Abstract
1.7 million cases of breast cancer are diagnosed every year with 522,000 deaths. Molecular classifications of breast cancer have resulted in improved treatments. However, treatments for triple negative breast cancer (TNBC) are lacking. Analysis of molecular targets for TNBC is a priority. One potential candidate is androgen receptor (AR) phosphorylation. This study assessed the role of AR phosphorylation at ser81/ser515 and their two upstream effectors, cyclin-dependent kinase 1 (pCDK1) and extracellular-regulated kinase 1/2 (pERK1/2) in 332 ductal breast cancer patients by immunohistochemistry.
pERK1/2 combined with AR-515 associated with improved cancer-specific survival (CSS, p = 0.038), decreased size (p = 0.001), invasive grade (p < 0.001), necrosis (p = 0.003), b-lymphocytes (p = 0.020), molecular subtype (p < 0.001) and estrogen receptor (ER)/progesterone receptor (PR)-status (p < 0.001). The cohort was therefore stratified into ER+ve and ER-ve patients. In ER+ve tumours, pERK1/2 combined with AR-515 associated with improved CSS (p = 0.038), smaller size (p = 0.004), invasive grade (p = 0.001), decreased b-lymphocytes (p = 0.013) and increased plasma cells (p = 0.048). In contrast, in TNBC patients, phosphorylation of AR-515 associated with poorer CSS (p = 0.007). pERK1/2 combined with AR-515 associated with decreased inflammation (p = 0.003), increased tumour stroma (p = 0.003) and tumour budding (p = 0.011), with trends towards decrease CSS (p = 0.065) and macrophage levels (p = 0.093).
In Conclusions, AR-515 may be an important regulator of inflammation in breast cancer potential via ERK1/2 phosphorylation. AR-515 is a potential prognostic marker and therapeutic target for TNBC.
Keywords: androgen receptor, phosphorylation, MAPK, breast cancer, triple negative
INTRODUCTION
Approximately 1.7 million cases of breast cancer are diagnosed every year. About 522,000 die of breast cancer yearly making it the 5th most common cause of cancer death globally [1]. A great effort is being channelled to improve the understanding of the pathogenesis of this disease as breast cancer is highly heterogeneous with an increasing number of sub-classifications being made [2–4]. In the past 2 decades, 4 molecular classifications of breast cancer have been extensively studied (Luminal A, Luminal B, HER2-type and Triple negative breast cancer (TNBC)) that have resulted in improved treatments [5, 6].
The majority of breast cancers comprise of luminal A and luminal B subtypes. These subtypes display oestrogen (ER) and/or progesterone receptors (PR) rendering these cancer cells susceptible to endocrine therapies e.g. anti-oestrogen therapies (Tamoxifen) [7, 8]. In HER2 positive breast cancer, the presence of HER2, a tyrosine kinase receptor that is part of the EGFR family, enables targeted therapeutics (Trastuzumab, Pertuzumab) to be effective [9, 10]. However, about 15% of breast cancer cases are triple receptor negative lacking expression of ER, PR or HER2 [11].
It has been shown that TNBC patients displaying pathological complete response (pCR) had better outcomes in terms of progression-free survival than patients who had not achieved pCR [12]. pCR is defined as an absence of any residual invasive breast cancer in the breast and axillary lymph nodes upon completion of chemotherapy [13]. Hence, there is an increasing need for targeted therapies to achieve pCR for TNBC cases. Current pathways that are being studied for this purpose include EGFR, aB-crystallin and androgen receptors (AR) [14–16].
Although numerous studies on AR have been published, the exact role of AR as tumour-promoting or anti-tumorigenic remains undecided. It is known that AR signalling plays a role in regulating cancer cell proliferation and apoptosis [17–19]. AR activation by the binding of androgens such as DHT to AR displaces HSP90 (heat shock protein 90), a chaperone protein to allow the dimerization of AR. The DHT–AR dimer complex then translocates to the nucleus to trigger the activation of the genetic machinery, stimulating cell proliferation. During this process, post-translational modifications such as phosphorylation are triggered at multiple sites within AR. It is now thought that it is these phosphorylation events that fully activate the AR and modulate its different cellular functions [20].
It was also reported that when Tamoxifen-resistant breast cancer cells that expressed high levels of AR were exposed to bicalutamide (anti-androgen), cell growth was shown to decrease as well as reversing Tamoxifen resistance [21], indicating that AR expression may be a mechanism of breast cancer cell adaptation to stimulate cell proliferation in an anti-oestrogen environment. A study by Ayca Gucalp et al. observed that bicalutamide in ER negative and AR positive breast cancer demonstrated improved progression-free survival [22], lending further support that AR or its signalling pathways may be a tangible route for treating patients in the ER negative subgroup.
The MAPK/ERK signalling cascade is heavily involved in the regulation of cancer cell proliferation, growth and differentiation. The stimulation of this pathway leads to the activation of a cascade of kinases (e.g. Ras, Raf, MEK), which ultimately leads to the activation of ERK1/2, which is associated with poor prognosis in breast cancer [23]. One function of ERK1/2 is to phosphorylate AR on ser-515. This is an example of ligand-independent activation via phosphorylation of AR, which is thought to be one of the main mechanisms of AR activation in cancer [24].
In contrast, AR phosphorylation at ser-81 is the prototypical site for dihydrotestosterone (DHT) activation, which is thought to be facilitated by activated Cdk1, as observed by Chen et al where Cdk1 inhibitors decreased ser-81 phosphorylation of AR in LNCaP cells and similarly decreased AR protein expression and transcriptional activity. Whereas transfected Cdk1 stimulated AR phosphorylation at ser-81 and increased AR protein expression [25]. This suggestion has been supported by another study by Yulia et al where in vitro kinase assays demonstrated an increase in ser-308 phosphorylation by CDK1 is responsible for Serine–81 phosphorylation [20]. Cdk1 phosphorylation of AR-81 has also been associated with decreased survival in prostate cancer patients [26].
This study aims to further understand the role of androgens and AR activation in breast cancer by determining its effect on patient survival. This is followed by the determination of the role of upstream pathways (i.e. Cdk1 and ERK1/2 pathways) on AR activation and their effects on cancer specific survival (CSS). We aim to confirm that the phosphorylation of AR at either ser-515 or ser-81 is a surrogate for AR activation and assess if the pathways responsible for this phosphorylation are potential targets for therapeutic intervention.
RESULTS
Phosphorylation of AR-515 associates with improved cancer-specific survival in ductal breast cancer patients
Only patients with staining for AR, AR-81 and AR-515 were included in the analysis (n = 332, Figure 1A). The majority of the patients (71%) were above 50 years old, had small tumour size ≤ 20 mm (58%), had grade II and III tumours (80%) and no involved lymph nodes (53%). ER positive tumours (69%), PR negative tumours (52%) and HER2 negative tumours (82%) formed the majority of tumours, with 20% of cases being triple negative. Overall, 119 (36%) had lumpectomy and radiotherapy, and 213 (64%) had mastectomy and radiotherapy. 176 (53%) of the patients received endocrine therapy alone, 62 (19%) of patients received adjuvant chemotherapy only, while 76 (23%) had both. The median survival was 148 months with 69 deaths from breast cancer and 68 deaths from non-cancer related causes.
Figure 1. AR-515 is associated with poorer patient survival in triple negative breast cancer.
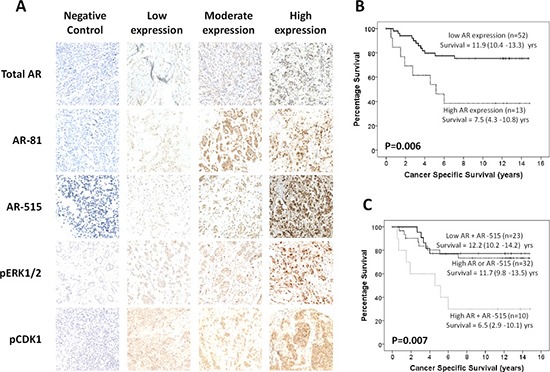
(A) Representative immunohistochemical images for AR, AR-81, AR-515, pCDK1 and pERK1/2. Negative, low, moderate and high nuclear staining is shown for each protein. Cytoplasmic staining can also be observed for some proteins but was not quantified as it represents the inactive form. (B) Kaplan-Meier curve showing that high total AR expression associates with poorer CSS in TNBC patients. (C) Kaplan-Meier curve showing that when total AR and AR-515 are combined, high expression of both proteins is associated with poorer CSS in TNBC patients.
