Abstract
BACKGROUND
The improper control of self-care in hypertension imposes a lot of financial burden on the health-care system. On the other hand, the importance of participatory care and high effectiveness of self-management programs have been confirmed. This study was aimed to examine the effect of an educational intervention on self-efficacy, self-care behaviors and blood pressure (BP) of hypertensive obese or overweight women in the primary health-care setting in Isfahan, Iran.
METHODS
This randomized controlled trial was an educational intervention program. It was performed among 146 hypertensive women of 30-65 age range who referred to 6 health care centers of Isfahan that randomly assigned to a control and intervention groups. The interventional group participated in the 6 weekly sessions including exercises, weight control, medication adherence, and home self-monitoring based on goal setting, and promotion of self-efficacy. The control group received routine care from health-care center and any special intervention has been done for the control group. Output variables were analyzed after intervention, and 6-month follow-up.
RESULTS
There are no significant differences between age, weight, body mass index and BP and biochemical variables except lipids as well as behavioral factors at the baseline. After 6 months intervention self-efficacy (< 0.001) and physical activity (< 0.001) improvement of in the intervention group was significantly different in comparison with the control group. After 6 months, there was a significant reduction in systolic (P < 0.001) and diastolic BP (P = 0.010) in the intervention group.
CONCLUSION
Participatory method of education could help us to convince patients to have better self-care to control disease. Furthermore, since adherence to the treatment of hypertensive patients in our society is low, organizing such courses can teach essential knowledge and skills to lifestyle change and prevention of complications. Performing these courses is recommended for other chronic disease patients in health-care centers to assess self-management programs on self-care behavior.
Keywords: Hypertension, Self-Care, Education, Women
Introduction
Hypertension is the important risk factor for premature death, stroke, and heart disease universal.1 Hypertension is responsible for half of cardiovascular deaths.2,3 The prevalence of hypertension among 30-55 and > 55-year-old population were approximately 23% and 50%, respectively, in Iran,4 and this prevalence in women is higher than men.5
The previous studies have shown that lifestyle changes such as weight loss, reduction of sodium intake, the dietary approaches to stop hypertension (DASH), regular exercise, reduction of stress, quitting smoking, and drinking in addition to medication affect the control of hypertension.6,7 In spite of these recommendations, the majority of hypertension cases remain uncontrolled.8 According to Esteghamati et al.,5 only 6% of Iranian hypertensive patients had controlled blood pressure (BP). On the other hand, although the level of awareness increased among Iranian, the rate of control of hypertension and lifestyle changes is lower than standard among Iranian population.5,9,10
Since the patients’ participation is the gold standard for the control of chronic disease such as hypertension,11 in fact, the gap between knowledge and practice is resolved by patients’ commitment in self-management model.12
Self-management is a relatively new paradigm in controlling chronic disease based on the behavioral theory of self-efficacy and an interactive approach between health-care providers, and patients.13 It seems that training patients for doing self-management could improve the medication adherence and healthy nutrition among chronic disease patients.14 This effectiveness is demonstrated in diabetic patients.15 Self-management in hypertensive patients equals to medications as prescription, and lifestyle changes that lead to the reduction in the crises of hypertension, and control of its complication.16 the advantages of home BP monitoring in international hypertension management guidelines have been accredited too.7
Moreover, using mobile technology as a new, accessible, and acceptable strategy has been effective in supporting healthy behavior such as weight reduction, hypertension control, and healthy nutrition too.17
Based on our knowledge, there are limited experiences to evaluate the impact of self-management in Iranian hypertensive patients. This study examined the effectiveness of integrative approach of self-management, home self-monitoring, and short message service (SMS) on some self-care behaviors and measurable variables such as weight and BP among hypertensive women attending to governmental health-care centers in Isfahan, Iran.
Materials and Methods
This study was a randomized controlled trial. The study population was selected by random cluster sampling from March 2015 to December 2015 in Isfahan. The methodology of the study approved by Isfahan University of Medical Sciences and after obtaining the ethical approval; informed consent form was obtained from each participant and registered in Iranian Randomized Control Trial (IRCT2014061218076N1).
