Abstract
Introduction: The unchanged global HIV incidence may be related to ignoring acute HIV infection (AHI). This scoping review examines diagnostic, clinical, and public health implications of identifying and treating persons with AHI.
Methods: We searched PubMed, in addition to hand-review of key journals identifying research pertaining to AHI detection and treatment. We focused on the relative contribution of AHI to transmission and the diagnostic, clinical, and public health implications. We prioritized research from low- and middle-income countries (LMICs) published in the last fifteen years.
Results and Discussion: Extensive AHI research and limited routine AHI detection and treatment have begun in LMIC. Diagnostic challenges include ease-of-use, suitability for application and distribution in LMIC, and throughput for high-volume testing. Risk score algorithms have been used in LMIC to screen for AHI among individuals with behavioural and clinical characteristics more often associated with AHI. However, algorithms have not been implemented outside research settings. From a clinical perspective, there are substantial immunological and virological benefits to identifying and treating persons with AHI – evading the irreversible damage to host immune systems and seeding of viral reservoirs that occurs during untreated acute infection. The therapeutic benefits require rapid initiation of antiretrovirals, a logistical challenge in the absence of point-of-care testing. From a public health perspective, AHI diagnosis and treatment is critical to: decrease transmission via viral load reduction and behavioural interventions; improve pre-exposure prophylaxis outcomes by avoiding treatment initiation for HIV-seronegative persons with AHI; and, enhance partner services via notification for persons recently exposed or likely transmitting.
Conclusions: There are undeniable clinical and public health benefits to AHI detection and treatment, but also substantial diagnostic and logistical barriers to implementation and scale-up. Effective early ART initiation may be critical for HIV eradication efforts, but widespread use in LMIC requires simple and accurate diagnostic tools. Implementation research is critical to facilitate sustainable integration of AHI detection and treatment into existing health systems and will be essential for prospective evaluation of testing algorithms, point-of-care diagnostics, and efficacious and effective first-line regimens.
Keywords: acute HIV infection, antiretroviral therapy, diagnostics, early HIV, guidelines, low- and middle-income countries, primary HIV
Introduction
Despite comprehensive HIV interventions and scaled-up antiretroviral therapy (ART) services in many regions, there are still two million new adult HIV cases each year [1]. Failure of existing prevention initiatives, in which many persons with HIV are not on ART nor virally suppressed, may explain some of the ongoing transmission events. However, the largely unchanged HIV incidence must in part be the result of current programmes failing to detect and treat acute HIV infection [2]. According to the original Fiebig classification [3], acute infection is defined as the period between viral acquisition and emergence of HIV-specific antibodies, generally accompanied by a burst of viremia [4]. By comparison, early infection, inclusive of the acute phase, represents an approximately 6-month period of increased transmission efficiency [5–9].People with acute or early infection (hereafter referred to as AHI) likely play a disproportionate role in HIV transmission [6,7]; heightened efforts to identify and manage persons with AHI are critical to decrease incidence.
Despite the importance of AHI, optimal clinical and public health strategies for AHI are unclear. The US Department of Health and Human Services HIV guidelines recommend universal screening and treatment of AHI and the European AIDS Clinical Society also recommends universal treatment for primary HIV infection [10–12]. Although the International AIDS Society and the World Health Organization’s (WHO) most recent guidelines support scale-up of testing and immediate treatment for all people diagnosed with HIV, there is no specific recommendation regarding diagnostic strategies or ART for persons with AHI [13–16]. From a public health standpoint, undiagnosed AHI could interfere with the extent to which comprehensive strategies such as Treat All could effectively achieve desired population health benefits. Undiagnosed AHI may also compromise the effectiveness of pre-exposure prophylaxis (PrEP), increasing the risk of resistant virus if PrEP is initiated [15,17]. Early treatment initiation is required to avert irreversible damage to the immune system [18], and to shrink the latent reservoir that renders HIV incurable [19,20]
A public health approach to AHI is necessary, especially in resource-constrained low- and middle-income countries (LMICs). The case for prioritizing resources to detect and treat persons with AHI demands a thorough evaluation of the state of knowledge and projected impact of AHI on new and established HIV epidemics. Previous AHI reviews have focused on basic science [19,21], concentrated epidemics in high-income countries [22–25], and programmatic considerations [26,27]. The purpose of this scoping review is to examine the diagnostic, clinical, and public health implications of identifying and treating persons with AHI, especially in LMIC settings.
Methods
We conducted a scoping review [28] synthesizing the most recent literature on clinical and public health implications of widespread AHI detection and treatment. This review includes clinical trials, observational studies, systematic and non-systematic reviews, mathematical modelling, and best practice guidelines. Scoping reviews are distinct from systematic reviews in the absence of a priori article criteria; although we emphasized research published in the last 15 years, there were no explicit inclusion nor exclusion criteria for articles. Instead, this included papers that map the current state of research, identifying gaps in knowledge [29]. We examined a broad range of literature and topics relevant to the clinical and public health effects of under-diagnosed and under-treated AHI. Based on the scoping review, we summarize key policy implications and areas for research priorities.
We identified studies using keyword searches in PubMed (last searched 8 October 2016), expert opinion, and current regional and international HIV testing and treatment guidelines. For database searches, we used phrases and synonymous variations of the following terms: acute HIV, primary HIV, early HIV, treatment, and diagnosis. We also identified studies based on searches of reference lists, hand-searching key journals identified from initial database inquiries, and unpublished conference abstracts. We prioritized inclusion of LMIC research. Our search included studies that provided empirical data on AHI published in the last fifteen years. We included studies that had the following elements: (1) focus on AHI detection, treatment, or public health features (i.e., algorithms to detect AHI, implications of AHI on PrEP); (2) provide empirical data on AHI testing or treatment outcomes; (3) evaluate natural history of AHI as it relates to morbidity and transmission; or (4) model the impact or role of AHI in emerging or established epidemics.
Results and discussion
Impact of AHI on secondary transmission
Data from clinical studies, phylogenetic research, and modelling support the importance of AHI in HIV transmission in LMIC as well as wealthy nations among both MSM and heterosexually-dominated epidemics. Highly infectious founder viruses [30] coupled with 10-fold higher viral loads [3,5–8,31,32] suggest there is a greater likelihood of transmission during AHI.
Empirical data estimating HIV transmission rates are sparse. The Rakai study is one of the largest prospective cohort studies to investigate transmission rates, enrolling greater than 15,000 adults from the Rakai district in Uganda and identifying over 400 serodiscordant couples for assessment of transmission events and the associated risk of transmission by stage of infection of the index participant [33]. Rakai data have been evaluated three separate times with widely different estimates for the extent to which AHI accounts for onward transmission among heterosexual serodiscordant couples (Table 1) [34–36]. These differences can be ascribed to adjustments in estimated duration of infectious stages; assumptions regarding determination of transmission hazards (i.e. reliance on self-reported coital frequency, as a function of time, or using predicted viral load trajectories); accounting for diversity in both infectiousness and susceptibility; and modification to the initial analyses’ couple exclusion criteria. Importantly, the proportion of transmissions attributable to AHI is likely to change with increased ART coverage – with more HIV-infected persons virally suppressed on ART, and thus less likely to transmit, persons with AHI may become an increasingly important population to target to reduce incidence.
Table 1.
Variability in estimated HIV-1 transmission risk during AHI vs. chronic infection as evaluated using Rakai-based HIV-discordant couple cohort
| Author, year | AHI definition (months) | Analytic methods | Assumptions | Outcomes: Increased infectiousness, AHI vs. chronic infection |
|---|---|---|---|---|
| Wawer et al.[34] | 0–5 | Estimated per coital transmission rates by index partner infection stage |
|
12-fold Per coital act: 0.0082 vs. 0.0007 |
| Hollingsworth et al.[35] | 0–3 | Probabilistic model estimated transmission hazards by infection stage |
|
26-fold Transmission hazard/100 person-years: 276 vs. 10.6 |
| Bellan et al.[36] | 0–1.7 | Simulated cohort model, fitting Rakai-population transmission events based on transmission hazard and AHI duration using Bayesian methods |
|
5-fold Median transmission hazard/year: 0.62 vs. 0.12 |
aOriginal cohort censorship of serodiscordant couples based on single study visits prior to (a) being lost to follow-up, (b) couple dissolution, or (c) study termination.
AHI – acute HIV infection; VL – viral load.
Modelling AHI’s role in epidemics
Phylogenetic research has demonstrated the importance of AHI in HIV epidemics. Phylogenetic studies show that persons with recent infection drive transmission clusters; however, estimates are highly variable, identifying persons with AHI as source infection for between 10% and 50% of all transmissions [22,37–47]. Discrepancies are due to differences in epidemic stage, definitions of AHI, and variation in risk behaviours (i.e., anal vs. vaginal intercourse) by region and population [48]. For example, partner-change patterns are likely variable across regions and sub-populations, thus estimates derived from European men who have sex with men (MSM) may not be generalizable to heterosexual transmission in sub-Saharan Africa.
Mathematical models largely agree that persons with AHI are responsible for a disproportionate share of all transmissions, although there is significant variability in estimates [34,49–54]. Models based on data from Malawi estimated that approximately 40% of transmissions were attributable to persons with AHI [9], similar to results from the US among MSM [54]. However, models populated using data from elsewhere in sub-Saharan Africa predict AHI-attributable transmissions <20% [55], or as low as 3% [56]. Similar to the discrepancies across phylogenetic studies, differences in mathematical model estimates can be traced to variation in model design and input assumptions. Ongoing population-based studies, including PopART [57] and SEARCH [58], will help to better parameterize models.
Diagnosing AHI
AHI diagnostics
Diagnosing AHI is complicated by its brief duration and absence of detectable antibodies. Third-generation HIV rapid diagnostic tests (RDTs), the backbone of testing in most LMICs [14], only detect HIV-specific antibodies, missing the earliest pre-antibody phase (Table 2). Fourth-generation antigen-antibody combination enzyme immunoassays (EIA) shorten the seroconversion detection window, detecting both HIV-1/2 antibodies and p24 antigens [59–64], and detects the majority of persons with AHI when applied after a negative 3rd generation test [65]. Fourth-generation tests are now standard in Europe, the USA, and parts of Latin America [66,67], but scale up may be more difficult in other LMIC where the majority of testing takes place in lower-tier health facilities. Although experience with 4th generation EIAs in LMICs has been largely restricted to research study settings, results are encouraging [68]. Nonetheless, compared to RNA testing, 4th generation assays miss patients in the earliest stages of AHI (prior to detectable p24 antigen [69]) – precisely the group that some studies suggest may benefit most from immediate treatment [19]. Fourth-generation tests may also be falsely negative in the setting of early treatment of AHI: one Thai study found that 17% of patients retested with 4th generation assays after treatment during AHI either failed to convert or reverted to nonreactivity, compared with 4% for 3rd generation tests [70]. Pilot testing of 4th generation EIAs and NAT such as the ongoing RV254/SEARCH010 cohort study [71] will be critical to better understand more widespread use of this technology.
