Abstract
Superficial mycoses are fungal infections restricted to the stratum corneum and to the hair shafts, with no penetration in the epidermis; they are: white piedra, black piedra, tinea versicolor, and tinea nigra. This study presents images of mycological tests performed in the laboratory, as well as exams performed at the authors office, in order to improve the dermatologist's knowledge about the diagnosis of these dermatoses, which are common in many countries.
Keywords: Culture, Culture media, Dermoscopy, Malassezia, Mycology, Mycoses, Physical examination, Phaeohyphomycosis, Piedra, Tinea, Tinea versicolor
Skin mycoses are frequent causes of dermatological medical appointments in Brazil, whether in public or private healthcare services.1 These are fungal infections that affect superficial layers of the skin, hair, and nails, and may be clinically classified as superficial mycoses or deep mycoses. Superficial mycoses are divided into actual superficial mycoses, superficial cutaneous mycoses, and superficial cutaneous-mucosal mycoses.2,3
Actual superficial mycoses are fungal infections of the corneum layer or hair cuticle, in which the host's cell-mediated immune response is minimal or absent. The presence of fungus is rarely symptomatic, which makes infection chronic. They are: white piedra, black piedra, tinea nigra, and pityriasis versicolor. 2,4,5
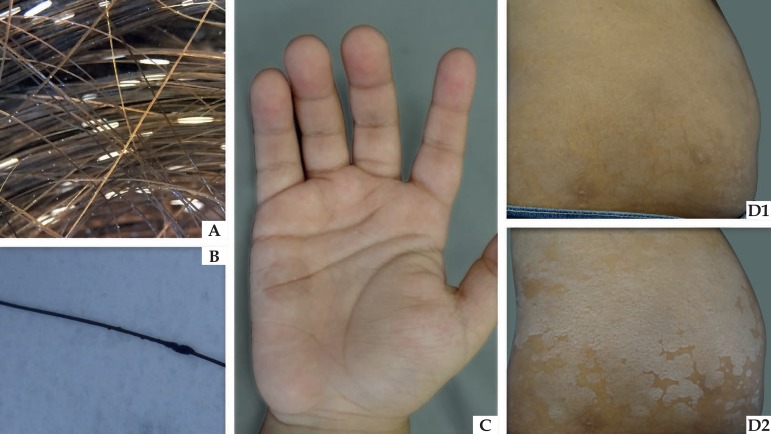
White piedra is a dermatosis caused by the yeasts of the Trichosporon sp: T. beigelii, T. asahii, T. ovoides, T. inkin, T. mucoides, T. asteroides and T. cutaneum genuses; it is clinically characterized by soft, whitish nodules attached to the hair cuticle, varying in color from white to light brown.2,4,5Black piedra, caused by the dematiaceous filamentous fungus Piedraia hortae, consists of black-colored, firm, irregular nodules, also located in the hair cuticle.2,4,5 Tinea nigra, caused by a distinct dematiaceous filamentous fungus, Hortaea werneckii, affects the corneum layer, especially of palmoplantar regions in children, producing an asymptomatic brownish macula.2,4,5 Pityriasis versicolor (PV) is caused by the yeasts of the Malassezia sp. : M. furfur, M. sympodialis, M. globosa, M. slooffiae, M. restricta and M. obtusa genuses. 5 It is characterized by multiple scaling macular lesions, whose colors vary from white to brownish (Figure 1).2,4,5,6
Figure 1.
Clinical appearance of actual superficial mycoses. (A) White piedra: whitish nodule attached to the hair shaft. (B) Black piedra: darkened nodule attached to the hair shaft. (C) Tinea nigra: brownish macula on children’s palms. (D) Pityriasis versicolor: scattered maculas on the abdomen (D1), which become more evident after skin stretching (Zireli’s sign – D2)
As these are mycoses, the gold standard for their diagnosis is the identification of fungal agents by means of direct mycological examination (DME), viewed under an optical microscope, associated with the agent's isolation in a fungus culture, with a macroscopic and microscopic mycelium analysis.