After coordinating to the authorities, in the first step, six health-care centers considered randomly from 10 health-care centers in Isfahan. All obese or overweight hypertensive patients which registered in the health-care system were invited by telephone. In the introductory session, a subject who was eligible and signed the consent form was participated in the study. In the second step, we used the method of randomized binary blocks so that the national code of the subjects has been sorted decently and each binary block randomly assigned to one of the intervention or control groups. So from each of these health-care centers, between 20-30 hypertensive women (depending on the under covered in every health care center) were selected randomly. The selection of the blocks was done by randomly.
In the introductory session, obese or overweight hypertensive women enrolled. The inclusion criteria were being hypertensive (BP ≥ 140/90 mm Hg)18 at least in recent 6 months, being on medication, having a body mass index (BMI) ≥ 25 kg/m2, being in the 30-65 age range, willing to take part in the survey, lacking the ability to walk, having no serious diseases such as diabetes or hypothyroidism or severe complications. The patients who preferred not to continue or were absent for more than 2 sessions were excluded from the study.
To detect a change of 5 mmHg in systolic BP19 with 95% confidence and 80% power, a sample size of 140 participants was considered with attention to the 20% attrition rate; the final sample size was estimated 170 ones for the two groups.
This study has been financially supported by the Vice Chancellor of Isfahan University of Medical Sciences with the project number (Reference: 393790.12/1/2014) and registered in Iran, Randomized Control Trial (IRCT2014061218076N1).
The subjects in the intervention group attended 6-weeks educational sessions weekly. The number of attendants was 8-15 to provide a dynamic group; the length of the session was 2-2.5 hours. One psychologist, a nutritionist and a sports coach (totally three trainers) administered the sessions in all of the health-care centers attended by the researcher. The bases of education were goal setting, promotion of self-efficacy20 and home self-monitoring. Goal setting principal based on SMART goal (specific, measurable, achievable, realistic, and time-related) was explained to them. Then, they set out a reasonable action-specific plan regarding to training topics in every week. Those included physical activity, positive thinking and relaxation, salt restriction and DASH diet, weight control. Furthermore, measurement of BP by a calibrated digital barometer and stretching exercise were trained practically too. According to this method, they were asked to perform and record the trained self-care behaviors on a specific card in home during the week. The following session they attempted to define and show their action plan. The group discussed about the ways to overcome the challenges. They were encouraged by coaches and other attendants. During the follow-up periods, the subjects received text messages (SMS) of the mentioned topics twice a week. One cardiologist-supervised the study and visited them if they had a problem such as medication side effects.
The patients of the control group did not receive any intervention by the researcher. Although, necessary routine care, according to the national protocol for management of hypertension was taken for them in the health-care centers.21 Screening of patients, measurement of BP, patient education and referral to the physician by the nurse on the certain time are headline of it.
These assessments (weight, BP, physical activity, self-efficacy, healthy nutrition) were done during the baseline before and after intervention and follow-up time. Biochemical tests were measured at baseline too. Conducting assessments and filling out the questionnaires performed by a trained nurse to minimize the possible observer-expectancy effect.
A standard mercury sphygmomanometer was used to measure BP according to international protocols.22 The weight was recorded in kilogram and measured using a weight capacity pre-calibrated digital scale without shoes or a heavy cover. The height was obtained by calculating the average of two readings in meters using a portable audiometer. The BMI was determined by dividing weight (kg) by height squared (m2). After at least 12 hours of overnight fasting, the venous blood specimen was collected at a certain laboratory for the measurement of blood-lipid. The participants were asked to complete a 24-hour urine sample. They were said to void their bladder at the first time in the morning. After that, all urine passed during the 24-hour period (day and night) must be collected and stored in a plastic container without any preservatives matter. Then, the samples were delivered to the referral lab to sodium measurement.
