Abstract
AIM
To evaluate the impact of spherical and aspherical intraocular lenses on the postoperative visual quality of age-related cataract patients using Optical Quality Analysis System (OQAS).
METHODS
Seventy-four eyes with age-related cataracts were randomly divided into spherical and aspherical lens implantation groups. Best-corrected visual acuity (BCVA) was measured preoperatively, one day, one week, two weeks, one month and two months after surgery. A biometric systems analysis using the OQAS objective scattering index (OSI) was performed.
RESULTS
There were no significant differences in visual acuity (P>0.05) before and after spherical and aspheric lens implantation. There was a negative linear correction between the OSI value and BCVA (r=-0.634, P=0.000), and positive corrections between the OSI value and the lens LOCUS III value of nucleus color (NC), nucleus opacity (NO), cortex (C) and posterior lens capsular (P) (r=0.704, P=0.000; r=0.514, P=0.000; r=0.276, P=0.020; r=0.417, P=0.000, respectively). OSI values of spherical vs aspherical lenses were 11.5±3.6 vs 11.8±3.4, 4.1±0.9 vs 3.3±0.8, 3.5±0.9 vs 2.7±0.7, 3.3±0.8 vs 2.6±0.7, 3.2±0.7 vs 2.5±0.8, and 3.2±0.8 vs 2.5±0.8 before and 1d, 1, 2wk, 1 and 2mo after surgery, respectively. All time points varied significantly (P<0.01) between the two groups.
CONCLUSION
Aspherical IOLs does not significantly affect visual acuity compared with spherical IOLs. The OSI value, was significantly lower in the aspherical lens group compared with the spherical lens. This study shows that objective visual quality of aspheric IOLs is better than that of the spherical lens by means of OQAS biological measurement method.
Keywords: optical quality analysis system, age-related cataract, spherical lens, aspherical lens, objective scattering index
INTRODUCTION
Cataract surgery using phacoemulsification and implantation of an intraocular lens (IOL) is a safe and effective operative intervention[1]. The goal of cataract surgery is not only to restore visual acuity but also to provide the best possible quality of vision. Aspherical IOLs were created to compensate for the spherical aberration of the cornea and to lessen total ocular spherical aberration by IOL implantation[2]–[4]. Several studies have compared aspheric with spherical IOLs during the past decades[5]–[11]. So far, the postoperative visual evaluation has been determined only on the basis of visual acuity, contrast sensitivity, or higher order aberrations. There are some controversial viewpoints about the optical quality of aspheric and spherical IOLs[8]–[11]. With the instructions available today, it is possible to study more precisely the optical quality difference between these two kinds of IOLs.
The Optical Quality Analysis System (OQAS) is a double-pass based instrument that clinically measures objective optical quality[12]–[18]. This system performs the measurements by analyzing the retinal image of a point source of light obtained after the focalization of a beam. It has been shown that the OQAS system provided repeatable and accurate measurements of the optical quality of the eye[12]–[18].
The aim of our study is to compare the optical quality of aspheric and spherical lens implantation using OQAS measurement. This study is the first time to compare the visual quality of aspheric and spherical lens implantation using OQAS.
SUBJECTS AND METHODS
Subjects
Thirty-eight consecutive Chinese patients (74 eyes) with age-related cataracts were enrolled from the Department of Ophthalmology, Sixth Peoples' Hospital Affiliated of Shanghai Jiaotong University. This study was approved by the Ethics Committee of the Sixth Peoples' Hospital Affiliated of Shanghai Jiaotong University, Shanghai, China. Written informed consent was obtained from all patients. The patients were randomly divided into two groups using a random number table. The patients underwent phacoemulsification and implantation of posterior chamber intraocular spherical IOLs (AR40) for 37 eyes and aspherical IOLs (ZA9003) for the other 37 eyes, respectively. The mean age of the patients was 69.3±8.2y (range 50-85y). Inclusion criteria were normal eye pressure, transparent central cornea, normal fundus examination, and at least 1600 endothelial cells per mm2 in the central cornea. Patients with a cataract other than a nuclear or corticonuclear cataract, with history of eye surgery, or with active ocular pathology were excluded from the study.
