Abstract
Purpose
To compare total colonic gas volume and segmental luminal distention according to patient position at CT colonography (CTC), and determine which two views should constitute the routine protocol.
Methods
Volumetric analysis was retrospectively performed on CTC examinations from 146 adults (mean age, 59.2 years; 81M/65F; mean BMI, 30.9) where supine, prone, and right lateral decubitus series were sequentially obtained using continuous low-pressure CO2 insufflation. Total colonic gas volumes were assessed using a novel automated volumetric tool. In addition, two radiologists scored distention by segment using a 4-point scale (4=Optimal/3=Adequate/2=Inadequate/1=Collapsed).
Results
Mean colonic gas volume (±SD) for supine, prone, and decubitus positioning was 1,617±567 ml, 1441±505 ml, and 1901±627 ml, respectively (p<0.001). Colonic volume was highest on the right lateral decubitus series in 73.3% (107/146) and lowest in 6.2% (9/146) of cases, whereas the prone series was highest in 0.7% (1/146) and lowest in 73.3% (107/146) of cases. Overall mean segmental reader scores and % inadequate/collapsed for supine, prone, and decubitus positions were 3.48/3.33/3.71, and 10.4%/12.1%/4.2%, respectively (p<0.001). The only mean segmental scores below 3.0 were the sigmoid on supine (2.68) and prone (2.58), compared with 3.23 on decubitus (p<0.001). Improvement in both decubitus and supine distention over prone increased further with increasing BMI (p<0.001).
Conclusions
The right lateral decubitus position consistently yields the best colonic distention at CTC, and significantly improves sigmoid evaluation. Prone distention was the worst, particularly as BMI increased. Routine supine and decubitus positioning should be considered for standard CTC protocols, particularly in obese individuals. Automated volumetric analysis provides for rapid objective assessment of colonic distention.
Introduction
Adequate luminal distention at CT colonography (CTC) is critical for CTC for diagnostic evaluation. Poor distention can render both excellent bowel preparation and robust CTC software moot, as lesion detection is compromised. Dual scanning in the supine and prone position was shown early on to provide for complementary evaluation at CTC, with improved polyp detection rates.1-4 As such, a combined supine-prone protocol has long served as the standard approach for performing CTC. With the use of manual room air, the prone position will generally provide better distention, whereas the supine is typically better when using automated carbon dioxide (CO2).5 In general, automated continuous low-pressure CO2 is now preferred over room air, as it provides for better overall distention, easier administration, an improved safety profile, and reduced post-procedural discomfort.6-9 For cases where inadequate distention affects the same colonic segment or focal area, a third series is generally advocated. This typically consists of a right lateral decubitus series for inadequate sigmoid evaluation.5,9,10 The rate of obtaining an additional decubitus series averages about 10% but can vary widely from 5% to 30% depending on the specific patient cohort.10 In patients for whom assuming the prone position is either difficult or impossible, a decubitus series is considered an acceptable substitute and is performed in conjunction with the supine series.11-13
Anecdotally, we have noted in our practice that when all three position positions are acquired (ie, supine, prone, and decubitus), the decubitus series seems to provide the best overall distention in most cases. If the decubitus position can be shown to provide significantly better luminal distention compared with the prone position on a consistent basis, it should perhaps replace it as a standard acquisition. We now have access to a novel automated CTC tool that can provide volumetric quantification of colonic gas and fluid, which allows for a more objective assessment of luminal distention in addition to the traditional subjective reader scoring by segment. The purpose of this study was to compare total colonic gas volume and segmental luminal distention according to patient position at CTC, and determine which two views should perhaps constitute the routine protocol.
Materials and Methods
Study Group
This retrospective study complied with the Health Insurance and Portability and Accountability Act and was approved by our institutional review board; the need for informed consent was waived. From a consecutive series of 1,823 CTC examinations performed at our medical center over an 18-month period (over 90% of cases as part of the screening program), we identified 146 cases where a supine, prone, and right lateral decubitus series were sequentially obtained (see specific distention technique below). Mean patient age was 59.2 years, with 65 women and 81 men. Mean patient body mass index (BMI) was 30.9 kg/m2 (range, 17.4-50.9 kg/m2). All patients underwent cathartic bowel preparation plus oral contrast for tagging the day before CTC examination.
