Abstract
Purpose
To determine the rate and associated factors for acquiring a decubitus series at CT colonography (CTC), in addition to the standard supine and prone series.
Materials and Methods
CTC examinations read centrally at one institution but performed at three different centers in 6,380 adults were reviewed to determine the frequency of an additional decubitus series. Results were analyzed according to study indication (primary screening versus diagnostic for incomplete colonoscopy), practice site (academic versus community), patient age, gender, body mass index (BMI), and temporal variation. At all sites, the CT technologist determined the need for an additional decubitus series, with infrequent radiologist input in select cases.
Results
The frequency for the CT technologist to obtain a decubitus series at screening was 9.7% (578/5952), compared with 22.9% (98/428) following failed colonoscopy (p<0.001). The decubitus rate at the academic center (9.4%, 550/5871) was significantly lower than the community hospitals (34.6% combined, 28/81) (p<0.001). The rate progressively increased with age, from 5.0% under age 50 to 28.0% over age 80. No significant difference was seen between men and women (10.3% versus 9.2%), but a strong correlation existed with increased BMI, rising to >25% for BMI over 40. Marked temporal variation existed at the academic center, with quarterly rates ranging from 0% to 17%.
Conclusions
The frequency for performing a third series at CTC varies considerably according to indication, practice site, patient age, BMI, and time. These results have important implications for clinical practice, including the need for improved training and feedback for CT technologists.
Introduction
CT colonography (CTC) is an effective technique for colorectal screening, comparable to traditional optical colonoscopy (OC) for the detection of advanced neoplasia.1-3 However, it is dependent upon technical factors such as optimized colonic distention to maintain quality. Based on well-established findings, 4-6 the standard American College of Radiology (ACR) CTC protocol7 specifies that the patient be scanned in both the supine and prone positions, to allow complete evaluation of the colon with dependent shifting of luminal fluid and complementary distention of non-dependent colonic segments. In a minority of cases, the same colonic segments will be collapsed on the standard positions, necessitating a third series to achieve full diagnostic evaluation. The sigmoid and/or descending colon account for the great majority of non-diagnostic segments, necessitating a right lateral decubitus series to complete the examination.8, 9 The rate at which a third series is acquired at CTC is currently unknown but has important implications for quality measures, radiation dose, procedural efficiency, and training. The purpose of this study was to determine the rate and associated factors for acquiring a third series at CTC.
Materials and Methods
Study Group
This retrospective study complied with the Health Insurance and Portability and Accountability Act and was approved by our institutional review board. The requirement for informed consent was waived. CTC examinations were performed on consecutive individuals from April of 2004 through August of 2009. A total of 6,380 individual patient examinations were reviewed and represent the study population. Both primary screening CTC examinations and patients referred for CTC due to previous incomplete optical colonoscopy were included for review. CTC exams were performed at three different hospital systems, including an academic center and two smaller community-based hospitals (referred to as Community Hospitals 1 & 2). All studies were interpreted centrally at the academic center by one of seven abdominal radiologists. The majority of exams (5,872/6,380; 92.0%) were performed at the academic center (main hospital and outpatient clinics) by the same group of CT technologists who rotate among the various sites within the center.
CT Colonography Technique
The CTC protocol utilized at these centers has been described in detail previously.9 In brief, the patient undergoes a laxative bowel cleansing and fecal tagging protocol on the day prior to the planned examination. During the study period, the laxatives used were sodium phosphate (Phosphosoda; CB Fleet, Lynchburg, VA), magnesium citrate (Sunmark, San Francisco, VA), or, rarely, polyethylene glycol (Golytely; Braintree Laboratories, Braintree, MA). Since 2008, magnesium citrate has been the standard cathartic agent, replacing sodium phosphate due to the potential for the very rare but serious complication of acute phosphate nephropathy. Comparative studies have demonstrated equal efficacy in bowel cleansing with these two agents.10 Fecal tagging is accomplished with a regimen consisting of 250 ml of 2.1% wt/vol barium sulfate (Readi-cat; Bracco Diagnostics, Princeton, NJ) and 60 ml of diatrizoate (Gastrograffin; Bracco Diagnostics).