The general questionnaire was created for the collection of basic demographic and clinical data. The English translated questionnaire (Stanford self-management questionnaire in chronic disease patients) that will be described in the following lines contains self-efficacy and physical activity.23 It was done through the translation-back-translation process. Nine experts were invited to assess the face and content validity index. The Persian version of the questionnaire was revised according to their comments. After the pilot test, the reliability coefficient of total scale was α = 0.79 with the internal reliability of 0.76.
The scale of self-efficacy consists of six questions scored on a Likert scale from 1 to 10 (“not at all confident” to “totally confident).” The score was the mean of the six items. The higher numbers indicate higher self-efficacy. This scale was defined as one scale to study self-efficacy in arthritis patients for the first time by Lorig et al.23 It evaluates the several domains that are common across lots of chronic diseases, such as the level of confidence in the symptom control, role function, and emotional functioning in control disease. The internal consistency reliability of this questionnaire was 0.91.24
Physical activity scale contains 6 items about the stretching exercise, walking, swimming, use of sports equipment, and other aerobic exercise in the past week (that explained to participants) and minutes of exercise during one week included; never, < 30, 30-60, 60-180, more than 180 minutes with 0-4 scores, respectively. Participants who scored 3-4 coded as adhering to walking recommendations. The test-retest correlation for the physical activities scale was 0.42-0.92.23
The DASH diet questionnaire is a research administrative scale based on DASH foundation. It consists of a diet rich in fruit and vegetables (8-10 servings/day), rich in low-fat dairy products (2-3 servings/day), and low in saturated fat, cholesterol, and salt (sodium chloride).25
13 questions concerning the participants’ diet in the week before the completing of the questionnaire were addressed: 2 about the intake of cooking and table salt; 4 about the consumption of fast food, canned food, and sausage; 3 about the type and amount of meat being consumed (red, chicken, or fish); 2 about the cooking fat (hydrogenate or unsaturated fat); 1 about the way of cooking (fried or boiled); and 1 about fresh fruit and vegetables. Answers were scored on a 5-point Likert scale, from “never” to “always.” (0-5). The reliability coefficient of total scale was α = 0.84. Higher score means healthier nutrition and reverse. The internal reliability obtained 0.79 after completion by 30 patients.
Analyst, cardiologist, and assessor were blinded to the group allocation. Patients were assured that the questionnaires were anonymous so that number and type of disease would be held confidential. Blindness: one of the staffs was unaware to participants.
Statistical analysis was performed using SPSS software (version 17.0, SPSS Inc., Chicago, IL, USA). The Shapiro-Wilk test was used to assess the normality of variables. Continuous data were reported based on mean ± standard deviation and discrete data such as educational level and marital status were calculated with number and (percent). T-test and chi-square test were used for continues and no continues demographic variables. Therefore, the repeated-measures analysis of covariance (ANCOVA) after adjusting for age, low-density lipoprotein (LDL), and cholesterol before, after intervention, and 6 months later was used to test group and time effects and group-by-time. Before repeated-measures, the assumption of ANCOVA test (Boxes test, Leven and Spherocity were checked. Friedman test was used to compare the rate of physical activity before, after intervention, and after 6 months later. The Wilcoxon test for paired samples was used to compare physical activity before intervention, immediately after intervention and 6-month follow-up. P < 0.050 was considered significant.
