Summary
Background
Millennium Development Goal (MDG) 5 calls for a reduction of 75% in the maternal mortality ratio (MMR) between 1990 and 2015. We estimated levels and trends in maternal mortality for 183 countries to assess progress made. Based on MMR estimates for 2015, we constructed scenario-based projections to highlight the accelerations needed to accomplish the Sustainable Development Goal (SDG) global target of less than 70 maternal deaths per 100,000 live births globally by 2030.
Methods
We updated the open access UN Maternal Mortality Estimation Inter-agency Group (MMEIG) database. Based upon nationally-representative data for 171 countries, we generated estimates of maternal mortality and related indicators with uncertainty intervals using a Bayesian model, which extends and refines the previous UN MMEIG estimation approach. The model combines the rate of change implied by a multilevel regression model with a time series model to capture data-driven changes in country-specific MMRs, and includes a data model to adjust for systematic and random errors associated with different data sources.
Results
The global MMR declined from 385 deaths per 100,000 live births (80% uncertainty interval ranges from 359 to 427) in 1990 to 216 (207 to 249) in 2015, corresponding to a relative decline of 43.9% (34.0 to 48.7) during the 25-year period, with 303,000 (291,000 to 349,000) maternal deaths globally in 2015. Regional progress in reducing the MMR since 1990 ranged from an annual rate of reduction of 1.8% (0 to 3.1) in the Caribbean to 5.0% (4.0 to 6.0) for Eastern Asia. Regional MMRs for 2015 range from 12 (11 to 14) for developed regions to 546 (511 to 652) for sub-Saharan Africa. Accelerated progress will be needed to achieve the SDG goal; countries will need to reduce their MMRs at an annual rate of reduction of at least 7.5%.
Interpretation
Despite global progress in reducing maternal mortality, immediate action is required to begin making progress towards the ambitious SDG 2030 target, and ultimately eliminating preventable maternal mortality. While the rates of reduction that are required to achieve country-specific SDG targets are ambitious for the great majority of high mortality countries, the experience and rates of change between 2000 and 2010 in selected countries–those with concerted efforts to reduce the MMR- provide inspiration as well as guidance on how to accomplish the acceleration necessary to substantially reduce preventable maternal deaths.
Funding
Funding from grant R-155-000-146-112 from the National University of Singapore supported the research by LA and SZ. AG is the recipient of a National Institute of Child Health and Human Development, grant # T32-HD007275. Funding also provided by USAID and HRP (the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction).
Introduction
At the landmark Millennium Summit in September 2000, world leaders agreed to improve the lives of the world’s poor through the acceptance of The Millennium Development Goals (MDGs). (1) The goals committed countries and international agencies to monitor progress on development and health outcomes between 1990 and 2015, including progress on reducing the maternal mortality ratio (MMR; number of maternal deaths per 100,000 live births) as MDG 5, which calls for a reduction of 75% in the MMR between 1990 and 2015.
The process of monitoring progress towards the MDG 5 target exposed the difficulties of measuring MMR, for which there is a paucity of high quality data in many countries. Although maternal mortality had clearly been recognized as a concern and discussed at fora such as the 1987 Safe Motherhood Conference (Nairobi, Kenya), I994 International Conference on Population and Development (Cairo, Egypt), 1995 Fourth World Congress on Women (Beijing, China), and the 1997 Safe Motherhood Technical Consultation (Colombo, Sri Lanka), the MDG announcement provided significant technical and political impetus to improve maternal health.
To assist in the monitoring of progress towards MDG 5, the United Nations Maternal Mortality Estimation Inter-Agency Group, consisting of WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division, has produced estimates for maternal mortality on a regular basis, focusing on country-specific estimates from 1990 to the year of assessment. (2–8) The year 2015 marks the end of the MDG era and is the right time to reflect on the progress made. For this final MDG 5 reporting year, the UN MMEIG carried out a comprehensive assessment of MMR levels and trends for 183 countries, using a new Bayesian model (16) that extends upon prior UN MMEIG estimation methods. (8–11) The resulting estimates presented in this paper provide the first comprehensive overview of the progress that has been made in reducing the MMR from 1990 to 2015 at the global, regional and country level. The year 2015 also marks the start of the Sustainable Development Goals (SDGs), which include the target of reducing global maternal mortality to less than 70 deaths per 100,000 live births by 2030, with no country exceeding twice the global MMR of 140 maternal deaths per 100,000 live births. (9, 10)To highlight the potential impact of meeting this SDG target, we constructed scenario-based projections from 2016 to 2030 based on the SDG target and compared them to a projection based on observed past rates of change.