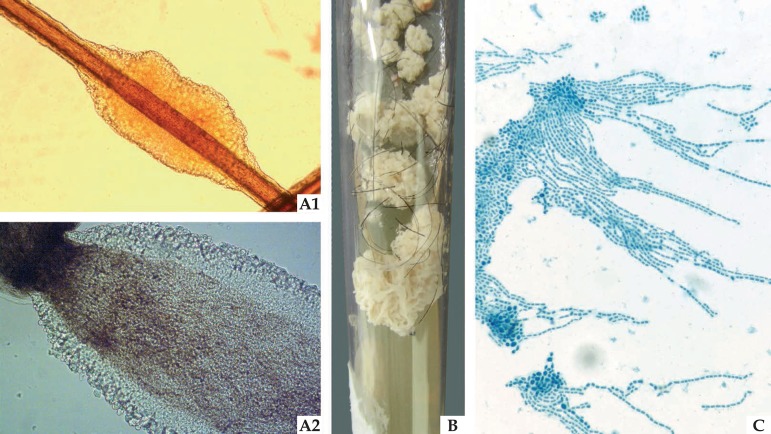
In white piedra, DME reveals hyaline nodules consisting of arthroconidia and some blastoconidia. The culture is white-yellowish yeast-like, with a cerebriform aspect. In micromorphology, it is possible to view rectangular, oval, or round arthroconidia, as well as the presence of blastoconidia (Figure 2).2,4,5
Figure 2.
Mycological examinations of white piedra: (A1) Optical microscopy (x40) offering a detailed illustration of the light color nodule attached to the pillar shaft. (A2) Optical microscopy (x100) illustrates the yeasts the make up the structure on the edge of the nodule. (B) Culture Mycosel medium (Difco, USA) with yeast-like colony, with the cerebriform filamentous appearance. (C) Microgrowth demonstrates yeasts with blasto-arthrospores, typical of Trichosporon sp
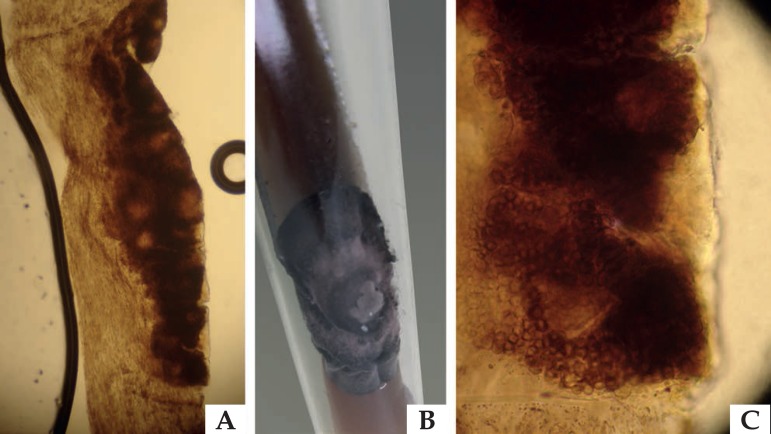
In black piedra, DME reveals dark nodules attached to the shaft, containing several ascus, with two to eight fusiform, curved ascospores. The culture is dark, and its growth is slow (Figure 3).2,4,5
Figure 3.
Mycological examinations of black piedra: (A) Optical microscopy (x40) offering a detailed illustration of the dark nodule attached to the pillar shaft. (B) Culture Mycosel medium (Difco, USA) with dematiaceous colony. (C) Optical microscopy (x100) identifying the ascus, round structures typical of parasitism caused by Piedraia hortae
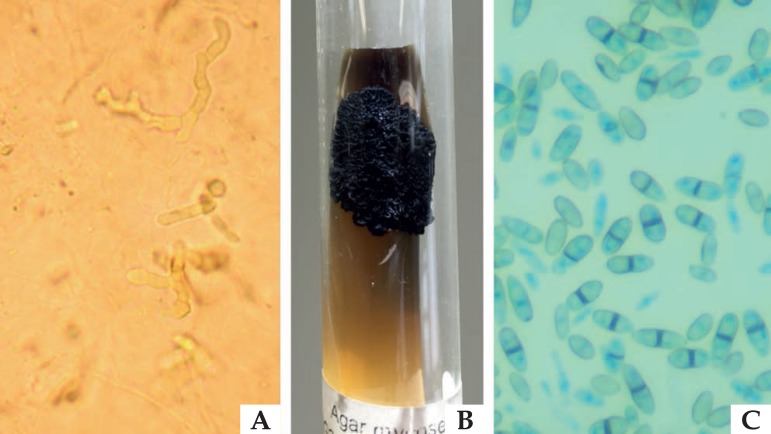
In tinea nigra, DME reveals dematiaceous septate hyphae, with a waxy culture, whose colors vary from greenish brown to black. Its microgrowth reveals yeast-like cells with binary fission (Figure 4).2,4,5
Figure 4.