Results
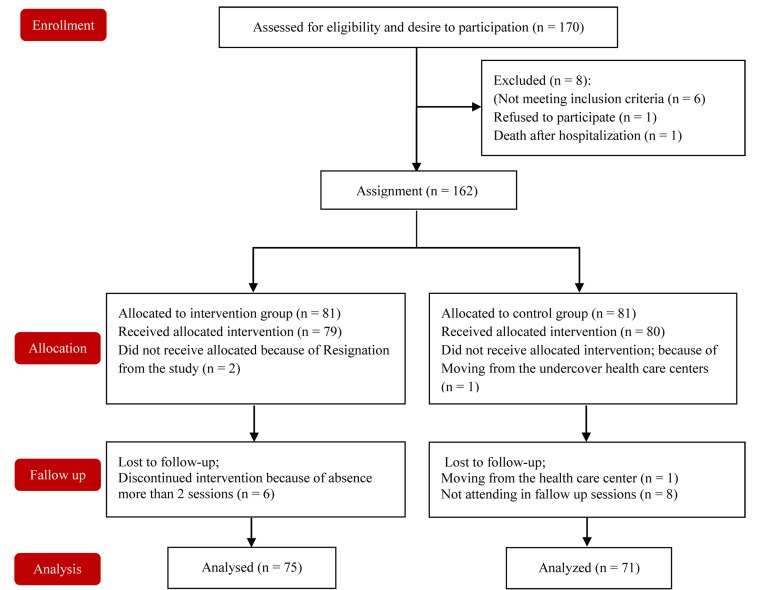
About 146 remained in the study. 10 of the control group left the study because of moving or not attending at the follow-up time. In the intervention group, 6 of them did not complete the study because of the absence of more than two sessions (n = 6). A total of 71 (87.6) in the control group and 74 (91.3) in the intervention group completed the follow-up. A diagram of enrollment and follow-up is shown in figure 1.
Figure 1.
Consort diagram
The baseline characteristics such as age, weight, BMI, BP and biochemical variables (P > 0.050) except cholesterol (P = 0.046) and LDL (P = 0.009) as shown at table 1. Before intervention, total self-efficacy, healthy nutrition, and physical activity have not significant difference in the control and intervention groups (P > 0.050) (Table 2).
Table 1.
Demographic characteristics of overweight or obese hypertensive women in two groups (n = 146)
| Variable | Intervention group | Control group | P |
|---|---|---|---|
| (n = 75) | (n = 71) | ||
| Age (year) | 54.14 ± 6.50 | 52.11 ± 6.50 | 0.062* |
| Weight (kg) | 74.06 ± 10.85 | 73.27 ± 11.79 | 0.672* |
| BMI (kg/m2) | 30.15 ± 4.41 | 30.07 ± 4.27 | 0.913* |
| Biochemical tests | |||
| Cholesterol (mg/dl) | 191.54 ± 41.62 | 205.11 ± 39.19 | 0.046* |
| TG (mg/dl) | 139.21 ± 70.55 | 159.12 ± 86.18 | 0.125* |
| HDL (mg/dl) | 51.25 ± 14.56 | 48.74 ± 15.23 | 0.314* |
| LDL (mg/dl) | 109.54 ± 36.86 | 124.94 ± 32.76 | 0.009* |
| Na (mg/dl) | 131.38 ± 94.20 | 132.90 ± 109.38 | 0.928* |
| Systolic BP | 135.53 ± 15.54 | 139.08 ± 13.84 | 0.148* |
| Diastolic BP | 82.40 ± 8.47 | 84.43 ± 8.80 | 0.157* |
| Duration of diagnosis of hypertension | 6.26 ± 5.86 | 5.68 ± 4.80 | 0.514* |
| Educational level number (%) | |||
| Illiterate | 25 (33.3) | 21 (29.6) | 0.606** |
| < 12 years education | 37 (49.3) | 33 (46.5) | |
| ≥ 12 years and more education | 13 (17.3) | 17 (23.9) | |
| Marital status | |||
| Married | 65 (86.7) | 59 (83.1) | 0.646** |
| Divorced or widow | 10 (13.3) | 12 (16.9) | |
| Self-evaluation of economic situation | |||
| Week | 16 (21.3) | 2 (16.9) | 0.149** |
| Medium | 50 (66.7) | 56 (78.9) | |
| Good | 9 (12.0) | 3 (4.2) | |
| History of backache or arthrosis (%) | 24 (32.0) | 33 (46.5) | 0.090** |
| The number of home self-monitoring | |||
| When I have an appointment with a physician | 19 (25.3) | 15 (21.1) | 0.293** |
| When I have headache | 17 (22.7) | 19 (26.8) | |
| Weekly-monthly | 24 (32.0) | 30 (42.3) | |
| Twice a week-twice a day | 15 (20.0) | 7 (9.9) |
Data shown as mean ± SD.
T-test
Chi-square.
