Abstract
Objective
This study tested the relationships among child executive function (EF), child-perceived parent fast food intake, and child self-reported subsequent consumption of high-calorie, low nutrient (HCLN) food.
Design
One year and 6-month longitudinal observation from larger randomized control trial
Setting
Southern California elementary schools
Subjects
Fourth and fifth grade children (n = 1,005) participating in the Pathways to Health obesity prevention program
Results
Child EF problems were associated with higher concurrent HCLN intake (B = 0.29, SE = 0.10, p < 0.001) and had a significant indirect effect through higher perceived frequency of parent fast food intake (indirect effect = 0.17, 95% CI = 0.11/0.25, p < 0.001). Longitudinally, child EF problems did not significantly predict higher HCLN intake a year and a half later (B = 0.01, SE = 0.10, p = 0.92, n = 848) but did have a significant indirect effect through higher perceived parent fast food intake (indirect effect = 0.05, 95% CI = 0.02/0.10, p < 0.001).
Conclusions
Children’s EF difficulties may increase their perception of parent concurrent fast food intake, contributing to their own unhealthy food intake. However, EF problems may not directly affect HCLN intake across time, except when problems are associated with child perception of more frequent parent consumption of convenience foods. Future research is needed to investigate the possibility that helping children perceive and understand role models’ convenience food consumption may improve child dietary consumption patterns.
Keywords: executive function, child obesity, social learning theory, high-calorie low-nutrient, snack foods
In 2009–2010, the prevalence of pediatric obesity in the United States was 16.9% (Ogden, Carroll, Kit, & Flegal, 2012). Obese children are at higher risk for metabolic syndrome, cardiovascular risk, insulin resistance syndrome, Type 2 diabetes, depression, and social stigma (Arslanian, 2002; Goran & Gower, 1998; Heuer, McClure, & Puhl, 2011; Keddie, 2011; Steinberger & Daniels, 2003; Weiss et al., 2004). Excessive intake of high-calorie foods such as sugar-sweetened beverages and fast food can contribute to energy imbalance, increasing obesity risk (Anderson & Butcher, 2006). Parents may affect child diet via food availability, modeling eating behaviors, and purchasing fast food meals, although study results are mixed (Boutelle, Fulkerson, Neumark-Sztainer, Story, & French, 2007; Campbell, Crawford, & Ball, 2006; Hendrie, Sohonpal, Lange, & Golley, 2013).
Social Learning Theory provides a framework to understand potential effects of parent behavior on child diet. According to Social Learning Theory, important persons such as parents and teachers influence children through modeling behavior (Bandura, 1977). Children observe others’ actions and rewards – observational learning – and may engage in those behaviors themselves (Bandura, 1977). Modeling could affect child intake of calorically-dense foods, or “high-calorie, low-nutrition/low-nutrient” (HCLN) foods (Bandini et al., 1999; Story, Sallis, & Orleans, 2009; Pentz, Spruijt-Metz, Chou, & Riggs, 2011). Supporting this interpretation, parents who model fruit and vegetable intake and regular physical activity typically have children with these diet and exercise patterns (Gross, Pollock, & Braun, 2010; Strauss, Rodzilsky, Burack, & Colin, 2001). In contrast, adult modeling of fast food consumption and provision of fast food meals is associated with child sugar-sweetened beverage consumption and obesity (Anderson, Rafferty, Lyon-Callo, Fussman, & Imes, 2011; Schroder, Fito, Covas, & Investigators, 2007; Lopez et al., 2012).
Child perception of modeled behavior is a crucial component of observational learning. Thus, cognitive factors that compromise accurate perception may alter what is learned. Executive Function (EF) is a set of psychological processes that could potentially influence the observational learning process. EF is the set of psychological processes that guide self-regulation, goal-oriented problem-solving, planning, and emotion regulation (Alvarez & Emory, 2006; Hongwanishkul, Happaney, Lee, & Zelazo, 2005; Zelazo, Carter, Reznick, & Frye, 1997). Key EF components include attention, working memory, and inhibitory processes (Alvarez & Emory, 2006). EF skills include “cool” skills, or cognitive, evaluative processes, and “hot” skills, or those relating to emotional regulation (Hongwanishkul, Happaney, Lee, & Zelazo, 2005).
However, EF difficulties could compromise observational learning and affect what children learn from modeled eating behavior. Children with EF difficulties may misperceive or misunderstand parents’ unhealthy behavior. EF difficulties could hinder children’s ability to understand infrequently modeled behavior (such as an occasional fast food meal) as an “exception to the rule” rather than a new model to follow. While children across the EF range may find it difficult to understand parent fast food intake as undesirable, EF difficulties could intensify misunderstandings. If EF difficulties impair child perception and encoding of modeled behavior, their own eating behavior may become unhealthier.
In fact, one study shows that temporary, experimental impairment of EF leads to person perception that relies more on routinized processing than cognitive flexibility with real-time information (Macrae, Bodenhausen, Schloerscheidt, & Milne, 1999). Thus, children with EF difficulties could potentially process a parent’s occasional fast food meal as a routine action and new rule to follow. Consequently, the perceived rule of acceptable fast food consumption would be expected to change children’s own dietary behavior.
Indeed, recent research suggests that child EF is associated with patterns of food intake, physical activity, and other health behaviors. EF difficulties have been associated with obesity in both male and female adolescents, and high-calorie or fatty snack intake in children and adults (Cserjesi, Moinar, Luminet, & Lenardo, 2007; Hall, 2012; Lokken, Boeka, Austin, Gunstad, & Harmon, 2009; Mond, Stich, Hay, Kraemer, & Baune, 2007; Riggs et al., 2010a; Smith, Hay, Campbell, & Trollor, 2011; Verdejo-Garcia et al., 2010). In contrast, EF proficiency has been associated with greater fruit and vegetable consumption and physical activity in adolescents (ex., Riggs, Mesirov, Shin, & Pentz, 2009).