Mycological examinations for tinea nigra: (A) Direct mycological examination of a sample collected through skin lesion scraping, clarified with KOH 10%, illustrating dematiaceous septate hyphae. (B) Culture Mycosel medium (Difco, USA) with dematiaceous colony with a waxy appearance. (C) Microgrowth revealing dematiaceous yeasts with binary fission, typical of Hortaea werneckii
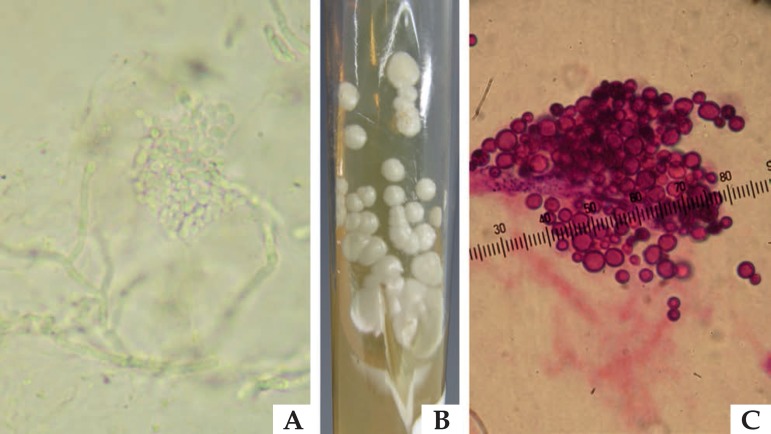
In pityriasis versicolor, DME consists of yeast-like cells, grouped in a "grape bunch" format, and of short and thick pseudo-hyphae. The culture medium, enriched with olive oil or ox bile, forms a white-yellowish yeast-like colony. Microgrowth identifies yeast-like cells with thin base single budding (Figure 5).2,4,5
Figure 5.
Mycological examinations for pityriasis versicolor: (A) Direct mycological examination of a sample collected through skin lesion scraping, clarified with KOH 10%, illustrating yeasts grouped in a “grape bunch” format, and of short and thick pseudo-hyphae. (B) Sabouraud agar culture, enriched with olive oil, with beige yeast-like colony. (C) Yeasts grouped with short base single budding, with “bowling pin” appearance, stained by the hematoxylin eosin method, typical of Malassezia sp microgrowth
However, not all dermatologists have access to diagnosis laboratories that offer such mycological examinations. Therefore, knowing the most accessible propedeutics and complementary methods to confirm the diagnosis is of great assistance. Among these propedeutic methods, Zireli's sign is of utmost importance for PV, in which the stretching of the affected skin may facilitate one's view of the lesion as it highlights the corneum layers that have been parasitized by Malassezia sp. in its pathogenic form6 (Figure 01 and Video 01).
Video 1.
Zireli's propedeutic maneuver: skin stretching causing detachment of corneum scales, which better illustrate pityriasis versicolor areas (Avaliable online)
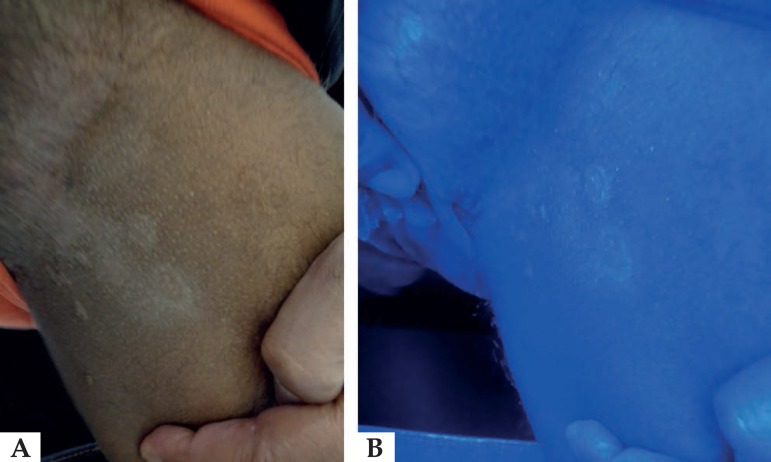
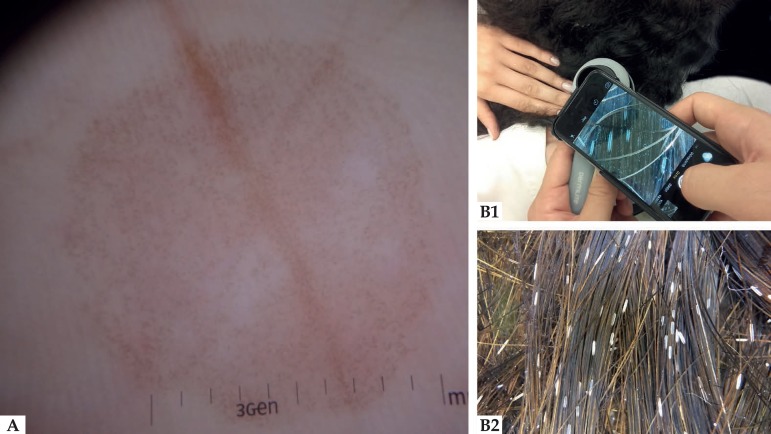
By using equipment available in medical offices, such as a wood lamp and a dermatoscope, it is also possible to increase diagnostic accuracy of lesions: in PV, irradiated skin may reveal yellowish or silver fluorescence, if caused by the Malassezia furfur species, which enables one to see the extent of the affected skin; dermatoscopy of tinea nigra reveals a non-melanocytic pattern macular lesion, with superficial chestnut-brown speckled pigmentation, with no prevalence of grooves or crests (Figure 6 and 7).7,8 Dermatoscopy of piedras is similar to the images obtained in direct examinations, but these present a weaker definition when compared to the images obtained in the optical microscope. Nevertheless, they are also very useful (Figure 7). With the dermatoscope, it is possible, for instance, to distinguish white piedra nodules from pediculosis induced nits.9