SD: Standard deviation; BP: Blood pressure; BMI: Body mass index; LDL: Low-density lipoprotein; HDL: High-density lipoprotein; TG: Triglycerides
Table 2.
Self-efficacy, some self-management behaviors before, after intervention and 6-month follow-up in the two groups overweight or obese hypertensive women (n = 146)
| Variable | Intervention group (n = 74) | Control group (n = 71) | P |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Self-efficacy* (0-10) | |||
| Before intervention | 6.84 ± 2.11 | 6.52 ± 2.70 | 0.428 |
| After intervention | 8.88 ± 1.80 | 7.15 ± 2.15 | < 0.001 |
| 6-month follow-up | 8.18 ± 1.87 | 7.29 ± 1.90 | 0.005 |
| P follow up** | < 0.001 | ||
| P group | < 0.001 | ||
| Healthy nutrition* (0-55) | |||
| Before intervention | 47.87 ± 4.95 | 46.38 ± 4.41 | 0.056*** |
| After intervention | 51.57 ± 4.16 | 48.52 ± 6.34 | < 0.001 |
| 6-month follow-up | 48.29 ± 4.84 | 47.49 ± 4.04 | 0.280 |
| P follow-up** | < 0.001 | ||
| P group | 0.250 | ||
| Physical activity (3-12)£ | |||
| Before intervention | 2.97 ± 2.72 | 2.74 ± 2.57 | 0.262*** |
| After intervention | 4.96 ± 2.91 | 2.11 ± 3.18 | < 0.001 |
| 6-month follow-up | 4.30 ± 2.99 | 2.91 ± 2.78 | 0.030 |
| P follow-up | < 0.001 | ||
| P group | < 0.001 | ||
Fridman;
P value from repeated measure analysis covariance controlling by age, cholesterol, and LDL.
T test, Paired comparison was used by Bonfferoni test.
Two related samples (Wilcoxon test).
SD: Standard deviation; LDL: Low-density lipoprotein
As shown in table 2, a significant difference is in the mean of self-efficacy between the groups (P < 0.001) and follow-up time (P < 0.001). So that the mean of self-efficacy improve immediately after intervention and 6 months later in comparison to control group after adjusting for baseline.
After adjusting for age, LDL, and cholesterol showed there is not significant difference in the mean of healthy nutrition between two groups (P = 0.250). Although the mean of healthy nutrition increases in the intervention group immediately after intervention (P < 0.001) and decreases after 6 months in the intervention group so that this improvement is not a sustainable change after 6 months. Furthermore, this difference between before intervention and 6 months later is not significant in the intervention group (P > 0.050).
Results showed there is not any significant difference between the mean of healthy nutrition in different times in control group.
Freidman test shows that there is a significant difference in physical activity between two groups after follow-up (P < 0.001). So that the intervention group immediately after intervention have a higher average of physical activity than the control group (P < 0.001). Although there is not any significant differences between immediately after intervention and 6 months later in terms of physical activity in the intervention group (P = 0.120) (Table 2).
Before intervention, there was not any significant difference between the mean of systolic BP between two groups (0.148). As shown in table 3, results show that there is a significant difference between systolic BP of intervention and control group overall (P = 0.045).
Table 3.
Comparison of weight, systolic blood pressure (SBP), diastolic blood pressure (DBP) before, immediately after intervention and 6-month follow-up in the two groups of overweight or obese hypertensive women (n = 146)
| Variable | Intervention group (n = 74) | Control group (n = 71) | P** |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Systolic BP | |||
| Before intervention | 135.53 ± 15.54 | 139.08 ± 13.84 | 0.148 |
| Immediately after intervention | 129.53 ± 15.63 | 129.71 ± 15.48 | 0.943 |
| 6-month follow-up | 128.80 ± 13.35 | 136.05 ± 14.48 | < 0.002 |
| P follow-up* | < 0.001 | ||
| P group | 0.045 | ||
| Diastolic BP | |||
| Before intervention | 82.40 ± 8.47 | 84.43 ± 8.8 | 0.157 |
| Immediately after intervention | 81.77 ± 11.72 | 82.81 ± 10.71 | 0.576 |
| 6-month follow-up | 79.13 ± 7.55 | 84.50 ± 7.66 | < 0.001 |
| P follow-up | 0.120 | ||
| P group | 0.010 | ||
| Weight | |||
| Before intervention | 74.06 ± 10.85 | 73.27 ± 10.79 | 0.674 |
| Immediately after intervention | 72.92 ± 10.40 | 72.95 ± 11.55 | 0.985 |
| 6-month follow-up | 72.34 ± 10.61 | 72.85 ± 12.50 | 0.792 |
| P follow up* | 0.093 | ||
| P group | 0.461 | ||
P value from repeated measure analysis covariance controlling by age, cholesterol, and LDL.