The relationship between nuclear AR activation and CSS is shown in Table 1. Only nuclear expression was investigated as this represents the active form of the protein. High levels of nuclear AR activation via phosphorylation of serine 81 (AR-81) or serine 515 (AR-515) were identified in 155 (47%) and 167 (50%) patients, respectively. Neither AR-81 (p = 0.842) nor AR-515 (p = 0.563) were associated with CSS alone. Therefore, upstream effectors of AR phosphorylation were investigated. AR-81 significantly correlated with nuclear CDK1 (p < 0.001) and AR-515 correlated with nuclear pERK1/2 (p < 0.001) as expected. However, AR-81 still showed no associations even when combined with CDK1 in the nucleus (p = 0.344). In contrast, AR-515 was significantly associated with improved CSS when combined with ERK1/2 phosphorylation in the nucleus (pERK1/2, p = 0.032). When nuclear pERK1/2 was assessed alone it was also significantly associated with improved CSS (p = 0.004). Therefore, further analysis was confined to nuclear pERK1/2 and AR-515.
Table 1. Relationship between ligand-independent AR phosphorylation and cancer-specific survival in patients with invasive ductal breast cancer (n = 332).
| N (%) | 10yr-CSS %(SE) | Univariate HR(95% CI) | P | |
|---|---|---|---|---|
| Total AR expression | ||||
| Low expression | 167 (50) | 79 (3) | 1.04 (0.65–1.67) | 0.869 |
| High expression | 165 (50) | 80 (3) | ||
| AR-81 phosphorylation | ||||
| Low expression | 177 (53) | 79 (3) | 0.95 (0.59–1.53) | 0.842 |
| High expression | 155 (47) | 78 (4) | ||
| AR-515 phosphorylation | ||||
| Low expression | 165 (50) | 78 (3) | 0.87 (0.54–1.40) | 0.563 |
| High expression | 167 (50) | 79 (3) | ||
| CDK1 phosphorylation (n = 227) | ||||
| Low expression | 118 (52) | 76 (4) | 1.00 (0.57–1.74) | 0.985 |
| High expression | 109 (48) | 77 (4) | ||
| ERK1/2 phosphorylation | ||||
| Low expression | 151 (45) | 72 (4) | 0.49 (0.30–0.80) | 0.004 |
| High expression | 181 (55) | 84 (3) | ||
| Combined AR + AR-81 | ||||
| Low AR + AR-81 | 91 (27) | 80 (4) | 1.00 (0.72–1.39) | 0.851 |
| High AR or AR-81 | 162 (49) | 77 (3) | ||
| High AR + AR-81 | 79 (24) | 79 (5) | ||
| Combined AR + AR-515 | ||||
| Low AR + AR-515 | 95 (29) | 78 (4) | 0.96 (0.70–1.31) | 0.903 |
| High AR or AR-515 | 142 (42) | 79 (4) | ||
| High AR + AR-515 | 95 (29) | 79 (5) | ||
| Combined pCDK1 + AR-81 (n = 227) | ||||
| Low pCDK1 + AR-81 | 68 (30) | 78 (6) | 0.88 (0.60–1.28) | 0.344 |
| High pCDK1 or AR-81 | 101 (44) | 72 (5) | ||
| High pCDK1 + AR-81 | 58 (26) | 83 (5) | ||
| Combined pERK1/2 + AR-515 | ||||
| Low pERK + AR-515 | 94 (28) | 77 (5) | 0.72 (0.53–0.98) | 0.032 |
| High pERK or AR-515 | 128 (39) | 73 (4) | ||
| High pERK + AR-515 | 110 (33) | 88 (3) | ||
The relationship between pERK1/2, AR-515, clinicopathological characteristics, and local inflammatory response is presented in Table 2. pERK1/2 was significantly associated with smaller size (p = 0.001), lower grade (p < 0.001), ER/PR+ve tumours (p < 0.001), molecular subtype (p < 0.001), lower necrosis (p = 0.003), weak Klintrup-Makinen (KM) grade (p = 0.004) and lower b-lymphocyte levels (p = 0.020). There was also a trend towards decreased HER2 (p = 0.096) and lower lymphovascular invasion (p = 0.099). When pERK1/2 was combined with AR-515 significant associations were still seen with smaller size (p = 0.017), lower grade (p < 0.001), ER+ve tumours (p = 0.013), PR+ve tumours (p = 0.008), decreased HER2 (p = 0.041), molecular subtype (p < 0.001), lower necrosis (p = 0.006), weak KM grade (p = 0.005) and lower b-lymphocytes (p = 0.023). Significant associations were now also seen with decreased proliferation (p = 0.009), lymphovascular invasion (p = 0.017) and increased tumour budding (p = 0.047).
Table 2. Relationship between clinico-pathological characteristics and ERK1/2 plus AR-515 in patients with invasive ductal breast cancer (n = 332).
| pERK1/2 | pERK1/2 + AR-515 | ||||||
|---|---|---|---|---|---|---|---|
| Low(n = 150) | High(n = 181) | P | Low pERK + AR-515(n = 93) | High pERK or AR-515(n = 128) | High pERK + AR-515(n = 110) | P | |
| Clinicopathological Characteristics | |||||||
| Age | 0.544 | 0.442 | |||||
| ≤ 50 years | 46 (31) | 50 (28) | 29 (31) | 32 (25) | 35 (31) | ||
| > 50 years | 104 (69) | 131 (72) | 64 (69) | 96 (75) | 75 (69) | ||
| Size | 0.001 | 0.017 | |||||
| ≤ 20 mm | 74 (49) | 117 (65) | 46 (49) | 73 (57) | 72 (65) | ||
| 21–50 mm | 68 (45) | 63 (34) | 44 (47) | 50 (39) | 37 (34) | ||
| > 50 mm | 8 (6) | 1 (1) | 3 (4) | 5 (4) | 1 (1) | ||
| Invasive Grade | < 0.001 | < 0.001 | |||||
| I | 14 (9) | 51 (28) | 10 (10) | 20 (16) | 35 (32) | ||
| II | 57 (38) | 84 (46) | 35 (38) | 64 (50) | 42 (38) | ||
| III | 79 (53) | 46 (26) | 48 (52) | 44 (34) | 33 (30) | ||
| Lymph Node Involvement | 0.874 | 0.779 | |||||
| No | 81 (54) | 96 (53) | 53 (57) | 63 (49) | 60 (55) | ||
| Yes | 69 (46) | 85 (47) | 40 (43) | 65 (51) | 50 (45) | ||
| ER Status | < 0.001 | 0.013 | |||||
| No | 68 (45) | 35 (19) | 35 (38) | 44 (34) | 24 (22) | ||
| Yes | 82 (55) | 146 (81) | 58 (62) | 84 (66) | 86 (88) | ||
| PR status | < 0.001 | 0.008 | |||||
| No | 94 (63) | 76 (42) | 55 (59) | 70 (55) | 45 (41) | ||
| Yes | 56 (37) | 105 (58) | 38 (41) | 58 (45) | 65 (59) | ||
| Her2 status | 0.096 | 0.041 | |||||
| No | 120 (80) | 157 (87) | 74 (80) | 104 (81) | 99 (90) | ||
| Yes | 30 (20) | 24 (13) | 19 (20) | 24 (19) | 11 (10) | ||
| Molecular Subtype | < 0.001 | < 0.001 | |||||
| Luminal A | 49 (33) | 108 (60) | 30 (32) | 61 (48) | 67 (61) | ||
| Luminal B | 36 (24) | 41 (23) | 32 (34) | 24 (19) | 22 (20) | ||
| TNBC | 44 (29) | 23 (13) | 21 (23) | 27 (21) | 18 (16) | ||
| Her2+ | 21 (14) | 9 (4) | 10 (11) | 16 (13) | 3 (3) | ||
| Tumour Necrosis | 0.003 | 0.006 | |||||
| Low | 61 (41) | 103 (57) | 40 (43) | 56 (44) | 68 (62) | ||
| High | 89 (59) | 78 (43) | 53 (57) | 72 (56) | 42 (38) | ||
| Ki67 proliferation index | 0.177 | 0.009 | |||||
| Low | 107 (71) | 140 (77) | 59 (63) | 100 (78) | 88 (80) | ||
| High | 43 (29) | 41 (23) | 34 (37) | 28 (22) | 22 (20) | ||
| Lymphatic Invasion | 0.961 | 0.859 | |||||
| No | 99 (66) | 119 (66) | 64 (69) | 80 (62) | 74 (67) | ||
| Yes | 51 (34) | 62 (34) | 29 (31) | 48 (38) | 36 (33) | ||
| Lymphovascular Invasion | 0.099 | 0.017 | |||||
| No | 127 (85) | 164 (91) | 76 (82) | 113 (88) | 102 (93) | ||
| Yes | 23 (15) | 17 (9) | 17 (18) | 15 (12) | 8 (7) | ||
| Inflammatory Infiltrate | |||||||
| Klintrup Makinen Grade | 0.004 | 0.005 | |||||
| Weak | 103 (69) | 149 (82) | 64 (69) | 94 (73) | 94 (85) | ||
| Strong | 47 (31) | 32 (18) | 29 (31) | 34 (27) | 16 (15) | ||
| CD68+ macrophages | 0.776 | 0.228 | |||||
| Low | 31 (21) | 32 (17) | 13 (14) | 31 (24) | 19 (17) | ||