Methods
This section describes the data inputs, adjustments, assumptions, and statistical model developed by the UN MMEIG to measure levels and trends in maternal mortality for women aged 15–49. Definitions and concepts which are relevant for the measurement of maternal mortality are given in Table 1.
Table 1.
Definitions related to maternal and pregnancy-related mortality.
| Maternal death | Death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes. |
| Pregnancy-related death | Death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the cause of death. |
| Late maternal death | Death of a woman from direct or indirect obstetric causes, more than 42 days, but less than one year after termination of pregnancy. |
| PM | Proportion of maternal deaths among deaths of women of reproductive age. |
| Pregnancy-related PM | Proportion of pregnancy-related deaths among deaths of women of reproductive age. |
| Maternal mortality ratio (MMR) | Number of maternal deaths per 100,000 live births. |
| Maternal mortality rate | The ratio of maternal deaths to the women-years of exposure for the age group 15–49. |
| Life time risk | The probability of a 15-year-old woman eventually dying from a maternal cause, assuming she is subjected throughout her lifetime to the risks of maternal death as estimated for that country-year. (17) |
| Annual (continuous) rate of reduction (ARR) | Measure of relative decline per year, defined as ARR = log(MMRt2/MMRt1)/(t1−t2) where t1 and t2 refer to different years with t1 < t2. |
Data on maternal mortality
The UN MMEIG maintains a publicly available data set with nationally-representative data relevant to maternal mortality including data from vital statistics from civil registration systems (VR), special inquiries, surveillance sites, population-based household surveys (including Demographic Health Surveys, Multiple Indicator Cluster Surveys and Reproductive and Health Surveys) and censuses. The data compilation and search strategy are described in the web appendix (p 1). A summary of how information relating to maternal mortality is collected and categorized by the MMEIG is given in
Table 2, and Table 3 summarizes, by source type, what information related to maternal mortality was used for constructing MMR estimates. Generally, the desired data input was the proportion of maternal deaths among deaths to women aged 15–49 (PM), and a reported MMR was used only if a PM was not available.
Table 2.
Overview of data sources, the collection method, and reporting characteristics.
| Data source type | Method of collection | Type of death reported | Time frame of death reported after pregnancy termination |
|---|---|---|---|
| Civil registration vital statistics (VR) | Death certificate data. certifier provides cause of death information which is coded into ICD. | Maternal |
|
| Specialized studies: Confidential Inquires, Reproductive-age mortality studies (RAMOS), Specialized Studies (e.g. using verbal autopsy, comparing maternal mortality surveillance systems with civil registration data) |
Review of causes and/or specific review for underreporting (combination of misclassification and incompleteness) | Maternal deaths | Depends on review parameters |
| Population-based surveys that collect sibling histories including: DHS; MICS4, Reproductive Health Survey, Maternal Mortality Survey, Family Health Survey |
Direct “sisterhood” method: A representative sample of women are asked about the survival of all their sisters, to determine:
|
Pregnancy- related | Two months |
| Census , post-census enumeration survey | Population censuses can include questions on deaths in households in defined recent reference period. Reported deaths of reproductive aged women trigger questions about the timing of death relative to pregnancy. | Pregnancy- related | Up to 1 year |
| Other sources reporting on maternal mortality: Maternal mortality surveillance system, Ministry of Health, National Statistical Offices |
Review of causes. | Maternal and/or pregnancy- related | Depends on review parameters |
Table 3.
Overview of data sources that are included in the maternal mortality model and the systematic and random errors associated with the observations for each source type that are taken into account in the data model.
| Data source type | Information used to construct maternal mortality estimates | Assumptions about systematic errors (reporting issues which result in biases) | Assumptions about random errors |
|---|---|---|---|
| A1. Civil registration vital statistics, ICD 9 (VR-ICD9) | PM (including late maternal deaths) |
|
Observations are subject to stochastic errors |
| A2. Civil registration vital statistics, ICD 10 (VR-ICD10) | PM | Misclassification of maternal deaths and/or incompleteness | |
| B. Specialized studies | Maternal deaths are used a model input if a rigorous assessment of the total number of all- cause deaths was also carried out in the study to confirm that all deaths to women of reproductive age were captured. Otherwise, the PM or MMR is used*. | No systematic errors | |
| C. Other data sources reporting on maternal mortality | PM or MMR* | Underreporting of maternal deaths | Observations may be subject to sampling, stochastic and/or additional random error |
| D. Other data sources reporting on pregnancy-related mortality, e.g. through sibling histories | Pregnancy-related PM or pregnancy- related MMR* |
|
PM takes precedence over the MMR.
