Abstract
Gray hair syndromes are rare syndromes which have an autosomal recessive inheritance and are characterized by pigmentary dilution of skin and hair, defects in immunological function, and nervous system defects. They comprise three disorders namely Chediak–Higashi syndrome (CHS), Griscelli syndrome (GPS), and Elejalde syndrome. Clinically, it is difficult to distinguish these disorders as their clinical features may overlap. Hence, to make a correct diagnosis and differentiate between CHS and GPS light microscopic examination of skin and hair shafts as well as peripheral blood smear evaluations should be done. In cases where the diagnosis is not possible chromosomal analysis for specific mutations can be done. In resource-poor settings where chromosomal analysis is not possible, and light microscopy findings are inconclusive, polarized microscopy can serve as a useful tool to distinguish between CHS and GPS. We report three cases with gray hair syndromes where the diagnosis on light microscopy and polarized microscopy of hair shaft correlated with the bone marrow examination findings and chromosomal analysis, thus emphasizing the importance of a noninvasive, cost-effective, and time-saving alternative in the diagnosis of these syndromes.
Key words: Chediak–Higashi syndrome, gray hair syndromes, Griscelli syndrome, polarized microscopy
INTRODUCTION
Gray hair syndromes are rare autosomal recessive disorders and include three disorders namely Chediak–Higashi syndrome (CHS), Griscelli syndrome (GPS), and Elejalde syndrome which are characterized by pigmentary dilution, immunological defects, and neurological defects.[1] Clinical features of these three syndromes overlap and hence to differentiate these syndromes light microscopy, peripheral blood smear examination, and bone marrow examination can be done. Keratin has refractile properties which can serve as a basis to do polarized microscopy of hair shaft and therefore can be used to differentiate these syndromes where light microscopy is inconclusive.[2]
CASE REPORTS
Case report 1
A 25-month-old female child born out of consanguineous marriage presented to pediatric outpatient department with recurrent episodes of diarrhea for 3 months. Her birth history was unremarkable, but developmental milestones were delayed.
On examination, the patient had silvery gray hair on the scalp, and mottled pigmentation was present over the face, neck, and both the extremities [Figure 1].
Figure 1.

(a) Silvery gray hair on the scalp and mottled pigmentation present over the face. (b) Silvery gray hair on the scalp. (c) Mottled pigmentation present over both upper and lower limbs. (d) Mottled pigmentation closer view
Pallor and mild hepatosplenomegaly was present. Nystagmus was present in both the eyes. Based on the above findings, differential diagnoses of fanconi anemia, GPS and CHS were made.
Complete blood picture revealed severe anemia and neutropenia. Peripheral blood smear did not reveal the presence of giant cytoplasmic granules in the leukocytes. Serum ferritin and reticulocyte count were within normal limits. Thyroid function test was normal. Bleeding time and clotting time were normal. Ophthalmological examination showed foveal aplasia and vision was normal on fundoscopy. Karyotyping done for chromatid breaks was found to be normal. The patient was referred to us for hair shaft examination.
On light microscopy, melanin clumps were seen which were large and regular [Figure 2].
Figure 2.
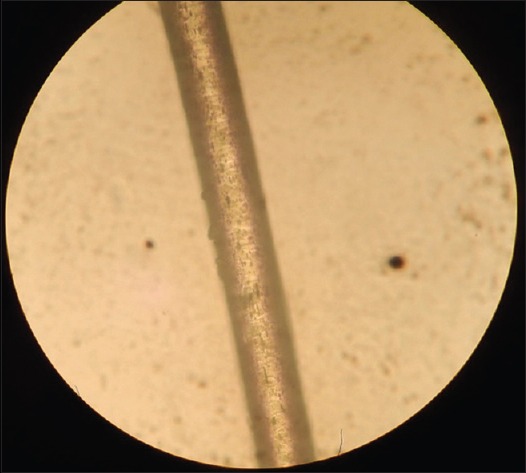
Light microscopy at ×40 magnification showing large regular clumps of melanin in the hair shaft
On polarized microscopy, bright shaft with different individual colors suggestive of CHS was seen [Figure 3].
Figure 3.
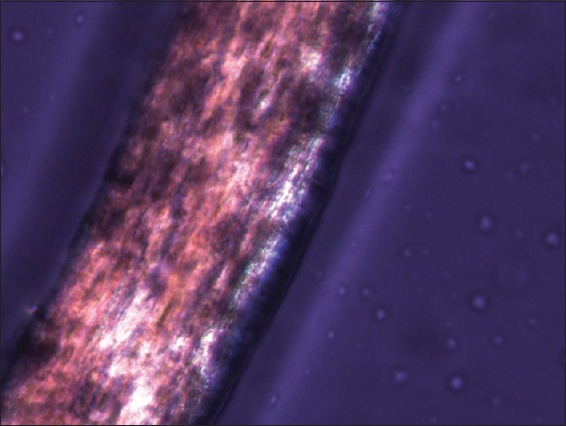
Polarized microscopy showing bright shaft with different individual colors
Bone marrow examination was thus done which showed large intracytoplasmic inclusion bodies in myeloid cells confirming the diagnosis of CHS.