Current Study
However, to our knowledge, no studies have examined the effect of EF on perceived parent dietary behavior and child consumption. This study tested whether child-perceived parent fast food intake mediated the relationship between child EF and child HCLN intake. We hypothesized that child-perceived parent fast food intake would mediate the relationship between child EF and HCLN, and we tested this hypothesis with (a) cross-sectional data and (b) data collected 1.5 years after the original assessment.
Method
Participants
Data came from students participating in the Pathways to Health (Pathways) school-based obesity prevention program, which is delivered by teachers and designed to improve executive function skills, healthy eating, and physical activity, by teaching affect regulation, impulse control, and decision-making skills (Riggs, Sakuma, & Pentz, 2007). Participants were students from 4th grade in 82 classrooms across 28 Southern California elementary schools (Riggs, Sakuma, & Pentz, 2007). Of the 1,587 participants at baseline, 1,005 had full active consent and were tracked over time. Schools were randomized to intervention and control conditions. The sample was 30% Caucasian, 29% Latino, 8% Asian, 3% African American, 15% Bi-racial, and 16% Other. About half (51%) were female, and 25% received free or reduced-price lunch at school. Data were collected at: (a) baseline, at the beginning of spring semester of 4th grade (Time 1; M = 9.27 years; n = 1,005), (b) the end of the 4th grade year, about 6 months later (Time 2; M = 9.65 years; n = 998), and (c) the end of 5th grade, about 1 year and 6 months after baseline (Time 3; M = 10.70 years; n = 859). Details of recruitment and retention are described in Riggs et al. (2012).
Measures
At each of the three time points, participants completed a 45-minute paper-and-pencil assessment in their classrooms, with trained administrators available to answer questions. The survey contained the same measures across waves and was administered aloud. As with other school-based studies, (e.g., Gortmaker, Peterson, Wiecha, Sobol, Dixit, Fox, & Laird, 1999), the authors were constrained to one class period for administering the survey. Due to this constraint on survey length, the authors used abbreviated versions of scales, as described in Riggs, Chou, Spruijt-Metz, & Pentz, (2010) and Riggs, Spruijt-Metz, Sakuma, Chou, & Pentz (2010). Construction of abbreviated scales proceeded through extensive pilot testing where full scales of EF and food intake were reduced to index items representing the highest loading items for each scale (Riggs et al., 2010b). Prior research with these measures indicated acceptable reliability with this population that was comparable to full scales (Riggs et al., 2010a, 2010b). All procedures involving human subjects/patients were approved by [removed]. Parental written consent and child assent were obtained for all participants.
Executive Function
Items from four of eight clinical sub-scales of the Behavioral Rating Inventory of EF, Self-Report (Guy, Isquith, & Gioia, 2004) were included to assess EF. Emotional control is the ability to modulate behavior in the face of an emotional response (e.g., “I yell, scream, or cry for no reason”). Inhibitory control refers to refraining from non-desirable behavior (e.g., “I do things without thinking first”). Working memory is a mental “work bench”, holding and manipulating components of a task while a solution is found (e.g., “I forget what I’m doing in the middle of things”). Organization of materials is keeping spaces orderly and important materials accessible (e.g., “My desk is a mess”). Item response choices were: 1 = Never, 2 = Sometimes, 3 = Often. Previous pilot analysis using the four full BRIEF-SR scales on 4th grade students demonstrated acceptable internal consistency coefficients (emotional control (10 items) = .63, inhibitory control (13 items) = .78, working memory (12 items) = .78, organization of materials (7 items) = .66,) (Riggs, Sakuma, & Pentz, 2007). Research on the BRIEF-SR suggests convergent and discriminant validity with measures of inattention and general child behavior, and demonstrates ecological validity (e.g., Child Behavior Checklist) (Gioia & Isquith, 2004; Gioia, Isquith, & Guy, 1998; Jarratt, Riccio, & Siekierski, 2005). Parent and teacher ratings on the BRIEF correspond to performance-based measures of EF (Toplak, Bucciarelli, Jain, & Tannock, 2009). Previous studies show that these abbreviated BRIEF scales demonstrate predictive validity when compared to full BRIEF-SR scales (Riggs et al., 2009). Internal consistencies were comparable to full scales: emotional control (6 items) α = .68, inhibitory control (6 items) α = .74, working memory (5 items) α = .71, organization of materials (5 items) α = .63,,. Subscales were significantly correlated with one another (ranging from r = .45 to r = .49, ps < .0001). Items were averaged to create subscales and, as with the full BRIEF-SR, scores from subscales were combined to create an overall EF score (Guy et al., 2004). The total EF score was the mean of the 4 subscales, and internal reliabilities were acceptable at each wave (T1 α = .81, T2 α = .79, T3 α = .77).
Child HCLN intake
To assess child HCLN food intake, 5 items were taken from a validated open-source food frequency questionnaire (Willett, Sampson, Stampfer, Rosner, Bain, Witschi et al., 1985) that has been used successfully in previous studies (Nguyen-Michel, Unger, & Spruijt-Metz, 2007; Riggs et al. 2007, Riggs et al. 2009, Riggs et al. 2010a, Riggs et al., 2010b, Riggs et al., 2011). The items assessed consumption of French fries, chips, doughnuts, candy, and non-diet soda (e.g., “How often do you eat corn chips, potato chips, popcorn, crackers?”). Response choices for snack food intake items were: 1 = Less than once a week; 2 = Once a week; 3 = 2–3 times a week, 4 = 4–6 times a week, 5 = Once a day, 6 = 2 or more of these a day. Abbreviated food frequency questionnaires have been validated for 4th grade youth (Field et al., 1999). Internal reliability for snack food items was acceptable (T1 α = .80, T2 α = .79, T3 α = .81).