Additional definitions used: Stochastic errors refer to differences between observed PMs and expected PMs due to the randomness associated with the event of a maternal death, i.e., when considering the event of a maternal death as the outcome of a random variable with a Bernouilli distribution with the probability of a maternal death given by the expected PM. Sampling error arises in observed PMs that are obtained from samples that are a subset of the population, e.g. in surveys or sample registration systems. In addition to sampling or stochastic errors, observations may be due to additional random errors, which are non-systematic errors that may occur at any point during the data collection process, e.g. due to how a questionnaire was administered or due to data entry errors. Abbreviations: PM = proportion of all-cause deaths that are maternal; MMR = maternal mortality ratio; VR = vital registration.
The full data base (and all model specifications) used in this analysis is available at http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/. The 2015 update to the UN MMEIG database included over 200 additional records (referring to VR reporting years, studies or reports), resulting in a database with 2608 records that refer to 3634 country-years of information in total, from 1985 until 2015 (see table 4). Source details for all non-VR data points are listed in the web appendix file (webappendix table 2, pp 5–81).
Table 4.
Overview of data inputs used in the maternal mortality model.
| Source type | # records | # country-years |
|---|---|---|
| A. VR | 2025 years of reporting | 2025 |
| B. Specialized studies | 224 studies | 364 |
| C. Other sources - reporting on maternal mortality | 178 reports/studies | 206 |
| D. Other sources - reporting on pregnancy-related mortality | 181 reports/studies | 1038 |
| All | 2608 records | 3634 |
Most data sources on maternal mortality have substantial uncertainty or known biases. The estimation approach attempts to account for these random and systematic errors, which are summarized in Table 3. For VR data, the observed proportion of maternal deaths among all deaths to women aged 15–49 was included as the data input. For VR country-years based on ICD-9, deaths coded to 630–676 were used and for those based upon ICD-10, data coded to codes O00-O95, O98-O99 and A34 were used (which include only those maternal deaths for which the timing corresponds to the definition of a maternal death). An important systematic bias associated with VR data is the potential misclassification of maternal deaths, resulting from error in medical reporting and certification of the cause of death or error in applying the correct ICD code. Misclassification in VR tends to result in undercounting of maternal deaths because there is higher likelihood of misclassifying a maternal death as a non-maternal death rather than in the opposite direction. Earlier analyses found that a large number of nationally representative inquiries into maternal death reporting conducted by countries with VR data consistently suggest that VR systems fail to record around 50% of maternal deaths. (6–8)
Some studies are only able to record information on pregnancy-related deaths (which refer to deaths to women while pregnant or within 42 days of termination of pregnancy, irrespective of the cause of death, see table 2). These observations are subject to systematic error as pregnancy-related deaths tend to exceed maternal deaths because of the inclusion of deaths that are not causally related to the pregnancy. However, because pregnancy-related deaths are (1) reported by a family member and (2) pertain to deaths occurring during pregnancy rather than deaths for which the cause has been medically classified, surveys such as the Demographic Health Survey, and other sources that report pregnancy-related deaths may also be subject to underreporting, especially for deaths occurring early in pregnancy (and thus unbeknownst to the reporting family member). (11)
Sources and construction of other model inputs
Several other inputs are used to estimate MMR and related outcomes. This includes life table entries from WHO life tables, which provides estimates of all-cause deaths among women of reproductive age (12), estimates of live births from the United Nations Population Division World Population Prospects 2015 (13), and estimates of deaths due to HIV/AIDS among females 15–49 years from UNAIDS (14) (details on how these inputs were used are provided in the statistical analysis section). Three covariates were used in the statistical analysis: the gross domestic product per capita (GDP), the general fertility rate (GFR), and the proportion of births delivered by a skilled health personnel (SAB). The rationale for the choice of these covariates has been described by Wilmoth et al (15), the sources and details on constructing trends for these covariates are also provided in the web appendix (section 3).
Statistical analysis
Maternal mortality indicators were estimated with a new Bayesian maternal mortality estimation model, referred to as the BMat model. (16) This model refines the approach previously used by the MMEIG to better incorporate trends in, and uncertainty around, country data. In summary, BMat is able to track high quality data very closely, handle countries that move from survey-based data sources in earlier time periods to newly scaled up VR in later time periods, and combine information from data and covariates for countries with limited data while producing covariate-driven estimates for countries without data. The flexibility of the BMat model eliminates the need for grouping countries based on data availability: one model is used for all countries, regardless of data sources available. Below we provide a technical summary of both the model set-up for MMR as well as the data model used to account for systematic and random errors in the data points; a technical description of the full model and software are available elsewhere. (16)
In the BMat model, the MMR for each country-year is modeled as the sum of the AIDS MMR and the non-AIDS MMR, where non-AIDS MMR refers to maternal deaths due to direct obstetric causes or to indirect causes other than HIV while AIDS maternal deaths are those AIDS deaths for which pregnancy was a substantial aggravating factor. Given the substantial impact of the HIV/AIDS epidemic on mortality in countries with generalized epidemics, the AIDS MMR was modeled separately to be able to capture the trends in maternal mortality associated with the epidemic, following the same procedure used for previous UN MMEIG publications (6–8).