Colonic insufflation was performed using our standard technique, 8, 9 consisting of automated low-pressure delivery of carbon dioxide (Protoco2l; Bracco Diagnostics) via rectal catheter, except for a small initial subset of 419 patients who underwent manual room air insufflation. Spasmolytics were not administered for any case. Supine scanning was performed after intracolonic equilibrium pressure was achieved and adequate distention was identified on the scout view by the CT technologist. The reconstructed transverse CT images were then immediately reviewed in cine mode by the technologist to ensure adequate colonic distention, with particular attention to the sigmoid and descending colon. This protocol was then repeated for the prone series. Placing pillows under the chest in an attempt to minimize compression of the transverse colon is generally performed for larger patients.
After supine and prone acquisition, the decision to perform an additional decubitus series was made immediately following review of the initial two positions by the CT technologist (Fig 1). The main criterion for performing a third (decubitus) series is when both the supine and prone views are truly nondiagnostic at the same anatomic location due to complete or near complete focal luminal collapse. In practice, however, a CT technologist may obtain a third series when focal distention is suboptimal but arguably “diagnostic” according to an experienced radiologist, making this determination somewhat subjective, which is unavoidable in clinical practice . During the start-up phase of our CTC program, only a few dedicated CT technologists were performing CTC and there was generally more dedicated training and radiologist input. However, as the program matured beyond the first year, this responsibility diffused throughout the entire pool of CT technologists, primarily through on-the-job style training. Radiologist input during the CTC examination beyond this point was been limited to select cases where the technologist requested specific guidance during a difficult exam.
Figure 1.
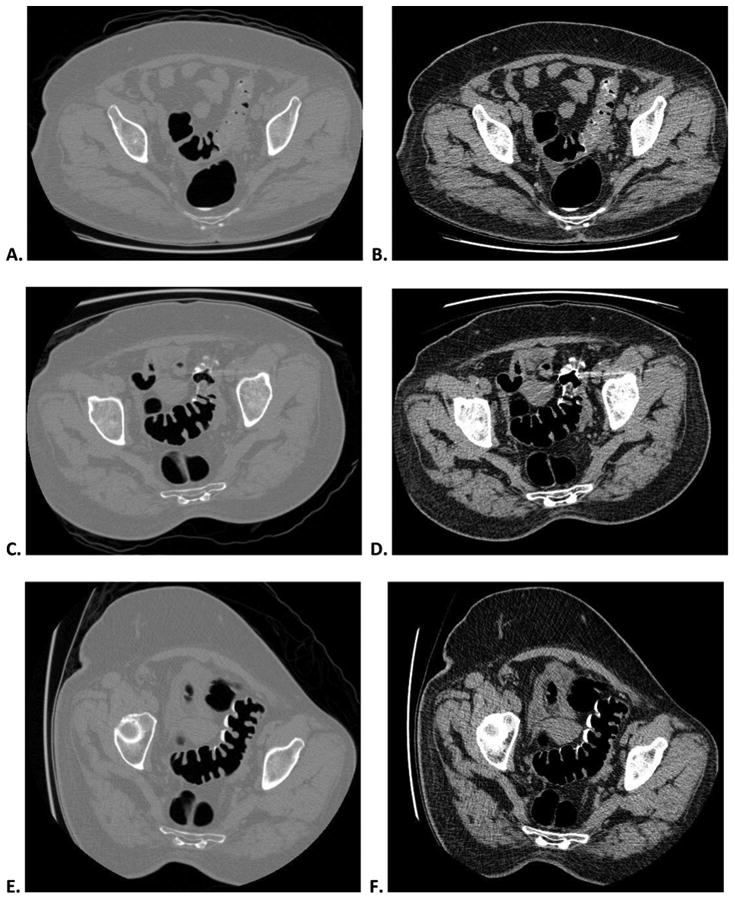

Decubitus position obtained for nondiagnostic sigmoid distention on both supine and prone series at CTC screening in an asymptomatic 60-year-old woman.