CTC Distention Technique
All examinations, including distention, scanning, and quality assurance steps, are performed by CT technologists experienced in CTC. Colonic distention with CO2 was achieved using a standard automated device (PROTOCO2L, Bracco Diagnostics). We do not employ spasmolytics. With the patient in the left lateral decubitus position, a small flexible rectal catheter is placed and an initial volume of 1–1.5 L of CO2 is instilled. To minimize transient discomfort related to the rectal distention, the equilibrium pressure is initially set at approximately 17-20 mm Hg and slowly increased to 25 mm Hg over the course of the examination. The patient is initially placed in the left lateral decubitus position until a total of approximately 2.5 L of CO2 has been delivered, rolled to a right lateral decubitus position for another 10.-1.5 L of CO2, and finally placed in the supine position until steady-state equilibrium has been reached. A scout view is obtained, followed by the full supine acquisition during end-expiration if distention appears to be adequate. The patient is then placed prone and repeat scanning occurs once equilibrium pressures are again observed. Care is taken to ensure active replacement of CO2 as needed during scanning.
Our CT technologists are trained to recognize inadequate distention, via immediate review of supine and prone 2D images at the console. The decision to perform a right lateral decubitus series is typically based on the presence of focal luminal collapse or near-collapse involving the same portion of the sigmoid or descending colon. The decision is usually made by the CT technologist, but the radiologist assigned to CTC that morning will occasionally be consulted. Because the left colon (sigmoid and descending) account for the vast majority of our cases with inadequate distention leading to a third series, we most often perform this in the right lateral decubitus position. Cases where a left lateral decubitus position was obtained were excluded from the study cohort.
CTC Acquisition Protocol
During the study period, CT Image acquisition was performed with 16- and 64-channel multi-detector CT scanners (GE Healthcare, Waukesha, WI). Scanning technique consisted of 1.25 mm collimation, 1 mm reconstruction interval, 120 kVp, and tube current modulation (noise index set at 50, 30-300 mA range).
Data Collection and Analysis
The total colonic gas volume for each patient position was derived using an automated tool available on a beta version of our CTC software (V3D Colon; Viatronix, Stony Brook, NY). This novel tool automatically segments and analyzes the colonic luminal gas and contrast-tagged fluid, providing the total volume of each, as well as the mean attenuation of the fluid.. Luminal fluid volumes and density were not of specific interest in this particular study but would be relevant when assessing the quality of bowel preparation. Furthermore, the residual fluid remains essentially static between the series. To complement the objective volumetric assessment, two radiologists independently scored luminal distention for each colonic segment on all three series for each case. An established 4-point scale was utilized,8 whereby a score of 4 signifies “optimal” luminal distention, a score of 3 signifies “adequate” distention, 2 signifies “inadequate” distention, and 1 signifies an area of focal collapse. Each segment was scored according to the worst area of distention within that segment. To allow for greater distinction between degrees of distention, 0.5-point increments between points were allowed.
Numerical variables were summarized with mean, SD (standard deviation), quartiles, and range; frequency count and percentages were used to summarize categorical variables. Friedman's test was used to test for positional differences in gas volume. Fisher's test was used to assess for positional differences in percent inadequate scores; separate analyses were done for each reader. Pearson correlations were obtained and tested with Fisher's z transform. P < 0.05 (two-sided) was the criterion for statistical significance. Statistical computations were obtained in R 3.0.1 (R Development Core Team 2013).