The model for the non-AIDS MMR consists of two components. The main component is a Bayesian hierarchical regression model. This regression model assumes that the logged proportion of non-AIDS maternal deaths among all non-AIDS deaths to women of reproductive age (the dependent variable) is a linear function of random country-specific intercepts and three predictor variables: GDP, GFR and SAB. This multilevel regression model was used in previous estimation rounds to obtain non-AIDS MMR estimates for countries without sufficient high quality data from vital registration systems. (6–8) In the BMat model, this regression model was extended to capture country-specific trends in the non-AIDS MMR as suggested by the data: the regression-based and hence covariate-driven estimates for rates of reduction in the non-AIDS MMR are combined with country-year-specific distortion terms. These distortion terms were modelled with a time series model and estimated for all country-years. The effect was as follows: if data in a country suggested that the non-AIDS MMR decreased faster in year t than expected based on covariates, the data-driven distortion term for that year was estimated to be greater than 0 to capture the acceleration in the MMR reduction beyond the reduction captured by covariates. Similarly, if the MMR reduced less than expected based on covariates, the distortion was estimated to be negative to capture the deceleration in the MMR reduction as compared to the expected covariate-based reduction. For countries with ample data across time, the distortion term plays a more dominant role in the estimation, allowing for the model to track patterns in country data, whereas for countries with limited data, the estimates are more strongly supported by the expected trend implied by the covariates. For countries with continuous time series of high-quality VR data, the model follows the data very closely (given adjustments for misclassification).
We used data quality models to account for systematic and random errors associated with the observed PMs: we assumed that each observed logged PM is equal to the sum of the true logged PM, adjusted for reporting issues to make it comparable to the observed value, and additional error which was assumed to be normally distributed. Details are provided in the technical documentation. (15, 16) In summary, adjustments for reporting issues (outlined in table 3) were similar to adjustments used in previous UN MMEIG studies (6–8). As compared to past MMEIG publications, late maternal deaths were excluded from ICD-10 based PMs, and adjustments were updated accordingly to reflect this change in data inputs. Uncertainty in the adjustment parameters was accounted for through prior distributions on the adjustment parameters and/or added to the overall error variance of the observation. For each observation, total error variance was set equal to its stochastic or sampling error variance, combined with a non-sampling or additional random error variance term for observations from surveys and miscellaneous sources. The resulting total error variances were taken into account in the model fitting such that, with systematic errors being equal, observations of the PM with smaller error variances carried a greater weight in determining the estimates as compared to observations with larger error variances.
Maternal mortality indicators
In addition to the MMR estimates, we also calculated the annual (continuous) rate of reduction (ARR), the life time risk of maternal mortality (LTR) (17) and the maternal mortality rate (MMRate). See table 1 for definitions.
Uncertainty assessment and reporting
The BMat model is a Bayesian model. We used a Markov Chain Monte Carlo (MCMC) algorithm to generate samples of the posterior distributions of all model parameters. (18) The MCMC sampling algorithm was implemented using JAGS 3·3·0 Open Source software (19) and the analysis was carried out in R. (20) Software programs and data are available [http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en].
The sampling algorithm produced a set of trajectories of the MMR for each country, from which other indicators and aggregate outcomes were derived. Point estimates for maternal mortality indicators are based on posterior medians or equivalently, 50th percentiles of posterior distributions. To obtain point estimates of relative reductions, ARRs, as well as aggregate outcomes (e.g., the global MMR) unrounded point estimates of the MMR were used. We computed 80% uncertainty intervals (UIs) for the MMR and all related outcomes using the 10th and 90th percentiles of the posterior distributions. The interpretation of such intervals is that there is a 10% chance that the true outcome is below the interval, and there is a 10% chance that the true outcome is above the interval. We chose to report 80% UIs as opposed to the more standard 95% intervals because of the substantial uncertainty inherent in maternal mortality outcomes: intervals based on higher uncertainty levels quickly lose their utility to present meaningful summaries of a range of likely outcomes.