Figure 6.
Patient exhibiting pityriasis versicolor lesions in the inguinal region (A), under Wood lamp, reveals silver fluorescence (B)
Figure 7.
Dermatoscopy of tinea nigra palmar lesion under polarized light (A) and polarized light dermatoscopy performed on child with whitish nodules attached to the hair (B1), illustrating structures that are similar to those viewed in optical microscopy (B2)
Actual superficial mycoses are dermatoses that commonly appear in several countries. Knowledge of their clinical aspects, mycological examinations, and complementary methods aid dermatologists in their routine practice.
Footnotes
Conflict of interest: None
Work conducted at the Dermatology Clinic, Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil.
Financial support: none.
REFERENCES
- 1.Sociedade Brasileira de Dermatologia Perfil nosológico das consultas dermatológicas no Brasil. An Bras Dermatol. 2006;81:549–558. [Google Scholar]
- 2.Zaitz C, Campbell I, Marques SA, Ruiz LRB, Framil VMS. Compêndio de Micologia Médica. 2.ed. Rio de Janeiro: Guanabara Koogan; 2010. [Google Scholar]
- 3.Odds FC, Arai T, Disalvo AF, Evans EG, Hay RJ, Randhawa HS, et al. Nomenclature of fungal diseases: a report and recomendations from a Sub-Committee of the International Society for Human and Animal Mycology (ISHAM) J Med Vet Mycol. 1992;30:1–10. doi: 10.1080/02681219280000021. [DOI] [PubMed] [Google Scholar]
- 4.Bonifaz A, Gómez-Daza F, Paredes V, Ponce RM. Tinea versicolor, tinea nigra, white piedra, and black piedra. Clin Dermatol. 2010;28:140–145. doi: 10.1016/j.clindermatol.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz RA. Superficial fungal infections. Lancet. 2004;364:1173–1182. doi: 10.1016/S0140-6736(04)17107-9. [DOI] [PubMed] [Google Scholar]
- 6.Framil VMS, Melhem MS, Szeszs MW, Zaitz C. New aspects in the clinical course of pityriasis versicolor. An Bras Dermatol. 2011 Nov-Dec;86(6):1135–1140. doi: 10.1590/s0365-05962011000600011. [DOI] [PubMed] [Google Scholar]
- 7.Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood's lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842–847. doi: 10.1111/jdv.12860. [DOI] [PubMed] [Google Scholar]
- 8.Darrigade AS, Saint-Marie D, Dufour J, Edouard S, Graille J, Cheuret M, et al. The value of dermoscopy in the diagnosis of tinea nigra. Ann Dermatol Venereol. 2014;141:167–169. doi: 10.1016/j.annder.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 9.Marques SA, Richini-Pereira VB, Camargo RM. White piedra and pediculosis capitis in the same patient. An Bras Dermatol. 2012;87:786–787. doi: 10.1590/s0365-05962012000500023. [DOI] [PubMed] [Google Scholar]