Results
Large differences were observed in the colonic gas volumes between the three patient positions at CTC, which was usually visually obvious (Figures 1 and 2). Mean gas volume (±SD) for supine, prone, and decubitus positioning was 1,617 ± 567 ml, 1441 ± 505 ml, and 1901 ± 627 ml, respectively (p<0.001) (Figure 3A). The right lateral decubitus series had the highest volume of the three positions in 73.3% (107 of 146 cases) and had the lowest volume in 6.2% (9 of 146 cases). In contrast, the prone series had the highest colonic volume of the three series in 0.7% (1 of 146 cases) and lowest volume in 73.3% (107 of 146 cases). The supine colonic gas volumes were intermediate between the decubitus and prone volumes, with the highest volume in 26.0% (38 of 146) and lowest in 20.5% (30 of 146). In terms of a typical CTC protocol where two views are standard, the decubitus series was one of the two best-distended views in 94% of all cases, the supine was among the two best in 79%, and the prone series was one of the two best in 27%.
Figure 1.
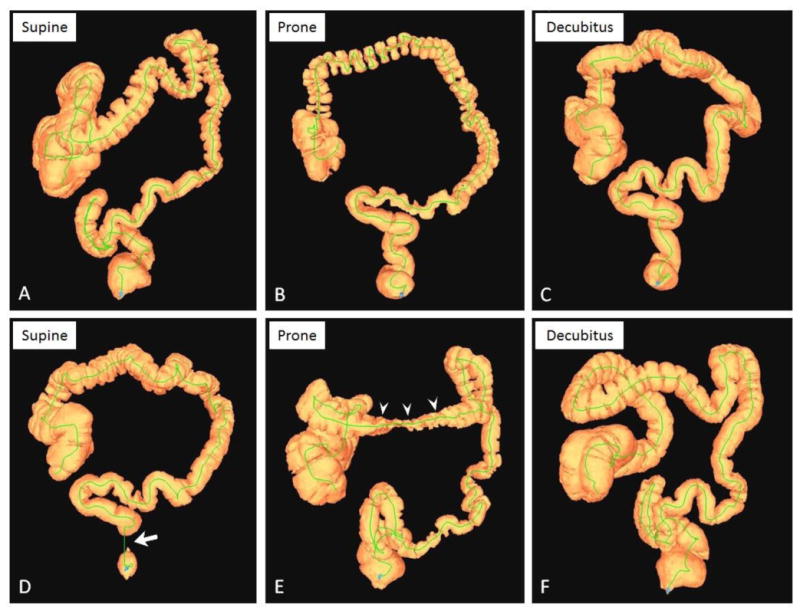
3D colon maps from CTC in two patients showing typical distention patterns.
A-C, CTC 3D colon maps from a 67-year-old man show intermediate/adequate distention in the supine position (A, colonic gas volume = 1429 ml), poor/inadequate distention in the prone position (B, gas volume = 973 ml), and optimal distention in the right lateral decubitus position (C, volume = 1963 ml). D-F, CTC 3D maps from a 51-year-old woman in the supine (D), prone (E), and decubitus (F) positions with colonic gas volumes of 1835 ml, 1639 ml, and 2452 ml, respectively. Note typical areas of inadequate distention in the rectum on supine (D, arrow) and transverse colon on prone (E, arrowheads), both of which are much better distended on the decubitus series (F).
Figure 2.
