Abstract
The incidence of acute kidney injury in pregnancy (P-AKI) has declined significantly over the last three decades in developing countries. However, it is still associated with significant fetomaternal mortality and morbidity. The diagnosis of P-AKI is based on the serum creatinine increase. The usual formulas for estimating glomerular filtration rate (GFR) are not validated in this population. The incidence of P-AKI with respect to total AKI cases has decreased in the last three decades from 25% in 1980s to 9% in 2000s at our centre. During the first trimester of gestation, AKI develops most often due to septic abortion or hyperemesis gravidarum. Septic abortion related AKI with respect to total AKI decreased from 9% to 5% in our study. Prevention of unwanted pregnancy and avoidance of septic abortion are keys to eliminate abortion associated AKI in early pregnancy. However, we have not seen AKI on account of hyperemesis gravidarum over a period of 33 years at our center. In the third trimester, the differential diagnosis of AKI in association with pregnancy specific conditions namely preeclampsia/HELLP syndrome, acute fatty liver of pregnancy and thrombotic microangiopathies of pregnancy (P-TMA) is more challenging, because these 3 conditions share several clinical features of thrombotic microangiopathy which makes the diagnosis very difficult on clinical grounds. It is imperative to distinguish these conditions to make appropriate therapeutic decisions. Typically, AFLP and HELLP syndrome improve after delivery of the fetus, whereas plasma exchange is the first-line treatment for pregnancy associated thrombotic microangioathies (P-TMA). We observed that preclampsia/eclampsia is the most common cause of AKI in late third trimester and postpartum periods followed by puerperal sepsis and postpartum hemorrhage. Pregnancy-associated thrombotic microangiopathies (aHUS/TTP) and AFLP are rare causes of AKI during pregnancy in developing countries.
Keywords: Acute fatty liver of pregnancy, AKI in pregnancy, hemolysis elevated liver enzymes and low platelet count syndrome, preeclampsia, thrombotic microangiopathy
Introduction
Acute kidney injury in pregnancy (P-AKI) usually occurs due to obstetrical complications such as septic abortion, abruptio placentae, uterine hemorrhage, intrauterine fetal death (IUD), and puerperal sepsis in women with previous healthy kidneys. However, there are still huge differences in the epidemiological characteristic of P-AKI with respect to incidence, causes, and outcome between developing and developed countries.[1,2,3] These differences are due to environmental, socioeconomic, and different health delivery systems.[3,4] P-AKI has decreased to 1/15,000–1/20,000 in the recent year from 1/3000 in 1960, with respect to the total number of pregnancies in developed countries. Similarly, the incidence of P-AKI has declined to 0%–1% in the last decade from 20% to 40% in the 1960s of total AKI cases.[4] The current incidence of P-AKI in developing countries has a declining trend. Despite decreasing incidence of P-AKI in developing countries, it still accounts for 5%–20% of total AKI population.[2,5,6] The focus of the present review is to discuss the clinical feature and differential diagnosis of pregnancy-specific disorders causing AKI in pregnant women.
Physiologic and Anatomic Changes in Kidney during Pregnancy
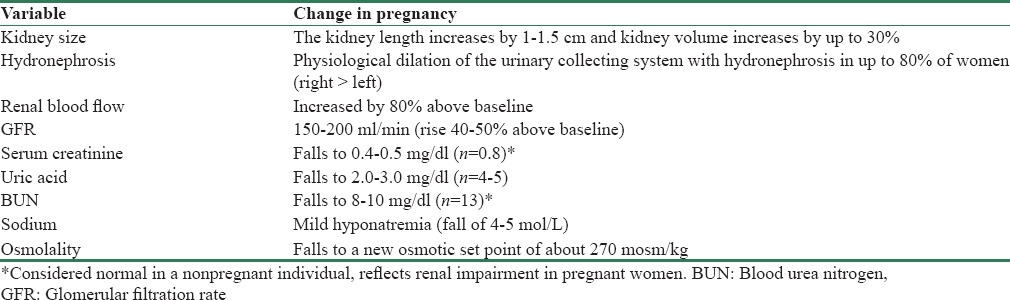
There are considerable changes that occur in the urinary tract system during normal pregnancy: kidneys increase in size by about 1–1.5 cm due to renal vascular and interstitial space volume expansion. The physiological hydronephrosis of pregnancy characterized by a dilation of the calyces, renal pelvis, and ureter occurs in over 90% of pregnant women.[7] This anatomical abnormality may be present until the 16th postpartum week and promotes urinary stasis in the ureter, leading to the development of urinary tract infection. The dilatation of the urinary system is due to the hormonal effects of progesterone, external compression by the gravid uterus, and morphological changes in the ureteral wall. The systemic vasodilatory state, typical of pregnancy, increases renal perfusion and glomerular filtration rate (GFR). The GFR increment causes an increase of uric acid clearance leading to hypouricemia. Proteinuria also increases and urinary protein excretion of 300 mg/day is considered physiological in normal pregnancy. Renal plasma flow can increase up to 85% in the second trimester of pregnancy. The GFR can reach 40%–50% of baseline throughout pregnancy and subsides in the first 3 months postpartum. These hemodynamic abnormalities result in a decrease of serum creatinine in pregnant women to 0.4–0.5 mg/dl. Systematic vasodilation leads to the stimulation of antidiuretic hormone, resulting in a decrease in plasma osmolality and plasma sodium by 4–5 mEq/L.[8] Minute ventilation increases due to progesterone-induced stimulation of the central respiratory center in the brain. This results in a decrease in pCO2 and a mild chronic respiratory alkalosis, which is compensated for renal excretion of bicarbonate. A decrease of about 4 mEq/L in bicarbonate concentration is common in the pregnant women. Table 1 shows anatomical and physiological changes occurring in the kidney of gravid women during normal pregnancy.[9]
Table 1.
Renal changes of normal pregnancy
Diagnosis of Acute Kidney Injury in Pregnancy
Diagnostic definition of renal diseases during pregnancy is not uniform and is highly variable in the literature,[10] and therefore, validated definition of P-AKI is not yet established. The use of the risk, injury, failure, loss of kidney function, and end-stage kidney disease (RIFLE) classification in pregnant women needs further study and is not consensual. The prognostic utility of RIFLE system has been demonstrated in nonpregnant women,[11] but there are few studies reporting its application in pregnancy.[12] Pregnancy is associated with a physiological increase in GFR by 50%–80% accompanied by an increase in plasma volume.[13] Together, these result in a normal gestational fall in serum creatinine, which can easily mask mild AKI. A creatinine level of ≥1 mg/dl or a rapid rise (by definition in 48 h) of 0.5 mg/dl above baseline should be investigated for evidence of AKI. The knowledge of these physiological adaptations in pregnancy is of clinical importance because serum creatinine and blood urea nitrogen of 1.0 mg/dl and 13 mg/dl, respectively, would be considered normal in a nonpregnant individual but reflect renal impairment in a pregnant women.[9] Since a consensus definition of P-AKI has not been established, therefore, the diagnosis of P-AKI is based on increase in serum creatinine. We have used following criteria for diagnosis of AKI in pregnant women (any one of the three); (1) sudden increase in serum creatinine >1 mg/dl, (2) oliguria/anuria, and (3) need for dialysis.[14]
Incidence of Acute Kidney Injury in Pregnancy
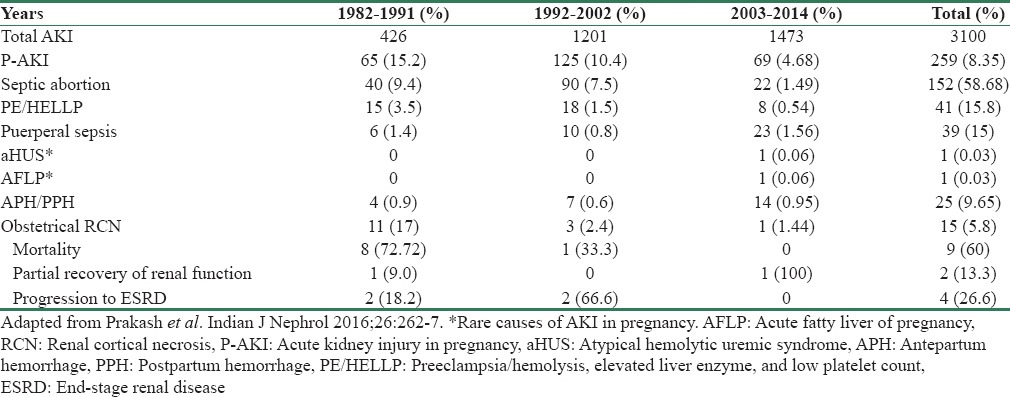
AKI is a rare complication of pregnancy in the developed countries because of markedly decreased incidence of P-AKI over the last three decades. Stratta et al. reported that the incidence of P-AKI in developed countries has declined from 1 in 3000 to 1 in 18,000 pregnancy since the 1960s.[4] In a recent study from Canada, AKI occurred in 1/10,000 pregnancies among 1.9 million pregnant women over a period of 15 years.[15] In contrast, in the developing countries, pregnancy-related complications still account for 15%–25% of total AKI and the most common cause of P-AKI is septic abortion.[16,17,18] Since 1980, P-AKI has declined in developing countries also and obstetrical complications constitute 9%–13% of total AKI cases.[3,18,19] We have reported that in our previous study, the prevalence of P-AKI among all cases of AKI decreased from 15% in the 1980s to 10% in the 1990s.[2] In our recent study, we noted that AKI complicated 1.78% of total delivery (1 in 56 birth) in the third trimester of pregnancy with maternal mortality of 20%.[19] Thus, the incidence of P-AKI is declining even in developing countries[2,5] but still accounts for 5%–8% of total AKI cases in different part of countries.[6,20] Table 2 shows changing trend of P-AKI in the last three decades at our center. The incidence of P-AKI decreased to 10.4% in 1992–2002 from 15.2% in 1982–1991, with declining trend continuing in 2013–2014 (4.68%). We noted that overall, incidence of P-AKI has decreased and preeclampsia (PE) and puerperal sepsis are the common causes of P-AKI [Table 2].[14] The decreasing trend in P-AKI was also noted in other Indian study and sepsis was the most common cause.[21] In contrast to India, a recent study from Pakistan reported rather increase in P-AKI over the last 10 years.[22]
Table 2.