| Moderate | 53 (35) | 79 (44) | 38 (41) | 42 (33) | 52 (47) | ||
| High | 66 (44) | 70 (39) | 42 (45) | 55 (47) | 39 (36) | ||
| CD4+ T-lymphocytes | 0.156 | 0.413 | |||||
| Low | 54 (36) | 82 (45) | 33 (35) | 54 (42) | 49 (44) | ||
| Moderate | 37 (25) | 36 (20) | 28 (30) | 21 (16) | 24 (22) | ||
| High | 59 (39) | 63 (35) | 32 (35) | 53 (41) | 37 (34) | ||
| CD8+ cytotoxic T-cells | 0.458 | 0.452 | |||||
| Low | 39 (26) | 51 (28) | 24 (25) | 33 (26) | 33 (30) | ||
| Moderate | 54 (36) | 69 (38) | 35(38) | 47 (37) | 41 (37) | ||
| High | 57 (38) | 61 (34) | 34 (37) | 48 (37) | 36 (33) | ||
| CD20+ B-lymphocytes | 0.020 | 0.023 | |||||
| Low | 65 (43) | 100 (55) | 42(45) | 58 (45) | 65 (59) | ||
| Moderate | 24 (16) | 28 (15) | 12 (13) | 25 (20) | 15 (14) | ||
| High | 61 (41) | 53 (30) | 39 (42) | 45 (35) | 30 (27) | ||
| CD138+ plasma cells | 0.225 | 0.111 | |||||
| Low | 78 (52) | 78 (43) | 51 (55) | 60 (47) | 45 (41) | ||
| Moderate | 19 (13) | 33 (18) | 13 (14) | 16 (13) | 23 (21) | ||
| High | 53 (35) | 70 (39) | 29 (31) | 52 (40) | 42 (38) | ||
| Tumour Stroma Percentage | 0.700 | 0.134 | |||||
| Low | 100 (66) | 117 (65) | 64 (69) | 88 (69) | 65 (59) | ||
| High | 50 (34) | 64 (35) | 29 (31) | 40 (31) | 45 (41) | ||
| Tumour Budding | 0.532 | 0.047 | |||||
| Low | 97 (65) | 111 (61) | 65 (70) | 81 (63) | 62 (56) | ||
| High | 53 (35) | 70 (39) | 28 (30) | 47 (37) | 48 (44) | ||
| Angiogenesis (n = 321) | 0.586 | 0.564 | |||||
| Low | 46 (31) | 55 (31) | 29 (32) | 46 (36) | 26 (25) | ||
| Moderate | 46 (31) | 62 (36) | 28 (31) | 40 (32) | 40 (38) | ||
| High | 55 (38) | 57 (33) | 34 (37) | 40 (32) | 38 (37) | ||
AR-515 associates with improved cancer-specific survival in ER+ve breast cancer patients
As pERK1/2 plus AR-515 associated with molecular subtype, we firstly stratified patients into ER+ve and ER-ve tumours (Supplementary Table 1). pERK1/2 was associated with improved CSS only in ER+ve tumours (p = 0.008). As pERK1/2 and AR-515 strongly correlated in ER+ve patients (p < 0.001) they were combined. However, when combined the survival effect was weakened (p = 0.038), suggesting that pERK can also act independently of AR-515 in ER+ve breast cancers. When ER+ve patients where stratified further, there was no difference in CSS between luminal A and luminal B subtypes for pERK1/2 alone or combined with AR-515 therefore further analysis was carried out in all ER+ve tumours (n = 228).
The relationship between pERK1/2, AR-515, clinicopathological characteristics, and local inflammatory response in ER+ve tumours is presented in Table 3. pERK1/2 was significantly associated with smaller size (p = 0.004), lower grade (p = 0.001), molecular subtype (p = 0.024), decreased proliferation (p = 0.006), lower b-lymphocytes (p = 0.013) and increased plasma cells (p = 0.048). There was also a trend towards decreased necrosis (p = 0.096). When pERK1/2 was combined with AR-515 significant associations where still seen with lower grade (p = 0.002), molecular subtype (p = 0.001), decreased proliferation (p = 0.001), lower b-lymphocytes (p = 0.006) and increased plasma cells (p = 0.023). Significant associations were now also seen with decreased necrosis (p = 0.009) and lymphovascular invasion (p = 0.029).
Table 3. Relationship between clinico-pathological characteristics and AR-515 in patients with ER + ve invasive ductal breast cancer (n = 228).
| pERK1/2 | pERK1/2 + AR-515 | ||||||
|---|---|---|---|---|---|---|---|
| Low(n = 150) | High(n = 181) | P | Low pERK + AR-515(n = 93) | High pERK or AR-515(n = 128) | High pERK + AR-515(n = 110) | P | |
| Clinicopathological Characteristics | |||||||
| Age | 0.544 | 0.442 | |||||
| ≤ 50 years | 46 (31) | 50 (28) | 29 (31) | 32 (25) | 35 (31) | ||
| > 50 years | 104 (69) | 131 (72) | 64 (69) | 96 (75) | 75 (69) | ||
| Size | 0.001 | 0.017 | |||||
| ≤ 20 mm | 74 (49) | 117 (65) | 46 (49) | 73 (57) | 72 (65) | ||
| 21–50 mm | 68 (45) | 63 (34) | 44 (47) | 50 (39) | 37 (34) | ||
| > 50 mm | 8 (6) | 1 (1) | 3 (4) | 5 (4) | 1 (1) | ||
| Invasive Grade | < 0.001 | < 0.001 | |||||
| I | 14 (9) | 51 (28) | 10 (10) | 20 (16) | 35 (32) | ||
| II | 57 (38) | 84 (46) | 35 (38) | 64 (50) | 42 (38) | ||
| III | 79 (53) | 46 (26) | 48 (52) | 44 (34) | 33 (30) | ||
| Lymph Node Involvement | 0.874 | 0.779 | |||||
| No | 81 (54) | 96 (53) | 53 (57) | 63 (49) | 60 (55) | ||
| Yes | 69 (46) | 85 (47) | 40 (43) | 65 (51) | 50 (45) | ||
| ER Status | < 0.001 | 0.013 | |||||
| No | 68 (45) | 35 (19) | 35 (38) | 44 (34) | 24 (22) | ||
| Yes | 82 (55) | 146 (81) | 58 (62) | 84 (66) | 86 (88) | ||
| PR status | < 0.001 | 0.008 | |||||
| No | 94 (63) | 76 (42) | 55 (59) | 70 (55) | 45 (41) | ||
| Yes | 56 (37) | 105 (58) | 38 (41) | 58 (45) | 65 (59) | ||
| Her2 status | 0.096 | 0.041 | |||||
| No | 120 (80) | 157 (87) | 74 (80) | 104 (81) | 99 (90) | ||
| Yes | 30 (20) | 24 (13) | 19 (20) | 24 (19) | 11 (10) | ||
| Molecular Subtype | < 0.001 | < 0.001 | |||||
| Luminal A | 49 (33) | 108 (60) | 30 (32) | 61 (48) | 67 (61) | ||
| Luminal B | 36 (24) | 41 (23) | 32 (34) | 24 (19) | 22 (20) | ||
| TNBC | 44 (29) | 23 (13) | 21 (23) | 27 (21) | 18 (16) | ||
| Her2+ | 21 (14) | 9 (4) | 10 (11) | 16 (13) | 3 (3) | ||
| Tumour Necrosis | 0.003 | 0.006 | |||||
| Low | 61 (41) | 103 (57) | 40 (43) | 56 (44) | 68 (62) | ||
| High | 89 (59) | 78 (43) | 53 (57) | 72 (56) | 42 (38) | ||
| Ki67 proliferation index | 0.177 | 0.009 | |||||
| Low | 107 (71) | 140 (77) | 59 (63) | 100 (78) | 88 (80) | ||
| High | 43 (29) | 41 (23) | 34 (37) | 28 (22) | 22 (20) | ||
| Lymphatic Invasion | 0.961 | 0.859 | |||||
| No | 99 (66) | 119 (66) | 64 (69) | 80 (62) | 74 (67) | ||
| Yes | 51 (34) | 62 (34) | 29 (31) | 48 (38) | 36 (33) | ||
| Lymphovascular Invasion | 0.099 | 0.017 | |||||
| No | 127 (85) | 164 (91) | 76 (82) | 113 (88) | 102 (93) | ||
| Yes | 23 (15) | 17 (9) | 17 (18) | 15 (12) | 8 (7) | ||
| Inflammatory Infiltrate | |||||||
| Klintrup Makinen Grade | 0.004 | 0.005 | |||||
| Weak | 103 (69) | 149 (82) | 64 (69) | 94 (73) | 94 (85) | ||
| Strong | 47 (31) | 32 (18) | 29 (31) | 34 (27) | 16 (15) | ||
| CD68+ macrophages | 0.776 | 0.228 | |||||
| Low | 31 (21) | 32 (17) | 13 (14) | 31 (24) | 19 (17) | ||
| Moderate | 53 (35) | 79 (44) | 38 (41) | 42 (33) | 52 (47) | ||
| High | 66 (44) | 70 (39) | 42 (45) | 55 (47) | 39 (36) | ||
| CD4+ T-lymphocytes | 0.156 | 0.413 | |||||
| Low | 54 (36) | 82 (45) | 33 (35) | 54 (42) | 49 (44) | ||
| Moderate | 37 (25) | 36 (20) | 28 (30) | 21 (16) | 24 (22) | ||
| High | 59 (39) | 63 (35) | 32 (35) | 53 (41) | 37 (34) | ||
| CD8+ cytotoxic T-cells | 0.458 | 0.452 | |||||
| Low | 39 (26) | 51 (28) | 24 (25) | 33 (26) | 33 (30) | ||
| Moderate | 54 (36) | 69 (38) | 35(38) | 47 (37) | 41 (37) | ||