The UIs for the MMR and related maternal mortality outcomes assess the uncertainty in the indicators based on the available data and uncertain model parameters, such as data adjustment parameters. The uncertainty assessment does not include the uncertainty in any of the demographic indicators that were used as inputs to our model, including the total number of deaths to women of reproductive ages and the number of births.
Country consultation
A Country Consultation process for maternal mortality estimates represents official communication between WHO and Member States, providing the opportunity for countries to share data or provide additional information about national data sources. The process does not involve obtaining approval from Member States regarding the estimates. The MMEIG estimates are intended to describe internationally comparable estimates of maternal mortality, hence they may differ from nationally quoted figures developed using other methodology. During the country consultation for the 2015 estimation round, the MMEIG received new data from twenty six countries that were deemed to be of sufficient quality for inclusion.
Scenario-based projection for 2030
We constructed a scenario-based projection for 2030 to highlight the potential impact of meeting the targets proposed in the post-2015, Sustainable Development Goal (SDG) Framework.(10). The SDG target is to reduce the global MMR to 70 deaths per 100,000 live births in 2030, and in addition, to reduce the MMR in all countries to be lower than twice the global MMR, thus 140, in 2030. (9) As a comparison, we also generated country-specific MMR projections from 2016 to 2030 based on the median of the country-specific ARRs that were estimated for the period 2000–2010, to represent what would happen if the “typical country” experience continued until 2030. The ARR for 2000–2010 was chosen to reflect the recent ARR, as opposed to a later period, to exclude more recent years for which MMR estimates are model-driven for the majority of countries. The median ARR was calculated based on all countries, regardless of the respective level of MMR in the year 2000, because SDG target rates will apply to all countries regardless of their starting level in 2015.
Role of funding
No funding bodies had any role in the study design, data collection and analysis; in the writing of the manuscript; and in the decision to submit the paper for publication. LA, DC, SZ, ABM, and DH had full access to all the data in the study and all authors had final responsibility for the decision to submit for publication.
Results
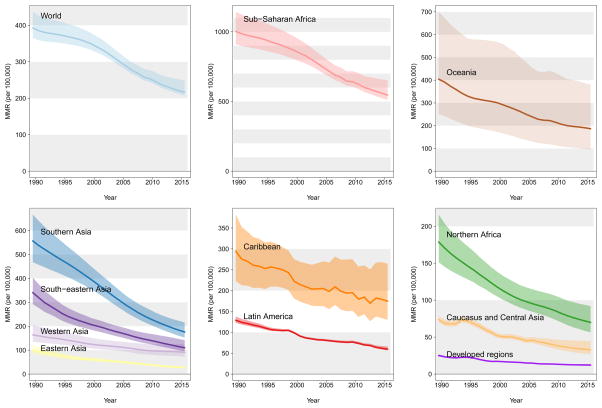
The global maternal mortality ratio decreased from 385 deaths per 100,000 live births (80% UI range from 359 to 427) in 1990 to 216 (207 to 249) in 2015, corresponding to a 43.9% (34.0 to 48.7) decline and an ARR of 2.3 % (1.7 to 2.7) for the period (figure 1 and webappendix table 3 ). Substantial differences between regions exist in terms of progress made as well as current levels of maternal mortality. The highest regional rate of decline for the period 1990–2015 was observed in Eastern Asia (ARR given by 5.0 % (4.0 to 6.0 )) and the lowest was in the Caribbean (ARR 1.8 (0.0 to 3.1)). Regional MMRs for 2015 range from 12 (11 to 14) for developed regions to 546 (511 to 652) for sub-Saharan Africa.
Figure 1. Global and regional MMR estimates (per 100,000 live births) from 1990 to 2015.
Shaded areas refer to 80% UIs. Note: y-axes differ; grey shaded areas in background are comparable across graphs.
The annual number of global deaths decreased from 532,000 (496,000 to 590,000) in 1990 to 303,000 (291,000 to 349,000) ) in 2015. The largest share of global maternal deaths in 2015 occurred in Sub-Saharan Africa (66.3%) corresponding to a total of 201,000 (188,000 to 240,000)) maternal deaths for that region. Estimates for all years can be downloaded from http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/ Cumulatively from 1990 to 2015, 10.7 million women died globally due to maternal causes.