Patient Examinations
All patients performed a thorough eye examination including best-corrected visual acuity (BCVA) and slit-lamp microscope (SuZhou 66 Co. Ltd., China). Preoperative BCVA was measured by Snellen charts. The visual acuity of counting fingers and hand motions were assigned values of 1/200 and 1/400, respectively. The postoperative BCVA of patients at 1, 2wk, 1 and 2mo was measured in the same manner as pre-operative BCVA. All cataracts were graded using the Lens Opacities Classification System III (LOCSIII).
Surgical Operation
All surgeries were operated by the same skilled surgeon (Wu Q), and the patients were examined by an researcher (Chen Y). The pupil was dilated with 0.5% tropicamide drops (Santen, Osaka, Japan) 30min prior to surgery, and the other eye was treated with a miotic drug to avoid glaucoma attack. Phacoemulsification was performed under topical anesthesia using 2% lidocaine (ALCON Co. Ltd., USA). The incision was performed at the 9 o'clock (right eye) or 2 o'clock (left eye) positions of the cornea. The chamber was injected using Viscoat immediately (SA Alcon-Couvreur NV, Rijksweg, Puurs, Belgium). Using continuous curvilinear capsulorhexis, the nucleus was removed using a “stop and chop” skill. An automated irrigation/aspiration instrument was introduced into the anterior chamber to remove the cortical remnants and to polish the posterior lens capsule (ACCURUS600DS, ALCON Co. Ltd., USA). The IOL was placed in the capsular bag.
Optical Quality Evaluation
We evaluated the optical quality parameters of the objective scatter index (OSI) using OQAS (VISIOMTRICS. Inc., Spanish) preoperatively as well as at 1, 2wk, 1 and 2mo after surgery. The OSI is calculated by measuring the amount of light outside retinal point spread function (PSF) image in term of the intensity of light in the center. The refractive error was fully corrected during these evaluations; the spherical error (up to -8.00 D) was corrected by the OQAS automatically, and the residual spherical error part (over -8.00 D) and cylindrical error part were corrected using an external lens. We established by OQAS a 4.0-mm pupil, and we also ensured that the pupil diameter was more than 4.0 mm in all subjects. The background illumination was kept at a low level of approximately 25 lx during examination.
Statistical Analysis
All analyses were performed using SPSS software version 19.0. Wilcoxon rank sum t-tests were employed for the preoperative and postoperative comparisons and comparisons between the spherical and aspherical groups of BCVA and lens opacity values. Single sample t-tests were used to analyze the preoperative comparisons of OSI values because some values could not be measured due to the severity of the cataract opacity. Paired sample t-tests were used to analyze the comparisons of OSI between the two groups at the same time after surgery. Bivariate correlation models and spearman correlation coefficients were used to analyze the relationship between OSI and BCVA and the relationship between OSI and lens opacity values. The results are expressed as the mean±SD, and a value of P<0.05 was considered statistically significant.
RESULTS
Best-corrected Visual Acuity Before and After Surgery
In the spherical IOL group, the mean BCVA improved at 1d to 0.61±0.16, at 1wk to 0.72±0.16, at 2wk to 0.8±0.15, at 1mo to 0.85±0.12 and at 2mo to 0.85±0.13. In the aspherical IOL group, the mean BCVA improved at 1d to 0.63±0.13, at 1wk to 0.74±0.15, at 2wk to 0.79±0.12, at 1mo to 0.86±0.12 and at 2mo to 0.87±0.11. There was no difference between the two groups in BCVA before and after surgery (P>0.05).
Lens Density Before Surgery
There are four types of cataract[19]. In the spherical IOL group, the mean nucleus opacity (NO) value was 2.66±0.96, the mean nucleus color (NC) value was 2.76±1.06, the mean cortex (C) value was 2.85±0.76, and the mean posterior lens capsular (P) value was 1.88±1.24. In the aspherical IOL group, the mean NO value was 2.68±0.93, the mean NC value was 2.71±1.13, the mean C value was 2.83±0.89, and the mean P value was 1.89±1.19. There was no difference in NC, NO, C, and P between the two groups (P>0.05). These results indicated that there was no significant difference in the severity of the two groups.