| High | 57 (38) | 61 (34) | 34 (37) | 48 (37) | 36 (33) | ||
| CD20+ B-lymphocytes | 0.020 | 0.023 | |||||
| Low | 65 (43) | 100 (55) | 42(45) | 58 (45) | 65 (59) | ||
| Moderate | 24 (16) | 28 (15) | 12 (13) | 25 (20) | 15 (14) | ||
| High | 61 (41) | 53 (30) | 39 (42) | 45 (35) | 30 (27) | ||
| CD138+ plasma cells | 0.225 | 0.111 | |||||
| Low | 78 (52) | 78 (43) | 51 (55) | 60 (47) | 45 (41) | ||
| Moderate | 19 (13) | 33 (18) | 13 (14) | 16 (13) | 23 (21) | ||
| High | 53 (35) | 70 (39) | 29 (31) | 52 (40) | 42 (38) | ||
| Tumour Stroma Percentage | 0.700 | 0.134 | |||||
| Low | 100 (66) | 117 (65) | 64 (69) | 88 (69) | 65 (59) | ||
| High | 50 (34) | 64 (35) | 29 (31) | 40 (31) | 45 (41) | ||
| Tumour Budding | 0.532 | 0.047 | |||||
| Low | 97 (65) | 111 (61) | 65 (70) | 81 (63) | 62 (56) | ||
| High | 53 (35) | 70 (39) | 28 (30) | 47 (37) | 48 (44) | ||
| Angiogenesis (n = 321) | 0.586 | 0.564 | |||||
| Low | 46 (31) | 55 (31) | 29 (32) | 46 (36) | 26 (25) | ||
| Moderate | 46 (31) | 62 (36) | 28 (31) | 40 (32) | 40 (38) | ||
| High | 55 (38) | 57 (33) | 34 (37) | 40 (32) | 38 (37) | ||
AR phosphorylation at Ser515 associates with poorer patient survival in TNBC
It was observed in patients with ER-ve breast cancer that high pERK1/2 plus AR-515 had a trend towards an effect on survival rate. It was hypothesised that the loss of significance and weaker correlation between pERK1/2 and AR-515 in ER-ve patients (p = 0.023) may be due to differences between the two ER-ve subtypes. Therefore, ER-ve patients were stratified into HER2-type and TNBC to further investigate these effects (Supplementary Table 2). In patients with TNBC, the correlation between pERK1/2 and AR-515 was strengthened (p = 0.010), however no significant effect on CSS was observed for pERK1/2 alone (p = 0.534) and only a trend towards poorer outcome was seen when combined with AR-515 (p = 0.065). However, high levels of AR-515 combined with total AR, representing full AR activation, associated with a significantly poorer outcome (p = 0.007, Figure 1A), and a similar effect was also seen when total AR was considered alone (p = 0.006, Figure 1B). In contrast, in patients with HER2-type cancers the correlation between pERK1/2 and AR-515 was lost (p = 0.949) and no significant associations were seen in these patients. However, there was a trend towards improved patient survival with AR-515 phosphorylation (p = 0.056) alone and when combined with pERK1/2 (p = 0.076), confirming our hypothesis that these two ER-ve subtypes respond differently to AR-515 phosphorylation.
Due to the detrimental effect of AR-515 phosphorylation in TNBC, associations with clinicopathological characteristics were assessed (Table 4). Full activation of the AR receptor as shown by AR-515 plus total AR significantly associated with increased lymphovascular invasion (p = 0.033), lower KM grade (p = 0.004), increased tumour-stroma percentage (TSP) (p = 0.033) and increased tumour budding (p = 0.007). When combined with pERK1/2 associations were still seen with lower KM grade (p = 0.003), increased TSP (p = 0.003) and increased tumour budding (p = 0.011). Trends towards association were also seen for increased age (p = 0.075) and decreased macrophages (p = 0.093).
Table 4. Relationship between clinico-pathological characteristics, pERK1/2 and AR-515 in patients with TNBC (n = 65).
| AR + AR-515 | pERK1/2 + AR-515 | |||||||
|---|---|---|---|---|---|---|---|---|
| Low AR + AR-515 (n = 21) |
High AR or AR-515 (n = 27) |
High AR + AR-515 (n = 17) |
P |
Low pERK + AR-515 (n = 23) |
High pERK or AR-515 (n = 32) |
High pERK + AR-515 (n = 10) |
P | |
| Clinicopathological Characteristics | ||||||||
|
Age ≤ 50 years > 50 years |
11 (48) 12 (52) |
12 (37) 20 (63) |
3 (30) 7 (70) |
0.304 | 12 (57) 9 (43) |
9 (33) 18 (67) |
5 (29) 12 (71) |
0.075 |
|
Size ≤ 20 mm 21–50 mm > 50 mm |
6 (26) 17 (74) 0 (0) |
20 (63) 11 (34) 1 (3) |
3 (30) 6 (60) 1 (10) |
0.648 | 6 (29) 15 (71) 0 (0) |
12 (44) 13 (48) 2 (8) |
11 (64) 6 (36) 0 (0) |
0.051 |
|
Invasive Grade I II III |
2 (9) 3 (13) 18 (78) |
1 (3) 7 (22) 24 (75) |
0 (0) 2 (20) 8 (80) |
0.641 | 1 (5) 2 (10) 18 (85) |
1 (4) 6 (22) 20 (74) |
1 (6) 4 (24) 12 (70) |
0.353 |
|
Lymph Node Involvement No Yes |
14 (62) 9 (39) |
19 (59) 13 (41) |
3 (30) 7 (70) |
0.169 | 14 (66) 7 (34) |
13 (48) 14 (52) |
9 (53) 8 (47) |
0.366 |
|
Tumour Necrosis Low High |
5 (22) 18 (78) |
11 (34) 21 (66) |
1 (10) 9 (90) |
0.806 | 5 (24) 16 (76) |
6 (22) 21 (78) |
6 (35) 11 (65) |
0.452 |
|
Ki67 proliferation index Low High |
17 (74) 6 (26) |
27 (84) 5 (16) |
8 (80) 2 (20) |
0.480 | 17 (81) 4 (19) |
22 (81) 5 (19) |
13 (76) 4 (24) |
0.744 |
|
Lymphatic Invasion No Yes |
15 (65) 8 (35) |
20 (62) 12 (38) |
4 (40) 6 (60) |
0.240 | 15 (71) 6 (29) |
16 (59) 11 (41) |
8 (53) 9 (47) |
0.129 |
|
Lymphovascular Invasion No Yes |
19 (83) 4 (17) |
28 (87) 4 (13) |
5 (50) 5 (50) |
0.033 | 17 (81) 4 (19) |
21 (78) 6 (22) |
14 (82) 3 (18) |
0.936 |
| Inflammatory Infiltrate | ||||||||
|
Klintrup Makinen Grade Weak Strong |
6 (26) 17 (74) |
22 (69) 10 (31) |
7 (70) 3 (30) |
0.004 | 5 (24) 16 (76) |
18 (67) 9 (33) |
12 (70) 5 (30) |
0.003 |
|
CD68+ macrophages Low Moderate High |
3 (13) 8 (35) 12 (52) |
10 (31) 6 (19) 16 (50) |
3 (30) 5 (50) 2 (20) |
0.111 | 2 (10) 7 (34) 12 (56) |
11 (41) 5 (18) 11 (41) |
3 (18) 7 (41) 7 (41) |
0.093 |
|
CD4+ T-lymphocytes Low Moderate High |
5 (22) 8 (35) 10 (43) |
6 (19) 6 (19) 20 (62) |
5 (50) 1 (10) 4 (40) |
0.604 | 3 (14) 7 (34) 11 (52) |
10 (37) 4 (15) 13 (48) |
3 (18) 4 (24) 10 (58) |
0.983 |
|
CD8+ cytotoxic T-cells Low Moderate High |
4 (12) 8 (35) 11 (47) |
7 (22) 4 (13) 21 (65) |
2 (20) 6 (60) 2 (20) |
0.522 | 4 (19) 6 (29) 12 (52) |
7 (26) 7 (26) 13 (48) |
3 (17) 5 (30) 9 (53) |
0.726 |
|
CD20+ B-lymphocytes Low Moderate High |
8 (35) 3 (13) 12 (52) |
9 (28) 5 (16) 18 (56) |
2 (20) 2 (20) 6 (60) |
0.488 | 7 (29) 3 (19) 12 (52) |
10 (37) 6 (22) 11 (41) |
3 (18) 1 (6) 13 (76) |
0.231 |
|
CD138+ plasma cells Low Moderate High |
7 (29) 2 (9) 14 (62) |
11 (34) 7 (22) 14 (44) |
3 (30) 1 (10) 6 (60) |
0.779 | 6 (29) 2 (10) 13 (61) |
12 (44) 4 (15) 11 (41) |
3 (18) 4 (24) 10 (58) |
0.302 |
|
Tumour Stroma Percentage Low High |
21 (91) 2 (9) |
19 (59) 13 (41) |
7 (70) 3 (30) |
0.033 | 19 (90) 2 (10) |
20 (74) 7 (26) |
8 (53) 9 (47) |
0.003 |
|
Tumour Budding Low High |
20 (87) 3 (13) |
22 (69) 10 (31) |
4 (40) 6 (60) |
0.007 | 19 (90) 2 (10) |
18 (67) 9 (33) |
9 (53) 8 (47) |
0.011 |
|
Angiogenesis Low Moderate High |
10 (51) 4 (12) 9 (39) |
10 (31) 6 (19) 16 (50) |
2 (20) 3 (30) 5 (50) |
0.255 | 9 (43) 3 (14) 9 (43) |
8 (30) 7 (26) 12 (44) |
5 (30) 3 (17) 9 (53) |
0.413 |
Is AR phosphorylation at Ser515 an independent prognostic factor for ER+ve or TNBC?