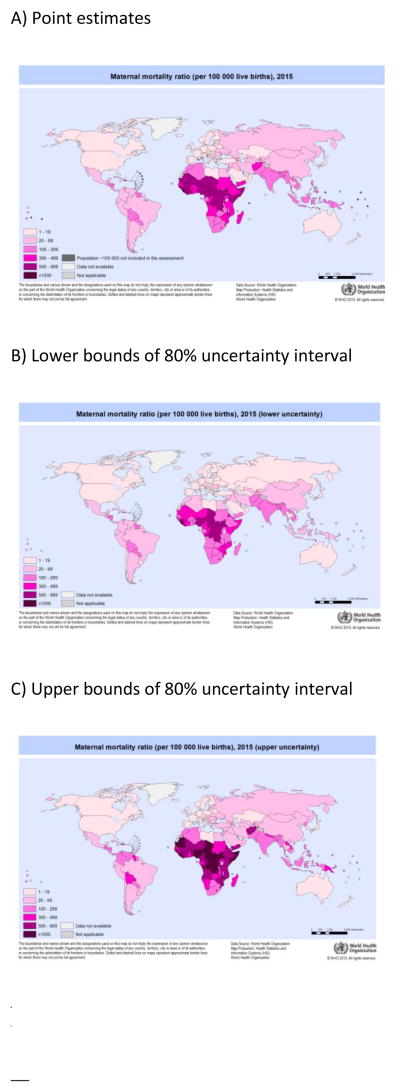
Regional findings may mask variation across countries within a region and regional MMRs may be driven by the MMRs of countries with larger numbers of live births. Country-specific MMR estimates are presented in webappendix table 3 for selected years, estimates for all years are included in figure 2 in the webappendix. Figure 2 illustrates the MMR level for 2015, with point estimates given in graph A, lower bounds of 80% UIs in B and upper bounds in C, where a lower (upper) bound refers to that MMR value for which there is a 10% chance that the country’s MMR is below (above) it. Globally in 2015, the median of the country-specific MMR point estimates was 54 and country levels range from 3 (2 to 3) deaths per 100,000 live births in Finland to 1360 (999 to 1980) in Sierra Leone. The lower bound of the 80% UIs exceeds 500 for eight countries (Central African Republic, Chad, Democratic Republic of the Congo, Guinea, Liberia, Nigeria, Sierra Leone, South Sudan), hence the chance that the MMR is below 500 is less than 10% for these countries. The point estimate for the MMR in 2015 exceeds 500 for an additional 12 countries (Burundi, Cameroon, Cote d’Ivoire, Eritrea, Gambia, Guinea-Bissau, Kenya, Malawi, Mali, Mauritania, Niger and Somalia). Based on point estimates, there are 10 countries with an MMR of 5 or less (Austria, Belarus, Czech Republic, Finland, Greece, Iceland, Italy, Kuwait, Norway, Poland, Spain, and Sweden). Based on the upper bounds of 80% UIs, there is at least a 90% chance that the MMR is less than 5 for Finland, Greece and Poland.
Figure 2. Maternal mortality ratio (per 100,000 live births) for 2015 by country.
A: point estimates, B: lower bounds of 80% UIs, C: upper bounds of 80% UIs
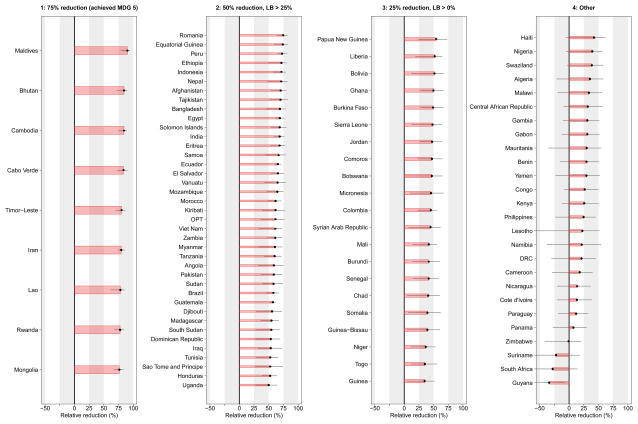
Figure 3 shows the relative reduction between 1990 and 2015 for the 95 countries with a high maternal mortality (point estimate of MMR greater than 100) in 1990. The countries are grouped into four categories as explained in table 5 based on the point estimate for the relative reduction between 1990 and 2015, to assess whether MDG 5 was achieved, as well as the lower bound of their respective 80% UI. For the countries in figure 3, the greatest progress in terms of a relative reduction in MMR has been made in the nine countries in category 1 (Bhutan, Cabo Verde, Cambodia, Iran, Lao, Maldives, Mongolia, Rwanda, Timor-Leste), for which the point estimate of the reduction between 1990 and 2015 suggests that MDG 5 target of a 75% reduction has been met. Of the category 1 countries, the probability of having reached MDG5 is greater than 90% for Cambodia and the Maldives but smaller than 90% for all other countries, suggesting that the finding is less certain for those countries. The other categories are based on point estimates as well as the lower bounds of the 80% UIs for the relative decline. The motivation for taking into account uncertainty intervals when grouping countries is to avoid drawing conclusions based solely on point estimates, which may be highly uncertain. For example, in Nigeria, the point estimate for the relative reduction in MMR since 1990 suggests a decrease of 39.6%. However, the lower bound of the 80% uncertainty interval is given by -5.0%, which is below 0, hence the chance that no progress has been made is greater than 10%; the available information on maternal mortality in Nigeria is too uncertain to absolutely state that progress has been made, illustrating the need to include uncertainty assessments in a categorization of country progress. The largest proportion of countries (21.3%, 39 countries) are in category 2; for countries in this category, the best estimate suggests at least a 50% reduction in MMR, and there is at least a 90% change that the MMR decreased by 25% since 1990. For the 21 countries in category 3, the best estimate suggests that the MMR reduced by at least 25% and there is at least a 90% change that the MMR has declined, but this does not hold true for the 26 countries in category 4. For category 4 countries, the chance that the MMR decreased is less than 90% or the point estimate of the country-specific decline is less than 25%.