Child-perceived parent fast food intake
To assess child-perceived parent fast food consumption, one item was used from the Midwestern Prevention Project (MPP) (Pentz, Johnson, Dwyer, Mackinnon, Hansen, & Flay, 1989): “In a usual week, how many times a day do you see either of your parents (or other important adult) eating fast food or packaged snacks like cookies or chips?” Response choices for this item ranged from: 1 = 0 times a day, 2 = 1 time a day; 3 =2 or more times/day. To our knowledge, this single item measure has not been validated against actual fast food consumption by adults. However, single-item measures have been found to be valid for other health indicators, such as overall health, in population studies and small pilots (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Rohrer, Herman, Merry, Naessens, & Houston, 2009).
Data analytic strategy
First, overall mean scores for child EF and self-reported HCLN intake were calculated. Second, attrition analysis was conducted to test differences between participants lost versus retained at follow-up. Third, intra-class correlation assessed the degree of clustering (children nested within classrooms) (Murray, Varnell, & Blitstein, 2004). Fourth, the direct effect of EF on HCLN and the indirect effect through perceived parent fast food intake were tested cross-sectionally and longitudinally. The SAS macro INDIRECT was used to estimate effects, which uses a bootstrapping method to calculate indirect effects and the underlying sampling distribution of the ab paths, rather than relying on assumed multivariate normality (Hayes, 2009; Preacher & Hayes, 2008). The INDIRECT macro provides a more accurate assessment of statistical significance of the indirect effect compared to traditional methods but does not account for clustering within schools. Therefore, results from the bootstrapping procedure were compared to those adjusted for clustered data using data mixed models (PROC MIXED) and the three-step mediation procedure outlined by Baron and Kenny (1986). The pattern of significance for the parameter estimates and ab paths was unchanged. Resampling was repeated 5,000 times, and unstandardized coefficients and standard errors are reported (Preacher & Hayes, 2008). Cross-sectional and longitudinal models were adjusted for gender, ethnicity, intervention group, and free/reduced lunch status. The longitudinal model also adjusted for baseline child HCLN. At Time 3, due to school closings and transitioning from elementary to middle school, 48 students changed group assignment and 146 were missing data on group. Therefore, intent-to-treat analysis was conducted: the group to which a student was originally assigned was used. Analysis was conducted using Statistical Analysis Software version 9.2 (SAS Institute, Cary, NC, USA).
Results
Table 1 shows descriptive statistics. Mean scores (see Table 1) and internal reliabilities (see Methods) were acceptable. At baseline, mean scores for child EF indicated overall proficiency, with children experiencing problems between “never” and “sometimes”, child self-reported HCLN food intake was between 1 and 3 times per week, and 51% of children reported perceiving that parents ate fast food or prepackaged foods about 1 time per day. As shown in Table 2, participants who did not complete measures at all time points were significantly more likely to receive free/reduced lunch and were less likely to be Caucasian than those who completed all waves. The intraclass correlation for the dependent variable, child HCLN intake at Time 3, was moderate (ICC = 0.07) and slightly larger than is typically observed in school-based studies (0.001 to 0.05; Stevens, Taber, Murray, & Ward, 2007).
Table 1.
Descriptive Statistics for Child EF, Perceived Parent Fast Food Intake, and Child HCLN across Three Waves of Data Collection
| Variable | N or Freq. | M or % | SD | Min. | Max. |
|---|---|---|---|---|---|
| Executive Function | |||||
| T1 | 1005 | 1.67 | 0.33 | 1.00 | 2.82 |
| T2 | 1005 | 1.69 | 0.33 | 1.00 | 2.86 |
| T3 | 859 | 1.66 | 0.33 | 1.00 | 2.63 |
| Child self-reported HCLN | |||||
| T1 | 1003 | 2.39 | 1.05 | 1.00 | 6.00 |
| T2 | 993 | 2.31 | 0.96 | 1.00 | 6.00 |
| T3 | 855 | 2.32 | 0.98 | 1.00 | 6.00 |
| Child-perceived Parent Fast Food Intake | |||||
| T1 | |||||
| 0 times/day | 268 | 26.75 | |||
| 1 time/day | 508 | 50.70 | |||
| 2 or more times/day | 226 | 22.55 | |||
| Missing | 3 | ||||
| T2 | |||||
| 0 times/day | 254 | 25.48 | |||
| 1 time/day | 527 | 52.86 | |||
| 2 or more times/day | 216 | 21.66 | |||
| Missing | 8 | ||||
| T3 | |||||
| 0 times/day | 233 | 27.25 | |||
| 1 time/day | 463 | 54.15 | |||
| 2 or more times/day | 159 | 18.60 | |||
| Missing | 150 | ||||
Note: HCLN = High-calorie, Low-nutrition: 1 = Less than once a week; 2 = Once a week; 3 = 2–3 times a week, 4 = 4–6 times a week, 5 = Once a day, 6 = 2 or more of these a day; Higher scores indicate EF proficiency
Table 2.