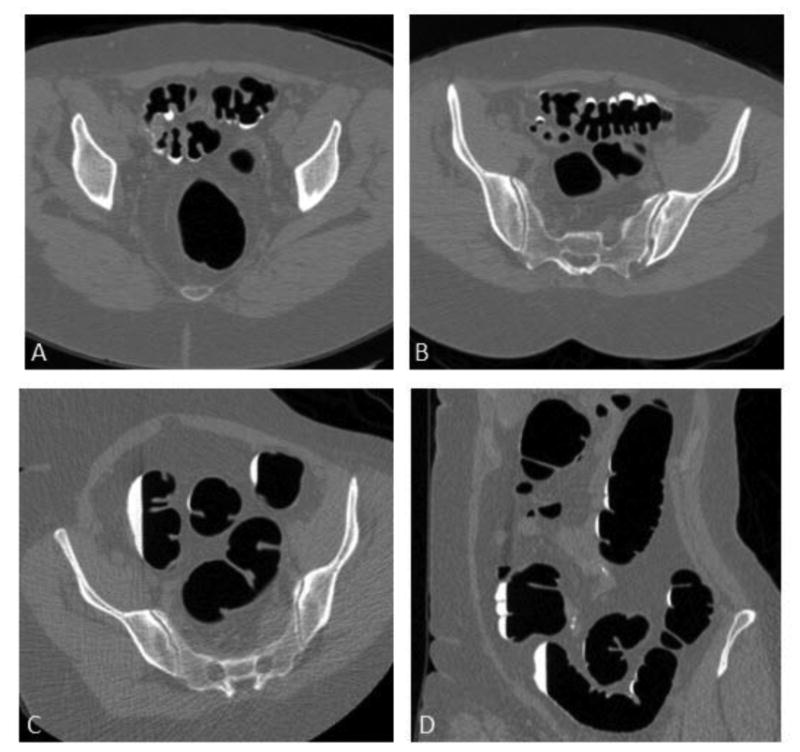
2D images from CTC examination in 65-year-old woman.
Transverse 2D CTC images from supine (A), prone (B), and right lateral decubitus (C) series show improved distention on the decubitus series. Coronal 2D decubitus image (D) also depicts excellent distention. Resolution of luminal narrowing and crowding of colonic folds greatly simplifies evaluation on both 2D and 3D views. Colonic gas volumes in supine, prone, and decubitus were 1388 ml, 1382 ml, and 2141 ml, respectively.
Figure 3.
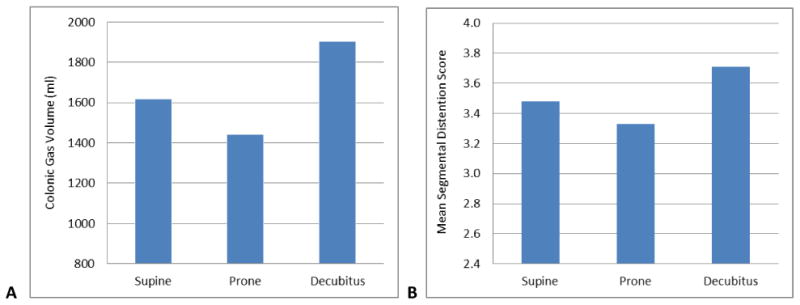
Colonic distention according to patient position in 146 subjects.
A, Bar graph shows mean colonic gas volume, which was greatest in the decubitus position (1901±627 ml), intermediate in the supine position (1,617±567 ml), and lowest in the prone position (1441±505 ml) (p< 0.0001).
B, Bar graph shows the mean overall segmental distention scores by position, pooled between the two readers, which match well with the automated volumetric results (p<0.001).
The mean pooled segmental distention reader scores summed over all six segments for the supine, prone, and decubitus positions were 3.48, 3.33, and 3.71, respectively (Figure 3B), with higher scores reflecting better distention (p<0.001). These subjective reader scores matched well with automated volumetric results (Figure 3). Pooled distention scores by segment for each position are shown in Figure 4. The only pooled segmental scores that were below 3.0 on average was for the sigmoid colon on both supine (mean score, 2.68) and prone (mean score, 2.58) positions, compared with a mean score of 3.23 for the right lateral decubitus series (p<0.001). The rectum was the only segment where the prone did not have the worst mean distention score, as supine distention was worse for this segment (Fig 4). Between the two readers, 10.4% of segments (182 of 1752 pooled segments) were either inadequate or collapsed on the supine series (pooled score ≥3.0), 12.1% (212 of 1752) were inadequate or collapsed on the prone series, and 4.2% (73 of 1752) were inadequate of collapsed on the decubitus series (p<0.001 for each reader). For the sigmoid colon, which is the most problematic segment, the overall percentage of inadequate or collapsed segments for the supine, prone, and decubitus series was 34.9% (102 of 292), 36.0% (105 of 292), and 17.5% (51 of 292), respectively (p?).
