocytes. FEBS letters. 2001;502:103–8. doi: 10.1016/s0014-5793(01)02675-8. [DOI] [PubMed] [Google Scholar]
- 40.Chouchani ET, Methner C, Nadtochiy SM, Logan A, Pell VR, Ding S, et al. Cardioprotection by S-nitrosation of a cysteine switch on mitochondrial complex I. Nature medicine. 2013;19:753–9. doi: 10.1038/nm.3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Booth EA, Marchesi M, Kilbourne EJ, Lucchesi BR. 17Beta-estradiol as a receptor-mediated cardioprotective agent. The Journal of pharmacology and experimental therapeutics. 2003;307:395–401. doi: 10.1124/jpet.103.054205. [DOI] [PubMed] [Google Scholar]
- 42.Robertson JF, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet. 2016;388:2997–3005. doi: 10.1016/S0140-6736(16)32389-3. [DOI] [PubMed] [Google Scholar]
- 43.Lee CI, Goodwin A, Wilcken N. Fulvestrant for hormone-sensitive metastatic breast cancer. The Cochrane database of systematic reviews. 2017;1:CD011093. doi: 10.1002/14651858.CD011093.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bross PF, Baird A, Chen G, Jee JM, Lostritto RT, Morse DE, et al. Fulvestrant in postmenopausal women with advanced breast cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2003;9:4309–17. [PubMed] [Google Scholar]
- 45.Lubahn DB, Moyer JS, Golding TS, Couse JF, Korach KS, Smithies O. Alteration of reproductive function but not prenatal sexual development after insertional disruption of the mouse estrogen receptor gene. Proceedings of the National Academy of Sciences of the United States of America. 1993;90:11162–6. doi: 10.1073/pnas.90.23.11162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gabel SA, Walker VR, London RE, Steenbergen C, Korach KS, Murphy E. Estrogen receptor beta mediates gender differences in ischemia/reperfusion injury. Journal of molecular and cellular cardiology. 2005;38:289–97. doi: 10.1016/j.yjmcc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 47.Pendaries C, Darblade B, Rochaix P, Krust A, Chambon P, Korach KS, et al. The AF-1 activation-function of ERalpha may be dispensable to mediate the effect of estradiol on endothelial NO production in mice. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:2205–10. doi: 10.1073/pnas.042688499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Favre J, Gao J, Henry JP, Remy-Jouet I, Fourquaux I, Billon-Gales A, et al. Endothelial estrogen receptor {alpha} plays an essential role in the coronary and myocardial protective effects of estradiol in ischemia/reperfusion. Arteriosclerosis, thrombosis, and vascular biology. 2010;30:2562–7. doi: 10.1161/ATVBAHA.110.213637. [DOI] [PubMed] [Google Scholar]
- 49.Nikolic I, Liu D, Bell JA, Collins J, Steenbergen C, Murphy E. Treatment with an estrogen receptor-beta-selective agonist is cardioprotective. Journal of molecular and cellular cardiology. 2007;42:769–80. doi: 10.1016/j.yjmcc.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 50.Schuster I, Mahmoodzadeh S, Dworatzek E, Jaisser F, Messaoudi S, Morano I, et al. Cardiomyocyte-specific overexpression of oestrogen receptor beta improves survival and cardiac function after myocardial infarction in female and male mice. Clin Sci (Lond) 2016;130:365–76. doi: 10.1042/CS20150609. [DOI] [PubMed] [Google Scholar]
- 51.Zhan Y, Liu Z, Li M, Ding T, Zhang L, Lu Q, et al. ERbeta expression in the endothelium ameliorates ischemia/reperfusion-mediated oxidative burst and vascular injury. Free radical biology & medicine. 2016;96:223–33. doi: 10.1016/j.freeradbiomed.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 52.Ihionkhan CE, Chambliss KL, Gibson LL, Hahner LD, Mendelsohn ME, Shaul PW. Estrogen causes dynamic alterations in endothelial estrogen receptor expression. Circulation research. 2002;91:814–20. doi: 10.1161/01.res.0000038304.62046.4c. [DOI] [PubMed] [Google Scholar]
- 53.Madak-Erdogan Z, Kim SH, Gong P, Zhao YC, Zhang H, Chambliss KL, et al. Design of pathway preferential estrogens that provide beneficial metabolic and vascular effects without stimulating reproductive tissues. Science signaling. 2016;9:ra53. doi: 10.1126/scisignal.aad8170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.