Table 2.
HIV diagnostics in the context of AHI
| Test | Advantages | Disadvantages | Cost (per test, USD)b |
|---|---|---|---|
| 3rd generation antibody (POC) |
|
|
|
| 4th generation antibody/antigen (EIA) |
|
|
|
| 4th generation (POC) |
|
|
|
| Nucleic acid amplification testing (NAT) technologiesa |
|
|
|
| NAT technology (POC) |
|
|
|
awith and without pooling;
ŦRamos et al. propose a modified testing algorithm through which reduced signal-to-cutoff ratios would trigger confirmatory Multispot and NAT testing to increase sensitivity of 4th generation testing in detecting AHI. This ratio is determined using the signal strength of a sample compared to the signal strength of an internal cutoff with ratios ≥1.0 defined as positive by the manufacturer; LMIC – low- and middle-income countries; NAT – nucleic acid amplification testing; POC – point-of-care.
bData from Cheryl Johnson, co-author.
The effectiveness of AHI diagnostics will depend on laboratory complexity, costs, and a range of implementation considerations. Ideal AHI diagnostics will provide reliable and rapid, preferably same visit results and would be easy to use by lay providers requiring minimal additional training for those versed in 3rd generation RDT. Use of more sensitive tests that shorten the window period are essential to confirm HIV-negative status prior to initiating PrEP as false-negative results risk development of drug resistance [17,73–76].
Diagnostic algorithms for AHI
Optimal algorithms must balance the consequences of missed diagnoses, false-positive results, and algorithm ease-of-use. Many updated HIV testing algorithms combine 3rd and/or 4th generation assays with more sensitive nucleic acid testing (NAT) technologies [12,67]. NAT has been used successfully for AHI screening in LMICs, even using finger stick specimens [32,69,77–85]. However, in large part due to the resource and logistical limitations, there have been no NAT or 4th generation assay programmes integrated as routine practice in LMICs.
In some populations (e.g., STI patients, MSM), screening for AHI with NAT is cost-effective [80,86–88]. Among MSM in the US, 3rd generation testing followed by NAT was cost saving compared to alternative algorithms [23], and NAT testing alone may be cost-effective [89]. Combining multiple samples for pooled NAT may be a cost-effective alternative compared to testing individual specimens [77,90–92]. In Thailand, the addition of pooled NAT following 4th generation testing improved AHI detection rates, increasing AHI diagnosis by nearly 40% [68,93]. Importantly, pooling strategies also increased screening costs by 22% [68]. These outcomes emphasize that ideal testing algorithms vary according to AHI prevalence, laboratory capacity, and screening volume. Some programmes have elected to recommend repeat testing for higher-risk, seronegative persons, though this approach fundamentally misses AHI diagnoses.
Point-of-care testing pipeline for AHI
Both NAT and 4th generation EIAs necessitate relatively sophisticated laboratory infrastructure, venipuncture whole blood, and patient follow-up. Although centralized laboratory testing has been implemented for other diagnostic and monitoring strategies in LMICs, including early-infant diagnosis and VL monitoring, centralized testing interferes with the rapid turnaround time preferred for AHI diagnosis and intervention. The Alere® Determine HIV-1/2 Ag/Ab “Combo” device is one of the most studied 4th generation point-of care (POC) technology on the market, and has recently received WHO prequalification status [94]. However, extensive field testing in both the UK and sub-Saharan Africa has demonstrated poor p24 detection rates and frequent false-positive results [95]. A pooled analysis of Determine Combo p24 antigen data from 17,000 participants showed poor sensitivity and high specificity [96–100]. Although newer versions of the Combo assay suggest improved p24 detection on stored specimens, field testing will be critical to confirm performance [101].
The Bio-Rad Geenius™ HIV 1/2 supplemental assay, an immunochromatographic rapid test, measures multiple antibodies and antigens and may simultaneously confirm infection and diagnose early post-antibody conversion acute infections, thus lengthening the diagnostic window for AHI [102]. Other promising POC NAT devices include the Alere Q® [103] (now with WHO prequalification status and validated for RNA detection among infants and children [104]), the SAMBA® semi-quantitative assay [105], the Liat® HIV Quant VL assay [106], and the Xpert® HIV-1 Qual assay [107,108]. Designed to run on the GeneXpert® platform, the dual HIV and TB-disease identification capacity of the Xpert® make it especially appealing given GeneXpert® existing and expanding presence in sub-Saharan Africa, and may be more sensitive and specific for diagnosing AHI compared to other diagnostics under evaluation [108]. Although none designed specifically for AHI screening, the various platforms’ capacity to detect HIV RNA suggests potential for future screening applications [71]. Ultimately, effective and affordable POC tests are needed for effective widespread AHI screening.
Clinical and symptom-driven risk-scores for AHI screening
Approximately 29–69% of persons with AHI may seek healthcare for symptoms immediately following HIV acquisition [109,110]. International guidelines have not established a diagnostic strategy for detecting persons with AHI [15]. In LMIC, prioritizing patients presenting with nonspecific symptoms related to acute retroviral illness, such as fever or gastrointestinal distress, may be one approach to optimize screening [110–113]. Unfortunately, AHI can be confused with malaria in many regions of Africa. In surveys of healthcare seeking febrile adults in Uganda [78] and Kenya [114], the prevalence of AHI was greater than 1% and in some clinics was similar to that of malaria [114]. Symptoms – including fever, rash, or diarrhoea – generally emerge approximately 2 weeks following HIV infection [32,115]. Among those presenting with symptoms, the number of symptoms correlates with higher pre-seroconversion peak plasma VL [116], and symptoms tend to cluster immediately preceding or during the period of peak viremia [32]. Although many patients with AHI do not develop symptoms [32], symptomatic patients who seek care during AHI present an opportunity for detection and immediate treatment initiation [117], and may identify persons with higher peak VL [116], and higher VL set point [32,118].
Risk-score algorithms concentrate scarce testing resources with substantial potential cost savings [82,119–121]. Screening patients who meet predefined algorithm thresholds (5–50% of all patients) may identify the majority (>80%) of persons with AHI [119]. However, performance of risk scores vary according to the prevalence of illness presenting with similar symptoms (e.g., malaria), the clinical setting (e.g., STI clinic), and the accuracy of reported symptoms or behaviours (Figure 1) [24].
Figure 1.
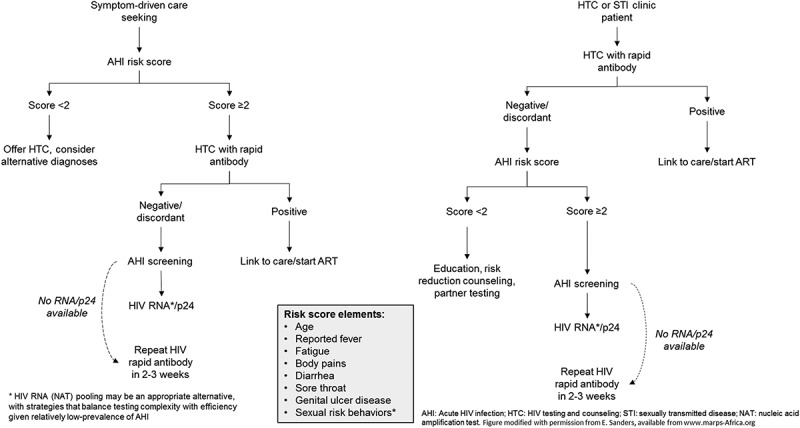
Algorithm for targeting acute HIV screening resources using clinical risk score.
Treating persons with AHI
Updated WHO guidelines recommend all HIV-infected persons receive ART, but make no recommendation about optimal regimens for those with AHI [15]. Treatment during AHI reduces viral reservoir seeding, limits viral diversity, preserves immune responses, and decreases chronic residual inflammation (Figure 2). The early interference with establishment of viral reservoirs may also have important implications for viral eradication efforts. Interruption of therapy initiated early during AHI may result in temporarily lower VL set point, delayed need for restarting ART [122], and, in some cases, sustained virological remission off therapy [123,124]. However, realizing these benefits requires very early ART initiation and may necessitate therapeutic regimens not currently widely available in LMIC.
Figure 2.
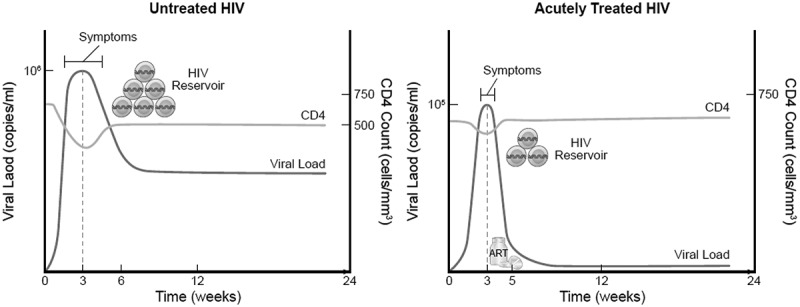
Projected viral load, CD4 cell count, reservoir seeding, and symptom duration comparing untreated vs. treated acute HIV infection.
Inflammatory and immune benefits of ART initiated during AHI
ART initiated during AHI may drastically change the course of infection. The seeding of viral reservoirs occurs soon after infection and poses a major barrier to cure efforts [125]. Viral reservoirs are a collection of cells harbouring virus despite suppressive therapy. ART initiated during the first two weeks of infection is the most effective strategy for limiting size of latent reservoirs [20,126–130]. Early ART reduces overall level of proviruses, and thus the number of intact, potentially transmissible, proviruses [131], preserves mucosal CD4 T-cell counts, and reverses inflammation in major anatomical reservoirs including gut and lymph nodes [132,133]. Early ART also reduces the number of infected cells, lowering cell-associated HIV DNA levels [130] and, in doing so, reducing the viral set point [134]. Conversely, ART initiated during chronic infection results in larger reservoirs, and contributes to rapid viral rebound with ART interruption [135–137].