Objective Scattering Index Values Comparison Between Spherical and Aspherical Intraocular Lens
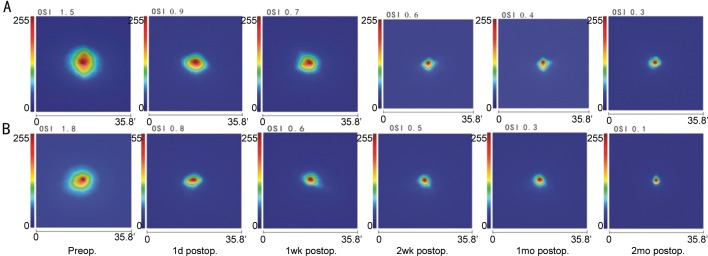
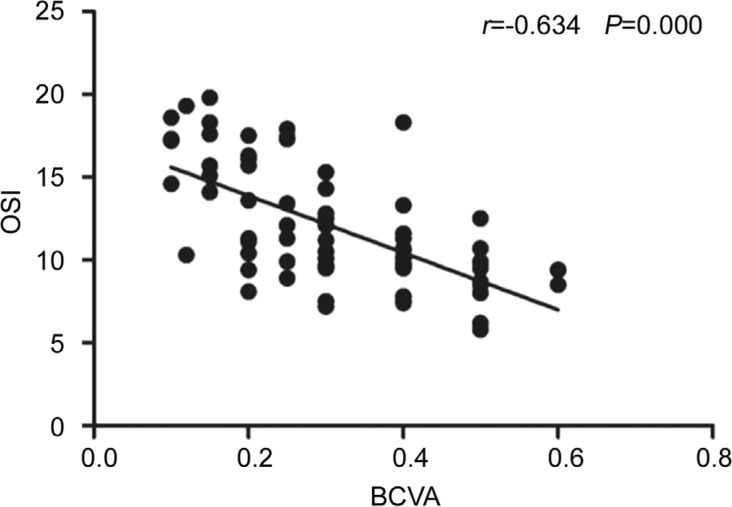
Figure 1 shows the diagrammatic change of OSI values in one patient in the aspherical group prior to and at 1d after surgery. The OSI value decreased from 1.8 to 0.8. Figure 2 shows the diagrammatic OSI value trends in the two groups. Table 1 shows the OSI values of the two groups. The preoperative OSI values of the spherical and aspherical lens groups were 11.5±3.6 and 11.8±3.4, respectively. There were no significant differences between the two groups (P>0.05). OSI values of spherical vs aspherical lenses were 4.1±0.9 vs 3.3±0.8, 3.5±0.9 vs 2.7±0.7, 3.3±0.8 vs 2.6±0.7, 3.2±0.7 vs 2.5±0.8, and 3.2±0.8 vs 2.5±0.8 1d, 1, 2wk, 1 and 2mo after surgery, respectively. There were significant differences (P<0.01) at all time points after surgery between the two groups.
Figure 1. Comparison of OSI change before and after cataract surgery.
The OSI value was 1.8 before surgery and 0.8 after surgery.
Figure 2. OSI changes with the time.
A: OSI changes with the time in the spherical group; B: OSI changes with the time in the aspherical group. 'An arc minute.
Table 1. OSI values differences between the two kinds of IOLs.
| OSI values | Spherical IOL | Aspherical IOL |
| Preop. | 11.5±3.6 | 11.8±3.4 |
| 1d postop. | 4.1±0.9 | 3.3±0.8a |
| 1wk postop. | 3.5±0.9 | 2.7±0.7a |
| 2wk postop. | 3.3±0.8 | 2.6±0.7a |
| 1mo postop. | 3.2±0.7 | 2.5±0.8a |
| 2mo postop. | 3.2±0.8 | 2.5±0.8a |
IOL: Intraocular lens; SD: Standard deviation. Comparison of OSI values between aspherical and spherical IOL at the same time before and after surgery. Values were tested with paired sample t-test. aP<0.05.