For ER+ve tumours, since pERK1/2 plus AR-515 had significant associations with improved patient survival, these factors were taken into univariate and multivariate analysis (Table 5). On univariate analysis, size (p = 0.002), invasive grade (p = 0.013), lymph node involvement (p = 0.009), necrosis (p < 0.001), proliferation index (p < 0.001), lymphatic invasion (p < 0.001), cytotoxic t-lymphocytes (p = 0.005), TSP (p = 0.009), tumour budding (p = 0.001) and angiogenesis (p = 0.043) were significantly associated with poorer CSS. Lymphovascular invasion (p = 0.054) and b-lymphocytes (p = 0.064) trended towards significance.
Table 5. Univariate and multivariate survival analysis in patients with invasive ductal breast cancer (n = 293).
| ER + ve (n = 228) | TNBC (n = 65) | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate HR(95% CI) | P | Multivariate HR(95% CI) | P | Univariate HR(95% CI) | P | Multivariate HR(95% CI) | P | |
| Clinicopathological Characteristics | ||||||||
| Age (< 50/> 50) | 1.92 (0.80–4.62) | 0.143 | - | - | 2.70 (0.98–7.44) | 0.055 | - | - |
| Size (< 20/20–50/ > 50) | 2.38 (1.36–4.15) | 0.002 | 1.58 (0.67–2.89) | 0.134 | 3.23 (1.19–7.78) | 0.022 | 1.20 (0.42–3.40) | 0.732 |
| Invasive Grade (I/II/III) | 1.83 (1.14–2.95) | 0.013 | 1.44 (0.83–2.48) | 0.193 | 1.38 (0.54–3.51) | 0.502 | - | - |
| Lymph Node Involvement (No/Yes) | 2.47 (1.25–4.88) | 0.009 | 1.48 (0.68–3.20) | 0.324 | 7.16 (2.38–21.5) | < 0.001 | 5.17 (1.59-16.8) | 0.006 |
| Tumour Necrosis (Low/High) | 3.19 (1.75–6.95) | < 0.001 | 2.33 (1.06–5.14) | 0.036 | 9.25 (1.34–69.2) | 0.030 | 4.82 (0.57-40.5) | 0.148 |
| Ki67 proliferation index (Low/High) | 3.59 (1.87–6.86) | < 0.001 | 2.59 (1.21–5.53) | 0.014 | 0.74 (0.22–2.53) | 0.629 | - | - |
| Lymphatic Invasion (No/Yes) | 3.40 (1.76–6.55) | < 0.001 | 2.17 (0.97–4.86) | 0.060 | 5.27 (1.91–14.5) | 0.001 | 2.61 (0.80-8.53) | 0.111 |
| Lymphovascular Invasion (No/Yes) | 2.25 (0.99–5.12) | 0.054 | - | - | 10.4 (4.13–26.0) | < 0.001 | 6.04 (1.98-18.4) | 0.002 |
| Inflammatory Characteristics | ||||||||
| Klintrup-Makinen Grade (Weak/Strong) | 0.71 (0.25–1.99) | 0.509 | - | - | 1.04 (0.43–2.50) | 0.938 | - | - |
| CD68+ macrophages (low/mod/high) | 1.01 (0.64–1.60) | 0.961 | - | - | 0.49 (0.29–0.85) | 0.011 | 0.32 (0.16–0.66) | 0.002 |
| CD4+ T-lymphocytes (low/mod/high) | 0.78 (0.53–1.41) | 0.199 | - | - | 1.02 (0.60–1.75) | 0.933 | - | - |
| CD8+ cytotoxic T-cells (low/mod/high) | 0.54 (0.35–0.83) | 0.005 | 0.44 (0.27–0.72) | 0.001 | 0.58 (0.34–0.99) | 0.047 | 0.72 (0.36–1.43) | 0.346 |
| CD20+ B-lymphocytes (low/mod/high) | 0.67 (0.43–1.03) | 0.064 | - | - | 1.15 (0.69–1.90) | 0.600 | - | - |
| CD138+ plasma cells (low/mod/high) | 1.11 (0.77–1.60) | 0.561 | - | - | 1.76 (0.99–3.14) | 0.055 | - | - |
| Tumour Stroma Percentage (low/high) | 2.38 (1.25–4.54) | 0.009 | 2.13 (1.06–4.27) | 0.033 | 2.09 (0.85–5.12) | 0.107 | - | - |
| Tumour Budding (low/high) | 3.07 (1.56–6.03) | 0.001 | 1.97 (0.91–4.26) | 0.084 | 1.69 (0.69–4.13) | 0.251 | - | - |
| Angiogenesis (low/high) | 1.55 (1.01–2.37) | 0.043 | 1.64 (1.00–2.70) | 0.051 | 1.42 (0.84–2.42) | 0.193 | - | - |
| AR Pathway | ||||||||
| Total AR (low/high) | 1.43 (0.72–2.84) | 0.309 | - | - | 3.31 (1.35–8.11) | 0.006 | 1.14 (0.41–3.17) | 0.801 |
| AR-515 (low/high) | 0.78 (0.41–1.51) | 0.459 | - | - | 1.70 (0.65–4.42) | 0.274 | - | - |
| pERK1/2 (low/high) | 0.43 (0.22–0.82) | 0.008 | 0.67 (0.43–1.04) | 0.073 | 1.33 (0.54–3.25) | 0.534 | - | - |
| AR+AR-515 (low AR + AR-515/high AR or AR-515/high AR + AR-515) | 1.04 (0.68–1.60) | 0.985 | - | - | 2.19 (1.14–4.20) | 0.007 | 0.96 (0.26–3.58) | 0.957 |
| pERK1/2+AR-515 (low pERK + AR-515/high pERK or AR-515/high pERK + AR-515) | 0.64 (0.42–0.98) | 0.038 | 0.76 (0.20–2.87) | 0.682 | 1.35 (0.77–2.34) | 0.065 | - | - |
On multivariate survival analysis including pERK1/2 plus AR-515; necrosis (p = 0.036), proliferation index (p = 0.014), cytotoxic t-lymphocytes (p = 0.001), and TSP (p = 0.033) were independent prognostic factors, with lymphatic invasion (p = 0.060), tumour budding (p = 0.084), angiogenesis (p = 0.051) and pERK1/2 (p = 0.073) showing trends towards independence. However, pERK1/2 plus AR-515 does not appear to be independently prognostic in these patients (p = 0.682).
For TNBC, since AR-51 plus total AR had significant associations with poorer patient survival, these factors were taken into univariate and multivariate analysis (Table 7). On univariate analysis, size (p = 0.022), lymph node involvement (p < 0.001), necrosis (p = 0.030), lymphatic invasion (p = 0.001), lymphvascular invasion (p < 0.001), macrophages (p = 0.011) and cytotoxic t-lymphocytes (p = 0.047) were significantly associated with poorer CSS. Age (p = 0.055) and plasma cells (p = 0.055) trended towards significance.
On multivariate survival analysis including AR-515 plus total AR; lymph node involvement (p = 0.006), lymphovascular invasion (p = 0.002), and macrophages (p = 0.002) were independent prognostic factors. However, AR-515 plus total AR (p = 0.957) nor AR alone (p = 0.801) appear to be independently prognostic in these patients.