T test, Paired comparison was used by Bonfferoni test.
SD: Standard deviation; LDL: Low-density lipoprotein; BP: Blood pressure
Trend of these changes is significant in two groups too (P < 0.001) so that systolic BP decrease as 7 mmHg in the intervention group, while this decrease is 3 mmHg in control group after 6 months (P < 0.001).
After adjusting for age, LDL, and cholesterol show, there is a significant difference in diastolic BP between the groups (P = 0.010) and follow-up time in the intervention group (P = 0.013). The changes of diastolic BP in control group is not significant at follow-up time (Table 3).
Before intervention, the control and intervention groups are not significantly different in the mean of weight (P < 0.674). Furthermore, there is not any significant difference in weight between two groups (P = 0.461). Although there was a decreasing trend in the mean of weight in two groups, this change is not a significant (Table 3).
Discussion
The results of this study showed that using the participatory method of education based on principals of chronic disease self-management among hypertensive women can improve the self-efficacy, physical activity, healthy nutrition, and reduces BP.
Similar to the results of Park et al.12 and Jung and Lee,26 our results showed significant improvement in self-efficacy, physical activity, and healthy nutrition after educational intervention. Therefore, control of behavior more efficient using this strategy as a key construct to boost of self-care behavior in educational programs. Physical activity in the intervention group improved significantly during follow ups. This result is similar to another behavioral interventions study.27 Studies have shown inactivity elevated hypertension prevalence as 5-12%28 and adherence to the physical activity is recommended to control of hypertension.29 The rate of physical activity in the subjects of our research was very low and the significant difference was nearly according to the related studies.30
Siu et al.27 and Obarzanek et al.31 studies showed benefits of these programs in physical activity, healthy diet and weight loss in Chines population. However, our results demonstrated an increase of adherence to a healthy diet was notable in the intervention group, although it was not effective to weight loss. It seems this difference was due to stretching exercise. Our participants recommended to focus more on stretching exercises than aerobic exercises. While other studies have shown sports which involve big muscles are effective in weight loss. The reason of doing more stretching exercises in our study may be related to comorbidities such as arthritis and back pain preferred to do this type of activity.
Other self-management studies have pointed to increase of healthy nutrition after participation in the self-management programs as an outcome.32 Hence, increases of exercise, as well as adherence to DASH, are different strategies to effect on one special group of hypertensive patients,29,33,34 designing a combined intervention could be considered in educational intervention.
In this study, nutrition situation immediately after educational sessions was better than 6 months later. It could be attributed to encouragement, support and close relationship between coach and participants during the sessions, while after removing external motivators, these changes are dropped. Moreover, nutritional habits are derived from in cultural and familial aspects and its change takes a lot of time. Therefore, other studies pointed to difficulty in long-term lifestyle change among patients.35
In this study, systolic and diastolic BP decreased significantly after intervention (7 and 2 mm/Hg), respectively. However, the mean difference in systolic and diastolic BP in control group was not statistically significant. Glynn et al.36 showed that the mean difference of changes in systolic BP was 1.7 mmHg to +1.3 mmHg and reduction of 1.8-2.5 mmHg in self-home monitoring of educational intervention, and the change of diastolic BP was no significant change to 8 mmHg. Decreases of systolic BP in other self-management studies have been confirmed too.22
Although this change of systolic BP in the current study was not substantial in clinical terms to prevent cardiovascular disease,37 this success besides other changes in patients’ lifestyle (healthy nutrition and physical activity) could be useful in the prognosis of hypertension in a long-term period. The use of a novel method of education in several health-care centers with different socioeconomic positions of patients is noticeable.