ART initiation during AHI also results in improved HIV-specific immune responses, potentially slowing disease progression [124]. CD4 T-cell depletion begins shortly after infection and delaying ART compromises immune system recovery [138–141]. CD4 cell counts and CD4/CD8 ratios predict long-term morbidity and mortality [142,143]; CD4, CD8, and CD4/CD8 ratios are more likely to normalize with treatment started during AHI compared to delayed treatment [141,144–147], with CD4 cell counts normalizing within one year [148]. Very early ART (within 40 days of the estimated date of infection) is associated with a significant increase in the CD4/CD8 ratio compared to delayed ART [149]. ART initiated during AHI is associated with lower T-cell activation levels at 48 months compared to ART initiated during chronic infection, improving immune-system recovery and potentially decreasing mortality [138]. Lifetime durability of these responses is unknown, although retrospective analyses suggest sustained reactions for up to five years [141].
Ideal ART regimens for AHI
In the era of expanded ART options, another consideration is what regimen is appropriate to start during AHI. Observational and randomized studies comparing standard ART to “intensified” regimens that include integrase or entry inhibitors consistently demonstrate similar effectiveness in raising CD4 T-cell counts, and lowering markers of immune activation and cell-associated DNA [150–153]. Although intensified regimens may not be necessary to reap virological or immunological benefits, intensified regimens result in a more rapid VL decline in blood and genital secretions [154]. Rapid VL reduction during AHI is critical to interrupt transmission, and is best facilitated by use of integrase inhibitors [155,156]. Other factors to consider in regimen selection include tolerability (i.e., toxicity), resistance (both transmitted and genetic barriers to acquiring mutations), and financial implications. Importantly, current WHO treatment guidelines do not include the newer entry inhibitors. Ultimately, in the setting of safe and potent ART options, the health consequences of not treating persons with AHI likely outweigh the risks inherent to withholding treatment.
Public health implications of AHI diagnosis and treatment
AHI accounts for a small, but nontrivial portion, of all new HIV diagnoses – identifying an additional two to 10% of HIV above antibody-only testing depending on risk profile of screened patient population (i.e. STI clinic vs. general outpatient setting) [79,83,84,90,157–161]. Insufficient attention to AHI-centric public health interventions could partially explain the stagnant global HIV incidence trends: primarily driven by LMIC in sub-Saharan Africa, and with significant heterogeneity by region, stable incidence despite increases in treatment coverage towards UN 90–90–90 treatment goals over the past five years reinforce inadequacy of current screening strategies [162–164].
PrEP in context of undiagnosed AHI
Missing persons with AHI could also have substantial consequences for PrEP programmes. WHO guidelines recommend PrEP for HIV-negative persons at substantial risk of HIV infection [15]. There is likely substantial overlap in the population that would be eligible for PrEP and those who are at greatest risk of AHI [165]. Given that PrEP formulations and WHO-recommended first-line therapy share a common tenofovir-containing backbone, induced resistance selected for by PrEP administration to persons with unrecognized AHI could have significant public health implications. Although induced resistance may decay following therapy interruption [166], these mutations must be accounted for in future ART selections. However, mandating complex AHI testing algorithms prior to PrEP initiation could impede PrEP implementation.
Public health interventions targeting AHI partners and behaviours
AHI screening enables partner notification services and behavioural interventions. AHI screening has proved feasible in several low-income [77,79,84], middle-income [32], and high-income settings [24,65,90]. Despite limited data regarding feasibility of AHI screening outside of clinical research settings, studies suggest that testing is both acceptable and effective. Implementation research is critical to tease out setting specific implementation barriers to more widespread AHI detection and treatment.
Assisted partner notification, including provider-initiated partner notification, is a proven, safe, and cost-effective intervention for identifying persons with undiagnosed infection [167–172], although programmes are rarely implemented in LMIC. AHI diagnosis may facilitate more effective partner services. Persons with AHI name twice as many sex partners in the three months preceding diagnosis compared to persons newly diagnosed with chronic infection [173,174]. In the context of more recent infection, named partners are also more likely to be infected with HIV [173,175], although many of these source partners may have been previously diagnosed [176].
AHI is often diagnosed during a period of increased sexual risk, suggesting the importance of rapid behavioural interventions [177–179]. Given that persons with AHI can name more recent sex partners who are respectively at greater risk of HIV, this provides an opportunity for behavioural interventions among serodiscordant couples [180] or serosorting [181]. The feasibility of behavioural interventions is complicated by the need for programmes to rapidly change behaviour in the setting of increased sexual risk activities, anxiety, depression, and substance abuse [181–184]. Despite perceived changes in behaviour, many with AHI are unable to abstain from sex or use condoms, particularly with long-term partners [185]. Incident sexually transmitted infections after diagnosis suggests ongoing risk behaviours despite risk reduction counselling and retention in care [186]. The appropriate duration and intensity of behavioural interventions is unknown, although it seems that modified post-test counselling can adequately convey messages of increased infectiousness and possibly facilitate behaviour change in the short term [177,178].
Unique challenges and opportunities in treating AHI
Along with appropriate counselling, early ART initiation during AHI is critical to limit the spread of HIV attributable to persons with AHI [9,187]. High viral loads are a modifiable risk factor for HIV transmission [3]. Same-day ART initiation for persons with AHI, in line with current Treat All initiatives, results in more rapid viral suppression compared to non-same day initiation [188]. ART in AHI is highly effective and viral failure is uncommon [189]. While virological response for persons with chronic infection is characterized by suppression 6 months after ART initiation, the most effective means of reducing transmission during AHI requires regimens that rapidly reduce viral burden in genital fluids. Among Thai MSM with AHI, comparing a 3-drug regimen (2 NRTI + 1 NNRTI) to that same regimen intensified with entry and integrase inhibitors (5 drug regimen, including raltegravir), persons on the 5-drug regimen achieved viral suppression in seminal fluid faster compared to standard regimen (13 vs. 24 days); this period of sustained viremia may represent a critical window of ongoing transmission [154]. Although not currently included in most first-line schedules in LMIC, the more rapid viral load decline with inclusion of an integrase inhibitor agent make this an important regimen modification to reap potential transmission benefits of early ART during AHI. Ultimately, data demonstrating the feasibility and effectiveness of early ART in suppressing viremia and interrupting transmission suggest that appropriately-implemented treatment-based interventions may change the course of the global epidemic.
Viral response depends on regimen and patients’ adherence behaviours. For example, the 24-week failure rate among a Thai cohort (1.1%) was significantly lower than the 10% failure rate among a Boston-based cohort also receiving early-ART [190]. The difference may be related to the differences in regimen selection, with the Boston study demanding a higher pill burden. Despite the potential suppression benefits of more potent regimens, compared to three-drug combinations, adherence to the intensified five-drug regimen is generally worse [150,151], likely related to the necessary twice-daily dosing and more frequent adverse effects. Although more complex regimens may be preferred for rapid reduction of VL, the adverse effects, risk of sub-standard adherence, and drug costs could prohibit widespread use.
System-wide barriers to AHI diagnosis and treatment scale up
Existing public health systems are poorly equipped to deal with AHI detection, treatment, and linkage to prevention and care. The potential to stop transmission during AHI using partner tracing, behavioural, or biomedical interventions relies on rapid diagnosis and ART initiation. Barriers to AHI diagnosis include complexity and expense of diagnostics, limited training among health professionals to implement diagnostics on a wide scale, and the relative brevity of the infection stage [191]. Increased HIV testing by lay providers has substantially improved access to HIV testing services [16]. Unfortunately, even 4th generation assays require non-capillary whole-blood or plasma specimens, and thus may not be ready for scale up. Point-of-care tests are critical for expansion of AHI screening, and there are promising alternative platforms under development and in early field implementation. However, cost, ease-of-use, adequate sensitivity for screening objectives, and efficient throughput for high-volume screening are still under investigation. In the absence of widely available diagnostics capable of detecting AHI, one strategy includes encouraging retesting 2–4 weeks after negative or inconclusive antibody results for persons with acute retroviral symptoms at time of presentation. Unfortunately, over 40% of participants failed to return for follow-up testing even after enhanced appointment reminders using SMS or in-person cues [192].
Barriers to diagnosis and treatment are intimately intertwined. Therapy initiated within two weeks of infection may be most beneficial for reduced transmission and improved immune response. However, this narrow window requires extremely sensitive diagnostic assays and system capacity to start ART almost immediately after a positive result. Although rapid and reliable diagnosis is the critical first step for AHI intervention, comprehensive management will also require appropriate provider messaging, patient education, and possibly AHI-specific treatment strategies.
Conclusions
AHI detection and treatment has important diagnostic, clinical, and public health implications [193]. Treatment is beneficial for the infected individual, with likely long-term immune-virological benefits with early treatment initiation, and extensive research has demonstrated advantages of early ART, regardless of regimen. Immediate ART is also advantageous to uninfected sex partners, reducing the risk of acquisition in the setting of suppressed viremia. Furthermore, immediate ART during AHI has profound implications for HIV cure efforts; by eliminating or limiting establishment of latent reservoirs and preserving immune responses, early ART during AHI may be the key to ongoing eradication strategies [194]. Although, currently, treatment interruption is an unfavourable approach for AHI management, the development of predictive algorithms with HIV eradication objectives, particularly in LMIC, will need to take into consideration parameters that may influence control of infection [195,196], such as route of infection, ethnicity, and hormonally driven gender-based differences [197,198], including evidence of lower rates of inducible virus among women on suppressive ART [199]
We identified several research priorities. First, we need prospective assessment of appropriate testing strategies and algorithms for AHI diagnosis, including evaluation of risk score performance for screening in LMIC using same-day POC tests. This is important for implementation and policies related to scaling up AHI detection and treatment as well as PrEP implementation in LMIC. Second, further diagnostic research on POC assays to detect early and acute infection is key. Third, we need investigations into the feasibility, cost-effectiveness and implications for treatment switch algorithms associated with incorporating integrase inhibitors into first-line regimen recommendations. Use of integrase inhibitors will be especially important among certain high-risk groups for whom rapid reduction in viral load is critical, such as pregnant women. Finally, implementation research in the context of expanded testing and treatment goals will become increasingly important to understand how to incorporate routine AHI detection and treatment into existing health systems.
The outlined research agenda is essential for guiding policy change. Nonetheless, we propose that LMIC with AHI testing capacity should immediately implement AHI screening among high-risk populations. Targeted screening utilizing risk score algorithms may help identify persons with AHI and focus limited resources without confining screening to specific clinics. Additional approaches include social and sexual partner recruitment and notification to help increase screening yields. Scaling up testing requires extensive personnel training and patient education and should be pursued in settings in which immediate ART as recommended through the Treat All policy can be offered.