Supine CTC images with polyp (A) and soft tissue (B) windowing show complete collapse of a long segment of sigmoid colon. Prone CTC images (C and D) show somewhat improved sigmoid distention but with persistent focal areas of collapse. Given these findings, the CT technologist obtained a third series in the right lateral decubitus position (E and F), which demonstrate good sigmoid distention, leading to overall diagnostic adequacy. Note how the segmental collapse is not apparent on the supine scout view (G), which is why we require online review of the 2D images in cine mode at the CT console by the. The majority of cases of inadequate distention involve the sigmoid colon.
Image acquisition was performed with 8- or 16-channel multidetector CT scanners (LightSpeed; GE Healthcare, Waukesha, WI). Technique consisted of 1.25 mm collimation, 1 mm reconstruction interval, 120 kVp, and either a fixed tube current-time product (50-75 mAs) or dose modulation (noise index set at 50, 30-300 mA range). CTC interpretation was performed on a dedicated 3D workstation (V3D Colon; Viatronix, Stony Brook, NY).
Data Analysis
The CTC program at [BLINDED] maintains a customized electronic database (Microsoft Access; Microsoft Corp., Redmond, WA) that allows for demographic queries including patient age, gender, height, weight, date of service, and diagnostic adequacy of the exam. To determine whether a third imaging series was undertaken, each exam was reviewed in all 6,380 patients. The data was subdivided and analyzed according to the center where it was performed (academic center versus community hospitals), study indication (primary screening versus diagnostic for incomplete colonoscopy), age, gender, body mass index (BMI), and date of service. The height and weight data were collected in inches and pounds, respectively, and BMI was calculated using the formula (weight/height2) × 703 as described by the Centers for Disease Control and Prevention.
A continuity-corrected Pearson chi-squared test was used to assess the association between the extra view rate and categorical factors: institution, incomplete OC vs. VC, gender, age group, and BMI groups. Because the use of manual room air insufflation corresponded to the start-up phase of our program when there was more concentrated expertise in making the determination for a third series, we believe this data does not truly reflect the distention technique. It has been shown previously that automated carbon dioxide improves colonic distention at CTC.8, 11 P < 0.05 (two-sided) was the criterion for statistical significance. All computations were obtained in R version 2.10.0 (R Development Core Team 2009). 95% confidence intervals were calculated using the Adjusted Wald method.
Results
The mean patient age of this cohort was 57.4 years ± 7.8 (n=6,380). There were 3,492 women (54.7%) and 2,888 men (45.3%). The mean BMI was 28.0, with a standard deviation of 6.1. The overall rate for an additional decubitus series, regardless of indication, was 10.6% (676/6,380). However, the decubitus rate was significantly lower for exams performed for primary screening at 9.7% (578/5,952) than those performed after failed optical colonoscopy at 22.9% (98/428) (p<0.001).
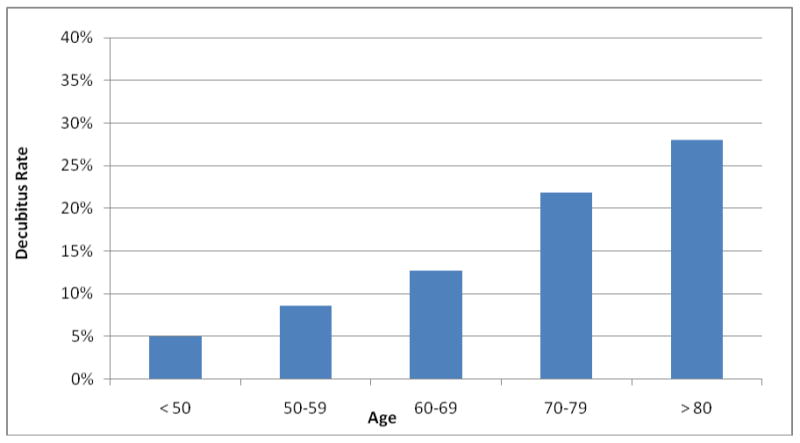
Gender demonstrated no statistically significant difference between male and females, with a rate of 10.3% (283/2736) for men and a rate of 9.2% (295/3216) for women (p=0.190). Positive associations were evident with increasing age. Figure 2 depicts the decubitus rate as a function of age. Older patient populations were seen more often requiring a decubitus position than younger persons. Statistically significant differences (p<0.0001) were seen between the age cohorts (grouped by decades): 5.0% (13/258) for under 50, 8.6% (353/4094) for 50-59, 12.8% (195/1530) for 60-69, 21.9% (82/375) for 70-79, and 28.0% (33/118) for over 80 years of age. The majority (n=5,624) who underwent CTC in our program were in the 50-70 year-old age range with the greatest percentage (64.2% of the total) in the 50-59 year-old age grouping. Patients below the age of 50 or over 80 were less common and more often underwent CTC for diagnostic purposes rather than routine screening.