Main causes and outcomes of acute kidney injury in pregnancy in last 33 years
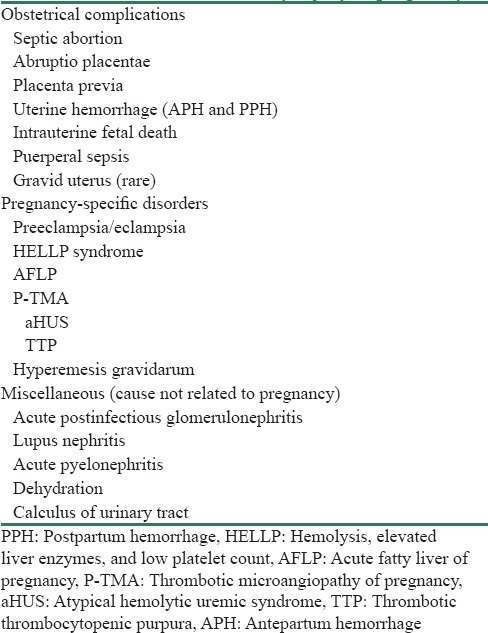
Etiology of Acute Kidney Injury in Pregnancy
Usually, the development of AKI during pregnancy follows a bimodal distribution with two incidence peaks: one in the first trimester caused by septic abortion and other in the third trimester and/or around delivery due to late obstetrical complications. AKI is a heterogeneous syndrome in pregnant women and is caused by multiple etiology. It occurs typically in otherwise healthy women who developed obstetrical complication or acquired pregnancy-related medical condition such as PE and/or hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome. However, several etiologies not related to pregnancy (acute gastroenteritis, malaria, pyelonephritis, lupus nephritis, and acute interstitial nephritis) are reported to cause P-AKI. It is useful to consider the causes of P-AKI in relation to obstetrical complications and pregnancy-associated-specific diseases. Accordingly, we have used following etiological classification of P-AKI. The causes of AKI in pregnant women are divided into three main groups: (1) obstetrical complications, (2) pregnancy-specific disorders, and (3) miscellaneous causes [Table 3].
Table 3.
Causes of acute kidney injury in pregnancy
Causes of Acute Kidney Injury in Pregnancy with Respect to Timing of Pregnancy
The causes of P-AKI are shown in Figure 1 based on their occurrence with respect to the timing of pregnancy. Approximately 75% cases of P-AKI occur during the late third trimester and in the early postpartum. The hypertensive complications of pregnancy, particularly PE and/or HELLP, are the leading causes of P-AKI in most parts of the world, including developing countries.[19,20,23] Approximately 1% of women with severe PE and 3%–15% of women with HELLP syndrome developed AKI. Other causes include septic abortion (first trimester) or puerperal sepsis, antepartum hemorrhage (APH) or postpartum hemorrhage (PPH), intrauterine death, acute fatty liver of pregnancy (AFLP), and thrombotic microangiopathy of pregnancy (P-TMA) [Table 2]. The following pregnancy-specific disorders causing P-AKI are discussed in this review article: (1) PE, (2) HELLP syndrome, (3) AFLP, and (4) P-TMAs, and (5) hyperemesis gravidarum.
Figure 1.
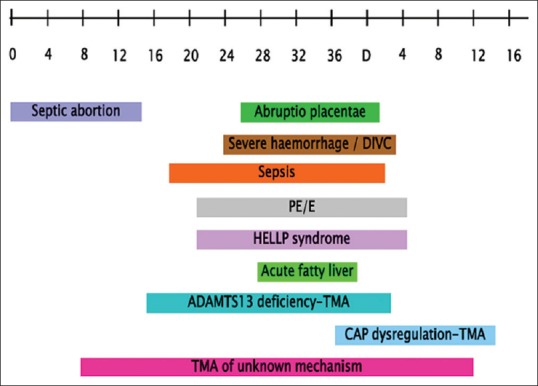
Timing of acute kidney injury with respect to the gestational period of the pregnancy. Atypical hemolytic-uremic syndrome typically occurs in postpartum period
Preeclampsia
Definition and pathogenesis
PE, a multisystem disorder unique to human pregnancy, is characterized by new-onset hypertension (blood pressure >140/90 mmHg) and proteinuria (>300 mg/dl) after 20 weeks of gestation.[24,25,26] The presence of hypertension combined with systemic involvement (such as thrombocytopenia, elevated levels of liver transaminases, renal insufficiency, pulmonary edema, and visual or cerebral disturbances) favors diagnosis of PE in the absence of proteinuria.[27,28] PE occurs mainly during the late second and third trimester, but it may occur up to the time of delivery and even postpartum. It complicates 3%–5% of all pregnancies, but the incidence is higher in primigravid females (7%) and females with certain risk factors such as diabetes mellitus, hypertension, and chronic kidney disease (CKD) (25%).[29,30]
The pathogenesis of PE is not fully understood but involves defects in placentation and systemic endothelial activation. In healthy pregnancy, placentation requires an extensive angiogenesis to establish an adequate and appropriate vascular network to supply fetal needs.[31,32,33] The placenta produces a wide variety of proangiogenic proteins (vascular endothelial growth factor [VEGF] and placental growth factor [PIGF]) and antiangiogenic mediators such as soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sEng); balance of both determines the normal placental development. The circulating concentration of antiangiogenic factors sFlt-1 and sEng are increased in PE. It is hypothesized that increased sFlt-1 effectively reduces the concentration/activity of VEGF, resulting in endothelial dysfunction, hypertension, and proteinuria.[34,35,36] Both sFlt-1 and sEng trigger endothelial dysfunction and severe PE.[37,38,39] Interestingly, coadministration of endoglin and sFlt-1 to pregnant rats leads to renal pathological lesions (i.e., glomerular endotheliosis) which is similar to those lesions noted in patients with PE/eclampsia (PE/E) and AKI.[37] In a rat model of sFlt-1-induced PE, recombinant VEGF-121 ameliorated hypertension and renal damage. These studies support the central role of placental antiangiogenic factors in the pathogenesis of PE.
Clinical features
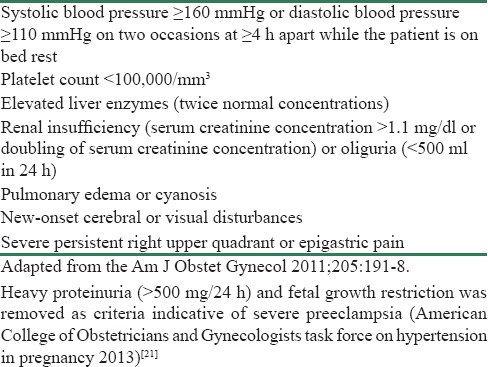
Traditionally, diagnosis of PE is based on new-onset hypertension and proteinuria at ≥20 weeks of gestation or in the absence of proteinuria, hypertension together with evidence of systemic disease (nonproteinuric PE). PE can be classified as early (<34 weeks) or late (≥34 weeks) according to gestational age at diagnosis or delivery [Table 4].[40,41] However, whether early or late PE has different pathogenetic mechanisms or merely gradations of the same underlying condition remains unclear.[42,43] PE can also be classified according to its severity [Table 5];[21,41] some professional organizations have abandoned the term “mild or severe” PE in favor of PE with or without severe features.[27,42,44] It is important to note that massive proteinuria and fetal growth retardation have been removed as indication of severe PE.[27]
Table 4.
Classification of preeclampsia
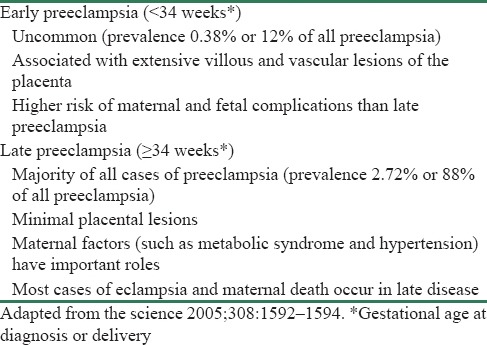
Table 5.