Figure 3. Relative reduction from 1990 to 2015 for 95 countries with MMR >100 in 1990.
Countries are grouped based on the categories from Table 6, where LB refers to lower bound of the 80% UI. Within each category, countries are sorted by the point estimate of the relative reduction. Horizontal lines refer to 80% UIs, such that there is a 1 in 10 chance that the relative reduction is greater than the reported upper bound and there is a 1 in 10 chance that the relative reductions is smaller than the reported lower bound. Abbreviations of country names: DRC = Democratic Republic of the Congo, OPT = Occupied Palestinian Territory.
Table 5. Categorization of countries based on evidence for progress in reducing the MMR between 1990 and 2015.
Categories are defined based on two probability statements regarding minimum relative reductions in the MMR between 1990 and 2015, where the first statement is true with at least 50% chance while the second statement is true with at least a 90% chance. The two columns on the right provide the corresponding criteria based on point estimates and lower bound of 80% UIs for the probability statements in each of the categories to hold true. Note that lower bounds of 80% UIs provide one-sided probability statements that refer to 10% or 90% chance.
| Category | Definition based on probabilities regarding relative reductions between 1990 and 2015 | Per cent reduction in MMR from 1990 to 2015 | |
|---|---|---|---|
| Point estimate for % reduction | Lower bound of 80% UI | ||
| 1 | Probability(reduction is at least 75%) > 50% | > 75% | Not applicable |
| 2 | Probability(reduction is at least 50%) > 50% AND Probability(reduction is at least 25%) > 90% |
> 50% | > 25% |
| 3 | Probability(reduction is at least 25%) > 50% AND Probability(reduction is at least 0%) > 90% |
> 25% | > 0% |
| 4 | Probability(reduction is at least 25%) < 50% OR Probability(reduction is at least 0%) < 90% |
Point estimate < 25% and/or lower bound < 0% | |
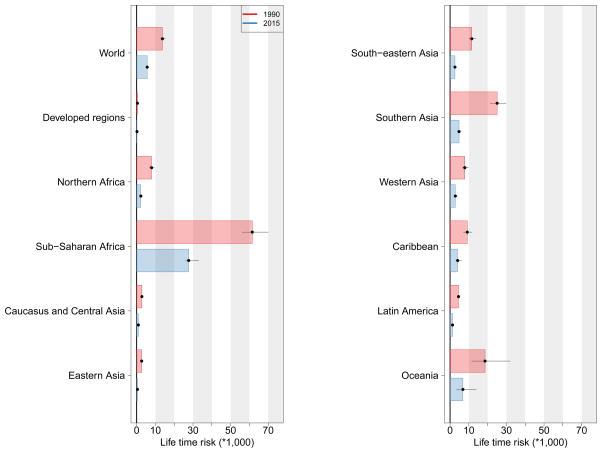
Global and regional estimates for the life time risk of a maternal deaths are displayed in Figure 4. Globally, the risk more than halved between 1990 and 2015, from 14 (13 to 15) maternal deaths per 1,000 women over their lifetimes to 6 (5 to 6) deaths, or equivalently, from 1 death per 73 women (66 to 78) in 1990 to 1 per 180 women (160 to 190) in 2015. The largest relative declines occurred in Eastern Asia and Southern Asia (declines of 84% and 81% respectively). The largest absolute decline occurred in sub-Saharan Africa, where the risk decreased from one per 16 women (14 to 18) in 1990 to one per 36 (30 to 39) in 2015. At the country level, life time risks in 2015 range from 1 per 23,700 (18,000 to 32,700) for Greece to 17 (12 to 23) for Sierra Leone. Similarly, the global maternal mortality rate decreased from 0.41 (0.38 to 0.45) per 1,000 women in 1990 to 0.17 (0.16 to 0.19) in 2015 and at country level in 2015, the rate ranges from 0.001 (0.001 to 0.002) in Greece to 2.0 (1.4 to 2.9) per 1,000 women in Sierra Leone (web appendix material table 4).