Figure 4.
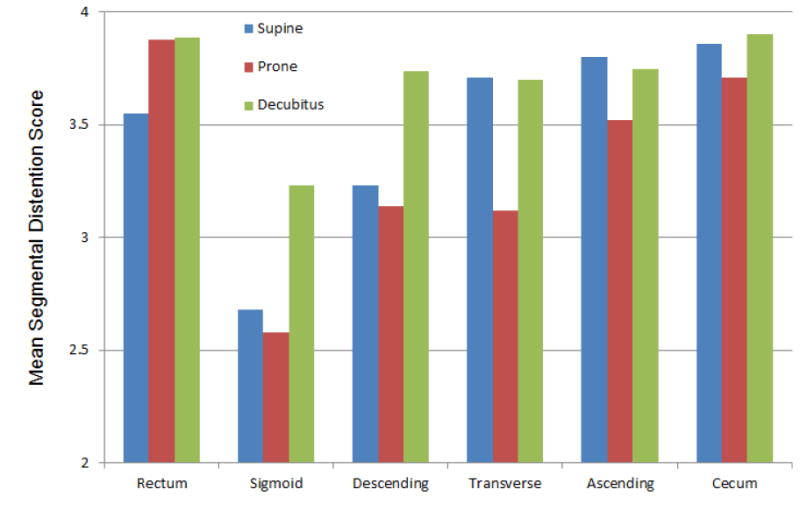
Mean segmental distention scores by colonic segment for each patient position.
Pooled scores from the two readers show that the prone position (red) yields the worst distention on average (higher scores) for all segments except for the rectum, where the supine (blue) is worst. The right lateral decubitus position (green) consistently provides the best distention throughout the colon (p<0.001).
Patient BMI was negatively correlated with colonic gas volume for each position: r= -0.076 in decubitus, -0.226 in prone, and -0.107 in the supine position (p < 0.024). However, when considering decubitus and supine colonic gas volume as a percentage difference compared with prone volume, the relative improvement in colonic distention over the prone position increased with BMI increases for both supine (0.213; p<0.001) and decubitus (0.280; p<0.001) positions. These correlations are plotted in Figure 5.
Figure 5.
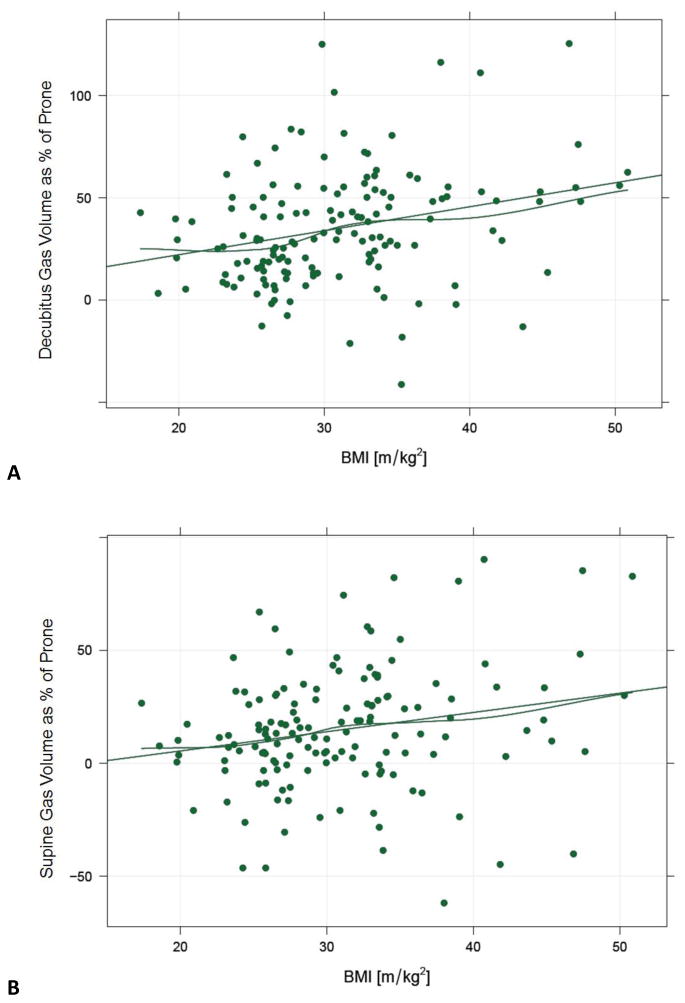
Correlation between colonic distention by position and patient BMI.