Conclusion
Obtained results showed using the participatory method of education, could help us to convince patients to have better self-care to control disease. Furthermore, since adherence to the treatment of hypertensive patients in our society is low, organizing such courses can teach essential knowledge and skills to lifestyle change and prevention of complications. Performing these courses is recommended for other chronic disease patients in healthcare centers to assess self-management programs on self-care behavior.
Limitations: The self-report of physical activity and nutrition were the limitations of our study. This study investigated behaviors of attended patients of urban government public health centers. Since subjects’ willing was considered to participate in the study, the selection bias was not avoidable and these results cannot be generalized to all hypertensive patients.
Acknowledgments
This study has been financially supported by the Vice Chancellor of Isfahan University of Medical Sciences with the project number (reference:393790.12/1/2014). The authors are very thankful to all of the patients for their contribution and appreciate other colleagues in healthcare centers for their support of the participants.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment and control: Data from the China Health and Retirement Longitudinal Study. Bull World Health Organ. 2014;92(1):29–41. doi: 10.2471/BLT.13.124495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Le C, Zhankun S, Jun D, Keying Z. The economic burden of hypertension in rural south-west China. Trop Med Int Health. 2012;17(12):1544–51. doi: 10.1111/j.1365-3156.2012.03087.x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. 10 facts on noncommunicable diseases [Online]. 2013. Available from: URL: http://www.who.int/features/factfiles/noncommunicable_diseases/en/
- 4.Haghdoost AA, Sadeghirad B, Rezazadehkermani M. Epidemiology and heterogeneity of hypertension in Iran: a systematic review. Arch Iran Med. 2008;11(4):444–52. [PubMed] [Google Scholar]
- 5.Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH, et al. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: The national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens. 2008;21(6):620–6. doi: 10.1038/ajh.2008.154. [DOI] [PubMed] [Google Scholar]
- 6.Finset A, Gerin W. How can we promote medication adherence and lifestyle changes in hypertensive patients? Patient Educ Couns. 2008;72(1):1–2. doi: 10.1016/j.pec.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 7. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension. Blood Press. 2013;22(4):193–278. doi: 10.3109/08037051.2013.812549. [DOI] [PubMed] [Google Scholar]
- 8.Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9(1):e84238. doi: 10.1371/journal.pone.0084238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gee ME, Bienek A, Campbell NR, Bancej CM, Robitaille C, Kaczorowski J, et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension). Am J Cardiol. 2012;109(4):570–5. doi: 10.1016/j.amjcard.2011.09.051. [DOI] [PubMed] [Google Scholar]
- 10.Khosravi A, Mehr GK, Kelishadi R, Shirani S, Gharipour M, Tavassoli A, et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: Experiences from the Isfahan healthy heart program. BMC Cardiovasc Disord. 2010;10:61. doi: 10.1186/1471-2261-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rafii F, Soleimani M, Seyedfatemi N. A model of patient participation with chronic disease in nursing care. Koomesh. 2011;12(3):293–304. doi: 10.1111/j.1442-2018.2010.00536.x. [DOI] [PubMed] [Google Scholar]
- 12.Park YH, Song M, Cho BL, Lim JY, Song W, Kim SH. The effects of an integrated health education and exercise program in community-dwelling older adults with hypertension: A randomized controlled trial. Patient Educ Couns. 2011;82(1):133–7. doi: 10.1016/j.pec.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Brady TJ, Murphy L, O'Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and healthcare utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis. 2013;10:120112. doi: 10.5888/pcd10.120112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kennedy A, Reeves D, Bower P, Lee V, Middleton E, Richardson G, et al. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: A pragmatic randomised controlled trial. J Epidemiol Community Health. 2007;61(3):254–61. doi: 10.1136/jech.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lorig K, Ritter PL, Ory MG, Whitelaw N. Effectiveness of a generic chronic disease self-management program for people with type 2 diabetes: A translation study. Diabetes Educ. 2013;39(5):655–63. doi: 10.1177/0145721713492567. [DOI] [PubMed] [Google Scholar]
- 16.Bosworth HB, Powers BJ, Oddone EZ. Patient self-management support: Novel strategies in hypertension and heart disease. Cardiol Clin. 2010;28(4):655–63. doi: 10.1016/j.ccl.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(Pt 1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Cardiovascular disease: A global brief on hypertension Silent killer, global public health crisis [Online]. 2013. Available from: URL: http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en.