This scoping review addresses the broad topic of clinical and public health implications of AHI. As a scoping review, we did not define inclusion nor exclusion criteria and, as such, we cannot assess the quality of published articles that are included in the review in a standardized fashion. Unlike systematic reviews, scoping reviews such as this do not synthesize evidence in a manner that allows relative weight of alternative research findings or interventions, offering instead a narrative from which future systematic reviews may be motivated. Despite these limitations, the scoping review provides flexibility and breadth in study design and publication inclusion on a fast-changing and, specifically in LMIC, under-researched topic.
Unchanged HIV incidence rates despite ART scale-up suggest the importance of targeting diagnostic and treatment interventions to groups responsible for a disproportionate share of new infections, including persons with AHI. Although current WHO guidelines recommend a Treat All approach, explicit guidance regarding AHI testing and treatment approaches are urgently needed. Further AHI research and policy development can help to fill this gap.
Acknowledgements
EJS is supported by Wellcome Trust and the KWTRP at the Centre for Geographical Medicine Research-Kilifi (supported by core funding from the Wellcome Trust (#077092)), with support from the International AIDS Vaccine Initiative. JDT is supported by NIAID R21AI20549. SF is supported by NIHR BRC. SER was supported by R01 AI114320, F30 MH098731 and T32 GM008719. The views expressed are those of the authors and should not be construed to represent the positions of the U.S. Army or the Department of Defense or other institutions listed.
Biography
All authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors. SER, MV, MD, MSC, and JDT contributed to the conception, design, and literature review. SER and JDT drafted the initial manuscript. JA, SF, CJ, EJS, OS, ASC, CDP, CF, MSC, MV, MD, and JDT provided substantive edits to the manuscript. All authors have read and approved the final manuscript.
Funding Statement
EJS is supported by Wellcome Trust and the KWTRP at the Centre for Geographical Medicine Research-Kilifi (supported by core funding from the Wellcome Trust (#203077/Z/16/Z)), with support from the International AIDS Vaccine Initiative. JDT is supported by NIAID R21AI20549. SF is supported by NIHR BRC. SER was supported by National Institutes of Health [R01 AI114320], [F30 MH098731] and [T32 GM008719].
Competing interests
MSC receives advisory board honorariums and/or travel reimbursement from Janssen Global Services, Roche Molecular Systems, and Merck Research outside the submitted manuscript. AS-C has received advisory board honorarium and/or speaker honorarium from ViiV healthcare, Gilead, Merck Sharp and Dohme and BMS and research grant from Merck Sharp and Dohme outside the submitted manuscript.
References
- [1].UNAIDS Prevention gap report. 2016. Available from: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf
- [2].Dehne KL, Dallabetta G, Wilson D, Garnett GP, Laga M, Benomar E, et al. HIV prevention 2020: a framework for delivery and a call for action. Lancet HIV. 2016;3(7):e323–13. [DOI] [PubMed] [Google Scholar]
- [3].Fiebig EW, Wright DJ, Rawal BD, Garrett PE, Schumacher RT, Peddada L, et al. Dynamics of HIV viremia and antibody seroconversion in plasma donors: implications for diagnosis and staging of primary HIV infection. Aids. 2003;17(13):1871–79. [DOI] [PubMed] [Google Scholar]
- [4].DHHS Panel on antiretroviral guidelines for adults and adolescents. Washington (DC) 2015. p. 133–39. Available from: http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf [Google Scholar]
- [5].Pilcher CD, Joaki G, Hoffman IF, Martinson FE, Mapanje C, Stewart PW, et al. Amplified transmission of HIV-1: comparison of HIV-1 concentrations in semen and blood during acute and chronic infection. Aids. 2007;21(13):1723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pilcher CD, Shugars DC, Fiscus SA, Miller WC, Menezes P, Giner J, et al. HIV in body fluids during primary HIV infection: implications for pathogenesis, treatment and public health. Aids. 2001;15(7):837–45. [DOI] [PubMed] [Google Scholar]
- [7].Pilcher CD, Tien HC, Eron JJ Jr., Vernazza PL, Leu SY, Stewart PW, et al. Brief but efficient: acute HIV infection and the sexual transmission of HIV. J Infect Dis. 2004;189(10):1785–92. [DOI] [PubMed] [Google Scholar]
- [8].Morrison CS, Demers K, Kwok C, Bulime S, Rinaldi A, Munjoma M, et al. Plasma and cervical viral loads among Ugandan and Zimbabwean women during acute and early HIV-1 infection. Aids. 2010;24(4):573–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Powers KA, Ghani AC, Miller WC, Hoffman IF, Pettifor AE, Kamanga G, et al. The role of acute and early HIV infection in the spread of HIV and implications for transmission prevention strategies in Lilongwe, Malawi: a modelling study. Lancet. 2011;378(9787):256–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Battegay M, Lundgren JD, Ryom L, editors. European AIDS clinical society Brussels, Belgium: EACS; 2017. [Google Scholar]
- [11].Panel on Antiretroviral Guidelines for Adults and Adolescents Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Washington DC, USA: Department of Health and Human Services; 2015. [Google Scholar]
- [12].Gokengin D, Geretti AM, Begovac J, Palfreeman A, Stevanovic M, Tarasenko O, et al. European guideline on HIV testing. Int J STD AIDS. 2014;25(10):695–704. [DOI] [PubMed] [Google Scholar]
- [13] IAS-USA.Antiretroviral treatment of adult HIV infection: 2014 recommendations of the international antiviral society-USA panel. San Francisco, CA: IAS-USA; 2014. [DOI] [PubMed]
- [14].WHO Consolidated guidelines on HIV prevention, diagnosis, treatment, and care for key populations. Geneva: WHO; 2013. [PubMed] [Google Scholar]
- [15].WHO Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2nd ed. Geneva: World Health Organization; 2016. September. [PubMed] [Google Scholar]
- [16].WHO Consolidated guidelines on HIV testing services. Geneva (Switzerland): WHO; 2015. July. [Google Scholar]
- [17].Fonner VA, Dalglish SL, Kennedy CE, Baggaley R, O’Reilly KR, Koechlin FM, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. Aids. 2016;30(12):1973–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Li JZ, Etemad B, Ahmed H, Aga E, Bosch RJ, Mellors JW, et al. The size of the expressed HIV reservoir predicts timing of viral rebound after treatment interruption. Aids. 2016;30(3):343–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ananworanich J, Dube K, Chomont N.. How does the timing of antiretroviral therapy initiation in acute infection affect HIV reservoirs? Curr Opin HIV AIDS. 2015;10(1):18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Archin NM, Vaidya NK, Kuruc JD, Liberty AL, Wiegand A, Kearney MF, et al. Immediate antiviral therapy appears to restrict resting CD4+ cell HIV-1 infection without accelerating the decay of latent infection. PNAS. 2012;109(24):9523–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Krebs SJ, Ananworanich J. Immune activation during acute HIV infection and the impact of early antiretroviral therapy. Curr Opin HIV AIDS. 2016;11(2):163–72. [DOI] [PubMed] [Google Scholar]
- [22].Fisher M, Pao D, Brown AE, Sudarshi D, Gill ON, Cane P, et al. Determinants of HIV-1 transmission in men who have sex with men: a combined clinical, epidemiological and phylogenetic approach. Aids. 2010;24(11):1739–47. [DOI] [PubMed] [Google Scholar]
- [23].Hoenigl M, Graff-Zivin J, Little SJ. Costs per diagnosis of acute HIV infection in community-based screening strategies: a comparative analysis of four screening algorithms. Clin Infect Dis. 2016;62(4):501–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kuruc JD, Cope AB, Sampson LA, Gay CL, Ashby RM, Foust EM, et al. Ten years of screening and testing for acute HIV infection in North Carolina. J Acquir Immune Defic Syndr. 2016;71(1):111–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].White PJ, Fox J, Weber J, Fidler S, Ward H. How many HIV infections may be averted by targeting primary infection in men who have sex with men? Quantification of changes in transmission-risk behavior, using an individual-based model. J Infect Dis. 2014;210 Suppl 2:S594–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Phanuphak P, Lo YR. Implementing early diagnosis and treatment: programmatic considerations. Curr Opin HIV AIDS. 2015;10(1):69–75. [DOI] [PubMed] [Google Scholar]
- [27].Suthar AB, Granich RM, Kato M, Nsanzimana S, Montaner JS, Williams BG. Programmatic implications of acute and early HIV infection. J Infect Dis. 2015;212(9):1351–60. [DOI] [PubMed] [Google Scholar]
- [28].Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- [29].Mays N, Roberts E, Popay J. Synthesising research evidence In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the organisation and delivery of health services: research methods. London: Routledge; 2001. p. 188–220. [Google Scholar]
- [30].Carlson JM, Schaefer M, Monaco DC, Batorsky R, Claiborne DT, Prince J, et al. HIV transmission. Selection bias at the heterosexual HIV-1 transmission bottleneck. Science. 2014;345(6193):1254031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Quinn TC, Brookmeyer R, Kline R, Shepherd M, Paranjape R, Mehendale S, et al. Feasibility of pooling sera for HIV-1 viral RNA to diagnose acute primary HIV-1 infection and estimate HIV incidence. Aids. 2000;14(17):2751–57. [DOI] [PubMed] [Google Scholar]
- [32].Robb ML, Eller LA, Kibuuka H, Rono K, Maganga L, Nitayaphan S, et al. Prospective study of acute HIV-1 infection in adults in East Africa and Thailand. N Engl J Med. 2016;374:2120–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wawer MJ, Sewankambo NK, Serwadda D, Quinn TC, Paxton LA, Kiwanuka N, et al. Control of sexually transmitted diseases for AIDS prevention in Uganda: a randomised community trial. Rakai Project Study Group. Lancet. 1999;353(9152):525–35. [DOI] [PubMed] [Google Scholar]
- [34].Wawer MJ, Gray RH, Sewankambo NK, Serwadda D, Li X, Laeyendecker O, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191(9):1403–09. [DOI] [PubMed] [Google Scholar]