Case report 2
A 45-day-old male child born out of consanguineous marriage was admitted with mild grade fever for 1 week. There was no history of a cough, cold, vomiting or loose stools. No history of seizures or rash was present.
On examination, abdomen was distended with mild hepatosplenomegaly present. Cutaneous examination showed generalized hypopigmentation of skin and gray hair over the scalp, eyebrows, and eyelashes as shown in Figure 4.
Figure 4.

Gray hair present on scalp
On laboratory investigations pancytopenia was present. Peripheral blood smear was normal.
Hair shaft examination under light microscopy showed large irregular melanin granules as shown in Figure 5, suggestive of GPS.
Figure 5.
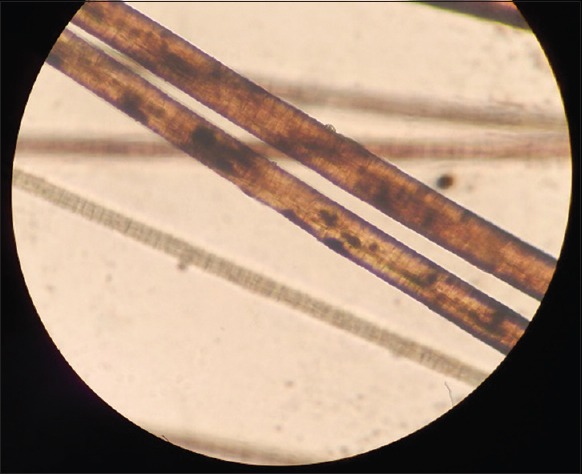
Light microscopy at ×40 magnification showing large irregular melanin granules
Bone marrow examination showed hypocellular marrow with hemophagocytosis thus confirming the diagnosis of GPS.
Case report 3
A 13-day-old female child born out of consanguineous marriage presented with grayish discoloration of scalp and eyebrow hair since birth [Figure 6]. There was a history of ear discharge from the left ear for 2 days. There was no history of fever, cough, or cold. No history of loose stools was present. Birth history was unremarkable. On clinical examination, hepatosplenomegaly was present. Laboratory evaluation showed the presence of pancytopenia. Peripheral blood smear was normal.
Figure 6.

Grayish discoloration of scalp and eyebrow hair
Hair shaft examination under light microscopy was inconclusive [Figure 7].
Figure 7.
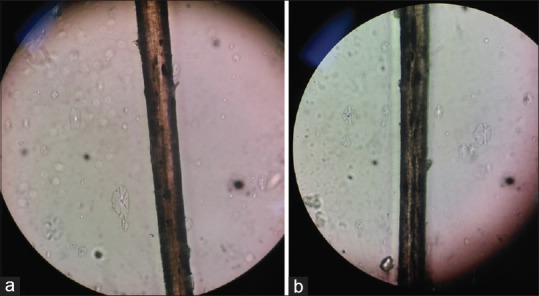
(a) Light microscopy of the hair shaft showing inconclusive results. (b) Light microscopy of the hair shaft showing inconclusive results
Polarized microscopy showed bright hair shaft with monotonous white appearance as shown in Figure 8.
Figure 8.
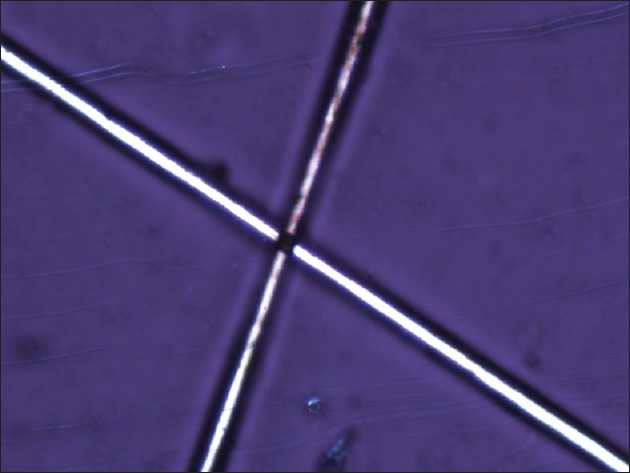
Polarized microscopy showing bright hair shaft with monotonous white appearance
A diagnosis of GPS was made. Bone marrow examination showed slightly hypocellular marrow with no intracytoplasmic inclusions. Genetic analysis revealed mutation in RAB27A gene thus confirming the diagnosis of GPS type 2.