mean±SD
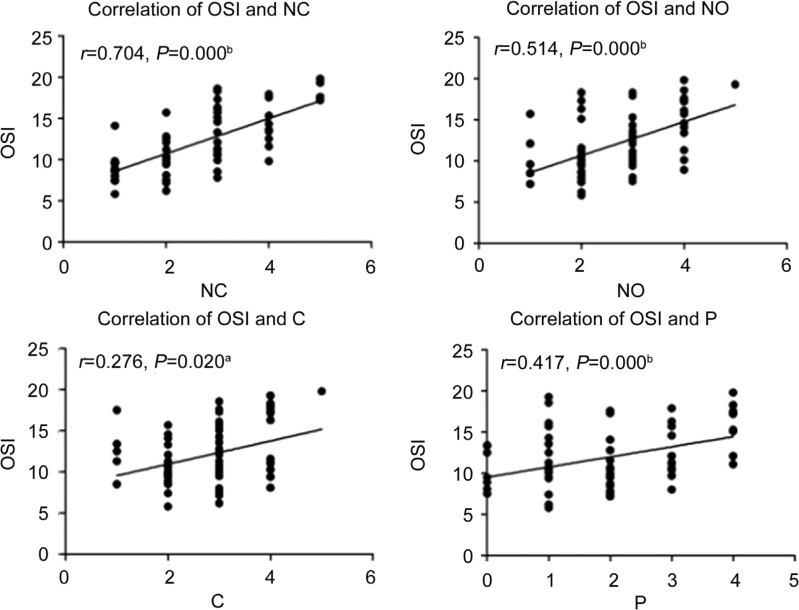
Correction of Objective Scattering Index and Best-corrected Visual Acuity Preoperatively
Figure 3 shows the correlations between the preoperative BCVA and the OSI values of all of the 74 eyes. There was a negative linear correction between the OSI value and BCVA (r=-0.634, P=0.000).
Figure 3. Corrections of BCVA and OSI preoperatively.
There a negative linear correction between the OSI value and BCVA (r= -0.634, P=0.000).
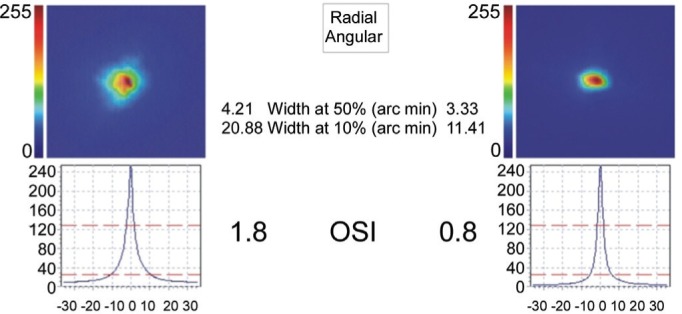
Correction of Objective Scattering Index and Lens Density Preoperatively
Figure 4 shows the preoperative positive linear correlations between the lens LOCUS III value and the OSI value of all the 74 eyes. There were positive linear correlations between the OSI value and the lens LOCUS III value of nucleus color (NC), nucleus opacity (NO), cortex (C) and posterior lens capsular (P) (r=0.704, P=0.000; r=0.514, P=0.000; r=0.276, P=0.020; r=0.417, P=0.000, respectively).
Figure 4. Correction of OSI and lens density preoperatively.
There were positive linear correlations between the OSI value and the lens LOCUS III value of nucleus color (NC), nucleus opacity (NO), cortex (C) and posterior lens capsular (P) (r=0.704, P=0.000; r=0.514, P=0.000; r=0.276, P=0.020; r=0.417, P=0.000, respectively). aP<0.05, bP<0.01.
DISCUSSION
The OQAS was designed in term of the double-pass technique[20], in which the image of a point-source object is directly recorded after reflection on the retina, and a double pass through the ocular media has been shown to accurately estimate the eye's optical quality[12],[21]. The OQAS is used to measure OSI, modulation transfer function threshold (MTF), IOL accommodation, etc. OSI is a ratio of 12 and 20 points from the perspective of the annular region of the light and the central 1 point perspective peak, and it is an important index of optical quality. In the present study, we evaluated the difference in OSI and its relationship with the BCVA and LOCUS. We objectively assessed the OSI, and thereby obtained new reference data for the IOL evaluation.
With the OQAS available, it is possible to study clinically the correction between the widespread subjective clinical classification for example BCVA and LOCUS III and the objective methods of quantifying lens opacification for example OSI. In our study, there was a negative linear correction between the OSI value and BCVA. and the corrections between OSI and LOCUS III were positive lines. For LOCUS III classification, the nucleus color affected OSI most significantly, and posterior lens capsular also had secondly significant impact on OSI. These results are similar to previous report[22] and suggest the suitability of using the OSI as a tool for detecting incipient cataracts.