Attrition Analysis for Baseline Values of Study Variables and Demographics
| Completed all waves (n = 848) | Did not complete all waves (n = 157) | Chi-Square or F test | p-value | |
|---|---|---|---|---|
| Executive Function | 1.66 | 1.71 | 2.79 | 0.10 |
| HCLN | 2.37 | 2.51 | 2.55 | 0.11 |
| Perceived Parent FF | ||||
| 0 times/day | 27.12% | 24.20% | 1.60 | 0.66 |
| 1 time/day | 50.59% | 50.32% | ||
| 2 or more/day | 22.05% | 24.84% | ||
| Missing | 0.24% | 0.64% | ||
| Age | 9.27 yrs | 9.27 yrs. | 0.04 | 0.84 |
| Gender (male) | 47.76% | 49.04% | 0.09 | 0.77 |
| Free/reduced lunch | 23.35% | 33.76% | 7.66 | 0.01* |
| Caucasian | 31.37% | 20.38% | 7.66 | 0.01* |
Note: HCLN = high-calorie, low-nutrition; FF = fast food
p < 0.05
Child EF Proficiency, Perceived Parent Fast Food Intake, and Child HCLN Intake
Table 3 shows cross-sectional results for each time point. The pattern across waves was relatively consistent. Child EF difficulties were associated with higher child HCLN consumption (Bs range: 0.46 – 0.61, ps < 0.001), and there were significant indirect effects through higher perceived parent fast food intake (ABs range = 0.16 – 0.18; 95% CIs = 0.10–0.11/0.24–0.25). Thus, cross-sectionally, EF difficulties were associated with higher self-reported HCLN intake, mediated by perceiving more frequent parent fast food consumption.
Table 3.
Cross-sectional results for mediated relationship between EF and HCLN intake via perceived parent fast food intake at three time points
| n | C | SE C | C′ | SE C′ | A | SE A | B | SE B | AB | 95% CI Lo.^ | 95% CI Up.^ | R2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time 1 | 1000 | 0.46** | 0.10 | 0.29** | 0.10 | 0.36** | 0.07 | 0.48** | 0.04 | 0.17 | 0.11 | 0.25 | 0.17 | 33.57 | < 0.001 |
| Time 2 | 986 | 0.61** | 0.09 | 0.44** | 0.09 | 0.37** | 0.07 | 0.47** | 0.04 | 0.18 | 0.11 | 0.25 | 0.19 | 37.58 | < 0.001 |
| Time 3 | 851 | 0.55** | 0.10 | 0.39** | 0.09 | 0.36** | 0.07 | 0.45** | 0.05 | 0.16 | 0.10 | 0.24 | 0.18 | 30.09 | < 0.001 |
p < 0.01
p < 0.001
bias corrected
Note: Covariates include child Hispanic ethnicity, gender, free/reduced lunch, and program group; C = the direct effect of the predictor variable on the outcome; C′ = the direct effect of the predictor on the outcome, adjusting for the mediator; A = the direct effect of the predictor on the mediator; B = the effect of the mediator on the outcome, adjusting for the predictor; AB = the indirect effect of the predictor on the outcome via the mediator; SE = standard error
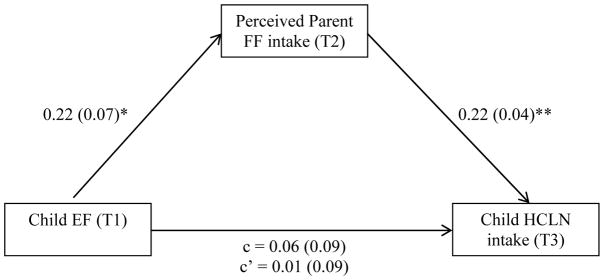
Longitudinally, child EF difficulties did not have a direct effect on higher HCLN intake a year and a half later (B = 0.01, SE = 0.10, t = 0.10, p = 0.92, n = 848) (see Figure 1). However, greater EF difficulties did have a significant indirect effect through higher perceived parent fast food intake at Time 2 (AB path = 0.05; SE = 0.02, 95% CI = (0.02/0.10), R2 = 0.23, F(7, 840) = 36.23, p < 0.001) suggesting that EF difficulties may increase children’s perception that parents consume fast foods more frequently over time (6 months), leading children to consume greater amounts of HCLN foods. Significant covariates were baseline child HCLN intake (B = 0.35, SE = 0.03, p < 0.001), free/reduced lunch status (B = 0.33, SE = 0.07, p < 0.001), and program group (Intervention vs. Control) (B = 0.15, SE = 0.06 p < 0.05). To explore differences by program group, the model was re-run for each group separately. There were no differences in significance values or coefficient magnitudes. The c and c′ paths were slightly larger in the Program group than the Control, but none significantly differed from zero (Program: c path = 0.09, SE = 0.13, p = 0.52; c′ path = 0.04, SE = 0.13, p = 0.78; Control: c path = 0.04, SE = 0.13, p = 0.76; c′ path = −0.01, SE = 0.13, p = 0.94). Indirect effects were similar for Program and Control: Program = 0.05, 95% CI = (0.01, 0.11), Control = 0.05, 95% CI = (0.01, 0.13).
Figure 1. Longitudinal Direct and Indirect Effects of Child EF on Perceived Parent Fast Food Intake and HCLN intake.
Indirect effect = 0.05, SE = 0.02, 95% CI = (0.02/0.10)
R2 = 0.23; F(7, 840) = 36.23, p < 0.001
N = 848
* p < 0.01
** p < 0.001
Note: Covariates include child gender (male = 1, female = 0, B = 0.01, SE = 0.06, p = 0.90), Hispanic ethnicity (B = 0.06, SE = 0.07, p = 0.34), free/reduced lunch status (B = 0.33, SE = 0.07, p < 0.001), program group (B = 0.15, SE = 0.06 p < 0.05) and baseline child HCLN intake (B = 0.35, SE = 0.03, p < 0.001); unstandardized parameter estimates are reported with standard errors in parentheses; higher EF scores indicate more EF difficulties.