Figure 2. Decubitus rate according to patient age.
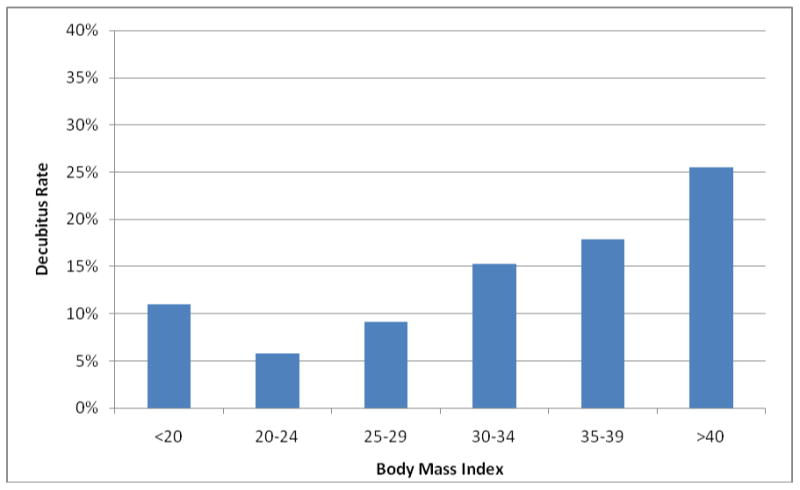
Height and weight data used to calculate the BMI were available for 6,237 of the 6,380 patients (97.8%) and is presented in Figure 3. Statistically significant differences (p<0.0001) were found when patients were grouped into low to underweight individuals (BMI < 20), normal weight (20-24.9), overweight (25-29.9), and varying degrees of obesity (≥ 30). The decubitus rate was increased for overweight and obese individuals (524/4134; 12.7%) compared to the normal weight group (108/1,875; 5.8%). Interestingly, the decubitus rate was higher for the thinnest individuals at 11.0% (25/228) than for the normal weight persons.
Figure 3. Decubitus rate according to body mass index (BMI).
Practice site affected the decubitus rate (Table 1). For primary CTC evaluation cases (excluding cases performed after failed colonoscopy), the decubitus rate was 9.4% (550/5871) at the academic center, whereas at the two community hospitals, the rates were considerably higher at 43.9% (18/41) and 25.0% (10/40) (p<0.0001).
Table 1. Decubitus Rates for Primary CTC Screening according to Practice Site.
| Institution | Number of Studies | Decubitus Views | Rate (95% CI) |
|---|---|---|---|
| Academic Center | 5871 | 550 | 9.4% (8.7-10.1) |
| Community Hospital 1 | 41 | 18 | 43.9% (29.9-60.3) |
| Community Hospital 2 | 40 | 10 | 25.0% (14.0-41.2) |
| Total | 5952 | 578 | 9.7% (9.0-10.5) |
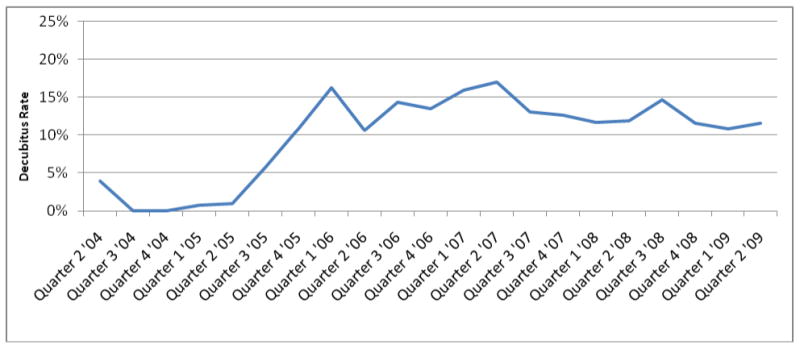
Figure 4 depicts the decubitus rate over time. A statistically significant different is seen between the first year rate and the subsequent years (0.5% vs 11.5%; p<0.0001). This corresponds to a program change where all CT technologists were required to perform CTC exams as opposed to a limited pool of dedicated CTC technologists in the first year.
