Dear Editor,
Hailey-Hailey disease, also called benign familial pemphigus, is an autosomal dominant disorder caused by mutations in the ATP2C1 gene. Positive family history is detected in two thirds of all cases. The prevalence is 1:50,000 and the incidence of sporadic mutations might be as high as 26%.1,2 We present a case of a patient who developed benign familial pemphigus in the seventh decade of life without any medical family history.
A 78-year-old white woman with hypertension and dyslipidemia presented with erythematous plaques in the groin with satellite pustules diagnosed as candidal intertrigo. The lesions had presented for 4 months and showed no improvement under topical and oral antifungal treatment (Figure 1). The patient reported severe itching. In two weeks' time, a new perineal erythema appeared with linear erosions and eczematous, circinate lesions with some flaccid vesicles involving her neck, back, and upper and lower extremities (Figure 2). The mucosal membranes were not involved. Blood test results were normal and cultures were negative. A punch biopsy of the perineal lesions was obtained and stained with hematoxylin-eosin and another punch was taken and studied through direct immunofluorescence. Indirect immunofluorescence was negative. Pathology data revealed hyperkeratosis and acanthosis with suprabasal acantholysis, which did not affect adnexal structures and resembled a "dilapidated brick wall" (Figure 3). Dyskeratotic keratinocytes were not observed. Direct immunofluorescence study showed no deposition of immunoreactants. These features were consistent with Hailey-Hailey's disease.
Figure 1.

Erythematous plaques with linear erosions
Figure 2.

Erythematous plaques and circinate lesions on the lower extremities
Figure 3.
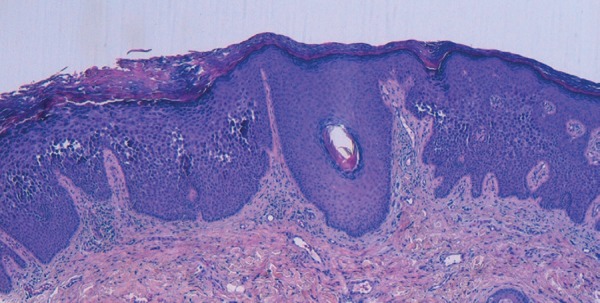
Acanthosis with suprabasal acantholysis. Dyskeratotic keratinocytes are not observed. Hematoxylin and eosin stain
Symptoms include erythematous plaques with blisters and fissures that appear predominantly in skin folds, sometimes with a circinate pattern. Many triggers have been identified (friction, perspiration, ultraviolet radiation). Most patients have worse symptoms during hot summer months when sweat and friction aggravate the eruption. Since the condition usually appears in the third or fourth decade, the onset of clinical manifestations in the seventh decade is uncommon. Lesion infection is the main problem because it causes pain, itching, and an unpleasant smell, with the associated adversity. White bands on the fingernails and pits on the palms can also occur. Dissemination or mucosal involvement is rare.
The diagnosis of Hailey-Hailey disease requires differentiation from other acantholytic dermatoses. Due to the localization of the lesions, differential diagnosis also includes candidal intertrigo, psoriasis inversa, and contact dermatitis. Although herpes simplex infection can mimic the vesicular lesions of Hailey-Hailey disease, Tzanck smear is useful to differentiate the diseases.3
There is no first-line treatment. However, wearing light and loose clothes to prevent sweating and friction is an important precaution. The most extended treatment includes topical and systemic antibiotics, topical and systemic corticosteroids, steroidsparing immunomodulators, botulinum toxin injections, retinoids, and dapsone. Although medical treatment is important in the control of disease exacerbations in Hailey-Hailey, many cases are recalcitrant, and medical therapy infrequently leads to prolonged remissions.
Carbon dioxide laser ablation is an option for recalcitrant Hailey-Hailey.4 If the disease causes extreme disability, surgery can be performed, with the use of grafts and flaps. Oxybutynin is an anti-muscarinic drug that was first associated with the resolution of hyperhidrosis in 1988. In our case, the patient made outstanding progress thanks to the administration of 5 mg/daily of this antiperspirant agent since sweat is one of the precipitating factors of new outbreaks.5
Footnotes
Conflict of interest: None.
Work performed at Hospital Universitari Sagrat Cor - Grupo Quirónsalud - Barcelona, Spain.
Financial support: None.
REFERENCES
- 1.Vasudevan B, Verma R, Badwal S, Neema S, Mitra D, Sethumadhavan T. Hailey-Hailey disease with skin lesions at unusual sites and a good response to acitretin. Indian J Dermatol Venereol Leprol. 2015;81:88–91. doi: 10.4103/0378-6323.148600. [DOI] [PubMed] [Google Scholar]
- 2.Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol. 1992;126:275–282. doi: 10.1111/j.1365-2133.1992.tb00658.x. [DOI] [PubMed] [Google Scholar]
- 3.Riahi RR, Yamazaki ML, Kelly BC. Tzanck smear utilized in the diagnosis of Hailey-Hailey disease mimicking genital herpes. Int J Dermatol. 2014;53:85–87. doi: 10.1111/j.1365-4632.2011.05423.x. [DOI] [PubMed] [Google Scholar]
- 4.Hochwalt PC, Christensen KN, Cantwell SR, Hocker TL, Otley CC, Brewer JD, et al. Carbon dioxide laser treatment for Hailey-Hailey disease: a retrospective chart review with patient-reported outcomes. Int J Dermatol. 2015;54:1309–1314. doi: 10.1111/ijd.12991. [DOI] [PubMed] [Google Scholar]
- 5.Kaniszewska M, Rovner R, Arshanapalli A, Tung R. The cutting edge: Oral glycopyrrolate for the treatment of Hailey-Hailey disease. JAMA Dermatol. 2015;151:328–329. doi: 10.1001/jamadermatol.2014.4578. [DOI] [PubMed] [Google Scholar]