Discussion
This study found that adolescents who have executive function difficulties report perceiving that parents consume convenience or snack foods more frequently, which was, in turn, positively associated with child consumption of high-calorie, low-nutrient foods. Similar to prior research, EF problems were associated with higher concurrent intake of high-calorie snack foods (Riggs et al., 2010a). The current study extends prior work by examining perceived parent behavior, according to a Social Learning Theory approach. Findings suggest that observational learning may affect child consumption of high-calorie snack foods, beyond the effects of gender, ethnicity, and SES. EF difficulties may compromise children’s’ ability to understand parents’ occasional fast food consumption as an isolated event rather than a new model to follow. Several factors may shed light on these findings. First, EF proficiency may increase awareness of parents’ expectations for healthy behavior and attempts to behave according to expectations. EF may raise awareness of parent rules (Vereecken, Legiest, De Bourdeaudhuij, & Maes, 2009). Second, EF proficiency could encourage children to attend to positive experiences when processing their surroundings, discounting potentially negative influences. During adolescence, prefrontal cortical development, associated with executive function, develops slower than the subcortex, which regulates appetitive behavior, partially explaining increases in risky behavior even when adolescents are aware of consequences (Somerville, Jones, & Casey, 2010). Similarly, adolescents with EF, prefrontal cortex, difficulties may experience heightened salience of highly palatable foods being consumed by role models, or may be more vulnerable to environmental stimuli such as food advertising (Moses & Baldwin, 2005). Third, EF could aid children in making personal decisions that align with long-term benefits, such as controlling impulsive eating. Finally, children with EF challenges may be difficult to manage during mealtimes, making fast food a quick, appealing option compared to quiet restaurants. Although the current results suggest that EF difficulties compromise perception of modeled behavior and potentially heighten obesity risk, further research is needed to untangle potential bi-directional relationships (Smith, Hay, Campbell, & Trollor, 2011).
Contrary to hypotheses, the current study did not find a direct, longitudinal effect of EF on HCLN consumption one and a half years later, although the mediated effect through perceived parent intake was significant. Potentially, the time between measures was too long. During this time, developmental changes in EF (Anderson, 2002), dietary intake patterns, or both could have occurred. Peers and media may also play a larger role in consumption patterns as children age, mitigating effects of parent behavior (Cullen, Baranowski, Rittenberry, & Olvera, 2000; Fitzgerald, Heary, Kelly, Nixon, & Shevlin, 2013).
Limitations
One limitation of this study is that EF and food intake were measured via self-report. Clinical differences may exist between the issues measured by the BRIEF versus performance measures (McAuley, Chen, Goos, Schachar, & Crosbie, 2010). In one study, task-based impulsivity but not self-reported impulsivity, was related to obesity (Verdejo-Garcia et al., 2010). Also, this study used a single-item measure of perceived parent fast food intake from previous research (Pentz et al., 1997). The measure has not been validated against multiple-item measures, such as multiple-item 24-hour dietary recalls (ex., Paeratakul, Ferdinand, Champagne, Ryan, & Bray, 2003). However, other studies have used single-item measures of adolescent self-reported fast food intake (ex., French, Story, Neumark-Sztainer, Fulkerson, & Hannan, 2001), and single-item measures have been found to be valid for other health indicators, such as overall health (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Rohrer, Herman, Merry, Naessens, & Houston, 2009). While this single-item measure has not been validated against actual parent diet to our knowledge, the study aimed to examine child perception – not actual parent intake – but effects of actual parent consumption remain unknown. However, future research could include measures of actual parent intake to investigate correspondence with child perceptions. Second, effects might have been stronger with a more comprehensive measure of dietary intake, although these abbreviated screeners have been used successfully in other studies (ex., Riggs et al. 2009). Potentially, self-reported intake of these foods is related to EF differently than intake assessed by 24-hour, 3 day dietary recalls. Third, the follow-up sample was less likely to receive free/reduced lunch and more likely to be Caucasian, possibly limiting generalizability. Fourth, effects of child EF could have been caused by differences in child perception, encoding, or memory retrieval, and specific cognitive functions remain unknown.
Implications for Theory, Policy, and Practice
This study found that child EF was indirectly related to subsequent child HCLN intake through child-perceived parent fast food intake. Results suggest that EF could affect observational learning of dietary behaviors. Although additional intervention research is needed examining actual parent food intake, one potential implication is that child diet could be improved by helping children understand occasional role model unhealthy food consumption. Programs focused solely on changing parents’ actual role modeling behavior may not address the issue of child perception and interpretation of modeled behavior. EF could operate less directly on children’s health behaviors than previously thought. Rather, EF may affect cognitive processing of observed modeled behaviors, suggesting that research assuming a direct modeling effect might consider investigating interpreted modeling instead. Programs could also educate parents about potential effects of their behavior on child consumption patterns and on the importance of explaining occasional exceptions. Additionally, EF may affect children’s interpretation of other observed modeled behaviors, such as those of peers or teachers, suggesting other avenues for future research and program design. Parent behavior plays an important role in child health. Parents provide healthy foods, engage in positive feeding practices, and can have supportive parenting styles. However, EF proficiency may allow children to benefit fully from role models’ healthy behaviors and minimize effects of less healthy behaviors.
Acknowledgments
This manuscript was supported by the National Institute of Health Grant R01HD052107-03; and the National Cancer Institute Training Fellowship T32CA009492-28.