- [35].Hollingsworth TD, Anderson RM, Fraser C. HIV-1 transmission, by stage of infection. J Infect Dis. 2008;198(5):687–93. [DOI] [PubMed] [Google Scholar]
- [36].Bellan SE, Dushoff J, Galvani AP, Meyers LA. Reassessment of HIV-1 acute phase infectivity: accounting for heterogeneity and study design with simulated cohorts. Plos Med. 2015;12(3):e1001801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Bezemer D, Van Sighem A, Lukashov VV, Van Der Hoek L, Back N, Schuurman R, et al. Transmission networks of HIV-1 among men having sex with men in the Netherlands. Aids. 2010;24(2):271–82. [DOI] [PubMed] [Google Scholar]
- [38].English S, Katzourakis A, Bonsall D, Flanagan P, Duda A, Fidler S, et al. Phylogenetic analysis consistent with a clinical history of sexual transmission of HIV-1 from a single donor reveals transmission of highly distinct variants. Retrovirology. 2011;8:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Hollingsworth TD, Pilcher CD, Hecht FM, Deeks SG, Fraser C. High Transmissibility During early HIV infection among men who have sex with men-San Francisco, California. J Infect Dis. 2015;211(11):1757–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kouyos RD, Von Wyl V, Yerly S, Boni J, Taffe P, Shah C, et al. Molecular epidemiology reveals long-term changes in HIV type 1 subtype B transmission in Switzerland. J Infect Dis. 2010;201(10):1488–97. [DOI] [PubMed] [Google Scholar]
- [41].Pao D, Fisher M, Hue S, Dean G, Murphy G, Cane PA, et al. Transmission of HIV-1 during primary infection: relationship to sexual risk and sexually transmitted infections. Aids. 2005;19(1):85–90. [DOI] [PubMed] [Google Scholar]
- [42].Brenner BG, Roger M, Stephens D, Moisi D, Hardy I, Weinberg J, et al. Transmission clustering drives the onward spread of the HIV epidemic among men who have sex with men in Quebec. J Infect Dis. 2011;204(7):1115–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Brown AE, Gifford RJ, Clewley JP, Kucherer C, Masquelier B, Porter K, et al. Phylogenetic reconstruction of transmission events from individuals with acute HIV infection: toward more-rigorous epidemiological definitions. J Infect Dis. 2009;199(3):427–31. [DOI] [PubMed] [Google Scholar]
- [44].Chibo D, Kaye M, Birch C. HIV transmissions during seroconversion contribute significantly to new infections in men who have sex with men in Australia. AIDS Res Hum Retroviruses. 2012;28(5):460–64. [DOI] [PubMed] [Google Scholar]
- [45].Frange P, Meyer L, Deveau C, Tran L, Goujard C, Ghosn J, et al. Recent HIV-1 infection contributes to the viral diffusion over the French territory with a recent increasing frequency. Plos One. 2012;7(2):e31695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Brenner BG, Roger M, Routy JP, Moisi D, Ntemgwa M, Matte C, et al. High rates of forward transmission events after acute/early HIV-1 infection. J Infect Dis. 2007;195(7):951–59. [DOI] [PubMed] [Google Scholar]
- [47].Ratmann O, Van Sighem A, Bezemer D, Gavryushkina A, Jurriaans S, Wensing A, et al. Sources of HIV infection among men having sex with men and implications for prevention. Sci Transl Med. 2016;8(320):320ra2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Dennis AM, Herbeck JT, Brown AL, Kellam P, De Oliveira T, Pillay D, et al. Phylogenetic studies of transmission dynamics in generalized HIV epidemics: an essential tool where the burden is greatest? J Acquir Immune Defic Syndr. 2014;67(2):181–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Miller WC, Rosenberg NE, Rutstein SE, Powers KA. Role of acute and early HIV infection in the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Pinkerton SD. How many sexually-acquired HIV infections in the USA are due to acute-phase HIV transmission? Aids. 2007;21(12):1625–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Prabhu VS, Hutchinson AB, Farnham PG, Sansom SL. Sexually acquired HIV infections in the USA due to acute-phase HIV transmission: an update. Aids. 2009;23(13):1792–94. [DOI] [PubMed] [Google Scholar]
- [52].Xiridou M, Geskus R, De Wit J, Coutinho R, Kretzschmar M. Primary HIV infection as source of HIV transmission within steady and casual partnerships among homosexual men. Aids. 2004;18(9):1311–20. [DOI] [PubMed] [Google Scholar]
- [53].Cohen MS, Shaw GM, McMichael AJ, Haynes BF. Acute HIV-1 infection. N Engl J Med. 2011;364(20):1943–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Volz EM, Ionides E, Romero-Severson EO, Brandt MG, Mokotoff E, Koopman JS. HIV-1 transmission during early infection in men who have sex with men: a phylodynamic analysis. Plos Med. 2013;10(12):e1001568;discussion e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Abu-Raddad LJ, Longini IM Jr.. No HIV stage is dominant in driving the HIV epidemic in sub-Saharan Africa. Aids. 2008;22(9):1055–61. [DOI] [PubMed] [Google Scholar]
- [56].Williams BG, Granich R, Dye C. Role of acute infection in HIV transmission. Lancet. 2011;378(9807):1913;author reply 4-5. [DOI] [PubMed] [Google Scholar]
- [57].PopART. Clinicaltrials.gov [Identifier: NCT01900977]. 2016. Available from: https://clinicaltrials.gov/ct2/show/NCT01900977
- [58].SEARCH. Clinicaltrials.gov [Identifier: NCT01864603]. 2016. Available from: https://clinicaltrials.gov/ct2/show/NCT01864603
- [59].Kfutwah A, Lemee V, Ngono HV, De Oliveira F, Njouom R, Plantier JC. Field evaluation of the Abbott ARCHITECT HIV Ag/Ab Combo immunoassay. J Clin Virol. 2013;58 Suppl 1:e70–5. [DOI] [PubMed] [Google Scholar]
- [60].Haukoos JS, Lyons MS, White DA, Hsieh YH, Rothman RE. Acute HIV infection and implications of fourth-generation HIV screening in emergency departments. Ann Emerg Med. 2014;64(5):547–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Patel P, Bennett B, Sullivan T, Parker MM, Heffelfinger JD, Sullivan PS. Rapid HIV screening: missed opportunities for HIV diagnosis and prevention. J Clin Virol. 2012;54(1):42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Piwowar-Manning E, Fogel JM, Richardson P, Wolf S, Clarke W, Marzinke MA, et al. Performance of the fourth-generation Bio-Rad GS HIV Combo Ag/Ab enzyme immunoassay for diagnosis of HIV infection in Southern Africa. J Clin Virol. 2015;62:75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Geren KI, Lovecchio F, Knight J, Fromm R, Moore E, Tomlinson C, et al. Identification of acute HIV infection using fourth-generation testing in an opt-out emergency department screening program. Ann Emerg Med. 2014;64(5):537–46. [DOI] [PubMed] [Google Scholar]
- [64].Ly TD, Ebel A, Faucher V, Fihman V, Laperche S. Could the new HIV combined p24 antigen and antibody assays replace p24 antigen specific assays? J Virol Methods. 2007;143(1):86–94. [DOI] [PubMed] [Google Scholar]
- [65].Peters PJ, Westheimer E, Cohen S, Hightow-Weidman LB, Moss N, Tsoi B, et al. Screening yield of HIV antigen/antibody combination and pooled HIV RNA testing for acute HIV infection in a high-prevalence population. Jama. 2016;315(7):682–90. [DOI] [PubMed] [Google Scholar]
- [66].Jurriaans S, Back NK, Wolthers KC. Ten years of HIV testing with fourth generation assays: the Amsterdam experience. J Clin Virol. 2011;52 Suppl 1:S67–9. [DOI] [PubMed] [Google Scholar]
- [67].Centers for Disease Control and Prevention (CDC) Laboratory testing for the diagnosis of HIV infection: updated recommendations. Atlanta (GA); 2014. June 27. [Google Scholar]
- [68].De Souza M, Phanuphak N, Pinyakorn S, Trichavaroj R, Pattanachaiwit S, Chomchey N, et al. Impact of nucleic acid testing relative to antigen/antibody combination immunoassay on the detection of acute HIV infection. Aids. 2015;29:793–800. [DOI] [PubMed] [Google Scholar]
- [69].Krajden M, Cook D, Mak A, Chu K, Chahil N, Steinberg M, et al. Pooled nucleic acid testing increases the diagnostic yield of acute HIV infections in a high-risk population compared to 3rd and 4th generation HIV enzyme immunoassays. J Clin Virol. 2014;61(1):132–37. [DOI] [PubMed] [Google Scholar]
- [70].De Souza MS, Pinyakorn S, Akapirat S, Pattanachaiwit S, Fletcher JL, Chomchey N, et al. Initiation of antiretroviral therapy during acute HIV-1 infection leads to a high rate of nonreactive HIV serology. Clin Infect Dis. 2016;63:555–61. [DOI] [PubMed] [Google Scholar]
- [71].RV254/SEARCH010. Clinicaltrials.gov [Identifier: NCT00796146]. 2016. [cited 2016 August25]. Available from: https://clinicaltrials.gov/ct2/show/NCT00796146
- [72].Ramos EM, Harb S, Dragavon J, Swenson P, Stekler JD, Coombs RW. Performance of an alternative HIV diagnostic algorithm using the ARCHITECT HIV Ag/Ab Combo assay and potential utility of sample-to-cutoff ratio to discriminate primary from established infection. J Clin Virol. 2013;58 Suppl 1:e38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. [DOI] [PubMed] [Google Scholar]
- [74].Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Bassett IV, Chetty S, Giddy J, Reddy S, Bishop K, Lu Z, et al. Screening for acute HIV infection in South Africa: finding acute and chronic disease. HIV Med. 2011;12(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Bebell LM, Pilcher CD, Dorsey G, Havlir D, Kamya MR, Busch MP, et al. Acute HIV-1 infection is highly prevalent in Ugandan adults with suspected malaria. Aids. 2010;24(12):1945–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Fiscus SA, Pilcher CD, Miller WC, Powers KA, Hoffman IF, Price M, et al. Rapid, real-time detection of acute HIV infection in patients in Africa. J Infect Dis. 2007;195(3):416–24. [DOI] [PubMed] [Google Scholar]
- [80].Gous N, Scott L, Perovic O, Venter F, Stevens W. Should South Africa be performing nucleic acid testing on HIV enzyme-linked immunosorbent assay-negative samples? J Clin Microbiol. 2010;48(9):3407–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Li J, Zhang H, Shen Z, Zhou Y, Fang N, Wang L, et al. Screening for acute HIV infections and estimating HIV incidence among female sex workers from low-grade venues in Guangxi, China. PLoS One. 2014;9(6):e99522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Mlisana K, Sobieszczyk M, Werner L, Feinstein A, Van Loggerenberg F, Naicker N, et al. Challenges of diagnosing acute HIV-1 subtype C infection in African women: performance of a clinical algorithm and the need for point-of-care nucleic-acid based testing. PLoS One. 2013;8(4):e62928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Pilcher CD, Price MA, Hoffman IF, Galvin S, Martinson FE, Kazembe PN, et al. Frequent detection of acute primary HIV infection in men in Malawi. Aids. 2004;18(3):517–24. [DOI] [PubMed] [Google Scholar]