Severe feature of preeclampsia (one or more of these findings)
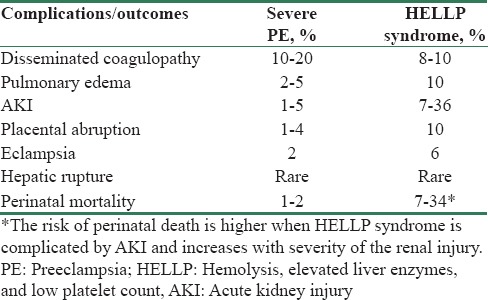
Usually, the clinical manifestations of PE are nonspecific even in severe disease. The most frequently reported symptoms are epigastric or right upper quadrant pain (40%–90% of patients). The other symptoms of PE are nausea, vomiting, headache, blurring of vision, and the sudden onset of edema. Severe PE (PE with severe features) is associated with maternal, fetal, or neonatal complications. The most common maternal complications of PE include (1) disseminated coagulopathy (10%–20%), (2) HELLP syndrome (20%), (3) pulmonary edema (2%–5%), (4) AKI (1%–5%), and (5) placental abruption (1%–2%).[45,46,47] Recent epidemiological studies revealed that PE can lead to several adverse outcomes on long-term follow-up. They include increased risk for CKD and higher risk of cardiovascular disease (chronic hypertension, ischemic heart disease, and stroke).[48,49,50,51]
Renal lesions and acute kidney injury in preeclampsia
The characteristic kidney lesion of PE is swelling and detachment of glomerular endothelial cells. This is often associated with subendothelial deposits, leading to capillary lumina obstruction.[52] PE is associated with altered hemodynamic abnormalities such as decreased renal plasma flow, reduction in GFR by 30%–40%, and renal vasoconstriction. Thus, kidney in preeclamptic women is highly susceptible to ischemic injury. Renal tubular secretion of uric acid is impaired in PE, resulting in elevated concentration of uric acid in the blood.[53] The urine sediment is usually bland. AKI occurs in approximately 1% of women with severe PE. AKI mostly occurs antepartum, but development of AKI in the early postpartum was reported. AKI most often develops in the setting of complication of PE such as placental abruption, disseminated intravascular coagulation (DIC), sepsis, postpartum bleeding, or intrauterine fetal death.[54,55,56] PE/E accounts for 15%–20% of P-AKI cases,[57] and the risk of P-AKI is higher in the setting of early-onset (<32 weeks gestation) PE/E.[58] Kuklina et al. reported that approximately 40% of AKI in pregnant women are caused by severe PE and HELLP syndrome.[59] PE/E was responsible for AKI in 43.9% and 35.3% of cases in pregnant women from India.[19,60] Thus, PE/E is the leading cause of P-AKI worldwide [Figure 1].[61] Reversal of AKI occurs following delivery of fetus in majority of patients with PE. However, persistent renal dysfunction and the need for long-term dialysis suggest preexisting hypertension and CKD.[54,57] The most common histological lesion in the setting of AKI in patients with PE/HELLP syndrome is acute tubular necrosis (ATN).[62,63,64] However, renal cortical necrosis has been reported in preeclamptic women with AKI.[2,19]
Hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome
HELLP syndrome is widely considered a variant of PE and occurs only in pregnant women. It resolves with delivery and is frequently but not always associated with hypertension and proteinuria.[65] It seems to be a distinct disease in view of 20% of pregnant women with HELLP syndrome do not have either hypertension or proteinuria.[65,66] HELLP syndrome was reported to occur in 1–2/10,000 pregnancy,[67] and it may complicate in 20% of women with severe PE.[54,57] The pathogenesis of HELLP syndrome is not fully known. However, increased level of antiangiogenic factors (sFlt-1 and sEng) and decrease concentration of proangiogenic mediators (PIGF) have been proposed in the pathogenesis of HELLP syndrome similar to PE.[68] HELLP syndrome seems to be a TMA-like disorder because of several clinical similarities between these two disorders:[59] mechanical hemolysis, thrombocytopenia, and AKI. The link between HELLP syndrome and complement dysregulation has been suspected in a recent study.[69]
HELLP syndrome occurs typically in the third trimester but may be diagnosed in the second trimester or in the postpartum period.[70] The clinical features are variable. The most common symptoms are epigastric/right upper quadrant pain, nausea, vomiting, and headache, but it may manifest by its complications such as DIC, placental abruption, AKI (7%–36%), pulmonary edema, hepatic capsular hematoma, and retinal detachment.[71,72,73] The diagnosis of HELLP syndrome is based on the following laboratory criteria:[73] (a) microangiopathic hemolytic anemia (MAHA): schistocytes in blood smear, serum bilirubin ≥1.2 mg/dl, lactate dehydrogenase (LDH) >600 U/L; (b) increased liver transaminases (alanine aminotransferase >70 U/L); and (c) platelet count < 100 × 103 cells/mm3. The decreased platelet count in a pregnant women during antenatal checkup may suggest the diagnosis of HELLP syndrome because thrombocytopenia is usually the first indication of this disease.[74,75] Maternal and perinatal outcomes of PE/E and HELLP syndrome are similar. However, certain complications are more frequent in HELLP syndrome in comparison to PE [Table 6][53]. Maternal mortality in HELLP syndrome is 1% and is most often due to cardiopulmonary complications, infection, or ruptured hepatic hematoma.[54] Perinatal mortality in HELLP syndrome ranges from 7% to 34% and depends on gestational age and maternal disease severity.[70]
Table 6.
Maternal and perinatal outcomes in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelet count syndrome
AKI is reported in 3%–15% cases of HELLP syndrome, and overall, it may account for 40% of all cases of P-AKI and may increase up to 60% of cases in severe form of this disease.[55,57,76,77] Dialysis is needed in approximately 10%–46% of patients with HELLP syndrome associated AKI during acute phase. However, even dialysis-requiring AKI has excellent prognosis with complete recovery of renal function in almost all cases.[55,57,78] Thus, majority (93%–100%) of patients with HELLP syndrome-related AKI have near complete reversal of renal function.[55,79,80] The progression to CKD is reported to occur in < 10% of patients who developed AKI on preexisting renal disease and/or hypertension.[79] Thus, prognosis of AKI in patients with HELLP syndrome is favorable. Kidney biopsy study revealed typical feature of TMA in < 15% of patients with HELLP-associated AKI.[63]
Acute fatty liver of pregnancy
AFLP is an obstetric emergency that, if left untreated, progresses to fulminant liver failure. It affects women in the third trimester of pregnancy and is characterized by sudden onset of acute liver failure with coagulopathy. Incidence of AFLP is 1/7000–1/20,000 pregnancies.[80,81] AFLP is an autosomal recessive genetic disorder which causes defective function of long-chain 3-hydroxyacyl-CoA dehydrogenase. This enzyme is involved in mitochondrial fatty acid beta-oxidation. Because of defective oxidation, there is an excessive accumulation of fetal fatty acid, which in turn is released into the maternal circulation. The increased load of long-chain fatty acid is deposited in the liver tissue which leads to impaired hepatic function in the mother.[82] The presence of lipid microvesicles infiltration of the hepatocytes, without inflammation, or necrosis are the typical histological findings in patients with AFLP.
The early presenting symptoms of AFLP are nonspecific with malaise, fever, nausea, vomiting, and abdominal pain. With progression of disease (jaundice and hepatic encephalopathy), other physical signs resolved.[83,84] The low fibrinogen level, prolonged prothrombin time, depressed antithrombin III levels, and thrombocytopenia are the main features of disease which lead to coagulopathy. Hyperbilirubinemia, increased hepatic transaminases, hypoglycemia, and leukocytosis are the other laboratory abnormalities in patients with AFLP. The absence of hypertension supports viral hepatitis rather than AFLP.[85] AFLP is a diagnosis of exclusion once viral hepatitis and biliary obstruction have been excluded. However, half of the patients have concomitant PE/HELLP syndrome, and at an early stage, the differential diagnosis may be difficult.[86] The presence of proteinuria, peripheral edema, and thrombocytopenia may favor diagnosis of PE/HELLP syndrome.[87,88] AKI is seen in 20%–100% of cases and etiology of AKI is multifactorial.[83,84] AKI in patients with AFLP is mostly mild and without need for dialysis support.[89,90] In most women, there is complete liver and kidney recovery after delivery. Renal insufficiency in AFLP is usually nonoliguric although oliguria and ATN can occur in the setting of hemorrhage-induced hypovolemia. The various factors that may contribute for AKI in AFLP include hypovolemia, coexisting PE, coagulopathy, hepatic failure, and intra-abdominal hemorrhage.
The urgent and immediate delivery of fetus is associated with favorable maternal and fetal prognosis. The earlier studies have reported very high (85%) rate of maternal and fetal mortality in women with AFLP.[91] However, the recent case series reported maternal and perinatal mortality ranging between 10% and 20%.[68,88,92,93]
Thrombotic microangiopathies of pregnancy
P-TMA are rare disorders occurring in 1/25,000 pregnancies.[94] TMAs in pregnancy are characterized by thrombi of fibrin and/or platelet in the microvasculature of various organs, endothelial swelling, accumulation of protein, and cell debris in the subendothelial layer and splitting of the glomerular basement membrane in some cases.[95,96,97,98] P-TMA may occur anytime during pregnancy or at puerperium, in previously healthy women. Thrombotic thrombocytopenic purpura (TTP) and hemolytic-uremic syndrome (HUS) may occur de novo with pregnancy, may relapse during pregnancy, and/or may recur with subsequent pregnancies.[99] Pregnancy-related TMA accounts for 8%–18% of all cases of TMA, and it is a secondary form of TMA.[97,98,99,100] P-TMA can be classified into three groups based on underlying pathogenic mechanism: (1) ADAMTS-13 deficiency related, (2) complement alternative pathway (CAP) dysregulation related, and (3) unknown mechanism. Depending on the dominant clinical mode of presentation, two clinical forms of syndrome have been described; (a) TTP and (b) HUS.
Thrombotic thrombocytopenic purpura
The combination of fever, severe thrombocytopenia, MAHA, and predominant neurologic symptoms (disorientation, ataxia, headache, focal deficits, seizures, or aphasia) are the presenting features of TTP.[101] Kidney function is usually normal, or mild renal dysfunction may occur in such patients. TTP is often diagnosed before delivery, especially in the second and third trimester, because the ADAMTS-13 level physiologically tends to be decreased during the last trimester.[102,103] The highest risk of TTP during the late second and third trimester seems to be due to progressive decrease in ADAMTS-13 activity and simultaneous steady increase in plasma concentration of von Willebrand factor during normal gestation.[102] Preliminary data suggest that the monitoring of ADAMTS-13 levels during pregnancy may help to identify patient at risk of TMA relapse.[104,105] Some authors have advocated prophylactic treatment of ADAMTS-13 deficiency using plasma exchange to maintain an enzyme activity of >10% in pregnant women with ADAMTS deficiency.[105]
Atypical hemolytic-uremic syndrome
P-TMA associated with complement activation pathway (CAP) dysregulation clinically presents as atypical HUS (aHUS). Clinical features of aHUS are similar to TTP, but renal involvement is more severe (serum creatinine >2.3 mg/dl) and the neurological manifestation is rare. aHUS occurs mainly in the first 6 months postpartum.[106] Pregnancy and delivery are usually uneventful in majority of the patients. Evidence of CAP dysregulation was reported in 80% of patients among 21 cases of pregnancy-related aHUS (P-aHUS) from the French aHUS Registry.[97] P-TMA caused by CAP dysregulation occurred mainly (80% of cases) during the postpartum period. Infections and bleeding, which frequently complicate the postpartum period, may trigger complement activation leading to TMA (aHUS). Eighty percent of Pregnancy associated Hemolytic uremic syndrome (P-aHUS) had CAP dysregulation with factor H (FH) and factor (FI) encoding gene (CFH and CFI, respectively) mutation, and 80% of patients reached end-stage renal disease during the first aHUS episode.