References
- Alvarez JA, Emory E. Executive function and the frontal lobes: A meta-analytic review. Neuropsychology Review. 2006;16(1):17–42. doi: 10.1007/s11065-006-9002-x. [DOI] [PubMed] [Google Scholar]
- Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychology. 2002;8(2):71–82. doi: 10.1076/chin.8.2.71.8724. [DOI] [PubMed] [Google Scholar]
- Anderson PM, Butcher KF. Childhood Obesity: Trends and Potential Causes. The Future of Children. 2006;16(1):19–45. doi: 10.1353/foc.2006.0001. [DOI] [PubMed] [Google Scholar]
- Ardila A, Rosselli W, Matute E, Guajardo S. The influence of the parents’ educational level on the development of executive functions. Developmental Neuropsychology. 2005;28(1):539–560. doi: 10.1207/s15326942dn2801_5. [DOI] [PubMed] [Google Scholar]
- Arslanian S. Type 2 diabetes in children: Clinical aspects and risk factors. Hormone Research. 2002;57:19–28. doi: 10.1159/000053308. [DOI] [PubMed] [Google Scholar]
- Bandini LG, Vu D, Must A, Cyr H, Goldberg A, Dietz WH. Comparison of high-calorie, low-nutrient-dense food consumption among obese and non-obese adolescents. Obesity Research. 1999;7(5):438–443. doi: 10.1002/j.1550-8528.1999.tb00431.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Learning Theory. Prentice-Hall; NY: 1977. [Google Scholar]
- Bandura A. Human agency in social cognitive theory. American Psychologist. 1989;44:1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Mendlein J, Resnicow K, Frank E, Cullen KW, Baranowski J. Physical activity and nutrition in children and youth: An overview of obesity prevention. Preventive Medicine. 2000;31:S1–S10. [Google Scholar]
- Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berkey CS, Rockett HRH, Field AE, Gillman MW, Frazier AL, Camargo CA, Colditz GA. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics. 2000;105:e56. doi: 10.1542/peds.105.4.e56. doi:e5610.1542/peds.105.4.e56. [DOI] [PubMed] [Google Scholar]
- Blair C. School readiness: Integrating cognition and emotion in a neurobiological conceptualization of children’s functioning at school entry. American Psychologist. 2002;57(2):111-111–127. doi: 10.1037/0003-066x.57.2.111. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Fulkerson JA, Neumark-Sztainer D, Story M, French SA. Fast food for family meals: relationships with parent and adolescent food intake, home food availability and weight status. Public Health Nutrition. 2007;10(1):16–23. doi: 10.1017/s136898000721794x. [DOI] [PubMed] [Google Scholar]
- Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. International Journal of Obesity. 2006;30(8):1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. Connected: the surprising power of our social networks and how they shape our lives. New York: Little, Brown and Co; 2009. [Google Scholar]
- Cserjesi R, Moinar D, Luminet O, Lenardo L. Is there any relationship between obesity and mental flexibility in children? Appetite. 2007;49(3):675–678. doi: 10.1016/j.appet.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Cullen KW, Baranowski T, Rittenberry L, Olvera N. Social-environmental influences on children’s diets: results from focus groups with African-, Euro- and Mexican-American children and their parents. Health Education Research. 2000;15(5):581–590. doi: 10.1093/her/15.5.581. [DOI] [PubMed] [Google Scholar]
- Dunton GF, Berrigan D, Ballard-Barbash R, Perna FM, Graubard BI, Atienza AA. Adolescents’ sports and exercise environments in a U.S. time use survey. American Journal of Preventive Medicine. 2010;39:122–129. doi: 10.1016/j.amepre.2010.03.022. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, … Wechsler H. Youth risk behavior surveillance - United States, 2005. Journal of School Health. 2006;76:353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- Farah MJ, Shera DM, Savage JH, Betancourt L, Giannetta JM, Brodsky NL, … Hurt H. Childhood poverty: Specific associations with neurocognitive development. Brain Research. 2006;1110(1):166–174. doi: 10.1016/j.brainres.2006.06.072. [DOI] [PubMed] [Google Scholar]
- Field AE, Peterson KE, Gortmaker SL, Cheung L, Rockett H, Fox MK, Colditz GA. Reproducibility and validity of a food frequency questionnaire among fourth to seventh grade inner-city school children: implications of age and day-to-day variation in dietary intake. Public health nutrition. 1999;2(03):293–300. doi: 10.1017/s1368980099000397. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: associations with nutrient intake, food choices and behavioral and psychosocial variables. International Journal of Obesity. 2001;25(12):1823–1833. doi: 10.1038/sj.ijo.0801820. [DOI] [PubMed] [Google Scholar]
- Gathercole SE, Pickering SJ, Knight C, Stegmann Z. Working memory skills and educational attainment: Evidence from national curriculum assessments at 7 and 14 years of age. Applied Cognitive Psychology. 2004;18(1):1–16. doi: 10.1002/acp.934. [DOI] [Google Scholar]
- Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Developmental Neuropsychology. 2004;25(1–2):135–158. doi: 10.1207/s15326942dn2501&2_8. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC. The regulatory role of executive control processes in children’s behavioral, social, and emotional functioning. Journal of Neuropsychiatry and Clinical Neurosciences. 1998:9. [Google Scholar]
- Goran MI, Gower BA. Abdominal obesity and cardiovascular risk in children. Coronary Artery Disease. 1998;9:483–487. doi: 10.1097/00019501-199809080-00003. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Archives of pediatrics & adolescent medicine. 1999;153(4):409. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- Gross SM, Pollock ED, Braun B. Family Influence: Key to Fruit and Vegetable Consumption among Fourth- and Fifth-grade Students. Journal of Nutrition Education and Behavior. 2010;42:235–241. doi: 10.1016/j.jneb.2009.05.007. [DOI] [PubMed] [Google Scholar]