Graphs depicting decubitus (A) and supine (B) gas volume as a percentage difference compared with the prone volume, plotted against BMI. Values above zero indicate a higher volume than the prone scan. As BMI increases, the degree of improvement in decubitus and supine distention increases further. Correlations are 0.280 (p<0.001) and 0.213 (p<0.001), respectively. The straight lines represent the least squares fit and the wavy lines apply a local smoother. In general, the percentage increase in distention is greater in the decubitus position at all BMI values.
Discussion
With the use of an automated tool that rapidly and objectively determines colonic gas volume at CTC, we have shown that luminal distention with CO2 in the right lateral decubitus position was clearly superior to the standard supine and prone positions in this cohort. This automated volumetric assessment matched well with the overall findings from the more standard segmental scoring by radiologists. Furthermore, because luminal distention in the prone position lags behind that of the supine position with CO2, consideration for a standard supine-decubitus CTC scanning protocol is warranted, especially for more obese individuals. In particular, this approach could significantly improve distention and evaluation of the sigmoid colon, which represents a singular challenge for CTC.
It is important to note that our findings specifically apply to colonic distention with automated continuous low-pressure CO2 delivery. With the use of manual room air, the relative superiority between supine and prone actually reverses, and the impact on the decubitus view is not well established. Michel et al5 reported that the prone view was superior to the supine view in the majority of cases with manual room air insufflation in a simple but large subjective reader study, whereas with automated CO2, the situation was reversed with supine being superior, which matches our current findings. There was no available comparison with the decubitus view in the series by Michel et al. Possible explanations for these supine-prone observations include the relative differences in colonic absorption and intraluminal pressures between the two distention techniques. Because room air is essentially not absorbed through the colonic wall, continued insufflation from supine to prone would be expected to increase overall luminal volume (as would a subsequent decubitus series). In addition, because there are no pressure safeguards with room air, the increased intraluminal pressures that are possible may resist partial luminal collapse related to surrounding patient girth. The impact of body habitus on luminal distention with low pressure CO2 is most pronounced in (morbid) obesity, which explains why distention relative to prone improves on decubitus and, to a lesser extent, supine positioning with increasing BMI. The fact that the prone position fares so poorly with CO2 argues against the sequential ordering as a possible explanation for why the decubitus is most voluminous.
Although the distention data from our study strongly support changing practice by replacing the prone series with a right lateral decubitus series as standard protocol, there are issues related to such a switch that should be carefully considered. The shifting of luminal fluid between the opposed supine and prone position is much more complementary than a supine-decubitus combination, where polyps would be more likely to be submerged on both views. Even with fluid tagging, submerged polyps remain a pitfall at CTC, particularly on the 3D view.14,15 The ability to distinguish pedunculated polyps from mobile debris might also be more difficult with only a 90-degree positional rotation. In addition, patient anatomy tends to appear somewhat more distorted in a lateral decubitus position. Given the high degree of dose reduction now possible with the recently developed iterative reconstruction techniques,16-18 one could even argue that the concern related to obtaining an additional sub-mSv series is moot.
There are, however, other potential benefits to employing a supine-decubitus CT standard beyond improve distention and lesion detection alone. A lateral decubitus position is much more comfortable and feasible for obese or otherwise debilitated patients, and would presumably increase patient acceptance. Gryspeerdt et al13 found that there were fewer breathing artifacts with a lateral decubitus position compared with prone, especially in the elderly. The examination would also be easier for CT technologists to conduct and may reduce its duration. Finally, if the supine-decubitus combination were to reduce the need for a third series, overall patient dose would also decrease accordingly.