Figure 4. Quarterly decubitus rate over a 5-year time period.
Discussion
The purpose of this analysis was to assess the largely unknown rate at which an additional decubitus series is performed at CTC following the standard supine and prone images and to correlate for associated factors that may affect this rate This rate reflects a balance between the need for obtaining an adequate examination and the desire to limit the overall time and radiation dose per case. While local experience, protocols, and standards of care will vary somewhat among different practices, our hope is that this data can be used for comparison and training purposes by other groups performing CTC. Our findings have helped to identify areas of potential improvement for our program, particularly in terms of ongoing CT technologist training and feedback. These results can also serve as an initial benchmark for other programs. When radiologists make the on-line decision for performing an additional decubitus view, we believe this rate can be kept under 10% for CTC screening. Keeping this rate under 10% will likely be more challenging when CT technologists determine the need for an additional series, as is the case for our program. Furthermore, for diagnostic CTC performed after incomplete colonoscopy, the decubitus rate will generally rise as we have previously demonstrated a significant increase in the anatomic challenges of redundancy, tortuosity, and diverticular disease.12 In the end, well under 1% of our CTC cases are deemed non-diagnostic due incomplete distention, suggesting that the decubitus view is salvaging a number of potentially borderline cases.
The goal of screening CTC is to evaluate the large intestine to find significant polyps with the potential to progress to colorectal cancer and to interrupt this disease process. For CTC to be successful, adequate luminal distention is essential. Thresholds at which extra positioning and imaging are deemed necessary will vary. The circumstance where an additional series is clearly necessary is when complete luminal collapse is seen at the same location on both supine and prone series. For borderline cases where diagnostic adequacy is more equivocal, the decision to perform a third series is quite subjective and will vary according to experience level and interpretive confidence. In our experience, there was a significant increase in the decubitus rate between the first year of the program, when there was more radiologist oversight and only a few CT technologists were involved, compared with subsequent years as the program matured, when many more technologists became involved with considerably less radiologist involvement. To implement a successful CTC screening program in a busy practice, we believe that delegating this quality assurance responsibility to the CT technologists is essential. However, this study suggests that ongoing training and continued feedback may be important to keep the decubitus rate at an acceptable level.
In addition to reviewing the planar scout projections, the CT technologists are instructed to evaluate the transverse 2D images for both supine and prone positions, with particular attention to the sigmoid and descending colon, to assess the degree of distention. Although technologists are generally accustomed to reviewing scout images for prescribing scan ranges and assessing position, assessing the 2D transverse images will be somewhat foreign at first to some. Nonetheless, this 2D review is critical to adequately gauge distention since overlapping loops of bowel and sigmoid redundancy limits evaluation on the scout view alone.13, 14 With less radiologist oversight, it is quite likely that the fear of a nondiagnostic exam could influence the technologist to have a lower threshold for obtaining an extra view. The use of CO2 has been shown to both improve distention and reduce post-procedural discomfort over manual room air distention.8, 15, 16 In addition, the automated nature of CO2 is strongly preferred by technologists, because the determination of an end point prior to scanning is much more straightforward compared with manual room air distention.8
Beyond the temporal influence we observed with the decubitus rate, we also found that the rate was substantially higher at the two low-volume community-based hospitals compared with the large academic center. These community hospitals utilize the identical protocol developed at the academic center,9, 17 but perform significantly fewer studies, which could have parallels with practices initiating a CTC program. Experience at our primary site has shown that our technologists become much more comfortable over time with handling colonic distention and patient counseling. As CTC continues to mature and quality assurance programs are instituted, the rate of performing a decubitus view may ultimately prove to be a useful quality measure.