- Guy SC, Isquith PK, Gioia GA. Behavior Rating Inventory of Executive Function -- Self-report version. Psychological Assessment Resources; Lutz, FL: 2004. [Google Scholar]
- Hall Peter A. Executive control resources and frequency of fatty food consumption: Findings from an age-stratified community sample. Health Psychology. 2012;31(2):235–241. doi: 10.1037/a0025407. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Communication Monographs. 2009;76(4):408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Hendrie G, Sohonpal G, Lange K, Golley R. Change in the family food environment is associated with positive dietary change in children. International Journal of Behavioral Nutrition and Physical Activity. 2013:10. doi: 10.1186/1479-5868-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuer CA, McClure KJ, Puhl RM. Obesity Stigma in Online News: A Visual Content Analysis. Journal of Health Communication. 2011;16:976–987. doi: 10.1080/10810730.2011.561915. [DOI] [PubMed] [Google Scholar]
- Hongwanishkul D, Happaney KR, Lee WSC, Zelazo PD. Assessment of hot and cool executive function in young children: Age-related changes and individual differences. Developmental Neuropsychology. 2005;28:617–644. doi: 10.1207/s15326942dn2802_4. [DOI] [PubMed] [Google Scholar]
- Jarratt KP, Riccio CA, Siekierski BM. Assessment of attention deficit hyperactivity disorder (ADHD) using the BASC and BRIEF. Applied Neuropsychology. 2005;12(2):83–93. doi: 10.1207/s15324826an1202_4. [DOI] [PubMed] [Google Scholar]
- Keddie AM. Associations Between Severe Obesity and Depression: Results From the National Health and Nutrition Examination Survey, 2005–2006. Preventing Chronic Disease. 2011:8. [PMC free article] [PubMed] [Google Scholar]
- Klenberg L, Korkman M, Lahti-Nuuttila P. Differential development of attention and executive functions in 3-to 12-year-old Finnish children. Developmental Neuropsychology. 2001;20(1):407–428. doi: 10.1207/s15326942dn2001_6. [DOI] [PubMed] [Google Scholar]
- Knai C, Pomerleau J, Lock K, McKee M. Getting children to eat more fruit and vegetables: A systematic review. Preventive Medicine. 2006;42:85–95. doi: 10.1016/j.ypmed.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Kremers SP, Brug J, de Vries H, Engels R. Parenting style and adolescent fruit consumption. Appetite. 2003;41:43–50. doi: 10.1016/s0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- Krolner R, Rasmussen M, Brug J, Klepp KI, Wind M, Due P. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part II: qualitative studies. International Journal of Behavioral Nutrition and Physical Activity. 2011;8:38. doi: 10.1186/1479-5868-8-112. doi:11210.1186/1479-5868-8-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel mediation modeling in group-based intervention studies. Evaluation Review. 1999;23(4):418–444. doi: 10.1177/0193841X9902300404. [DOI] [PubMed] [Google Scholar]
- Lokken KL, Boeka AG, Austin HM, Gunstad J, Harmon CM. Evidence of executive dysfunction in extremely obese adolescents: a pilot study. Surgery for Obesity and Related Diseases. 2009;5(5):547–552. doi: 10.1016/j.soard.2009.05.008. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Mackinnon DP, Dwyer JH. Estimating Mediated effects in prevention studies. Evaluation Review. 1993;17(2):144–158. doi: 10.1177/0193841x9301700202. [DOI] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037//1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Taborga MP, Morgan-Lopez AA. Mediation designs for tobacco prevention research. Drug and Alcohol Dependence. 2002;68:S69–S83. doi: 10.1016/s0376-8716(02)00216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macrae CN, Bodenhausen GV, Schloerscheidt AM, Milne AB. Tales of the unexpected: Executive function and person perception. Journal of Personality and Social Psychology. 1999;76(2):200–213. doi: 10.1037/0022-3514.76.2.200. [DOI] [PubMed] [Google Scholar]
- McAuley T, Chen S, Goos L, Schachar R, Crosbie J. Is the behavior rating inventory of executive function more strongly associated with measures of impairment or executive function? Journal of the International Neuropsychological Society. 2010;16(3):495–505. doi: 10.1017/s1355617710000093. [DOI] [PubMed] [Google Scholar]
- Mond JM, Stich H, Hay PJ, Kraemer A, Baune BT. Associations between obesity and developmental functioning in pre-school children: a population-based study. International Journal of Obesity. 2007;31(7):1068–1073. doi: 10.1038/sj.ijo.0803644. [DOI] [PubMed] [Google Scholar]
- Murray DM, Varnell SP, Blitstein JL. Design and analysis of group-randomized trials: A review of recent methodological developments. American Journal of Public Health. 2004;94(3):423–432. doi: 10.2105/ajph.94.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Michel ST, Unger JB, Spruijt-Metz D. Dietary correlates of emotional eating in adolescence. Appetite. 2007;49:494–499. doi: 10.1016/j.appet.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity and Trends in Body Mass Index Among US Children and Adolescents, 1999–2010. Jama-Journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paeratakul S, Ferdinand DP, Champagne CM, Ryan DH, Bray GA. Fast-food consumption among US adults and children: Dietary and nutrient intake profile. Journal of the American Dietetic Association. 2003;103(10):1332–1338. doi: 10.1016/s0002-8223(03)01086-1. http://dx.doi.org/10.1016/S0002-8223(03)01086-1. [DOI] [PubMed] [Google Scholar]