The counseling of patients with complement gene abnormalities who wish to start a pregnancy remains a difficult issue. The risk of P-aHUS varies according to the underlying complement gene abnormality; this risk was highest (20%–30%) for patients with CFH and C3 mutations and lower (10%–15%) for those patients with CFI and membrane cofactor protein mutation.[101]
Differential diagnosis TMA and AKI in pregnancy
The presence of TMA and AKI in pregnancy is one of the most challenging differential diagnoses. Several pregnancy-specific disorders such as PE/HELLP syndrome, TTP, HUS, and AFLP share many clinical, laboratory, and pathological features [Table 7]. It is difficult to establish clinical distinctions between these entities with certainty on clinical ground alone. However, the exact diagnosis of these pregnancy-specific disorders is mandatory to make appropriate therapeutic decision, which may save the lives of both the mother and the fetus.[74] Delivery of fetus improves the clinical manifestations of AFLP and HELLP syndrome. However, there is no benefit of delivery in patients with P-TMA. Plasma exchange is the first-line treatment for patients with HUS/TTP.
Table 7.
Comparison of clinical and laboratory characteristics of hemolysis, elevated liver enzymes, and low platelet count, thrombotic thrombocytopenic purpura, hemolytic-uremic syndrome, and acute fatty liver of pregnancy
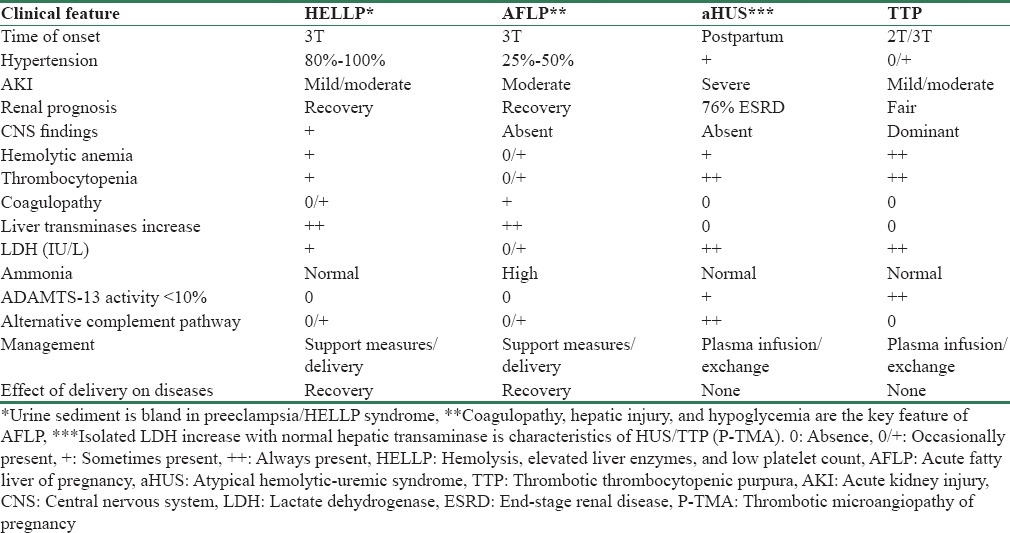
Distinguishing acute fatty liver of pregnancy from HELLP syndrome
Distinguishing AFLP from HELLP syndrome is difficult and challenging because both disorders share many clinical and laboratory features. The situation becomes more complicated and differential diagnosis between AFLP/HELLP syndrome may be impossible because up to 50% of women with AFLP have concomitant PE. However, the clinical distinction between AFLP and HELLP syndrome is of academic importance because prompt delivery of the fetus is appropriate and suitable treatment for both disorders. The clinical clues to distinguish AFLP versus HELLP syndrome are as follows:
Coagulopathy and hypoglycemia are the key features of AFLP
Profoundly depressed antithrombin levels or severe transaminitis suggest AFLP
Thrombocytopenia is either mild or absent in AFLP while it is moderate to severe in HELLP syndrome.
Distinguishing TTP/HUS and HELLP syndrome
The clinical and hematological features of HUS/TTP and PE/HELLP are similar because both have MAHA, thrombocytopenia, and renal disease [Table 7]. Further, concomitant PE/HELLP syndrome may occur in approximately 20% of women with pregnancy-associated TMA. This ambiguity can present a challenge to management as severe PE/HELLP is generally an indication for expedient delivery, while TTP typically responds to plasma exchange, with continuation of the pregnancy for weeks to months. Further, concomitant TTP and PE/HELLP syndrome carry very high (44.4%) maternal mortality. Therefore, both delivery and plasma exchange are probably indicated to optimize chances for maternal survival in this setting. The clinical clues for the diagnosis of pregnancy-associated TTP/HUS are as follows:
The coagulation abnormalities such as elevated antithrombin, elevated D-dimer, and high fibrinogen levels are absent in TTP/HUS while they are common in HELLP syndrome
Isolated LDH increase with normal hepatic transaminase favors HUS/TTP
Severely increased hepatic transaminases level strongly suggests HELLP syndrome.
Hyperemesis gravidarum
Hyperemesis gravidarum is the most common cause of AKI in the first trimester of pregnancy in developed countries but rarely reported from developing countries. We observed no case of AKI complicating hyperemesis gravidarum in our study in the last three decades. Since hyperemesis gravidarum is unique to pregnancy, its clinical feature is presented here. The true incidence of hyperemesis gravidarum has not been documented and may vary from as low as 3/1000 pregnancies to 1/100.[107] It is defined as severe and persistent nausea and vomiting, leading to weight loss, exceeding 5% of the prepregnancy body weight, and ketonuria.[108] These patients present in the first trimester of pregnancy with AKI associated with hypokalemic metabolic alkalosis. Other laboratory abnormalities may include an increase in hematocrit (hemoconcentration), mild elevation in aminotransferases, and mild hyperthyroidism.[109,110] The thyroid-stimulating activity of human chorionic gonadotropin hormone is a possible cause of hyperthyroidism in patients with hyperemesis gravidarum.[109] Symptomatic treatment with antiemetics and intravenous fluids usually corrects the renal function, acid–base, and electrolyte abnormalities.[111]
Treatment of Acute Kidney Injury in Pregnancy
The management of P-AKI includes three considerations: (i) supportive measures to preserve renal function, (ii) dialysis, and (iii) treatment of the underlying pregnancy-specific disease.
Renal function supportive measures
The important general measures to minimize renal injury (such as treatment of etiology, avoidance of nephrotoxic drugs or treatment of an infectious disease) should be started as soon as possible. The second step is administration of intravenous fluids to restore or maintain renal perfusion.[112,113] This procedure also prevents hypovolemia and ensures an adequate uteroplacental perfusion and fetal well-being. These general measures are followed by pharmacological therapy of AKI and its known complications such as hypertension, hyperkalemia, metabolic acidosis, and anemia. Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists are contraindicated in pregnancy and diuretics are not recommended because of the high risk of volume depletion. The use of hydralazine is associated with adverse maternal and fetal outcomes in a recent study.[74] Therefore, the first-line treatment options in pregnant women with hypertension are methyldopa and labetalol.[114] The dihydropyridine calcium-channel blockers can also be used successfully and safely in pregnancy. The administration of insulin, glucose, and ion exchange resin is recommended for the treatment of hyperkalemia. The erythropoiesis-stimulating agent is safe in pregnancy, but higher doses are usually required to obtain the desired therapeutic effect in pregnant women.[115]
Dialysis
The indications for dialysis in P-AKI are similar to the general population, and they include uremic symptoms (encephalopathy, pericarditis, or neuropathy), volume overload, hyperkalemia, and/or metabolic acidosis unresponsive to initial medical treatment. However, early start of dialysis is recommended when GFR falls to below 20 ml/min/1.73 m2.[116] The intermittent hemodialysis is preferred and dialysis of choice in most patients. It is essential to keep certain aspects in mind when dialysis is prescribed in pregnant women with AKI. They include (i) increased dialysis dose (daily dialysis with duration of more than 20 h/week). This will improve the uremic environment, a high risk factor for prematurity and polyhydramnios, and minimize hemodynamic fluctuations of hemodialysis. The hemodialysis-related hemodynamic fluctuation and volume depletion can cause diminished uteroplacental perfusion and increased placental oxidative state[117] and (ii) it is advised to maintain certain dialysis parameters in narrow range in pregnant women, such as bicarbonate to 25 mEq/L and sodium to 135 mEq/L.[118] Both conventional and low molecular weight heparin are safe to use in pregnancy during hemodialysis treatment because they do not cross the placental barrier.[115]
Treatment of the Underlying Pregnancy-specific Diseases
Preeclampsia/HELLP syndrome
The treatment of severe PE/HELLP syndrome depends on illness severity, gestational age, and fetal well-being. Before 24 weeks of gestation, pregnancy discontinuance is recommended since studies show no fetal survival benefit and only increase the risk of severe maternal complications.[71,119] Between 24 and 32 weeks of gestation, expectant management is a reasonable approach.[116] Delivery is the treatment of choice for pregnancy ≥32 weeks.[71,86,120] Some clinical situations are considered indications for prompt delivery regardless of gestational age: worsening maternal conditions, eclampsia, or signs of fetal compromise.[116] Some studies show benefit of corticosteroid therapy in HELLP syndrome. However, the results of the only randomized controlled trial published to date do not show any impact of steroid therapy on length of hospitalization, on the speed of recovery or the development of complications.[74] There is no specific treatment of PE yet available. Thadhani et al. have shown that removal of sFlt-1 from circulation using therapeutic apheresis is associated with proteinuria reduction and prolongation of pregnancy without major adverse maternal or fetal consequences in patients with PE.[121] However, further controlled study is needed to confirm the beneficial effect of apheresis in patients with PE.