We measured the OSI values at one day, one week, two weeks, one month, and two months after surgery. With the time increase, the OSI values were decreased until one month after surgery which indicated that the eye conditions were stable from one month after operation.
Our results showed that OSI values decreased both in the spherical IOL and aspherical IOL groups compared with preoperative values. Due to the opacity of the lens, the intraocular scattering of the preoperative value was higher than that in a pseudophakic eye. In our study, the mean preoperative OSI value was 12.0±3.6. The values calculated in our study were slightly higher than those in previous studies[19],[22]. The reason for the difference is that the degree of cataract in our study was more serious than that in previous studies[19],[22]. The OSI in the aspherical IOL implantation group was lower than that in the spherical IOL implantation group. The reason for this may be that the spherical aberrant reduction in the aspherical IOL implantation group reduces the out-of-focus light, thus reducing the OSI value[23]. These results illustrate that reducing IOL aberration improves visual quality.
In conclusion, the OSI values measured by OQAS correctly isolates the information related to intraocular scattering and highlights the relevance of pre and postoperative optical quality evaluation in cataract patients. Our results showed that the OSI values in the aspheric IOL group was lower than that in the spherical IOL group, which indicates that the optical quality in the aspheric IOL group was better than that in the spherical IOL group as measured by the OQAS.
Acknowledgments
Conflicts of Interest: Chen Y, None; Wang X, None; Zhou CD, None; Wu Q, None.
REFERENCES
- 1.Powe NR, Schein OD, Gieser SC, Tielsch JM, Luthra R, Javitt J, Steinberg EP. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Arch Ophthalmol. 1994;112(2):239–252. doi: 10.1001/archopht.1994.01090140115033. [DOI] [PubMed] [Google Scholar]
- 2.Rajabi MT, Korouji S, Farjadnia M, Naderan M, Rajabi MB, Khosravi B, Tabatabaie SM. Higher order aberration comparison between two aspherical intraocular lenses: MC6125AS and Akreos advanced optics. Int J Ophthalmol. 2015;8(3):565–568. doi: 10.3980/j.issn.2222-3959.2015.03.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jia LX, Li ZH. Clinical study of customized aspherical intraocular lens implants. Int J Ophthalmol. 2014;7(5):816–821. doi: 10.3980/j.issn.2222-3959.2014.05.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kretz FT, Tandogan T, Khoramnia R, Auffarth GU. High order aberration and straylight evaluation after cataract surgery with implantation of an aspheric, aberration correcting monofocal intraocular lens. Int J Ophthalmol. 2015;8(4):736–741. doi: 10.3980/j.issn.2222-3959.2015.04.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang Y, Song H, Chen J, Tang X. Comparison of pseudophakic retinal straylight in spherical/aspherical and hydrophobic/hydrophilic intraocular lens. Int J Ophthalmol. 2015;8(6):1146–1150. doi: 10.3980/j.issn.2222-3959.2015.06.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu J, Zhao J, Ma L, Liu G, Wu D, Zhang J. Contrast sensitivity and spherical aberration in eyes implanted with AcrySof IQ and AcrySof Natural intraocular lens: the results of a meta-analysis. PLoS One. 2013;8(10):e77860. doi: 10.1371/journal.pone.0077860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schuster AK, Tesarz J, Vossmerbaeumer U. The impact on vision of aspheric to spherical monofocal intraocular lenses in cataract surgery: a systematic review with meta-analysis. Ophthalmology. 2013;120(11):2166–2175. doi: 10.1016/j.ophtha.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 8.Trueb PR, Albach C, Montés-Micó R, Ferrer-Blasco T. Visual acuity and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses. Ophthalmology. 2009;116(5):890–895. doi: 10.1016/j.ophtha.