Correlation of the decubitus rate with patient age and body mass index revealed interesting results, which were not completely unexpected. The decubitus rate steadily rose with patient age as shown in Figure 2. The most likely explanation for this observation is the increasing frequency of diverticular disease in older age groups, particularly involving the sigmoid colon.18 The bowel wall changes of myochosis, perhaps coupled with spasm, can result in collapse or at least suboptimal distention. Additional explanations could include weaker anal sphincter tone allowing for escape of rectal gas, as well as difficulties lying either in the standard prone or supine positions on the CT gantry table. Gryspeerdt et al have suggested the use of supine and left lateral decubitus positioning for CTC in elderly patients in lieu of the usual supine-prone combination.19 The correlation of the decubitus rate with BMI also matched our initial suspicions. The rate was somewhat higher in underweight individuals, which could possibly be explained by intra-abdominal crowding due to lack of significant intraperitoneal fat. An increased rate of incomplete colonoscopy has also been noted with low-BMI individuals.20 For overweight and obese individuals, the decubitus rates showed progressive increase. Because the CO2 apparatus is a very low-level pressure system, it is likely that the extrinsic pressure related to the abdominal girth can overwhelm the intraluminal gas pressure and cause collapse. This factor is coupled with the many other practical difficulties encountered in evaluating obese individuals.
Like many other practices, our CTC program commonly receives referrals following failed or aborted optical colonoscopy.21-25 Not surprisingly, the rate at which an extra series was obtained in this cohort was more than twice that of our screening population. Many of the reasons leading to a failed colonoscopy, particularly diverticular disease, redundancy, tortuosity, and occlusive masses can all lead to greater challenges with distention at CTC.12
AS CTC continues to progress towards more widespread acceptance, one concern that is frequently voiced is that of radiation dose.26 CTC protocols have been devised to minimize radiation while still providing a diagnostic evaluation. The current effective dose for a single CTC series is generally on the order of 2.5 mSv, resulting in a total effective dose of approximately 5 mSv when two views are performed, and 7.5 mSv when three views are performed. Although this difference is unlikely to be clinically relevant, the ALARA approach should motivate programs to limit a third series as much as possible without significantly impacting diagnostic quality. Further reductions in dose are expected in the near future related to novel reconstruction and denoising algorithms. Regardless, the small theoretical risks related to low-dose radiation, which may or may not even exist, are clearly less than the known measurable risk related to optical colonoscopy.27-32
This study sought to establish a baseline rate for obtaining an additional decubitus position at CTC. We acknowledge several limitations. Given the large cohort size, specific reasons for obtaining a decubitus series in each case were not specifically evaluated. The clear increase in the rate of decubitus series beyond the first year of our screening program, as well as the discrepancy between the community and academic centers, suggests that at least some additional series could have been avoided. As this study was not designed to address this issue, this would be better addressed with a smaller study cohort with retrospective readers. Similarly, this study did not address whether the decubitus position actually provided benefit to the diagnostic quality of the exam, which could also be addressed by a retrospective study design. Our experience has taught us that segmental sigmoid underdistention is by far the most common culprit of inadequate distention.8 The relatively small numbers of patients at the community hospitals is an additional limitation that limits our comparison, although the striking difference in decubitus rates allows this to already approach statistical significance. Finally, because spasmolytics such as glucagon and buscopan are not employed in our CTC program, we cannot assess their effect on the decubitus rate. It would be interesting to compare our decubitus rate of 9.7% with the rate seen in the ACRIN trial, which did employ glucagon.2