Acute fatty liver of pregnancy
The prompt and urgent delivery with supportive care is the essential component in the management of women with AFLP. The glycemic control with glucose administration and correction of coagulopathy with fresh frozen plasma, blood transfusion, or cryoprecipitate will help in stabilization of maternal condition. Hepatic encephalopathy is treated with low protein diet and oral lactulose. Delivery should be induced immediately to avoid progression to liver failure. Interventions such as mechanical ventilation and parenteral nutrition may be needed in more severe cases. Since most cases resolve spontaneously after delivery, liver transplantation is rarely needed.[122,123] Maternal and fetal mortality rates were as high as 85% in pregnancies complicated by AFLP in earlier reports.[91] However, recent case series report much lower maternal mortality (0%–12.5%). Overall, fetal and perinatal mortality rates have also improved ranging between 6.6% and 15% with improvement in health care.[81,86,88] Recurrence of AFLP is rare in subsequent pregnancies; only four cases of recurrent AFLP are reported in the literature.[124,125]
Pregnancy-associated thrombotic microangiopathies
The treatment of TMA occurring during pregnancy should be tailored to the underlying pathogenic mechanisms. The treatment of TTP includes fresh frozen plasma infusion and plasmapheresis to correct ADAMTS-13 deficiency and remove the ADAMTS-13 circulating antibodies.[110] In suspected case of autoimmune ADAMTS-13 deficiency, steroids are recommended as initial immunosuppressive therapy. The B-cell depleting antibody rituximab is probably the optimal second-line therapy for cases resistant to plasma exchange or fresh frozen plasma infusion.[102] However, potential fetal toxicity associated with rituximab is of concern.[126,127] Treatment of aHUS also includes plasma infusion and plasma exchange to restore the missing mediators (factor H and I) and remove anti-factor H.[95,128] In approximately 50% of patients, renal function does not improve during their first episode of aHUS with plasma exchange therapy.[102] The criteria use to define aHUS resistant to plasma exchange therapy include (i) the absence of platelet count increase, (ii) absence of LDH level decrease, and (iii) absence of significant decrease (>25%) of serum creatinine, despite 3–5 plasma exchange. The use of potent inhibitor of CAP activation is indicated for cases resistant to plasma therapy. The optimal first line of the current treatment for patients with aHUS is eculizumab (monoclonal humanized IgG antibody) regardless of evidence of underlying CAP dysregulation. Eculizumab is a powerful inhibitor of C5 and thus prevents the generation of C5a and C5b.[129,130] The standard eculizumab regimen includes 4 weekly 900 mg infusions, followed by 1200 mg infusion every fortnight. Eculizumab is the most expensive drug in the world, with an annual cost of treatment being around $500,000/patients. Hence, the use of eculizumab may vary in different countries and institutions because of economic constraints. Response to therapy is indicated by normalization of platelet count and LDH level and atleast 25% decrease of serum creatinine. The potential fetotoxicity of eculizumab is usually not a concern in P-HUS because it most frequently occurs after delivery. Platelet transfusions should be avoided if possible because of risk of increased microvascular thrombosis. The maternal mortality in P-TMA has declined in recent years and is now between 10% and 20%.[128]
Conclusions
The management of P-AKI is a major clinical challenge because it poses a risk to two lives (mother and fetus). It is largely due to preventable obstetrical complications but can be caused by certain pregnancy-specific diseases. Pregnancy hypertensive complications, notably PE/HELLP syndrome, are the leading cause of P-AKI worldwide. TMA (aHUS/TTP) is a clinically challenging but fortunately rare causes of P-AKI. Puerperal sepsis and obstetrical hemorrhage (APH and PPH) still account for AKI in the postpartum period in addition to PE/HELLP syndrome in developing countries. The implementation of specific interventions for the prevention and management of sepsis and hypertensive complications in pregnant women may reduce the burden of P-AKI in developing countries. Fortunately, overall, incidence of P-AKI has probably decreased in developing countries with improved maternal prognosis. However, fetal mortality is still very high even in developed countries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This article is dedicated to the mentor and supervisor Prof. Pramod K. Srivastava MD, DCH, Former Professor, Department of General Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi - 221 005, India.
References
- 1.Jayakumar M, Prabahar MR, Fernando EM, Manorajan R, Venkatraman R, Balaraman V. Epidemiologic trend changes in acute renal failure – A tertiary center experience from South India. Ren Fail. 2006;28:405–10. doi: 10.1080/08860220600689034. [DOI] [PubMed] [Google Scholar]
- 2.Prakash J, Kumar H, Sinha DK, Kedalaya PG, Pandey LK, Srivastava PK, et al. Acute renal failure in pregnancy in a developing country: Twenty years of experience. Ren Fail. 2006;28:309–13. doi: 10.1080/08860220600583658. [DOI] [PubMed] [Google Scholar]
- 3.Selcuk NY, Tonbul HZ, San A, Odabas AR. Changes in frequency and etiology of acute renal failure in pregnancy (1980-1997) Ren Fail. 1998;20:513–7. doi: 10.3109/08860229809045140. [DOI] [PubMed] [Google Scholar]
- 4.Stratta P, Besso L, Canavese C, Grill A, Todros T, Benedetto C, et al. Is pregnancy-related acute renal failure a disappearing clinical entity? Ren Fail. 1996;18:575–84. doi: 10.3109/08860229609047680. [DOI] [PubMed] [Google Scholar]
- 5.Prakash J, Vohra R, Wani IA, Murthy AS, Srivastva PK, Tripathi K, et al. Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing countries: A single-centre experience of 22 years from Eastern India. Nephrol Dial Transplant. 2007;22:1213–7. doi: 10.1093/ndt/gfl761. [DOI] [PubMed] [Google Scholar]
- 6.Kumar KS, Krishna CR, Kumar VS. Pregnancy related acute renal failure. J Obstet Gynaecol India. 2006;56:308–10. [Google Scholar]
- 7.Rasmussen PE, Nielsen FR. Hydronephrosis during pregnancy: A literature survey. Eur J Obstet Gynecol Reprod Biol. 1988;27:249–59. doi: 10.1016/0028-2243(88)90130-x. [DOI] [PubMed] [Google Scholar]
- 8.Lindheimer MD, Barron WM, Davison JM. Osmoregulation of thirst and vasopressin release in pregnancy. Am J Physiol. 1989;257(2 Pt 2):F159–69. doi: 10.1152/ajprenal.1989.257.2.F159. [DOI] [PubMed] [Google Scholar]
- 9.Maynard SE, Karumanchi SA, Thadhani R. Hypertension and kidney disease in pregnancy. In: Brenner BM, Rector B, editors. The Kidney. 8th ed. Philadelphia: Saunders, Elsevier; 2008. pp. 1567–95. [Google Scholar]
- 10.Piccoli GB, Conijn A, Attini R, Biolcati M, Bossotti C, Consiglio V, et al. Pregnancy in chronic kidney disease: Need for a common language. J Nephrol. 2011;24:282–99. doi: 10.5301/JN.2011.7978. [DOI] [PubMed] [Google Scholar]
- 11.Abosaif NY, Tolba YA, Heap M, Russell J, El Nahas AM. The outcome of acute renal failure in the intensive care unit according to RIFLE: Model application, sensitivity, and predictability. Am J Kidney Dis. 2005;46:1038–48. doi: 10.1053/j.ajkd.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Silva GB, Jr, Monteiro FA, Mota RM, Paiva JG, Correia JW, Bezerra Filho JG, et al. Acute kidney injury requiring dialysis in obstetric patients: A series of 55 cases in Brazil. Arch Gynecol Obstet. 2009;279:131–7. doi: 10.1007/s00404-008-0682-8. [DOI] [PubMed] [Google Scholar]
- 13.Dunlop W. Serial changes in renal haemodynamics during normal human pregnancy. Br J Obstet Gynaecol. 1981;88:1–9. doi: 10.1111/j.1471-0528.1981.tb00929.x. [DOI] [PubMed] [Google Scholar]
- 14.Prakash J, Pant P, Prakash S, Sivasankar M, Vohra R, Doley PK, et al. Changing picture of acute kidney injury in pregnancy: Study of 259 cases over a period of 33 years. Indian J Nephrol. 2016;26:262–7. doi: 10.4103/0971-4065.161018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hildebrand AM, Liu K, Shariff SZ, Ray JG, Sontrop JM, Clark WF, et al. Characteristics and outcomes of AKI treated with dialysis during pregnancy and the postpartum period. J Am Soc Nephrol. 2015;26:3085–91. doi: 10.1681/ASN.2014100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prakash J, Tripathi K, Usha, Pandey LK, Srivastava PK. Pregnancy related acute renal failure in Eastern India. J Nephrol. 1995;8:214–8. [Google Scholar]