- [84].Rutstein SE, Pettifor AE, Phiri S, Kamanga G, Hoffman IF, Hosseinipour MC, et al. Incorporating acute HIV screening into routine HIV testing at sexually transmitted infection clinics, and HIV testing and counseling centers in Lilongwe, Malawi. J Acquir Immune Defic Syndr. 2016;71(3):272–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Serna-Bolea C, Munoz J, Almeida JM, Nhacolo A, Letang E, Nhampossa T, et al. High prevalence of symptomatic acute HIV infection in an outpatient ward in southern Mozambique: identification and follow-up. Aids. 2010;24(4):603–08. [DOI] [PubMed] [Google Scholar]
- [86].Cragin L, Pan F, Peng S, Zenilman JM, Green J, Doucet C, et al. Cost-effectiveness of a fourth-generation combination immunoassay for human immunodeficiency virus (HIV) antibody and p24 antigen for the detection of HIV infections in the USA. HIV Clin Trials. 2012;13(1):11–22. [DOI] [PubMed] [Google Scholar]
- [87].Juusola JL, Brandeau ML, Long EF, Owens DK, Bendavid E. The cost-effectiveness of symptom-based testing and routine screening for acute HIV infection in men who have sex with men in the USA. Aids. 2011;25(14):1779–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Karris MY, Anderson CM, Morris SR, Smith DM, Little SJ. Cost savings associated with testing of antibodies, antigens, and nucleic acids for diagnosis of acute HIV infection. J Clin Microbiol. 2012;50(6):1874–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Hoenigl M, Chaillon A, Mehta SR, Smith DM, Graff-Zivin J, Little SJ. Screening for acute HIV infection in community-based settings: cost-effectiveness and impact on transmissions. J Infect. 2016;73:476–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Pilcher CD, Fiscus SA, Nguyen TQ, Foust E, Wolf L, Williams D, et al. Detection of acute infections during HIV testing in North Carolina. N Engl J Med. 2005;352(18):1873–83. [DOI] [PubMed] [Google Scholar]
- [91].Klausner JD, Grant RM, Kent CK. Detection of acute HIV infections. N Engl J Med. 2005;353(6):631–33;author reply −3. [DOI] [PubMed] [Google Scholar]
- [92].Hutchinson AB, Patel P, Sansom SL, Farnham PG, Sullivan TJ, Bennett B, et al. Cost-effectiveness of pooled nucleic acid amplification testing for acute HIV infection after third-generation HIV antibody screening and rapid testing in the USA: a comparison of three public health settings. Plos Med. 2010;7(9):e1000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Emerson B, Plough K. Detection of acute HIV-1 infections utilizing NAAT technology in Dallas, Texas. J Clin Virol. 2013;58 Suppl 1:e48–53. [DOI] [PubMed] [Google Scholar]
- [94].WHO WHO Prequalification of In Vitro Diagnostics: PUBLIC REPORT (Alere™ HIV Combo). Geneva: WHO; 2016. Available from: http://www.who.int/diagnostics_laboratory/evaluations/pq-list/hiv-rdts/160712_final_public_report_0243_013_00_v3.pdf [Google Scholar]
- [95].Smallwood M, Vijh R, Nauche B, Lebouche B, Joseph L, Pant Pai N. Evaluation of a rapid point of care test for detecting acute and established HIV infection, and examining the role of study quality on diagnostic accuracy: a bayesian meta-analysis. Plos One. 2016;11(2):e0149592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Conway DP, Holt M, McNulty A, Couldwell DL, Smith DE, Davies SC, et al. Multi-centre evaluation of the determine HIV combo assay when used for point of care testing in a high risk clinic-based population. Plos One. 2014;9(4):e94062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Duong YT, Mavengere Y, Patel H, Moore C, Manjengwa J, Sibandze D, et al. Poor performance of the determine HIV-1/2 Ag/Ab combo fourth-generation rapid test for detection of acute infections in a national household survey in Swaziland. J Clin Microbiol. 2014;52(10):3743–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Rosenberg NE, Kamanga G, Phiri S, Nsona D, Pettifor A, Rutstein SE, et al. Detection of acute HIV infection: a field evaluation of the determine(R) HIV-1/2 Ag/Ab combo test. J Infect Dis. 2012;205(4):528–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Jones CB, Kuldanek K, Muir D, Phekoo K, Black A, Sacks R, et al. Clinical evaluation of the Determine HIV-1/2 Ag/Ab Combo test. J Infect Dis. 2012;206(12):1947–49;author reply 9-50. [DOI] [PubMed] [Google Scholar]
- [100].Lewis JM, Macpherson P, Adams ER, Ochodo E, Sands A, Taegtmeyer M. Field accuracy of fourth-generation rapid diagnostic tests for acute HIV-1: a systematic review. Aids. 2015;29(18):2465–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Fitzgerald N, Cross M, O’Shea S, Fox J. Diagnosing acute HIV infection at point of care: a retrospective analysis of the sensitivity and specificity of a fourth-generation point-of-care test for detection of HIV core protein p24. Sex Transm Infect. 2017;93(2):100–1. [DOI] [PubMed] [Google Scholar]
- [102].Keating SM, Kassanjee R, Lebedeva M, Facente SN, MacArthur JC, Grebe E, et al. Performance of the bio-rad geenius HIV1/2 supplemental assay in detecting ‘recent’ HIV infection and calculating population incidence. J Acquir Immune Defic Syndr. 2016;73:581–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Jani IV, Meggi B, Mabunda N, Vubil A, Sitoe NE, Tobaiwa O, et al. Accurate early infant HIV diagnosis in primary health clinics using a point-of-care nucleic acid test. J Acquir Immune Defic Syndr. 2014;67(1):e1–4. [DOI] [PubMed] [Google Scholar]
- [104].WHO WHO Prequalification of in vitro diagnostics: PUBLIC REPORT (Alere™ q HIV-1/2 Detect). Geneva: WHO; 2016. [Google Scholar]
- [105].Ritchie AV, Ushiro-Lumb I, Edemaga D, Joshi HA, De Ruiter A, Szumilin E, et al. SAMBA HIV semiquantitative test, a new point-of-care viral-load-monitoring assay for resource-limited settings. J Clin Microbiol. 2014;52(9):3377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Scott L, Gous N, Carmona S, Stevens W. Laboratory evaluation of the liat HIV quant (IQuum) whole blood and plasma HIV-1 viral load assays for point-of-care testing in South Africa. J Clin Microbiol. 2015;53:1616–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Garrett NJ, Drain PK, Werner L, Samsunder N, Abdool Karim SS. Diagnostic accuracy of the point-of-care xpert HIV-1 viral load assay in a South African HIV clinic. J Acquir Immune Defic Syndr. 2016;72(2):e45–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Michaeli M, Wax M, Gozlan Y, Rakovsky A, Mendelson E, Mor O. Evaluation of xpert HIV-1 qual assay for resolution of HIV-1 infection in samples with negative or indeterminate geenius HIV-1/2 results. J Clin Virol. 2016;76:1–3. [DOI] [PubMed] [Google Scholar]
- [109].Hoenigl M, Green N, Camacho M, Gianella S, Mehta SR, Smith DM, et al. Signs or symptoms of acute HIV infection in a cohort undergoing community-based screening. Emerg Infect Dis. 2016;22(3):532–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Sanders EJ, Wahome E, Mwangome M, Thiong’o AN, Okuku HS, Price MA, et al. Most adults seek urgent healthcare when acquiring HIV-1 and are frequently treated for malaria in coastal Kenya. Aids. 2011;25(9):1219–24. [DOI] [PubMed] [Google Scholar]
- [111].Sudarshi D, Pao D, Murphy G, Parry J, Dean G, Fisher M. Missed opportunities for diagnosing primary HIV infection. Sex Transm Infect. 2008;84(1):14–16. [DOI] [PubMed] [Google Scholar]
- [112].Powers KA, Cohen MS. Acute HIV-1 infection in sub-Saharan Africa: a common occurrence overlooked. Aids. 2014;28(9):1365–67. [DOI] [PubMed] [Google Scholar]
- [113].Prins HA, Mugo P, Wahome E, Mwashigadi G, Thiong’o A, Smith A, et al. Diagnosing acute and prevalent HIV-1 infection in young African adults seeking care for fever: a systematic review and audit of current practice. Int Health. 2014;6(2):82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Sanders EJ, Mugo P, Prins HA, Wahome E, Thiong’o AN, Mwashigadi G, et al. Acute HIV-1 infection is as common as malaria in young febrile adults seeking care in coastal Kenya. Aids. 2014;28(9):1357–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Lindback S, Karlsson AC, Mittler J, Blaxhult A, Carlsson M, Briheim G, et al. Viral dynamics in primary HIV-1 infection. Karolinska Institutet Primary HIV Infection Study Group. Aids. 2000;14(15):2283–91. [DOI] [PubMed] [Google Scholar]
- [116].Lavreys L, Baeten JM, Overbaugh J, Panteleeff DD, Chohan BH, Richardson BA, et al. Virus load during primary human immunodeficiency virus (HIV) type 1 infection is related to the severity of acute HIV illness in Kenyan women. Clin Infect Dis. 2002;35(1):77–81. [DOI] [PubMed] [Google Scholar]
- [117].Sanders EJ, Chirro O, Oduor C, Mangi J, Wahome E, Price M, et al. Outcomes of AHI screening and immediate ART initiation in Coastal Kenya. Seattle, Washington, USA: CROI; 2017. [Google Scholar]
- [118].Lavreys L, Baeten JM, Chohan V, McClelland RS, Hassan WM, Richardson BA, et al. Higher set point plasma viral load and more-severe acute HIV type 1 (HIV-1) illness predict mortality among high-risk HIV-1-infected African women. Clin Infect Dis. 2006;42(9):1333–39. [DOI] [PubMed] [Google Scholar]