- 19.Lorig KR, Holman H. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 20.Samavat T, Hojatzadeh A, Naderi Asiabar Z. The Manual implementation of the national program for prevention and control of high blood pressure 2002 [Online]. 2002. Available from: URL: http://health.bpums.ac.ir/UploadedFiles/xfiles/File/M-Behdashti/rule/pishgiri/gheyre%20vagir/kontorol%20feshar%20khoon-behvarz.pdf.
- 21.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 22.Stanford Patient Education Research Center Stanford University, School of Medicine. Sample questionnaire chronic disease [Online]. 2007. Available from: URL: http://patienteducation.stanford.edu/research/cdquest.pdf.
- 23.Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 24.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension. 2006;47(2):296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 25.Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: Chronic disease self-management programs for older adults. Ann Intern Med. 2005;143(6):427–38. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 26.Jung H, Lee JE. The impact of community-based eHealth self-management intervention among elderly living alone with hypertension. J Telemed Telecare. 2017;23(1):167–73. doi: 10.1177/1357633X15621467. [DOI] [PubMed] [Google Scholar]
- 27.Siu AM, Chan CC, Poon PK, Chui DY, Chan SC. Evaluation of the chronic disease self-management program in a Chinese population. Patient Educ Couns. 2007;65(1):42–50. doi: 10.1016/j.pec.2006.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geleijnse JM, Grobbee DE, Kok FJ. Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. J Hum Hypertens. 2005;19(Suppl 3):S1–S4. doi: 10.1038/sj.jhh.1001953. [DOI] [PubMed] [Google Scholar]
- 29.Jones DW, Hall JE. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43(1):1–3. doi: 10.1161/01.HYP.0000110061.06674.ca. [DOI] [PubMed] [Google Scholar]
- 30.Hordern MD, Dunstan DW, Prins JB, Baker MK, Singh MA, Coombes JS. Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport. 2012;15(1):25–31. doi: 10.1016/j.jsams.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Obarzanek E, Vollmer WM, Lin PH, Cooper LS, Young DR, Ard JD, et al. Effects of individual components of multiple behavior changes: The PREMIER trial. Am J Health Behav. 2007;31(5):545–60. doi: 10.5555/ajhb.2007.31.5.545. [DOI] [PubMed] [Google Scholar]
- 32.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–62. [PubMed] [Google Scholar]
- 33.Khosravi A, Pourheidar B, Roohafza H, Moezzi M, Mousavi M, Hajiannejad A, et al. Evaluating factors associated with uncontrolled hypertension: Isfahan cohort study, Iran. ARYA Atheroscler. 2014;10(6):311–8. [PMC free article] [PubMed] [Google Scholar]
- 34.Sadeghi M, Shiri M, Roohafza H, Rakhshani F, Sepanlou S, Sarrafzadegan N. Developing an appropriate model for self-care of hypertensive patients: first experience from EMRO. ARYA Atheroscler. 2013;9(4):232–40. [PMC free article] [PubMed] [Google Scholar]
- 35.Serour M, Alqhenaei H, Al-Saqabi S, Mustafa AR, Ben-Nakhi A. Cultural factors and patients' adherence to lifestyle measures. Br J Gen Pract. 2007;57(537):291–5. [PMC free article] [PubMed] [Google Scholar]
- 36.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 37.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]