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Semeraro F, Romano MR, Duse S, Costagliola C. Quality of vision in patients implanted with aspherical and spherical intraocular lens: Intraindividual comparison. Indian J Ophthalmol. 2014;62(4):461–463. doi: 10.4103/0301-4738.116489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tzelikis PF, Akaishi L, Trindade FC, Boteon JE. Spherical aberration and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses: a comparative study. Am J Ophthalmol. 2008;145(5):827–833. doi: 10.1016/j.ajo.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 11.van Gaalen KW, Koopmans SA, Jansonius NM, Kooijman AC. Clinical comparison of the optical performance of aspheric and spherical intraocular lenses. J Cataract Refract Surg. 2010;36(1):34–43. doi: 10.1016/j.jcrs.2009.06.040. [DOI] [PubMed] [Google Scholar]
- 12.Ye C, Ng PK, Jhanji V. Optical quality assessment in normal and forme fruste keratoconus eyes with a double-pass system: a comparison and variability study. Br J Ophthalmol. 2014;98(11):1478–1483. doi: 10.1136/bjophthalmol-2013-304494. [DOI] [PubMed] [Google Scholar]
- 13.Hu AL, Qiao LY, Zhang Y, Cai XG, Li L, Wan XH. Reproducibility of optical quality parameters measured at objective and subjective best focuses in a double-pass system. Int J Ophthalmol. 2015;8(5):1043–1050. doi: 10.3980/j.issn.2222-3959.2015.05.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Effect of femtosecond laser setting on visual performance after small-incision lenticule extraction for myopia. Br J Ophthalmol. 2015;99(10):1381–1387. doi: 10.1136/bjophthalmol-2015-306717. [DOI] [PubMed] [Google Scholar]
- 15.Xiao XW, Hao J, Zhang H, Tian F. Optical quality of toric intraocular lens implantation in cataract surgery. Int J Ophthalmol. 2015;8(1):66–71. doi: 10.3980/j.issn.2222-3959.2015.01.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu CC, Xue T, Wang QM, Zhou YN, Huang JH, Yu AY. Repeatability and reproducibility of a double-pass optical quality analysis device. PLoS One. 2015;10(2):e0117587. doi: 10.1371/journal.pone.0117587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martínez-Roda JA, Vilaseca M, Ondategui JC, Aguirre M, Pujol J. Effects of aging on optical quality and visual function. Clin Exp Optom. 2016;99(6):518–525. doi: 10.1111/cxo.12369. [DOI] [PubMed] [Google Scholar]
- 18.Kamiya K, Shimizu K, Igarashi A, Kobashi H. Time course of optical quality and intraocular scattering after refractive lenticule extraction. PLoS One. 2013;8(10):e76738. doi: 10.1371/journal.pone.0076738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Artal P, Benito A, Perez GM, Alcon E, De Casas A, Pujol J, Marín JM. An objective scatter index based on double-pass retinal images of a point source to classify cataracts. PLoS One. 2011;6(2):e16823. doi: 10.1371/journal.pone.0016823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santamaria J, Artal P, Bescós J. Determination of the point-spread function of human eyes using a hybrid optical-digital method. J Opt Soc Am A. 1987;4(6):1109–1114. doi: 10.1364/josaa.4.001109. [DOI] [PubMed] [Google Scholar]
- 21.Kamiya K, Shimizu K, Igarashi A, Kobashi H, Ishii R, Sato N. Clinical evaluation of optical quality and intraocular scattering after posterior chamber phakic intraocular lens implantation. Invest Ophthalmol Vis Sci. 2012;53(6):3161–3166. doi: 10.1167/iovs.12-9650. [DOI] [PubMed] [Google Scholar]
- 22.Vilaseca M, Romero MJ, Arjona M, Luque SO, Ondategui JC, Salvador A, Güell JL, Artal P, Pujol J. Grading nuclear, cortical and posterior subcapsular cataracts using an objective scatter index measured with a double-pass system. Br J Ophthalmol. 2012;96(9):1204–1210. doi: 10.1136/bjophthalmol-2011-301055. [DOI] [PubMed] [Google Scholar]
- 23.Ohtani S, Gekka S, Honbou M, Kataoka Y, Minami K, Miyata K, Oshika T. One-year prospective intrapatient comparison of aspherical and spherical intraocular lenses in patients with bilateral cataract. Am J Ophthalmol. 2009;147(147):984–989. doi: 10.1016/j.ajo.2008.12.037. [DOI] [PubMed] [Google Scholar]