DISCUSSION
This study suggests that effects of activation via phosphorylation of AR at Ser515 are subtype-dependent. In ER+ve and HER2-type patients AR-515 is associated with good prognosis, but in TNBC patients AR-515 is associated with poor prognosis. These effects of AR phosphorylation appear to be associated with inflammation. In ER+ve tumours AR-515 was associated with an increase in b-lymphocytes, therefore combating tumour spread. In contrast, in TNBC tumours AR-515 was associated with a decrease in macrophages, increased proliferation, increased tumour to stroma percentage and invasion. Emphasising the need for a personalised medicine approach, as the TNBC patients could benefit from anti-androgen therapy.
In the current study, AR-515 phosphorylation is associated with decreased Ki67 in ER+ve tumours, confirming previous reports that AR is a good prognostic factor in ER+ve breast cancer due to an anti-proliferative effect [27, 28]. In contrast in TNBC, AR expression is associated with poor prognosis, an increase in proliferation rate, lymphatic invasion and decreased survival [27, 29, 30]. However, current data on the role of AR in breast cancer is controversial with some groups showing a good prognosis for AR-positive TNBC patients [31, 32]. Conversely, other groups have reported similar outcomes to the present study showing a good prognosis for AR/ER-positive patients and a poor prognosis for AR-positive TNBC patients [33, 34]. However, these studies only considered total AR expression, with no analysis of AR phosphorylation and data from the current study suggests that these opposing effects of AR may be due to differential phosphorylation of AR and therefore differential survival effects.
To date little work has been reported on AR phosphorylation in breast cancer, even though this is now thought to be the main post-translational modification needed to fully activate AR [20]. One study observed up-regulation of AR-213 and AR-650 phosphorylation in invasive ductal adenocarcinoma; however patient survival was not investigated [35]. To our knowledge the current study is the first to report AR-515 phosphorylation is associated with poorer patient outcomes in TNBC. This is in line with observations in prostate cancer where AR-515 was associated with decreased CSS and proliferation [26].
ERK1/2 has been proposed to phosphorylate AR-515 in response to EGF stimulation. Ponguta et al. used site directed mutagenesis within the n-terminal region of AR to delineate that AR-515 was the phosphorylation site affected by EGF stimulation [36]. Chia et al. also showed that inhibition of ERK1/2 phosphorylation reduces expression of AR in ER-ve breast cancers. Interestingly, they also showed that AR inhibition leads to down-regulation of ERK1/2 target genes suggesting that AR can regulate ERK1/2 phosphorylation and kinase activity, creating a feedback loop [37]. In the current study, AR and pERK1/2 show a strong correlation and combination of these two proteins strengthens their individual effects, suggesting that ERK1/2 may be responsible for phosphorylation of AR-515 in these patients.
In the current study, AR-515 is present in all breast cancers; however the phenotypic and survival affects are subtype-dependent. In ER+ve breast cancers, AR-515 phosphorylation leads to an improved survival, this may be due to AR-515 increasing the rate of maturation of b-lymphocytes into plasma cells. This is in contrast to a previous study, that suggests total AR can inhibit b-lymphocyte development resulting in suppression of systemic inflammation, however AR phosphorylation sites were not taken into account [38]. It is also interesting that in the current study only pERK1/2 was shown to be an independent prognostic factor in ER+ve tumours, suggesting it may be a driver of this pathway potentially via phosphorylation of AR-515.
In TNBC we observed that phosphorylation of AR-515 leads to poorer survival possibly via down-regulation of inflammation. This has previously been observed in prostate cancer, where DHT treatment and AR activation was associated with decreased local inflammation, inflammatory growth factor production and T-lymphocyte proliferation [39]. This detrimental effect of AR-515 on inflammation and survival, suggests that anti-androgen therapy may be of therapeutic benefit to patients with TNBC. This is in line with current clinical trials were TNBC patients are responding to anti-androgen therapy [22, 40]. Currently, 30% of TNBC patients respond to chemotherapy, but there are no approved targeted treatments for the other 70%. Clinical trials are underway for the use of PARP inhibitors in BRCA1 mutated TNBC and PI3K inhibitors in PTEN mutated TNBC. Anti-androgens are a being trialled as potential treatment for AR-positive patients, which is currently around 10–15% TNBC patients, however using AR phosphorylation as a biomarker rather than total AR expression may increase the frequency of AR in TNBC, as even when AR expression is low, the receptor can still be activated via one of its many phosphorylation sites [20]. It has recently been shown that combining anti-androgens with a PI3K inhibitor increases their sensitivity in TNBC patients [41].
In conclusion, this study demonstrates subtype-specific differences in the effects of AR-515 phosphorylation in breast cancer patients. In ER+ve breast cancers, high phosphorylation of AR-515 conveys a protective effect. This is potentially due to an increased inflammatory response within the tumour when AR-515 is phosphorylated. However, in TNBC patients, phosphorylation of AR-515 associates with a poorer prognosis, possibly due to a down regulation of local inflammation. This difference in survival may be due to different substrates phosphorylating AR-515. In ER+ve patients, AR-515 strongly correlates with pERK1/2, suggesting ERK1/2 may phosphorylate AR-515 in these patients. However, this is not seen in TNBC patients suggesting another kinase is responsible. The data also suggests that AR may be an important regulator of inflammation in breast cancer and maybe a potential prognostic biomarker for TNBC. It also confirms the need to consider phosphorylation of the AR when investigating activation, as differing phosphorylation sites have varied downstream effects. Further investigation is now needed to delineate how AR phosphorylation is influencing inflammation, is it a direct association or is another factor involved. The data for TNBC also needs to be confirmed in a larger dataset as one limitation of this study is the low number of TNBC cases within the cohort.
MATERIALS AND METHODS
Patient cohort characteristics
Patients presenting with invasive ductal breast cancer at Glasgow Royal Infirmary, Western Infirmary and Stobhill Hospital between 1995 and 1998 with formalin-fixed paraffin embedded blocks of the primary tumour available for evaluation were studied (n = 474). The study was approved by the Research Ethics Committee of the West Glasgow University Hospitals NHS Trust.
Clinicopathological data including age, tumour size, tumour grade, lymph node status, type of surgery and use of adjuvant treatment (chemotherapy, hormonal therapy and/or radiotherapy) were retrieved from the routine reports. Tumour grade was assigned according to the Nottingham Grading System. ER and PR status were assessed on tissue microarrays (TMAs) using immunohistochemistry (IHC) with Dako (Glostrup, Denmark) ER antibody and Leica (Wetzlar, Germany) PR antibody and scored according to the American Society of Clinical Oncology and College of American Pathologists guidelines with a cut-off value of 1% positive tumour nuclei [42]. Her2 status were assessed visually using TMAs as previously described, that is, a score 3 þ is regarded as positive; 2 þ is regarded as equivocal, leading to referral for Her-2 FISH; and 0 and 1 þ are regarded as negative [43].
Full-section haematoxylin and eosin (H&E) slides for the 474 patients were used to score local inflammatory infiltrate according to Klintrup-Makinen (KM) criteria. KM scoring of slides was carried out as previously described. Briefly, tumours were scored on four-point scores based on appearances at the tumour invasive margin. A score of 0 signified that there were no inflammatory cells at tumour's invasive margin; score 1 indicated a mild and patchy inflammatory cells; score 2 denoted a prominent band-like inflammatory reaction at the invasive margin; and score 3 revealed a florid cup-like inflammatory infiltrate at the invasive edge [43, 44]. Individual immune cell types were assessed using IHC staining on TMA sections for macrophages, helper and cytotoxic T-lymphocytes and plasma cells using CD68, CD4, CD8 and CD138 antibodies, respectively [45].
Full-section H&E slides were also used to score the tumour stroma percentage (TSP) as previously reported [46]. Briefly, at 5x magnification, an area representative of the tumour invasive margin was selected, and then a single field of 10x magnification was examined, ensuring that tumour cells were present at all four sides of the image and the area of stroma was calculated as a percentage.
Lymphatic and blood vessel (lymphovascular) invasion were assessed, on 2.5-μm thick sections, using IHC staining with the lymphatic endothelial marker D2-40 (Covance, Monoclonal Antibody, SIG-3730, Princeton, NJ, USA) diluted 1:100 and vascular endothelial marker Factor VIII (Mouse Monoclonal Antibody, NCL-L-Vwf, Leica, Newcastle, UK) diluted 1:100 as previously described [47]. Ki67 proliferation index was assessed by IHC using the median as the cut-off. Tumour budding was evaluated as clusters of 1-5 cancer cells within the tumour microenvironment.
The molecular subtypes were defined as follows: Luminal A: oestrogen (ER) and/or progesterone receptor (PR) positive, Her-2 negative or low proliferative index (< 15%); Luminal B: hormone receptor positive, Her-2 positive or high proliferative index (> 15%); Her-2 subtype: Her-2 positive and hormone receptor negative, any proliferative index; and triple negative: Her-2 negative, hormone receptor negative, any proliferative index.