- 17.Chugh KS, Sakhuja V, Malhotra HS, Pereira BJ. Changing trends in acute renal failure in third-world countries – Chandigarh study. Q J Med. 1989;73:1117–23. [PubMed] [Google Scholar]
- 18.Prakash J, Tripathi K, Singh RG. Acute renal failure in pregnancy. J Obstet Gynaecol India. 1985;35:233–8. [Google Scholar]
- 19.Prakash J, Niwas SS, Parekh A, Pandey LK, Sharatchandra L, Arora P, et al. Acute kidney injury in late pregnancy in developing countries. Ren Fail. 2010;32:309–13. doi: 10.3109/08860221003606265. [DOI] [PubMed] [Google Scholar]
- 20.Goplani KR, Shah PR, Gera DN, Gumber M, Dabhi M, Feroz A, et al. Pregnancy-related acute renal failure: A single-center experience. Indian J Nephrol. 2008;18:17–21. doi: 10.4103/0971-4065.41283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gopalakrishnan N, Dhanapriya J, Muthukumar P, Sakthirajan R, Dineshkumar T, Thirumurugan S, et al. Acute kidney injury in pregnancy – A single center experience. Ren Fail. 2015;37:1476–80. doi: 10.3109/0886022X.2015.1074493. [DOI] [PubMed] [Google Scholar]
- 22.Naqvi R, Ahmed E, Sheikh R, Rizvi A. Obstetrical acute kidney injury: 25 years experience from nephrology care unit in Pakistan. Open Access Libr J. 2015;2:1–7. [Google Scholar]
- 23.Arora N, Mahajan K, Jana N, Taraphder A. Pregnancy-related acute renal failure in Eastern India. Int J Gynaecol Obstet. 2010;111:213–6. doi: 10.1016/j.ijgo.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 24.Roberts JM, Gammill HS. Preeclampsia: Recent insights. Hypertension. 2005;46:1243–9. doi: 10.1161/01.HYP.0000188408.49896.c5. [DOI] [PubMed] [Google Scholar]
- 25.Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R. Pre-eclampsia part 1: Current understanding of its pathophysiology. Nat Rev Nephrol. 2014;10:466–80. doi: 10.1038/nrneph.2014.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Streegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Preeclampsia. Lancet. 2010;736:631–44. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 27.American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–31. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 28.Lowe SA, Brown MA, Dekker GA, Gatt S, McLintock CK, McMahon LP, et al. Guidelines for the management of hypertensive disorders of pregnancy 2008. Aust N Z J Obstet Gynaecol. 2009;49:242–6. doi: 10.1111/j.1479-828X.2009.01003.x. [DOI] [PubMed] [Google Scholar]
- 29.Prakash J. The kidney in pregnancy: A journey of three decades. Indian J Nephrol. 2012;22:159–67. doi: 10.4103/0971-4065.98750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Umans JG. Obstetric nephrology: Preeclampsia – The nephrologist's perspective. Clin J Am Soc Nephrol. 2012;7:2107–13. doi: 10.2215/CJN.05470512. [DOI] [PubMed] [Google Scholar]
- 31.Karumanchi SA, Maynard SE, Stillman IE, Epstein FH, Sukhatme VP. Preeclampsia: A renal perspective. Kidney Int. 2005;67:2101–13. doi: 10.1111/j.1523-1755.2005.00316.x. [DOI] [PubMed] [Google Scholar]
- 32.Yagel S. Angiogenesis in gestational vascular complications. Thromb Res. 2011;127(Suppl 3):S64–6. doi: 10.1016/S0049-3848(11)70018-4. [DOI] [PubMed] [Google Scholar]
- 33.Maynard S, Epstein FH, Karumanchi SA. Preeclampsia and angiogenic imbalance. Annu Rev Med. 2008;59:61–78. doi: 10.1146/annurev.med.59.110106.214058. [DOI] [PubMed] [Google Scholar]
- 34.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350:672–83. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 35.Silasi M, Cohen B, Karumanchi SA, Rana S. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin North Am. 2010;37:239–53. doi: 10.1016/j.ogc.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 36.Kita N, Mitsushita J. A possible placental factor for preeclampsia: SFlt-1. Curr Med Chem. 2008;15:711–5. doi: 10.2174/092986708783885309. [DOI] [PubMed] [Google Scholar]
- 37.Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12:642–9. doi: 10.1038/nm1429. [DOI] [PubMed] [Google Scholar]
- 38.Chen Y. Novel angiogenic factors for predicting preeclampsia: sFlt-1, PIGF and soluble endoglin. Open Clin Chem J. 2009;2:1–6. [Google Scholar]
- 39.Foidart JM, Schaaps JP, Chantraine F, Munaut C, Lorquet S. Dysregulation of anti-angiogenic agents (sFlt-1, PLGF, and sEndoglin) in preeclampsia – A step forward but not the definitive answer. J Reprod Immunol. 2009;82:106–11. doi: 10.1016/j.jri.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 40.Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005;308:1592–4. doi: 10.1126/science.1111726. [DOI] [PubMed] [Google Scholar]
- 41.von Dadelszen P, Magee LA, Roberts JM. Subclassification of preeclampsia. Hypertens Pregnancy. 2003;22:143–8. doi: 10.1081/PRG-120021060. [DOI] [PubMed] [Google Scholar]
- 42.Ogge G, Chaiworapongsa T, Romero R, Hussein Y, Kusanovic JP, Yeo L, et al. Placental lesions associated with maternal underperfusion are more frequent in early-onset than in late-onset preeclampsia. J Perinat Med. 2011;39:641–52. doi: 10.1515/JPM.2011.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sibai BM. Evaluation and management of severe preeclampsia before 34 weeks’ gestation. Am J Obstet Gynecol. 2011;205:191–8. doi: 10.1016/j.ajog.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 44.Lindheimer MD, Roberts JM, Cunningham GC, Chesley L. Introduction, History, Controversies and Definitions. In: Lindheimer MD, Roberts JM, Cunningham GC, editors. Chesley's Hypertensive Disorders in Pregnancy. Oxford (UK): Elsevier; 2009. pp. 1–24. [Google Scholar]
- 45.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365:785–99. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 46.Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, et al. Pregnancy outcomes in healthy nulliparas who developed hypertension. Calcium for preeclampsia prevention study group. Obstet Gynecol. 2000;95:24–8. doi: 10.1016/s0029-7844(99)00462-7. [DOI] [PubMed] [Google Scholar]
- 47.Bombrys AE, Barton JR, Nowacki EA, Habli M, Pinder L, How H, et al. Expectant management of severe preeclampsia at less than 27 weeks’ gestation: Maternal and perinatal outcomes according to gestational age by weeks at onset of expectant management. Am J Obstet Gynecol. 2008;199:247.e1–6. doi: 10.1016/j.ajog.2008.06.086. [DOI] [PubMed] [Google Scholar]
- 48.Romundstad PR, Magnussen EB, Smith GD, Vatten LJ. Hypertension in pregnancy and later cardiovascular risk: Common antecedents? Circulation. 2010;122:579–84. doi: 10.1161/CIRCULATIONAHA.110.943407. [DOI] [PubMed] [Google Scholar]
- 49.Terry MB, Perrin M, Salafia CM, Zhang FF, Neugut AI, Teitelbaum SL, et al. Preeclampsia, pregnancy-related hypertension, and breast cancer risk. Am J Epidemiol. 2007;165:1007–14. doi: 10.1093/aje/kwk105. [DOI] [PubMed] [Google Scholar]
- 50.Strobl I, Windbichler G, Strasak A, Weiskopf-Schwendinger V, Schweigmann U, Ramoni A, et al. Left ventricular function many years after recovery from pre-eclampsia. BJOG. 2011;118:76–83. doi: 10.1111/j.1471-0528.2010.02780.x. [DOI] [PubMed] [Google Scholar]
- 51.Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359:800–9. doi: 10.1056/NEJMoa0706790. [DOI] [PubMed] [Google Scholar]
- 52.Thornton JG, Macdonald AM. Twin mothers, pregnancy hypertension and preeclampsia. Br J Obstet Gynaecol. 1999;106:570–5. doi: 10.1111/j.1471-0528.1999.tb08326.x. [DOI] [PubMed] [Google Scholar]
- 53.Koopmans CM, van Pampus MG, Groen H, Aarnoudse JG, van den Berg PP, Mol BW. Accuracy of serum uric acid as a predictive test for maternal complications in pre-eclampsia: Bivariate meta-analysis and decision analysis. Eur J Obstet Gynecol Reprod Biol. 2009;146:8–14. doi: 10.1016/j.ejogrb.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 54.Sibai BM, Ramadan MK. Acute renal failure in pregnancies complicated by hemolysis, elevated liver enzymes, and low platelets. Am J Obstet Gynecol. 1993;168(6 Pt 1):1682–7. doi: 10.1016/0002-9378(93)90678-c. [DOI] [PubMed] [Google Scholar]
- 55.Gul A, Aslan H, Cebeci A, Polat I, Ulusoy S, Ceylan Y. Maternal and fetal outcomes in HELLP syndrome complicated with acute renal failure. Ren Fail. 2004;26:557–62. doi: 10.1081/jdi-200031750. [DOI] [PubMed] [Google Scholar]