In summary, the frequency for performing a decubitus series at CTC in our practice varied considerably according to study indication, practice site, patient age, BMI, and over time. The decubitus rates were similar between men and women. When considering our findings, it is critical to note that the CT technologist is primarily responsible for determining the need for a decubitus series – not the radiologist. These results have important implications for clinical practice, including the need for improved training and feedback for CT technologists. Our results also establish an initial benchmark for other programs to compare against their own experience. Future improvements in technique and training will likely lead to a lower rate in obtaining a third decubitus series at CTC
References
- 1.Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. New England Journal of Medicine. 2003;349:2191–200. doi: 10.1056/NEJMoa031618. [DOI] [PubMed] [Google Scholar]
- 2.Johnson CD, Chen MH, Toledano AY, et al. Accuracy of CT colonography for detection of large adenomas and cancers. New England Journal of Medicine. 2008;359:1207–17. doi: 10.1056/NEJMoa0800996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim DH, Pickhardt PJ, Taylor AJ, et al. CT colonography versus colonoscopy for the detection of advanced neoplasia. New England Journal of Medicine. 2007;357:1403–12. doi: 10.1056/NEJMoa070543. [DOI] [PubMed] [Google Scholar]
- 4.Yee J, Kumar NN, Hung RK, Akerkar GA, Kumar PR, Wall SD. Comparison of supine and prone scanning separately and in combination at CT colonography. Radiology. 2003;226:653–61. doi: 10.1148/radiol.2263010701. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher JG, Johnson CD, Welch TJ, et al. Optimization of CT colonography technique: Prospective trial in 180 patients. Radiology. 2000;216:704–11. doi: 10.1148/radiology.216.3.r00au41704. [DOI] [PubMed] [Google Scholar]
- 6.Chen SC, Lu DSK, Hecht JR, Kadell BM. CT colonography: Value of scanning in both the supine and prone positions. American Journal of Roentgenology. 1999;172:595–9. doi: 10.2214/ajr.172.3.10063842. [DOI] [PubMed] [Google Scholar]
- 7.ACR Practice Guideline for the Performance of Computed Tomography (CT) Colonography in Adults. Reston, VA: American College of Radiology; 2006. [DOI] [PubMed] [Google Scholar]
- 8.Shinners TJ, Pickhardt PJ, Taylor AJ, Jones DA, Olsen CH. Patient-controlled room air insufflation versus automated carbon dioxide delivery for CT colonography. American Journal of Roentgenology. 2006;186:1491–6. doi: 10.2214/AJR.05.0416. [DOI] [PubMed] [Google Scholar]
- 9.Pickhardt PJ. Screening CT colonography: How I do it. American Journal of Roentgenology. 2007;189:290–8. doi: 10.2214/AJR.07.2136. [DOI] [PubMed] [Google Scholar]
- 10.Borden ZS, Pickhardt PJ, Kim DH, Lubner MG, Agriantonis DJ, Hinshaw JL. Bowel Preparation for CT Colonography: Blinded Comparison of Magnesium Citrate and Sodium Phosphate for Catharsis. Radiology. 2010;254:138–44. doi: 10.1148/radiol.09090398. [DOI] [PubMed] [Google Scholar]
- 11.Burling D, Taylor SA, Halligan S, et al. Automated insufflation of carbon dioxide for MDCT colonography: Distension and patient experience compared with manual insufflation. American Journal of Roentgenology. 2006;186:96–103. doi: 10.2214/AJR.04.1506. [DOI] [PubMed] [Google Scholar]
- 12.Hanson ME, Pickhardt PJ, Kim DH, Pfau PR. Anatomic factors predictive of incomplete colonoscopy based on findings at CT colonography. American Journal of Roentgenology. 2007;189:774–9. doi: 10.2214/AJR.07.2048. [DOI] [PubMed] [Google Scholar]
- 13.Kim DH, Pickhardt PJ. Colonic distention for CT colonography. In: Pickhardt PJ, editor. Colonography: principles & practice of virtual colonoscopy. Philadelphia: Suanders; 2010. pp. 131–47. [Google Scholar]
- 14.Choi M, Taylor AJ, VonBerge JL, Bartels CM, Pickhardt PJ. Can the CT scout reliably assess for adequate colonic distention at CT colonography? American Journal of Roentgenology. 2005;184:21–2. [Google Scholar]