There have been previous efforts to provide automated assessment of colonic distention at CTC.19-21 To our knowledge, prior attempts have provided primarily linear diameter assessment and not a true volumetric analysis. Volume data are objective, more robust, likely less error prone, and also amplify true differences compared with linear measures. Volumetric assessment in our study matched well with the more subjective reader distention scores, which are considerably more labor intensive. This automated QA tool has other potential uses. For example, we are currently investigating its use for assessing bowel prep fidelity by measuring residual fluid volumes and density. This may be an effective means for comparing the performance of different bowel preps at CTC.
We acknowledge limitations to our study. By definition, we only included CTC examinations where all three series were obtained, which may introduce a selection bias since the supine and prone views were already considered suboptimal in some way. Therefore, the improvement in distention on the decubitus series may not be as severe for cases where supine and prone distention are excellent. We did not alter the temporal sequence for obtaining each series, as each was performed in a supine-prone-decubitus order. Although this may affect the overall results, the fact that the second series (prone) was the worst and the third series (decubitus) was best argues against a strong temporal bias. We did not assess the effect of luminal distention upon lesion detection, but this has been repeatedly shown in earlier CTC studies. 1-4 Finally, the automated volumetric tool we utilized does not provide segmental data and cannot identify areas of inadequate distention. Rather, it rapidly and objectively provides total colonic volume data as an overall assessment.
In summary, we have found that the right lateral decubitus position consistently yields the best overall colonic distention at CTC, and significantly improves sigmoid evaluation. Colonic distention tends to be worst in the prone position. Our findings support the use of right lateral decubitus positioning for routine CTC, in conjunction with the supine position, to optimize colonic distention for lesion detection. Automated volumetric analysis provides for rapid objective assessment of colonic distention.
References
- 1.Chen SC, Lu DSK, Hecht JR, Kadell BM. CT colonography: Value of scanning in both the supine and prone positions. American Journal of Roentgenology. 1999;172:595–9. doi: 10.2214/ajr.172.3.10063842. [DOI] [PubMed] [Google Scholar]
- 2.Morrin MM, Farrell RJ, Keogan MT, Kruskal JB, Yam CS, Raptopoulos V. CT colonography: colonic distention improved by dual positioning but not intravenous glucagon. European Radiology. 2002;12:525–30. doi: 10.1007/s003300100954. [DOI] [PubMed] [Google Scholar]
- 3.Yee J, Kumar NN, Hung RK, Akerkar GA, Kumar PR, Wall SD. Comparison of supine and prone scanning separately and in combination at CT colonography. Radiology. 2003;226:653–61. doi: 10.1148/radiol.2263010701. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher JG, Johnson CD, Welch TJ, et al. Optimization of CT colonography technique: Prospective trial in 180 patients. Radiology. 2000;216:704–11. doi: 10.1148/radiology.216.3.r00au41704. [DOI] [PubMed] [Google Scholar]
- 5.Michel SJ, Pickhardt PJ, Kim DH, Taylor AJ. Effect of colonic distention on superiority of supine versus prone views in screening computed tomographic colonography. Clin Imaging. 2007;31:325–8. doi: 10.1016/j.clinimag.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Burling D, Taylor SA, Halligan S, et al. Automated insufflation of carbon dioxide for MDCT colonography: Distension and patient experience compared with manual insufflation. American Journal of Roentgenology. 2006;186:96–103. doi: 10.2214/AJR.04.1506. [DOI] [PubMed] [Google Scholar]