- Pearson N, Biddle SJH. Sedentary Behavior and Dietary Intake in Children, Adolescents, and Adults A Systematic Review. American Journal of Preventive Medicine. 2011;41(2):178–188. doi: 10.1016/j.amepre.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Pearson N, Biddle SJH, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutrition. 2009;12:267–283. doi: 10.1017/S1368980008002589. [DOI] [PubMed] [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Johnson CA, Dwyer JH, Mackinnon DM, Hansen WB, Flay BR. A comprehensive community approach to adolescent drug-abuse prevention: Effects on cardiovascular disease risk behaviors. Annals of Medicine. 1989;21:219–222. doi: 10.3109/07853898909149937. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Spruijt-Metz D, Chou CP, Riggs NR. High Calorie, Low Nutrient Food/Beverage Intake and Video Gaming in Children as Potential Signals for Addictive Behavior. International Journal of Environmental Research and Public Health. 2011;8(12):4406–4424. doi: 10.3390/ijerph8124406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rhoades BL, Greenberg MT, Lanza ST, Blair C. Demographic and familial predictors of early executive function development: Contribution of a person-centered perspective. Journal of Experimental Child Psychology. 2011;108(3):638–662. doi: 10.1016/j.jecp.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs NR, Mesirov C, Shin HS, Pentz MA. The Relationship Between Executive function and Food Intake and Physical Activity in Children. Obesity. 2009;17:S212–S212. [Google Scholar]
- Riggs NR, Sakuma KL, Pentz MA. Preventing risk for obesity by promoting self-regulation and decision-making skills: Pilot results from the PATHWAYS to health program (PATHWAYS) Evaluation Review. 2007;31:287–310. doi: 10.1177/0193841x06297243. [DOI] [PubMed] [Google Scholar]
- Riggs NR, Spruijt-Metz D, Chou CP, Pentz MA. Relationships between executive function and lifetime substance use and obesity-related behaviors in fourth grade youth. Child Neuropsychology. 2012;18:1–11. doi: 10.1080/09297049.2011.555759. [DOI] [PubMed] [Google Scholar]
- Riggs NR, Spruijt-Metz D, Sakuma KL, Chou CP, Pentz MA. Executive function and Food Intake in Children. Journal of Nutrition Education and Behavior. 2010a;42:398–403. doi: 10.1016/j.jneb.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs N, Chou CP, Spruijt-Metz D, Pentz MA. Executive function as a Correlate and Predictor of Child Food Intake and Physical Activity. Child Neuropsychology. 2010b;16(3):279–292. doi: 10.1080/09297041003601488. [DOI] [PubMed] [Google Scholar]
- Sarsour K, Sheridan M, Jutte D, Nuru-Jeter A, Hinshaw S, Boyce WT. Family Socioeconomic Status and Child Executive Functions: The Roles of Language, Home Environment, and Single Parenthood. Journal of the International Neuropsychological Society. 2011;17(1):120–132. doi: 10.1017/s1355617710001335. [DOI] [PubMed] [Google Scholar]
- Smith E, Hay P, Campbell L, Trollor JN. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obesity Reviews. 2011;12(9):740–755. doi: 10.1111/j.1467-789X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- Somerville LH, Jones RM, Casey BJ. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and Cognition. 2010;72(1):124–133. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D. Etiology, Treatment, and Prevention of Obesity in Childhood and Adolescence: A Decade in Review. Journal of Research on Adolescence. 2011;21:129–152. doi: 10.1111/j.1532-7795.2010.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberger J, Daniels SR. Obesity, insulin resistance, diabetes, and cardiovascular risk in children - An American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism) Circulation. 2003;107:1448–1453. doi: 10.1161/01.cir.0000060923.07573.f2. [DOI] [PubMed] [Google Scholar]
- Stevens J, Taber DR, Murray DM, Ward DS. Advances and controversies in the design of obesity prevention trials. Obesity. 2007;15(9):2163–2170. doi: 10.1038/oby.2007.257. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Rodzilsky D, Burack G, Colin M. Psychosocial correlates of physical activity in health children. Archives of Pediatrics & Adolescent Medicine. 2001;155:897–902. doi: 10.1001/archpedi.155.8.897. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Bucciarelli S, Jain U, Tannock R. Executive Functions: Performance-Based Measures and the Behavior Rating Inventory of Executive Function (BRIEF) in Adolescents with Attention Deficit/Hyperactivity Disorder (ADHD) Child Neuropsychology. 2009;15(1):53–72. doi: 10.1080/09297040802070929. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Perez-Exposito M, Schmidt-Rio-Valle J, Fernandez-Serrano MJ, Cruz F, Perez-Garcia M, … Campoy C. Selective Alterations Within Executive Functions in Adolescents With Excess Weight. Obesity. 2010;18(8):1572–1578. doi: 10.1038/oby.2009.475. [DOI] [PubMed] [Google Scholar]
- Vereecken C, Legiest E, De Bourdeaudhuij I, Maes L. Associations Between General Parenting Styles and Specific Food-Related Parenting Practices and Children’s Food Consumption. American Journal of Health Promotion. 2009;23(4):233–240. doi: 10.4278/ajhp.07061355. [DOI] [PubMed] [Google Scholar]
- Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S. Obesity and the metabolic syndrome in children and adolescents. New England Journal of Medicine. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. American Journal of Epidemiology. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nature Medicine. 2006;12:62–66. doi: 10.1038/nm0106-62. [DOI] [PubMed] [Google Scholar]
- Zelazo PD, Carter A, Reznick JS, Frye D. Early development of executive function: A problem-solving framework. Review of General Psychology. 1997;1(2):198-198–226. doi: 10.1037/1089-2680.1.2.198. [DOI] [Google Scholar]
- Zhao XS, Lynch JG, Chen QM. Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis. Journal of Consumer Research. 2010;37(2):197–206. doi: 10.1086/651257. [DOI] [Google Scholar]