- [119].Sanders EJ, Wahome E, Powers KA, Werner L, Fegan G, Lavreys L, et al. Targeted screening of at-risk adults for acute HIV-1 infection in sub-Saharan Africa. Aids. 2015;29 Suppl 3:S221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Powers KA, Miller WC, Pilcher CD, Mapanje C, Martinson FE, Fiscus SA, et al. Improved detection of acute HIV-1 infection in sub-Saharan Africa: development of a risk score algorithm. Aids. 2007;21(16):2237–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Wahome E, Fegan G, Okuku HS, Mugo P, Price MA, Mwashigadi G, et al. Evaluation of an empiric risk screening score to identify acute and early HIV-1 infection among MSM in Coastal Kenya. Aids. 2013;27(13):2163–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Grijsen ML, Steingrover R, Wit FW, Jurriaans S, Verbon A, Brinkman K, et al. No treatment versus 24 or 60 weeks of antiretroviral treatment during primary HIV infection: the randomized Primo-SHM trial. PLoS Med. 2012;9(3):e1001196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Saez-Cirion A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, Girault I, Lecuroux C, et al. Post-treatment HIV-1 controllers with a long-term virological remission after the interruption of early initiated antiretroviral therapy ANRS VISCONTI Study. PLoS Pathog. 2013;9(3):e1003211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Fidler S, Porter K, Ewings F, Frater J, Ramjee G, Cooper D, et al. Short-course antiretroviral therapy in primary HIV infection. N Engl J Med. 2013;368(3):207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].McMichael AJ, Borrow P, Tomaras GD, Goonetilleke N, Haynes BF. The immune response during acute HIV-1 infection: clues for vaccine development. Nat Rev Immunol. 2010;10(1):11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Buzon MJ, Martin-Gayo E, Pereyra F, Ouyang Z, Sun H, Li JZ, et al. Long-term antiretroviral treatment initiated at primary HIV-1 infection affects the size, composition, and decay kinetics of the reservoir of HIV-1-infected CD4 T cells. J Virol. 2014;88(17):10056–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Cheret A, Bacchus-Souffan C, Avettand-Fenoel V, Melard A, Nembot G, Blanc C, et al. Combined ART started during acute HIV infection protects central memory CD4+ T cells and can induce remission. J Antimicrob Chemother. 2015;70(7):2108–20. [DOI] [PubMed] [Google Scholar]
- [128].Strain MC, Little SJ, Daar ES, Havlir DV, Gunthard HF, Lam RY, et al. Effect of treatment, during primary infection, on establishment and clearance of cellular reservoirs of HIV-1. J Infect Dis. 2005;191(9):1410–18. [DOI] [PubMed] [Google Scholar]
- [129].Ananworanich J, Schuetz A, Vandergeeten C, Sereti I, De Souza M, Rerknimitr R, et al. Impact of multi-targeted antiretroviral treatment on gut T cell depletion and HIV reservoir seeding during acute HIV infection. PLoS One. 2012;7(3):e33948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Laanani M, Ghosn J, Essat A, Melard A, Seng R, Gousset M, et al. Impact of the timing of initiation of antiretroviral therapy during primary HIV-1 infection on the decay of cell-associated HIV-DNA. Clin Infect Dis. 2015;60(11):1715–21. [DOI] [PubMed] [Google Scholar]
- [131].Bruner KM, Murray AJ, Pollack RA, Soliman MG, Laskey SB, Capoferri AA, et al. Defective proviruses rapidly accumulate during acute HIV-1 infection. Nat Med. 2016;22:1043–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Allers K, Puyskens A, Epple HJ, Schurmann D, Hofmann J, Moos V, et al. The effect of timing of antiretroviral therapy on CD4(+) T-cell reconstitution in the intestine of HIV-infected patients. Mucosal Immunol. 2016;9(1):265–74. [DOI] [PubMed] [Google Scholar]
- [133].Jenabian MA, El-Far M, Vyboh K, Kema I, Costiniuk CT, Thomas R, et al. Immunosuppressive tryptophan catabolism and gut mucosal dysfunction following early HIV infection. J Infect Dis. 2015;212(3):355–66. [DOI] [PubMed] [Google Scholar]
- [134].Ananworanich J, Chomont N, Eller LA, Kroon E, Tovanabutra S, Bose M, et al. HIV DNA set point is rapidly established in acute HIV infection and dramatically reduced by early ART. EBioMedicine. 2016;11:68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Besson GJ, Lalama CM, Bosch RJ, Gandhi RT, Bedison MA, Aga E, et al. HIV-1 DNA decay dynamics in blood during more than a decade of suppressive antiretroviral therapy. Clin Infect Dis. 2014;59(9):1312–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Murray JM, Zaunders JJ, McBride KL, Xu Y, Bailey M, Suzuki K, et al. HIV DNA subspecies persist in both activated and resting memory CD4+ T cells during antiretroviral therapy. J Virol. 2014;88(6):3516–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Rothenberger MK, Keele BF, Wietgrefe SW, Fletcher CV, Beilman GJ, Chipman JG, et al. Large number of rebounding/founder HIV variants emerge from multifocal infection in lymphatic tissues after treatment interruption. Proc Natl Acad Sci U S A. 2015;112(10):E1126–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Jain V, Hartogensis W, Bacchetti P, Hunt PW, Hatano H, Sinclair E, et al. Antiretroviral therapy initiated within 6 months of HIV infection is associated with lower T-cell activation and smaller HIV reservoir size. J Infect Dis. 2013;208(8):1202–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Le T, Wright EJ, Smith DM, He W, Catano G, Okulicz JF, et al. Enhanced CD4+ T-cell recovery with earlier HIV-1 antiretroviral therapy. N Engl J Med. 2013;368(3):218–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Schuetz A, Deleage C, Sereti I, Rerknimitr R, Phanuphak N, Phuang-Ngern Y, et al. Initiation of ART during early acute HIV infection preserves mucosal Th17 function and reverses HIV-related immune activation. PLoS Pathog. 2014;10(12):e1004543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Herout S, Mandorfer M, Breitenecker F, Reiberger T, Grabmeier-Pfistershammer K, Rieger A, et al. Impact of early initiation of antiretroviral therapy in patients with acute HIV infection in Vienna, Austria. PLoS One. 2016;11(4):e0152910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142].Buggert M, Frederiksen J, Noyan K, Svard J, Barqasho B, Sonnerborg A, et al. Multiparametric bioinformatics distinguish the CD4/CD8 ratio as a suitable laboratory predictor of combined T cell pathogenesis in HIV infection. J Immunol. 2014;192(5):2099–108. [DOI] [PubMed] [Google Scholar]
- [143].Young J, Psichogiou M, Meyer L, Ayayi S, Grabar S, Raffi F, et al. CD4 cell count and the risk of AIDS or death in HIV-infected adults on combination antiretroviral therapy with a suppressed viral load: a longitudinal cohort study from COHERE. PLoS Med. 2012;9(3):e1001194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Mussini C, Lorenzini P, Cozzi-Lepri A, Lapadula G, Marchetti G, Nicastri E, et al. CD4/CD8 ratio normalisation and non-AIDS-related events in individuals with HIV who achieve viral load suppression with antiretroviral therapy: an observational cohort study. Lancet HIV. 2015;2(3):e98–106. [DOI] [PubMed] [Google Scholar]
- [145].Cao W, Mehraj V, Trottier B, Baril JG, Leblanc R, Lebouche B, et al. Early initiation rather than prolonged duration of antiretroviral therapy in HIV infection contributes to the normalization of CD8 T-cell counts. Clin Infect Dis. 2016;62(2):250–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Thornhill J, Inshaw J, Oomeer S, Kaleebu P, Cooper D, Ramjee G, et al. Enhanced normalisation of CD4/CD8 ratio with early antiretroviral therapy in primary HIV infection. J Int AIDS Soc. 2014;17 Suppl 3(4):19480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Hocqueloux L, Avettand-Fenoel V, Jacquot S, Prazuck T, Legac E, Melard A, et al. Long-term antiretroviral therapy initiated during primary HIV-1 infection is key to achieving both low HIV reservoirs and normal T cell counts. J Antimicrob Chemother. 2013;68(5):1169–78. [DOI] [PubMed] [Google Scholar]
- [148].Ananworanich J, Sacdalan CP, Pinyakorn S, Chomont N, De Souza M, Luekasemsuk T, et al. Virological and immunological characteristics of HIV-infected individuals at the earliest stage of infection. J Virus Erad. 2016;2:43–48. [PMC free article] [PubMed] [Google Scholar]
- [149].Hoenigl M, Chaillon A, Little SJ. CD4/CD8 cell ratio in acute HIV infection and the impact of early antiretroviral therapy. Clin Infect Dis. 2016;63:425–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Cheret A, Nembot G, Melard A, Lascoux C, Slama L, Miailhes P, et al. Intensive five-drug antiretroviral therapy regimen versus standard triple-drug therapy during primary HIV-1 infection (OPTIPRIM-ANRS 147): a randomised, open-label, phase 3 trial. Lancet Infect Dis. 2015;15(4):387–96. [DOI] [PubMed] [Google Scholar]
- [151].Markowitz M, Evering TH, Garmon D, Caskey M, La Mar M, Rodriguez K, et al. A randomized open-label study of 3- versus 5-drug combination antiretroviral therapy in newly HIV-1-infected individuals. J Acquir Immune Defic Syndr. 2014;66(2):140–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Bottani GM, Oreni ML, Orofino G, Tau P, Di Nardo Stuppino S, Colella E, et al. Treatment outcome in HIV+ patients receiving 3- or 4-drug regimens during PHI. J Int AIDS Soc. 2014;17 Suppl 3(4):19778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Ananworanich J, Chomont N, Fletcher JL, Pinyakorn S, Schuetz A, Sereti I, et al. Markers of HIV reservoir size and immune activation after treatment in acute HIV infection with and without raltegravir and maraviroc intensification. J Virus Erad. 2015;1(2):116–22. [PMC free article] [PubMed] [Google Scholar]
- [154].Phanuphak N, Teeratakulpisarn N, Van Griensven F, Chomchey N, Pinyakorn S, Fletcher JL, et al. Anogenital HIV RNA in Thai men who have sex with men in Bangkok during acute HIV infection and after randomization to standard vs. intensified antiretroviral regimens. J Int AIDS Soc. 2015;18:19470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Stellbrink HJ, Reynes J, Lazzarin A, Voronin E, Pulido F, Felizarta F, et al. Dolutegravir in antiretroviral-naive adults with HIV-1: 96-week results from a randomized dose-ranging study. Aids. 2013;27(11):1771–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Molina JM, Clotet B, Van Lunzen J, Lazzarin A, Cavassini M, Henry K, et al. Once-daily dolutegravir versus darunavir plus ritonavir for treatment-naive adults with HIV-1 infection (FLAMINGO): 96 week results from a randomised, open-label, phase 3b study. Lancet HIV. 2015;2(4):e127–36. [DOI] [PubMed] [Google Scholar]
- [157].Patel P, Klausner JD, Bacon OM, Liska S, Taylor M, Gonzalez A, et al. Detection of acute HIV infections in high-risk patients in California. J Acquir Immune Defic Syndr. 2006;42(1):75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Patel P, Mackellar D, Simmons P, Uniyal A, Gallagher K, Bennett B, et al. Detecting acute human immunodeficiency virus infection using 3 different screening immunoassays and nucleic acid amplification testing for human immunodeficiency virus RNA, 2006-2008. Arch Intern Med. 2010;170(1):66–74. [DOI] [PubMed] [Google Scholar]
- [159].Priddy FH, Pilcher CD, Moore RH, Tambe P, Park MN, Fiscus SA, et al. Detection of acute HIV infections in an urban HIV counseling and testing population in the USA. J Acquir Immune Defic Syndr. 2007;44(2):196–202. [DOI] [PubMed] [Google Scholar]