DISCUSSION
Three gray hair syndromes, namely, CHS, GPS, and Elejalde, are rare autosomal recessive disorders characterized by gray hair, pigmentary dilution of skin with a grayish discoloration with associated ocular hypopigmentation in a few of them. Pigmentary dilution is a result of giant hypopigmented melanosomes clustered around the nucleus in melanosomes and their inefficient transfer to keratinocytes. Sometimes, speckled hypo- and hyper-pigmentation on sun-exposed areas is reported to occur in CHS.[3] The same was observed in our case 1. Differentiating features of the three gray hair syndromes are shown in Table 1. Light microscopy of the hair is a simple, noninvasive, bedside technique that can help in differentiating CHS from GPS. Normal hair shafts are cylindrical, of variable diameters and have a uniform pigmentation within a shaft.[2]
Table 1.
Differentiating features of the three gray hair syndromes
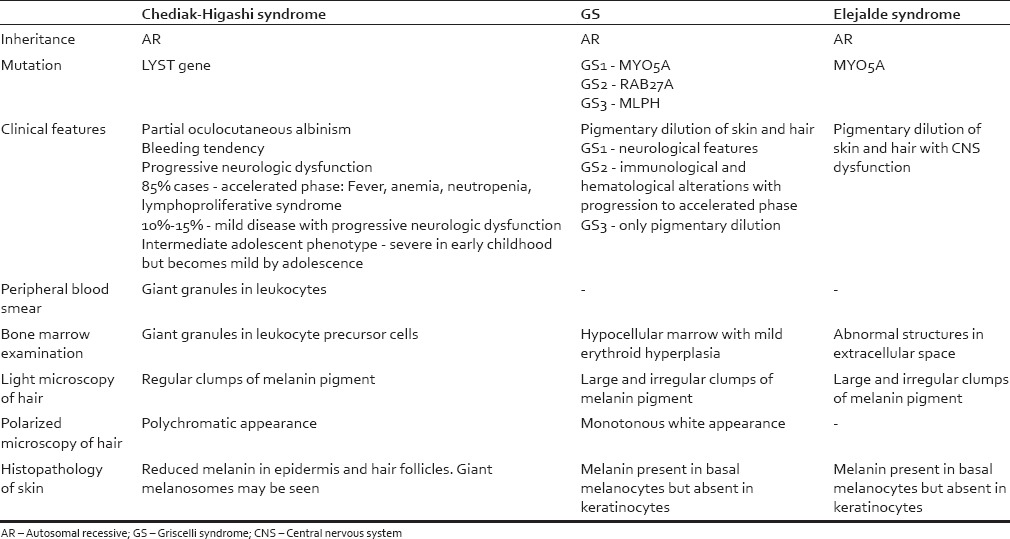
In CHS hair examination under light microscopy shows uniformly distributed melanin pigment granules which are larger than in normal hair. Hair examination in GPS by light microscopy shows larger irregular clumps of melanin pigment.
Polarized light microscopy reveals the whitish, monotonous appearance of hair in patients with GPS, as against their polychromatic appearance in CHS patients.[2] Thus, polarizing microscopy helps to distinguish among the two in cases where light microscopy is inconclusive. The reasons for this variation as evident on polarized light microscopy are not known.[2]
We highlight the importance of hair microscopy as an easy, cost-effective, time-saving, and most importantly a noninvasive technique for diagnosing gray hair syndromes, thus obviating the need for bone marrow examination and chromosomal analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mancini AJ, Chan LS, Paller AS. Partial albinism with immunodeficiency: Griscelli syndrome: Report of a case and review of the literature. J Am Acad Dermatol. 1998;38(2 Pt 2):295–300. doi: 10.1016/s0190-9622(98)70568-7. [DOI] [PubMed] [Google Scholar]
- 2.Valente NY, Machado MC, Boggio P, Alves AC, Bergonse FN, Casella E, et al. Polarized light microscopy of hair shafts aids in the differential diagnosis of Chédiak-Higashi and Griscelli-Prunieras syndromes. Clinics (Sao Paulo) 2006;61:327–32. doi: 10.1590/s1807-59322006000400009. [DOI] [PubMed] [Google Scholar]
- 3.Al-Khenaizan S. Hyperpigmentation in Chediak-Higashi syndrome. J Am Acad Dermatol. 2003;49(5 Suppl):S244–6. doi: 10.1016/s0190-9622(03)00123-3. [DOI] [PubMed] [Google Scholar]