- 7.Pickhardt PJ. Incidence of colonic perforation at CT colonography: Review of existing data and implications for screening of asymptomatic adults. Radiology. 2006;239:313–6. doi: 10.1148/radiol.2392052002. [DOI] [PubMed] [Google Scholar]
- 8.Shinners TJ, Pickhardt PJ, Taylor AJ, Jones DA, Olsen CH. Patient-controlled room air insufflation versus automated carbon dioxide delivery for CT colonography. American Journal of Roentgenology. 2006;186:1491–6. doi: 10.2214/AJR.05.0416. [DOI] [PubMed] [Google Scholar]
- 9.Pickhardt PJ. Screening CT colonography: how I do it. AJR Am J Roentgenol. 2007;189:290–8. doi: 10.2214/AJR.07.2136. [DOI] [PubMed] [Google Scholar]
- 10.Buchach CM, Kim DH, Pickhardt PJ. Performing an additional decubitus series at CT colonography. Abdominal Imaging. 2011;36:538–44. doi: 10.1007/s00261-010-9666-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neri E, Halligan S, Hellstrom M, et al. The second ESGAR consensus statement on CT colonography. European Radiology. 2013;23:720–9. doi: 10.1007/s00330-012-2632-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McFarland EG, Fletcher JG, Pickhardt P, et al. ACR Colon Cancer Committee white paper: status of CT colonography 2009. J Am Coll Radiol. 2009;6:756–72.e4. doi: 10.1016/j.jacr.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Gryspeerdt SS, Herman MJ, Baekelandt MA, van Holsbeeck BG, Lefere PA. Supine/left decubitus scanning: a valuable alternative to supine/prone scanning in CT colonography. European Radiology. 2004;14:768–77. doi: 10.1007/s00330-004-2264-x. [DOI] [PubMed] [Google Scholar]
- 14.Pickhardt PJ, Choi JHR. Electronic cleansing and stool tagging in CT colonography: Advantages and pitfalls with primary three-dimensional evaluation. American Journal of Roentgenology. 2003;181:799–805. doi: 10.2214/ajr.181.3.1810799. [DOI] [PubMed] [Google Scholar]
- 15.Pickhardt PJ, Kim DH. CT Colonography: Pitfalls in Interpretation. Radiologic Clinics of North America. 2013;51:69–88. doi: 10.1016/j.rcl.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fletcher JG, Grant KL, Fidler JL, et al. Validation of Dual-Source Single-Tube Reconstruction as a Method to Obtain Half-Dose Images to Evaluate Radiation Dose and Noise Reduction: Phantom and Human Assessment Using CT Colonography and Sinogram-Affirmed Iterative Reconstruction (SAFIRE) J Comput Assist Tomogr. 2012;36:560–9. doi: 10.1097/RCT.0b013e318263cc1b. [DOI] [PubMed] [Google Scholar]
- 17.Flicek KT, Hara AK, Silva AC, Wu Q, Peter MB, Johnson CD. Reducing the radiation dose for CT colonography using adaptive statistical iterative reconstruction: A pilot study. AJR Am J Roentgenol. 2010;195:126–31. doi: 10.2214/AJR.09.3855. [DOI] [PubMed] [Google Scholar]
- 18.Pickhardt PJ, Lubner MG, Kim DH, et al. Abdominal CT With Model-Based Iterative Reconstruction (MBIR): Initial Results of a Prospective Trial Comparing Ultralow-Dose With Standard-Dose Imaging. Am J Roentgenol. 2012;199:1266–74. doi: 10.2214/AJR.12.9382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deshpande KK, Summers RM, Van Uitert RL, et al. Quality assessment for CT colonography: Validation of automated measurement of colonic distention and residual fluid. American Journal of Roentgenology. 2007;189:1457–63. doi: 10.2214/AJR.07.2327. [DOI] [PubMed] [Google Scholar]
- 20.Van Uitert RL, Summers RM, White JM, Deshpande KK, Choi JR, Pickhardt PJ. Temporal and multiinstitutional quality assessment of CT colonography. AJR Am J Roentgenol. 2008;191:1503–8. doi: 10.2214/AJR.07.3591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hung PW, Paik DS, Napel S, et al. Quantification of distention in CT colonography: Development and validation of three computer algorithms. Radiology. 2002;222:543–54. doi: 10.1148/radiol.2222010600. [DOI] [PubMed] [Google Scholar]