Immunohistochemistry
Antibody validation for AR-81, AR-515, pERK1/2 and pCDK1 was carried out as previously described [23, 26]. Immunohistochemistry (IHC) was conducted in triplicate on TMAs for Cdk1 phosphorylated at Thr-161 (pCdk1), phosphorylated ERK1/2 (pERK1/2), total AR and AR phosphorylated at ser-81 (AR-81), or ser-515 (AR-515). Slides were dewaxed in xylene and rehydrated through graded alcohol. For total AR, antigen retrieval was performed in Dako cytomation target retrieval solution (Dako UK Ltd.) in a pre-heated water bath, 99°C, 20 min. pERK1/2 antigen retrieval was performed in pH9 Tris-EDTA buffer (10 mM Trizma Base, 0.25 mM EDTA), 96°C, 20 min. Antigen retrieval for remaining proteins was performed under pressure in Tris-EDTA buffer (5 mM Trizma Base, 1 mM EDTA, pH 8), 5 min. Endogenous peroxidase were blocked with 3% H2O2. Sections were further blocked using 5% horse serum (10% casein for pERK1/2) in Tris-buffered saline (TBS). Antibodies for pCdk1 (Abcam), pERK1/2 (Cell Signaling Technology, USA), AR-81 (Merk Millipore, USA), AR-515 (Eurogentec Ltd., Southampton, UK) were incubated overnight at 4°C diluted in Dako antibody diluent at 1:150 (Dako UK Ltd.) Total AR antibody (Dako UK Ltd.) was incubated overnight at 4C at 1:4000. Bound antibody complex was visualised using EnVision plus kit (Dako UK Ltd.) followed by 3,3-diaminobenzidine tetrahydrochloride (DAB, Dako UK Ltd.). Nuclei were counterstained with haematoxylin and blued with Scots Tap Water Substitute, dehydrated through graded alcohol and xylene and mounted with Di-N-Butyl Phthalate in xylene (DPX).
TMAs were scanned using the Hamamatsu NanoZoomer (Welwyn Gardens City, Hertfordshire, UK) at × 20 magnification, and visualization was carried out using Slidepath Digital Image Hub, version 4.0.1 (Leica Biosystems, UK).
Scoring
Only nuclear expression was scored as this represents the active form of each protein. Tissue staining intensity was scored by two blinded independent observers using a weighted histo-score (H-score) method [48, 49]. The H-score was calculated from the formula: (0 × % cells staining negative) + (1 × % cells staining weakly positive) + (2 x % cells staining moderately positive) + (3 × % cells staining strongly positive). The mean H-score from staining conducted in triplicate was used for analysis. Intra-class correlation coefficients (ICCCs) confirmed histo-scoring consistency between observers [49].
Statistical analysis
Only patients with a score for AR, AR-81 and AR-515 were included in the analysis (n = 332). Cut-off values for high or low protein expression were determined by the median of the average values of the intensity of staining. The relationships between variables were assessed using contingency table analysis with the X2 test for linear trend. Correlations coefficients were analysed using a Spearman's rho. Kaplan– Meier curves with log rank analysis was used to examine the effect of protein expression on CSS. Univariate survival analysis was performed using Cox proportional hazards regression. Variables with P-value of < 0.05 were entered into a multivariable model using a backwards conditional method for all patients and triple negative patients. All statistical analyses were two-sided and significance defined as P-value < 0.05. All statistical analysis was performed using the SPSS software version 22 (IBM SPSS, Chicago, IL, USA).
SUPPLEMENTARY MATERIALS FIGURES AND TABLES
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
FUNDING
This work was supported by the University of Glasgow and the Glasgow Breast Cancer Endowment Fund.
REFERENCES
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 3.Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–10874. doi: 10.1073/pnas.191367098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lonning PE, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418–8423. doi: 10.1073/pnas.0932692100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, Perou CM, Ellis MJ, Nielsen TO. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–750. doi: 10.1093/jnci/djp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheang MC, Voduc D, Bajdik C, Leung S, McKinney S, Chia SK, Perou CM, Nielsen TO. Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clinical cancer research. 2008;14:1368–1376. doi: 10.1158/1078-0432.CCR-07-1658. [DOI] [PubMed] [Google Scholar]
- 7.Ward HW. Anti-oestrogen therapy for breast cancer: a trial of tamoxifen at two dose levels. Br Med J. 1973;1:13–14. doi: 10.1136/bmj.1.5844.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knoop AS, Lænkholm AV, Jensen MB, Nielsen KV, Andersen J, Nielsen D, Ejlertsen B, Danish Breast Cancer Cooperative Group Estrogen receptor, Progesterone receptor, HER2 status and Ki67 index and responsiveness to adjuvant tamoxifen in postmenopausal high-risk breast cancer patients enrolled in the DBCG 77C trial. European journal of cancer. 2014;50:1412–1421. doi: 10.1016/j.ejca.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 9.Mavroudis D, Saloustros E, Malamos N, Kakolyris S, Boukovinas I, Papakotoulas P, Kentepozidis N, Ziras N, Georgoulias V. Breast Cancer Investigators of Hellenic Oncology Research Group (HORG), Athens, Greece. Six versus 12 months of adjuvant trastuzumab in combination with dose-dense chemotherapy for women with HER2-positive breast cancer: a multicenter randomized study by the Hellenic Oncology Research Group (HORG) Ann Oncol. 2015;26:1333–1340. doi: 10.1093/annonc/mdv213. [DOI] [PubMed] [Google Scholar]
- 10.Agus DB, Gordon MS, Taylor C, Natale RB, Karlan B, Mendelson DS, Press MF, Allison DE, Sliwkowski MX, Lieberman G, Kelsey SM, Fyfe G. Phase I clinical study of pertuzumab, a novel HER dimerization inhibitor, in patients with advanced cancer. J Clin Oncol. 2005;23:2534–2543. doi: 10.1200/JCO.2005.03.184. [DOI] [PubMed] [Google Scholar]
- 11.Dai X, Xiang L, Li T, Bai Z. Cancer Hallmarks, Biomarkers and Breast Cancer Molecular Subtypes. J Cancer. 2016;7:1281–1294. doi: 10.7150/jca.13141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 13.Sikov WM. Relevance of pCR in breast cancer trials. Oncology (Williston Park) 2014;28(884):886. [PubMed] [Google Scholar]
- 14.Moyano JV, Evans JR, Chen F, Lu M, Werner ME, Yehiely F, Diaz LK, Turbin D, Karaca G, Wiley E, Nielsen TO, Perou CM, Cryns VL. AlphaB-crystallin is a novel oncoprotein that predicts poor clinical outcome in breast cancer. J Clin Invest. 2006;116:261–270. doi: 10.1172/JCI25888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masuda H, Zhang D, Bartholomeusz C, Doihara H, Hortobagyi GN, Ueno NT. Role of epidermal growth factor receptor in breast cancer. Breast Cancer Res Treat. 2012;136:331–345. doi: 10.1007/s10549-012-2289-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chia K, O’Brien M, Brown M, Lim E. Targeting the androgen receptor in breast cancer. Curr Oncol Rep. 2015;17:4. doi: 10.1007/s11912-014-0427-8. [DOI] [PubMed] [Google Scholar]
- 17.Kameyama K, Horie K, Mizutani K, Kato T, Fujita Y, Kawakami K, Kojima T, Miyazaki T, Deguchi T, Ito M. Enzalutamide inhibits proliferation of gemcitabine-resistant bladder cancer cells with increased androgen receptor expression. Int J Oncol. 2017;50:75–84. doi: 10.3892/ijo.2016.3781. [DOI] [PubMed] [Google Scholar]
- 18.Hoang DT, Iczkowski KA, Kilari D, See W, Nevalainen MT. Androgen receptor-dependent and -independent mechanisms driving prostate cancer progression: Opportunities for therapeutic targeting from multiple angles. Oncotarget. 2017;8:3724–3745. doi: 10.18632/oncotarget.12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heisler LE, Evangelou A, Lew AM, Trachtenberg J, Elsholtz HP, Brown TJ. Androgen-dependent cell cycle arrest and apoptotic death in PC-3 prostatic cell cultures expressing a full-length human androgen receptor. Mol Cell Endocrinol. 1997;126:59–73. doi: 10.1016/s0303-7207(96)03970-6. [DOI] [PubMed] [Google Scholar]