- 15.Sumanac K, Zealley I, Fox BM, et al. Minimizing postcolonoscopy abdominal pain by using CO2 insufflation: A prospective, randomized, double blind, controlled trial evaluating a new commercially available CO2 delivery system. Gastrointestinal Endoscopy. 2002;56:190–4. doi: 10.1016/s0016-5107(02)70176-4. [DOI] [PubMed] [Google Scholar]
- 16.Robson NK, Lloyd M, Regan F. The Use of Carbon-Dioxide as an Insufflation Agent in Barium Enema - Does It Have a Role. British Journal of Radiology. 1993;66:197–8. doi: 10.1259/0007-1285-66-783-197. [DOI] [PubMed] [Google Scholar]
- 17.Pickhardt PJ, Kim DH. CT colonography (virtual colonoscopy): A practical approach for population screening. Radiologic Clinics of North America. 2007;45:361. doi: 10.1016/j.rcl.2007.03.011. -+ [DOI] [PubMed] [Google Scholar]
- 18.Sanford MF, Pickhardt PJ. Diagnostic performance of primary 3-dimensional computed tomography colonography in the setting of colonic diverticular disease. Clinical Gastroenterology and Hepatology. 2006;4:1039–47. doi: 10.1016/j.cgh.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Gryspeerdt SS, Herman MJ, Baekelandt MA, van Holsbeeck BG, Lefere PA. Supine/left decubitus scanning: a valuable alternative to supine/prone scanning in CT colonography. European Radiology. 2004;14:768–77. doi: 10.1007/s00330-004-2264-x. [DOI] [PubMed] [Google Scholar]
- 20.Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. American Journal of Gastroenterology. 2000;95:2784–7. doi: 10.1111/j.1572-0241.2000.03186.x. [DOI] [PubMed] [Google Scholar]
- 21.Yucel C, Lev-Toaff AS, Moussa N, Durrani H. CT colonography for incomplete or contraindicated optical colonoscopy in older patients. American Journal of Roentgenology. 2008;190:145–50. doi: 10.2214/AJR.07.2633. [DOI] [PubMed] [Google Scholar]
- 22.Morrin MM, Kruskal JB, Farrell RJ, Goldberg SN, McGee JB, Raptopoulos V. Endoluminal CT colonography after an incomplete endoscopic colonoscopy. American Journal of Roentgenology. 1999;172:913–8. doi: 10.2214/ajr.172.4.10587120. [DOI] [PubMed] [Google Scholar]
- 23.Macari M, Berman P, Dicker M, Milano A, Megibow AJ. Usefulness of CT colonography in patients with incomplete colonoscopy. American Journal of Roentgenology. 1999;173:561–4. doi: 10.2214/ajr.173.3.10470879. [DOI] [PubMed] [Google Scholar]
- 24.Hanson ME, Pickhardt PJ, Kim DH, Pfau PR. Anatomic factors predictive of incomplete colonoscopy based on findings at CT colonography. AJR Am J Roentgenol. 2007;189:774–9. doi: 10.2214/AJR.07.2048. [DOI] [PubMed] [Google Scholar]
- 25.Copel L, Sosna J, Kruskal JB, Raptopoulos V, Farrell RJ, Morrin MM. CT colonography in 546 patients with incomplete colonoscopy. Radiology. 2007;244:471–8. doi: 10.1148/radiol.2442060837. [DOI] [PubMed] [Google Scholar]
- 26.Brenner DJ, Georgsson MA. Mass Screening With CT Colonography: Should the Radiation Exposure Be of Concern? Gastroenterology. 2005;129:328–37. doi: 10.1053/j.gastro.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 27.Radiation risk in perspective: position statement of the Health Physics Society. Health Physics Society; Adopted January 1996, revised August 2004. [Google Scholar]
- 28.Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: A population-based study. J Natl Cancer Inst. 2003;95:230–6. doi: 10.1093/jnci/95.3.230. [DOI] [PubMed] [Google Scholar]
- 29.Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg. 2008;143:701–6. doi: 10.1001/archsurg.143.7.701. [DOI] [PubMed] [Google Scholar]
- 30.Kim DH, Pickhardt PJ, Taylor AJ, Menias CO. Imaging evaluation of complications at optical colonoscopy. Curr Probl Diagn Radiol. 2008;37:165–77. doi: 10.1067/j.cpradiol.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Levin TR. Complications of colonoscopy. Annals of Internal Medicine. 2007;147:213–4. doi: 10.7326/0003-4819-147-3-200708070-00016. [DOI] [PubMed] [Google Scholar]
- 32.Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and Perforation After Outpatient Colonoscopy and Their Risk Factors in Usual Clinical Practice. Gastroenterology. 2008;135:1899–906. doi: 10.1053/j.gastro.2008.08.058. [DOI] [PubMed] [Google Scholar]