- 56.Haddad B, Barton JR, Livingston JC, Chahine R, Sibai BM. Risk factors for adverse maternal outcomes among women with HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Am J Obstet Gynecol. 2000;183:444–8. doi: 10.1067/mob.2000.105915. [DOI] [PubMed] [Google Scholar]
- 57.Drakeley AJ, Le Roux PA, Anthony J, Penny J. Acute renal failure complicating severe preeclampsia requiring admission to an obstetric intensive care unit. Am J Obstet Gynecol. 2002;186:253–6. doi: 10.1067/mob.2002.120279. [DOI] [PubMed] [Google Scholar]
- 58.Mattar F, Sibai BM. Eclampsia. VIII. Risk factors for maternal morbidity. Am J Obstet Gynecol. 2000;182:307–12. doi: 10.1016/s0002-9378(00)70216-x. [DOI] [PubMed] [Google Scholar]
- 59.Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113:1299–306. doi: 10.1097/AOG.0b013e3181a45b25. [DOI] [PubMed] [Google Scholar]
- 60.Packham DK, Mathews DC, Fairley KF, Whitworth JA, Kincaid-Smith PS. Morphometric analysis of pre-eclampsia in women biopsied in pregnancy and post-partum. Kidney Int. 1988;34:704–11. doi: 10.1038/ki.1988.236. [DOI] [PubMed] [Google Scholar]
- 61.Fakhouri F, Vercel C, Frémeaux-Bacchi V. Obstetric nephrology: AKI and thrombotic microangiopathies in pregnancy. Clin J Am Soc Nephrol. 2012;7:2100–6. doi: 10.2215/CJN.13121211. [DOI] [PubMed] [Google Scholar]
- 62.Kahra K, Draganov B, Sund S, Hovig T. Postpartum renal failure: A complex case with probable coexistence of hemolysis, elevated liver enzymes, low platelet count, and hemolytic uremic syndrome. Obstet Gynecol. 1998;92(4 Pt 2):698–700. doi: 10.1016/s0029-7844(98)00196-3. [DOI] [PubMed] [Google Scholar]
- 63.Abraham KA, Kennelly M, Dorman AM, Walshe JJ. Pathogenesis of acute renal failure associated with the HELLP syndrome: A case report and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2003;108:99–102. doi: 10.1016/s0301-2115(02)00352-4. [DOI] [PubMed] [Google Scholar]
- 64.Fang JT, Chen YC, Huang CC. Unusual presentation of mesangial proliferative glomerulonephritis in HELLP syndrome associated with acute renal failure. Ren Fail. 2000;22:641–6. doi: 10.1081/jdi-100100905. [DOI] [PubMed] [Google Scholar]
- 65.Sibai BM. Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Obstet Gynecol. 2004;103(5 Pt 1):981–91. doi: 10.1097/01.AOG.0000126245.35811.2a. [DOI] [PubMed] [Google Scholar]
- 66.Barton JR, Sibai BM. Gastrointestinal complications of pre-eclampsia. Semin Perinatol. 2009;33:179–88. doi: 10.1053/j.semperi.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 67.Pan C, Perumalswami PV. Pregnancy-related liver diseases. Clin Liver Dis. 2011;15:199–208. doi: 10.1016/j.cld.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 68.Joshi D, James A, Quaglia A, Westbrook RH, Heneghan MA. Liver disease in pregnancy. Lancet. 2010;375:594–605. doi: 10.1016/S0140-6736(09)61495-1. [DOI] [PubMed] [Google Scholar]
- 69.Fakhouri F, Jablonski M, Lepercq J, Blouin J, Benachi A, Hourmant M, et al. Factor H, membrane cofactor protein, and factor I mutations in patients with hemolysis, elevated liver enzymes, and low platelet count syndrome. Blood. 2008;112:4542–5. doi: 10.1182/blood-2008-03-144691. [DOI] [PubMed] [Google Scholar]
- 70.Picinni P, Gallo G. Diagnosis and management of HELLP syndrome. In: Ronco C, Bellomo R, Kellum J, editors. Critical Care Nephrology. 2nd ed. Philadelphia, PA: Saunders; 2009. pp. 337–40. [Google Scholar]
- 71.Hu Y, Dutz JP, MacCalman CD, Yong P, Tan R, von Dadelszen P. Decidual NK cells alter in vitro first trimester extravillous cytotrophoblast migration: A role for IFN-gamma. J Immunol. 2006;177:8522–30. doi: 10.4049/jimmunol.177.12.8522. [DOI] [PubMed] [Google Scholar]
- 72.Haram K, Svendsen E, Abildgaard U. The HELLP syndrome: Clinical issues and management. A review. BMC Pregnancy Childbirth. 2009;9:8. doi: 10.1186/1471-2393-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baxter JK, Weinstein L. HELLP syndrome: The state of the art. Obstet Gynecol Surv. 2004;59:838–45. doi: 10.1097/01.ogx.0000146948.19308.c5. [DOI] [PubMed] [Google Scholar]
- 74.Ganesan C, Maynard SE. Acute kidney injury in pregnancy: The thrombotic microangiopathies. J Nephrol. 2011;24:554–63. doi: 10.5301/JN.2011.6250. [DOI] [PubMed] [Google Scholar]
- 75.Reyes H, Sandoval L, Wainstein A, Ribalta J, Donoso S, Smok G, et al. Acute fatty liver of pregnancy: A clinical study of 12 episodes in 11 patients. Gut. 1994;35:101–6. doi: 10.1136/gut.35.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Haddad B, Barton JR, Livingston JC, Chahine R, Sibai BM. HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome versus severe preeclampsia: Onset at ≤28.0 weeks’ gestation. Am J Obstet Gynecol. 2000;183:1475–9. doi: 10.1067/mob.2000.106975. [DOI] [PubMed] [Google Scholar]
- 77.Abraham KA, Connolly G, Farrell J, Walshe JJ. The HELLP syndrome, a prospective study. Ren Fail. 2001;23:705–13. doi: 10.1081/jdi-100107367. [DOI] [PubMed] [Google Scholar]
- 78.Celik C, Gezginç K, Altintepe L, Tonbul HZ, Yaman ST, Akyürek C, et al. Results of the pregnancies with HELLP syndrome. Ren Fail. 2003;25:613–8. doi: 10.1081/jdi-120022553. [DOI] [PubMed] [Google Scholar]
- 79.Sibai BM, Ramadan MK, Usta I, Salama M, Mercer BM, Friedman SA. Maternal morbidity and mortality in 442 pregnancies with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome) Am J Obstet Gynecol. 1993;169:1000–6. doi: 10.1016/0002-9378(93)90043-i. [DOI] [PubMed] [Google Scholar]
- 80.Selçuk NY, Odabas AR, Cetinkaya R, Tonbul HZ, San A. Outcome of pregnancies with HELLP syndrome complicated by acute renal failure (1989-1999) Ren Fail. 2000;22:319–27. doi: 10.1081/jdi-100100875. [DOI] [PubMed] [Google Scholar]
- 81.Knight M, Nelson-Piercy C, Kurinczuk JJ, Spark P, Brocklehurst P UK Obstetric Surveillance System. A prospective national study of acute fatty liver of pregnancy in the UK. Gut. 2008;57:951–6. doi: 10.1136/gut.2008.148676. [DOI] [PubMed] [Google Scholar]
- 82.Lee NM, Brady CW. Liver disease in pregnancy. World J Gastroenterol. 2009;15:897–906. doi: 10.3748/wjg.15.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Castro MA, Fassett MJ, Reynolds TB, Shaw KJ, Goodwin TM. Reversible peripartum liver failure: A new perspective on the diagnosis, treatment, and cause of acute fatty liver of pregnancy, based on 28 consecutive cases. Am J Obstet Gynecol. 1999;181:389–95. doi: 10.1016/s0002-9378(99)70567-3. [DOI] [PubMed] [Google Scholar]
- 84.Usta IM, Barton JR, Amon EA, Gonzalez A, Sibai BM. Acute fatty liver of pregnancy: An experience in the diagnosis and management of fourteen cases. Am J Obstet Gynecol. 1994;171:1342–7. doi: 10.1016/0002-9378(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 85.Devarbhavi H, Kremers WK, Dierkhising R, Padmanabhan L. Pregnancy-associated acute liver disease and acute viral hepatitis: Differentiation, course and outcome. J Hepatol. 2008;49:930–5. doi: 10.1016/j.jhep.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 86.Guntupalli SR, Steingrub J. Hepatic disease and pregnancy: An overview of diagnosis and management. Crit Care Med. 2005;33(10 Suppl):S332–9. doi: 10.1097/01.ccm.0000182555.39644.7f. [DOI] [PubMed] [Google Scholar]
- 87.Pereira SP, O’Donohue J, Wendon J, Williams R. Maternal and perinatal outcome in severe pregnancy-related liver disease. Hepatology. 1997;26:1258–62. doi: 10.1002/hep.510260525. [DOI] [PubMed] [Google Scholar]
- 88.Santana L, Hernández Medina E, O’Shanahan G, Sánchez-Palacios M. Acute renal failure in acute fatty liver of pregnancy: Apropos of a case. Nefrologia. 2005;25:453–4. [PubMed] [Google Scholar]
- 89.Koroshi A, Babameto A. Acute renal failure during acute fatty liver of pregnancy. Nephrol Dial Transplant. 2002;17:1110–2. doi: 10.1093/ndt/17.6.1110. [DOI] [PubMed] [Google Scholar]
- 90.Kaplan MM. Acute fatty liver of pregnancy. N Engl J Med. 1985;313:367–70. doi: 10.1056/NEJM198508083130606. [DOI] [PubMed] [Google Scholar]
- 91.Fesenmeier MF, Coppage KH, Lambers DS, Barton JR, Sibai BM. Acute fatty liver of pregnancy in 3 tertiary care centers. Am J Obstet Gynecol. 2005;192:1416–9. doi: 10.1016/j.ajog.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 92.Ko H, Yoshida EM. Acute fatty liver of pregnancy. Can J Gastroenterol. 2006;20:25–30. doi: 10.1155/2006/638131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Westbrook RH, Yeoman AD, Joshi D, Heaton ND, Quaglia A, O’Grady JG, et al. Outcomes of severe pregnancy-related liver disease: Refining the role of transplantation. Am J Transplant. 2010;10:2520–6. doi: 10.1111/j.1600-6143.2010.03301.x. [DOI] [PubMed] [Google Scholar]