- [160].Stekler J, Swenson PD, Wood RW, Handsfield HH, Golden MR. Targeted screening for primary HIV infection through pooled HIV-RNA testing in men who have sex with men. Aids. 2005;19(12):1323–25. [DOI] [PubMed] [Google Scholar]
- [161].Stevens W, Akkers E, Myers M, Motloung T, Pilcher CD, Venter F, editors. High prevalence of undetected, acute HIV infection in a South African primary care clinic. Abstract presented at: Third IAS Conference on HIV Pathogenesis and Treatment; 2005; Rio de Janeiro, Brazil. [Google Scholar]
- [162].Gaolathe T, Wirth KE, Holme MP, Makhema J, Moyo S, Chakalisa U, et al. Botswana’s progress toward achieving the 2020 UNAIDS 90-90-90 antiretroviral therapy and virological suppression goals: a population-based survey. Lancet HIV. 2016;3(5):e221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].UNAIDS UNAIDS fact sheet 2016. Geneva, Switzerland: UNAIDS; 2016. [Google Scholar]
- [164].Collaborators GH, Wang H, Wolock TM, Carter A, Nguyen G, Kyu HH, et al. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980-2015: the Global Burden of Disease Study 2015. Lancet HIV. 2016;3(8):e361–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Liegler T, Abdel-Mohsen M, Bentley LG, Atchison R, Schmidt T, Javier J, et al. HIV-1 drug resistance in the iPrEx preexposure prophylaxis trial. J Infect Dis. 2014;210(8):1217–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [166].Weis JF, Baeten JM, McCoy CO, Warth C, Donnell D, Thomas KK, et al. Preexposure prophylaxis-selected drug resistance decays rapidly after drug cessation. Aids. 2016;30(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Brown LB, Miller WC, Kamanga G, Nyirenda N, Mmodzi P, Pettifor A, et al. HIV partner notification is effective and feasible in sub-Saharan Africa: opportunities for HIV treatment and prevention. J Acquir Immune Defic Syndr. 2011;56(5):437–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Henley C, Forgwei G, Welty T, Golden M, Adimora A, Shields R, et al. Scale-up and case-finding effectiveness of an HIV partner services program in Cameroon: an innovative HIV prevention intervention for developing countries. Sex Transm Dis. 2013;40(12):909–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [169].Se R, Lb B, Ak B, Sb W, Kamanga G, Mmodzi P, et al. Cost-effectiveness of provider-based HIV partner notification in urban Malawi. Health Policy Plan. 2014;29(1):115–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Wamuti BM, Erdman LK, Cherutich P, Golden M, Dunbar M, Bukusi D, et al. Assisted partner notification services to augment HIV testing and linkage to care in Kenya: study protocol for a cluster randomized trial. Implement Sci. 2015;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Cherutich P, Golden M, Wamuti BM, Richardson B, Ásbjörnsdóttir KH, Otieno FA, et al. Effectiveness of partner services for HIV in Kenya: a cluster randomized trial. Abstract presented at: CROI; 2016. February 22-25; Boston, Massachusetts, USA. [Google Scholar]
- [172].Rosenberg NE, Mtande TK, Saidi F, Stanley C, Jere E, Paile L, et al. Recruiting male partners for couple HIV testing and counselling in Malawi’s option B+ programme: an unblinded randomised controlled trial. Lancet HIV. 2015;2(11):e483–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Moore ZS, McCoy S, Kuruc J, Hilton M, Leone P. Number of named partners and number of partners newly diagnosed with HIV infection identified by persons with acute versus established HIV infection. J Acquir Immune Defic Syndr. 2009;52(4):509–13. [DOI] [PubMed] [Google Scholar]
- [174].Joseph Davey DL, Beymer MR, Roberts C, Bolan RK, Klausner JD. Sexual behavior during acute HIV infection among men who have sex with men, in Los Angeles, California. J Infect Dis. 2016;213(12):2020–21. [DOI] [PubMed] [Google Scholar]
- [175].Brenner BG, Wainberg MA. Future of phylogeny in HIV prevention. J Acquir Immune Defic Syndr. 2013;63 Suppl 2:S248–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [176].Cope AB, Powers KA, Kuruc JD, Leone PA, Anderson JA, Ping LH, et al. Ongoing HIV transmission and the HIV care continuum in North Carolina. Plos One. 2015;10(6):e0127950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [177].Corneli A, Pettifor A, Kamanga G, Golin C, McKenna K, Ou SS, et al. HPTN 062: a feasibility and acceptability pilot intervention to reduce HIV transmission risk behaviors among individuals with acute and early HIV infection in Lilongwe, Malawi. AIDS Behav. 2014;18(9):1785–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Pettifor A, Corneli A, Kamanga G, McKenna K, Rosenberg NE, Yu X, et al. HPTN 062: a pilot randomized controlled trial exploring the effect of a motivational-interviewing intervention on sexual behavior among individuals with acute HIV infection in Lilongwe, Malawi. Plos One. 2015;10(5):e0124452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [179].Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Van Lunzen J, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. Jama. 2016;316(2):171–81. [DOI] [PubMed] [Google Scholar]
- [180].Hino S, Grodensky C, Hamela G, Massa C, Golin C, Rutstein SE, et al. Influence of suspected source of infection on disclosure among people with acute HIV in Malawi. Abstract presented at: IAS 2015; 2015. July 19-22; Vancouver, Canada. [Google Scholar]
- [181].Steward WT, Remien RH, Higgins JA, Dubrow R, Pinkerton SD, Sikkema KJ, et al. Behavior change following diagnosis with acute/early HIV infection-a move to serosorting with other HIV-infected individuals. The NIMH multisite acute HIV infection study: III. AIDS Behav. 2009;13(6):1054–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [182].Atkinson JH, Higgins JA, Vigil O, Dubrow R, Remien RH, Steward WT, et al. Psychiatric context of acute/early HIV infection. The NIMH multisite acute HIV infection study: IV. AIDS Behav. 2009;13(6):1061–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Zetola NM, Pilcher CD. Diagnosis and management of acute HIV infection. Infect Dis Clin North Am. 2007;21(1):19–48, vii. [DOI] [PubMed] [Google Scholar]
- [184].Kelly JA, Morin SF, Remien RH, Steward WT, Higgins JA, Seal DW, et al. Lessons learned about behavioral science and acute/early HIV infection. The NIMH MULTISITE ACUTE HIV infection study: V. AIDS Behav. 2009;13(6):1068–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Pettifor A, MacPhail C, Corneli A, Sibeko J, Kamanga G, Rosenberg N, et al. Continued high risk sexual behavior following diagnosis with acute HIV infection in South Africa and Malawi: implications for prevention. AIDS Behav. 2011;15(6):1243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Cope AB, Crooks AM, Chin T, Kuruc JD, McGee KS, Eron JJ, et al. Incident sexually transmitted infection as a biomarker for high-risk sexual behavior after diagnosis of acute HIV. Sex Transm Dis. 2014;41(7):447–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].Rutstein SE, Pettifor A, Phiri S, Pasquale D, Dennis AM, Hosseinipour MC, et al, editors. Abstract presented at: Pilot study of immediate antiretrovirals and behavioral intervention for persons with acute HIV infection: opportunity for interrupting transmission. ISSTDR; 2015; Brisbane, Australia. [Google Scholar]
- [188].Pilcher CD, Ospina-Norvell C, Dasgupta A, Jones D, Hartogensis W, Torres S, et al. The effect of same-day observed initiation of antiretroviral therapy on HIV viral load and treatment outcomes in a U.S. public health setting. J Acquir Immune Defic Syndr. 2017;74(1):44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].Crowell TA, Phanuphak N, Pinyakorn S, Kroon E, Fletcher JL, Colby D, et al. Virologic failure is uncommon after treatment initiation during acute HIV infection. Aids. 2016;30:1943–50. [DOI] [PubMed] [Google Scholar]
- [190].Kassutto S, Maghsoudi K, Johnston MN, Robbins GK, Burgett NC, Sax PE, et al. Longitudinal analysis of clinical markers following antiretroviral therapy initiated during acute or early HIV type 1 infection. Clin Infect Dis. 2006;42(7):1024–31. [DOI] [PubMed] [Google Scholar]
- [191].Routy JP, Cao W, Mehraj V. Overcoming the challenge of diagnosis of early HIV infection: a stepping stone to optimal patient management. Expert Rev Anti Infect Ther. 2015;13(10):1189–93. [DOI] [PubMed] [Google Scholar]
- [192].Mugo PM, Wahome EW, Gichuru EN, Mwashigadi GM, Thiong’o AN, Prins HA, et al. Effect of text message, phone call, and in-person appointment reminders on uptake of repeat HIV testing among outpatients screened for acute HIV infection in Kenya: a randomized controlled trial. PLoS One. 2016;11(4):e0153612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].Cohen MS, Dye C, Fraser C, Miller WC, Powers KA, Williams BG. HIV treatment as prevention: debate and commentary–will early infection compromise treatment-as-prevention strategies? PLoS Med. 2012;9(7):e1001232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194].Robb ML, Ananworanich J. Lessons from acute HIV infection. Curr Opin HIV AIDS. 2016;11:555–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Saez-Cirion A, Pancino G, Definition LO, History N. Heterogeneity of HIV controllers In: Pancino G, Silvestri G, Fowke KR, editors. Models of protection against HIV/SIV. London: Elsevier; 2012. p. 233–52. [Google Scholar]
- [196].Okulicz JF, Lambotte O. Epidemiology and clinical characteristics of elite controllers. Curr Opin HIV AIDS. 2011;6(3):163–68. [DOI] [PubMed] [Google Scholar]
- [197].Karn J. Estrogen blocks HIV re-emergence from latency and points to gender-specific differences in HIV reservoirs. Abstract presented at: IAS; 2015; Vancouver, BC. [Google Scholar]
- [198].Stohr W, Fidler S, McClure M, Weber J, Cooper D, Ramjee G, et al. Duration of HIV-1 viral suppression on cessation of antiretroviral therapy in primary infection correlates with time on therapy. PLoS One. 2013;8(10):e78287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [199].Scully E, Gandhi M, Johnston R, Gorelick R, Lifson JD, Lewin SR, et al. Sex-based differences in HIV reservoir activity and residual immune activation. Abstract presented at: CROI; 2017. February 13-16; Seattle, WA. [Google Scholar]