- 20.Koryakina Y, Ta HQ, Gioeli D. Androgen receptor phosphorylation: biological context and functional consequences. Endocr Relat Cancer. 2014;21:T131–145. doi: 10.1530/ERC-13-0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Amicis F, Thirugnansampanthan J, Cui Y, Selever J, Beyer A, Parra I, Weigel NL, Herynk MH, Tsimelzon A, Lewis MT, Chamness GC, Hilsenbeck SG, Ando S, Fuqua SA. Androgen receptor overexpression induces tamoxifen resistance in human breast cancer cells. Breast Cancer Res Treat. 2010;121:1–11. doi: 10.1007/s10549-009-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gucalp A, Tolaney S, Isakoff SJ, Ingle JN, Liu MC, Carey LA, Blackwell K, Rugo H, Nabell L, Forero A, Stearns V, Doane AS, Danso M, et al. Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic Breast Cancer. Clinical cancer research. 2013;19:5505–5512. doi: 10.1158/1078-0432.CCR-12-3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGlynn LM, Kirkegaard T, Edwards J, Tovey S, Cameron D, Twelves C, Bartlett JM, Cooke TG. Ras/Raf-1/MAPK pathway mediates response to tamoxifen but not chemotherapy in breast cancer patients. Clinical cancer research. 2009;15:1487–1495. doi: 10.1158/1078-0432.CCR-07-4967. [DOI] [PubMed] [Google Scholar]
- 24.Azzam DG, Tay JW, Greeve MA, Harvey JM, Bentel JM. ERK/MAPK regulation of the androgen responsiveness of breast cancer cells. Adv Exp Med Biol. 2008;617:429–435. doi: 10.1007/978-0-387-69080-3_41. [DOI] [PubMed] [Google Scholar]
- 25.Chen S, Gulla S, Cai C, Balk SP. Androgen receptor serine 81 phosphorylation mediates chromatin binding and transcriptional activation. J Biol Chem. 2012;287:8571–8583. doi: 10.1074/jbc.M111.325290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willder JM, Heng SJ, McCall P, Adams CE, Tannahill C, Fyffe G, Seywright M, Horgan PG, Leung HY, Underwood MA, Edwards J. Androgen receptor phosphorylation at serine 515 by Cdk1 predicts biochemical relapse in prostate cancer patients. Br J Cancer. 2013;108:139–148. doi: 10.1038/bjc.2012.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park S, Koo JS, Kim MS, Park HS, Lee JS, Lee JS, Kim SI, Park BW, Lee KS. Androgen receptor expression is significantly associated with better outcomes in estrogen receptor-positive breast cancers. Ann Oncol. 2011;22:1755–1762. doi: 10.1093/annonc/mdq678. [DOI] [PubMed] [Google Scholar]
- 28.Hickey TE, Robinson JL, Carroll JS, Tilley WD. Minireview: The androgen receptor in breast tissues: growth inhibitor, tumor suppressor, oncogene? Mol Endocrinol. 2012;26:1252–1267. doi: 10.1210/me.2012-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pistelli M, Caramanti M, Biscotti T, Santinelli A, Pagliacci A, De Lisa M, Ballatore Z, Ridolfi F, Maccaroni E, Bracci R, Berardi R, Battelli N, Cascinu S. Androgen receptor expression in early triple-negative breast cancer: clinical significance and prognostic associations. Cancers (Basel) 2014;6:1351–1362. doi: 10.3390/cancers6031351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu R, Dawood S, Holmes MD, Collins LC, Schnitt SJ, Cole K, Marotti JD, Hankinson SE, Colditz GA, Tamimi RM. Androgen receptor expression and breast cancer survival in postmenopausal women. Clinical cancer research. 2011;17:1867–1874. doi: 10.1158/1078-0432.CCR-10-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asano Y, Kashiwagi S, Goto W, Tanaka S, Morisaki T, Takashima T, Noda S, Onoda N, Ohsawa M, Hirakawa K, Ohira M. Expression and Clinical Significance of Androgen Receptor in Triple-Negative Breast Cancer. Cancers (Basel) 2017:9. doi: 10.3390/cancers9010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang C, Pan B, Zhu H, Zhou Y, Mao F, Lin Y, Xu Q, Sun Q. Prognostic value of androgen receptor in triple negative breast cancer: A meta-analysis. Oncotarget. 2016;7:46482–46491. doi: 10.18632/oncotarget.10208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang HS, Kuang XY, Sun WL, Xu Y, Zheng YZ, Liu YR, Lang GT, Qiao F, Hu X, Shao ZM. Androgen receptor expression predicts different clinical outcomes for breast cancer patients stratified by hormone receptor status. Oncotarget. 2016;7:41285–41293. doi: 10.18632/oncotarget.9778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi JE, Kang SH, Lee SJ, Bae YK. Androgen receptor expression predicts decreased survival in early stage triple-negative breast cancer. Annals of surgical oncology. 2015;22:82–89. doi: 10.1245/s10434-014-3984-z. [DOI] [PubMed] [Google Scholar]
- 35.Ren Q, Zhang L, Ruoff R, Ha S, Wang J, Jain S, Reuter V, Gerald W, Giri DD, Melamed J, Garabedian MJ, Lee P, Logan SK. Expression of androgen receptor and its phosphorylated forms in breast cancer progression. Cancer. 2013;119:2532–2540. doi: 10.1002/cncr.28092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ponguta LA, Gregory CW, French FS, Wilson EM. Site-specific androgen receptor serine phosphorylation linked to epidermal growth factor-dependent growth of castration-recurrent prostate cancer. J Biol Chem. 2008;283:20989–21001. doi: 10.1074/jbc.M802392200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chia KM, Liu J, Francis GD, Naderi A. A feedback loop between androgen receptor and ERK signaling in estrogen receptor-negative breast cancer. Neoplasia. 2011;13:154–166. doi: 10.1593/neo.101324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ellis TM, Moser MT, Le PT Flanigan RC, Kwon ED. Alterations in peripheral B cells and B cell progenitors following androgen ablation in mice. Int Immunol. 2001;13:553–558. doi: 10.1093/intimm/13.4.553. [DOI] [PubMed] [Google Scholar]
- 39.Vignozzi L, Cellai I, Santi R, Lombardelli L, Morelli A, Comeglio P, Filippi S, Logiodice F, Carini M, Nesi G, Gacci M, Piccinni MP, Adorini L, Maggi M. Antiinflammatory effect of androgen receptor activation in human benign prostatic hyperplasia cells. J Endocrinol. 2012;214:31–43. doi: 10.1530/JOE-12-0142. [DOI] [PubMed] [Google Scholar]
- 40.Traina TA, O’Shaughnessy J, Nanda R, Schwartzberg L, Abramson V, Cortes J, Peterson A, Tudor IC, Blaney M, Steinberg JL, Kelly C, Trudeau M, Awada A, et al. Preliminary results from a phase 2 single-arm study of enzalutamide, an androgen receptor (AR) inhibitor, in advanced AR plus triple-negative breast cancer (TNBC) Cancer Research. 2015:75. [Google Scholar]
- 41.Lehmann BD, Bauer JA, Schafer JM, Pendleton CS, Tang L, Johnson KC, Chen X, Balko JM, Gomez H, Arteaga CL, Mills GB, Sanders ME, Pietenpol JA. PIK3CA mutations in androgen receptor-positive triple negative breast cancer confer sensitivity to the combination of PI3K and androgen receptor inhibitors. Breast Cancer Res. 2014;16:406. doi: 10.1186/s13058-014-0406-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S. American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract. 2010;6:195–197. doi: 10.1200/JOP.777003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mohammed ZM, Going JJ, Edwards J, Elsberger B, Doughty JC, McMillan DC. The relationship between components of tumour inflammatory cell infiltrate and clinicopathological factors and survival in patients with primary operable invasive ductal breast cancer. Br J Cancer. 2012;107:864–873. doi: 10.1038/bjc.2012.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klintrup K, Makinen JM, Kauppila S, Vare PO, Melkko J, Tuominen H, Tuppurainen K, Makela J, Karttunen TJ, Makinen MJ. Inflammation and prognosis in colorectal cancer. European journal of cancer. 2005;41:2645–2654. doi: 10.1016/j.ejca.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 45.Mohammed ZM, Going JJ, Edwards J, Elsberger B, McMillan DC. The relationship between lymphocyte subsets and clinico-pathological determinants of survival in patients with primary operable invasive ductal breast cancer. Br J Cancer. 2013;109:1676–1684. doi: 10.1038/bjc.2013.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gujam FJ, Edwards J, Mohammed ZM, Going JJ, McMillan DC. The relationship between the tumour stroma percentage, clinicopathological characteristics and outcome in patients with operable ductal breast cancer. Br J Cancer. 2014;111:157–165. doi: 10.1038/bjc.2014.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gujam FJ, Going JJ, Edwards J, Mohammed ZM, McMillan DC. The role of lymphatic and blood vessel invasion in predicting survival and methods of detection in patients with primary operable breast cancer. Crit Rev Oncol Hematol. 2014;89:231–241. doi: 10.1016/j.critrevonc.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 48.McCarty KS, Jr, Szabo E, Flowers JL, Cox EB, Leight GS, Miller L, Konrath J, Soper JT, Budwit DA, Creasman WT, Seigler HF, McCarty KS., Sr Use of a monoclonal anti-estrogen receptor antibody in the immunohistochemical evaluation of human tumors. Cancer Res. 1986;46:4244s–4248s. [PubMed] [Google Scholar]
- 49.Kirkegaard T, Edwards J, Tovey S, McGlynn LM, Krishna SN, Mukherjee R, Tam L, Munro AF, Dunne B, Bartlett JM. Observer variation in immunohistochemical analysis of protein expression, time for a change? Histopathology. 2006;48:787–794. doi: 10.1111/j.1365-2559.2006.02412.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