- 94.Matthews JH, Benjamin S, Gill DS, Smith NA. Pregnancy-associated thrombocytopenia: Definition, incidence and natural history. Acta Haematol. 1990;84:24–9. doi: 10.1159/000205022. [DOI] [PubMed] [Google Scholar]
- 95.Fakhouri F, Frémeaux-Bacchi V. Does hemolytic uremic syndrome differ from thrombotic thrombocytopenic purpura? Nat Clin Pract Nephrol. 2007;3:679–87. doi: 10.1038/ncpneph0670. [DOI] [PubMed] [Google Scholar]
- 96.Noris M, Remuzzi G. Thrombotic microangiopathy after kidney transplantation. Am J Transplant. 2010;10:1517–23. doi: 10.1111/j.1600-6143.2010.03156.x. [DOI] [PubMed] [Google Scholar]
- 97.Fakhouri F, Roumenina L, Provot F, Sallée M, Caillard S, Couzi L, et al. Pregnancy-associated hemolytic uremic syndrome revisited in the era of complement gene mutations. J Am Soc Nephrol. 2010;21:859–67. doi: 10.1681/ASN.2009070706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kremer Hovinga JA, Vesely SK, Terrell DR, Lämmle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115:1500–11. doi: 10.1182/blood-2009-09-243790. [DOI] [PubMed] [Google Scholar]
- 99.Veyradier A, Obert B, Houllier A, Meyer D, Girma JP. Specific von Willebrand factor-cleaving protease in thrombotic microangiopathies: A study of 111 cases. Blood. 2001;98:1765–72. doi: 10.1182/blood.v98.6.1765. [DOI] [PubMed] [Google Scholar]
- 100.Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010;5:1844–59. doi: 10.2215/CJN.02210310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.George JN. The thrombotic thrombocytopenic purpura and hemolytic uremic syndromes: Evaluation, management, and long-term outcomes experience of the Oklahoma TTP-HUS Registry, 1989-2007. Kidney Int Suppl. 2009;75:S52–4. doi: 10.1038/ki.2008.622. [DOI] [PubMed] [Google Scholar]
- 102.George JN. The association of pregnancy with thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Curr Opin Hematol. 2003;10:339–44. doi: 10.1097/00062752-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 103.Mannucci PM, Canciani MT, Forza I, Lussana F, Lattuada A, Rossi E. Changes in health and disease of the metalloprotease that cleaves von Willebrand factor. Blood. 2001;98:2730–5. doi: 10.1182/blood.v98.9.2730. [DOI] [PubMed] [Google Scholar]
- 104.Raman R, Yang S, Wu HM, Cataland SR. ADAMTS13 activity and the risk of thrombotic thrombocytopenic purpura relapse in pregnancy. Br J Haematol. 2011;153:277–9. doi: 10.1111/j.1365-2141.2010.08558.x. [DOI] [PubMed] [Google Scholar]
- 105.Scully M, Starke R, Lee R, Mackie I, Machin S, Cohen H. Successful management of pregnancy in women with a history of thrombotic thrombocytopaenic purpura. Blood Coagul Fibrinolysis. 2006;17:459–63. doi: 10.1097/01.mbc.0000240918.65306.20. [DOI] [PubMed] [Google Scholar]
- 106.Ruggenenti P, Cravedi P, Remuzzi G. Thrombotic microangiopathies including hemolytic uremic syndrome. In: Floege J, Johnson R, Feehally J, editors. Comprehensive Clinical Nephrology. 4th ed. Philadelphia, PA: Mosby; 2010. pp. 344–55. [Google Scholar]
- 107.Källén B. Hyperemesis during pregnancy and delivery outcome: A registry study. Eur J Obstet Gynecol Reprod Biol. 1987;26:291–302. doi: 10.1016/0028-2243(87)90127-4. [DOI] [PubMed] [Google Scholar]
- 108.Goodwin TM. Hyperemesis gravidarum. Clin Obstet Gynecol. 1998;41:597–605. doi: 10.1097/00003081-199809000-00014. [DOI] [PubMed] [Google Scholar]
- 109.Abell TL, Riely CA. Hyperemesis gravidarum. Gastroenterol Clin North Am. 1992;21:835–49. [PubMed] [Google Scholar]
- 110.Goodwin TM, Montoro M, Mestman JH, Pekary AE, Hershman JM. The role of chorionic gonadotropin in transient hyperthyroidism of hyperemesis gravidarum. J Clin Endocrinol Metab. 1992;75:1333–7. doi: 10.1210/jcem.75.5.1430095. [DOI] [PubMed] [Google Scholar]
- 111.Krane NK. Acute renal failure in pregnancy. Arch Intern Med. 1988;148:2347–57. [PubMed] [Google Scholar]
- 112.Jeong JY, Kim SH, Lee HJ, Sim JS. Atypical low-signal-intensity renal parenchyma: Causes and patterns. Radiographics. 2002;22:833–46. doi: 10.1148/radiographics.22.4.g02jl04833. [DOI] [PubMed] [Google Scholar]
- 113.Brown M, Mangos G, Peek M, Plaat F. Renal disease in pregnancy. In: Powrin R, Greene M, Camman W, editors. De Swiet's Medical Disorders in Obstetric Practice. 5th ed. Oxford: Wiley-Blackwell; 2010. [Google Scholar]
- 114.Vidaeff AC, Carroll MA, Ramin SM. Acute hypertensive emergencies in pregnancy. Crit Care Med. 2005;33(10 Suppl):S307–12. doi: 10.1097/01.ccm.0000183163.33710.37. [DOI] [PubMed] [Google Scholar]
- 115.Anantharaman P, Schmidt R, Holley J. Pregnancy and renal diseases. In: Nissenson A, Berns J, Lerma E, editors. Current Diagnosis and Treatment: Nephrology and Hypertension. USA: Mc-Graw-Hill International Edition; 2009. pp. 497–8. [Google Scholar]
- 116.Krane NK, Hamrahian M. Pregnancy: Kidney diseases and hypertension. Am J Kidney Dis. 2007;49:336–45. doi: 10.1053/j.ajkd.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 117.Okundaye I, Abrinko P, Hou S. Registry of pregnancy in dialysis patients. Am J Kidney Dis. 1998;31:766–73. doi: 10.1016/s0272-6386(98)70044-7. [DOI] [PubMed] [Google Scholar]
- 118.Lindheimer M, Conrad K, Umans J. The normal and disease kidney in pregnancy. In: Schrier R, editor. Diseases of the Kidney and Urinary Tract. 8th ed. Vol. 3. Philadelphia, PA: Lippincott Williams and Wilkinson; 2007. p. 1933. [Google Scholar]
- 119.Magee LA, Yong PJ, Espinosa V, Côté AM, Chen I, von Dadelszen P. Expectant management of severe preeclampsia remote from term: A structured systematic review. Hypertens Pregnancy. 2009;28:312–47. doi: 10.1080/10641950802601252. [DOI] [PubMed] [Google Scholar]
- 120.Gaugler-Senden IP, Huijssoon AG, Visser W, Steegers EA, de Groot CJ. Maternal and perinatal outcome of preeclampsia with an onset before 24 weeks’ gestation. Audit in a tertiary referral center. Eur J Obstet Gynecol Reprod Biol. 2006;128:216–21. doi: 10.1016/j.ejogrb.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 121.Thadhani R, Hagmann H, Schaarschmidt W, Roth B, Cingoez T, Karumanchi SA, et al. Removal of soluble fms-like tyrosine kinase-1 by dextran sulfate apheresis in preeclampsia. J Am Soc Nephrol. 2016;27:903–13. doi: 10.1681/ASN.2015020157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Slater DN, Hague WM. Renal morphological changes in idiopathic acute fatty liver of pregnancy. Histopathology. 1984;8:567–81. doi: 10.1111/j.1365-2559.1984.tb02369.x. [DOI] [PubMed] [Google Scholar]
- 123.Amon E, Allen SR, Petrie RH, Belew JE. Acute fatty liver of pregnancy associated with preeclampsia: Management of hepatic failure with postpartum liver transplantation. Am J Perinatol. 1991;8:278–9. doi: 10.1055/s-2007-999396. [DOI] [PubMed] [Google Scholar]
- 124.Barton JR, Sibai BM, Mabie WC, Shanklin DR. Recurrent acute fatty liver of pregnancy. Am J Obstet Gynecol. 1990;163:534–8. doi: 10.1016/0002-9378(90)91191-e. [DOI] [PubMed] [Google Scholar]
- 125.MacLean MA, Cameron AD, Cumming GP, Murphy K, Mills P, Hilan KJ. Recurrence of acute fatty liver of pregnancy. Br J Obstet Gynaecol. 1994;101:453–4. doi: 10.1111/j.1471-0528.1994.tb11926.x. [DOI] [PubMed] [Google Scholar]
- 126.Gall B, Yee A, Berry B, Birchman D, Hayashi A, Dansereau J, et al. Rituximab for management of refractory pregnancy-associated immune thrombocytopenic purpura. J Obstet Gynaecol Can. 2010;32:1167–71. doi: 10.1016/S1701-2163(16)34741-7. [DOI] [PubMed] [Google Scholar]
- 127.Chakravarty EF, Murray ER, Kelman A, Farmer P. Pregnancy outcomes after maternal exposure to rituximab. Blood. 2011;117:1499–506. doi: 10.1182/blood-2010-07-295444. [DOI] [PubMed] [Google Scholar]
- 128.Martin JN, Jr, Bailey AP, Rehberg JF, Owens MT, Keiser SD, May WL. Thrombotic thrombocytopenic purpura in 166 pregnancies: 1955-2006. Am J Obstet Gynecol. 2008;199:98–104. doi: 10.1016/j.ajog.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 129.Kaplan M. Eculizumab (Alexion) Curr Opin Investig Drugs. 2002;3:1017–23. [PubMed] [Google Scholar]
- 130.Woodruff TM, Nandakumar KS, Tedesco F. Inhibiting the C5-C5a receptor axis. Mol Immunol. 2011;48:1631–42. doi: 10.1016/j.molimm.2011.04.014. [DOI] [PubMed] [Google Scholar]