Figure 4.
Life time risk (*1,000) of a maternal death 1990 and 2015, globally and by region.
If the world would succeed in reducing the global MMR to less than 70 deaths per 100,000 live births by 2030 (the SDG target), there would be 89,000 maternal deaths in 2030, and about 2.5 million deaths cumulatively between 2016 and 2030 (table 6). This projection of maternal mortality is substantially lower than the projection of a global MMR of 161 deaths per 100,000 live births in 2030 based country-specific ARRs of 2.9%, which is the median of the country-specific ARRs for the period 2000–2010 and represents the projection for a typical country. Regional projected MMRs range from 4 to 128 maternal deaths per 100,000 live births under the SDG scenario, compared to outcomes between 8 and 357 under the more conservative projection.
Table 6. Overview of projections of MMR and maternal deaths for 2030 based on two scenarios.
Scenario 1 is based on past experience in a typical country (ARR of 2.9%) and scenario 2 is based on the SDG goal of a global MMR < 70 by 2030, and MMR < 140 for all countries. MMR is stated as deaths per 100,000 live births.
| Scenario 1: Projection based on ARR of 2.9% | Scenario 2: SDG projection based on global MMR <70 by 2030, and MMR <140 for all countries | |||||
|---|---|---|---|---|---|---|
| MMR in 2030 | Maternal deaths in 2030 | Cumulative maternal deaths | MMR in 2030 | Maternal deaths in 2030 | Cumulative maternal deaths | |
| World | 162 | 224000 | 3912000 | 64 | 89000 | 2521000 |
| Developed regions | 21 | 320 | 6400 | 10 | 160 | 4700 |
| Northern Africa | 18 | 2400 | 50000 | 9 | 1200 | 37000 |
| Sub-Saharan Africa | 43 | 3900 | 76000 | 21 | 1900 | 55000 |
| Caucasus and Central Asia | 123 | 370 | 6500 | 62 | 180 | 4600 |
| Eastern Asia | 359 | 162000 | 2711000 | 128 | 58000 | 1652000 |
| South-eastern Asia | 116 | 41000 | 783000 | 58 | 20000 | 567000 |
| Southern Asia | 119 | 760 | 15000 | 59 | 370 | 11000 |
| Western Asia | 72 | 7900 | 151000 | 36 | 3900 | 109000 |
| Caribbean | 8 | 1100 | 21000 | 4 | 530 | 15000 |
| Latin America | 43 | 1700 | 34000 | 21 | 840 | 25000 |
| Oceania | 59 | 3200 | 58000 | 30 | 1600 | 42000 |
At the country-level, the SDG-required ARR for 2016–2030 is 7.5% for all countries with an MMR below 432 deaths per 100,000 live births in 2015, which is beyond the ARR of 5.5% that was required for MDG 5. Ten countries (Belarus, Cambodia, Estonia, Kazakhstan, Lebanon, Mongolia, Poland, Rwanda, Timor-Leste, Turkey) had point estimates of the ARRs in 2000–2010 that exceeded this SDG-required ARR. For 30 countries with MMRs greater than 432 in 2015, SDG-target ARRs exceed 7.5% to reduce the MMR to be below 140 in 2030.
Discussion
Our analysis provides a comprehensive analysis of global maternal mortality trends based on the latest data available from 171 countries. Globally, the MMR decreased by 43.9% (34.0 to 48.7) from 1990 to 2015, with a global 2015 MMR estimate of 216 (207 to 249) deaths per 100,000 live births, corresponding to a total of 303,000 (291,000 to 349,000) maternal deaths. Hence, the maternal mortality ratio has declined substantially between 1990 and 2015 but progress has been much slower than required to meet the MDG 5 target of reducing the MMR by 75% between 1990 and 2015. The global summary masks variation in progress across regions and in particular, across countries. At the country level, among countries with an MMR greater than 100 in 1990, changes range from an increase of 34.0 (6.5 to 91.2) for Guyana to a decrease of 90.0% (78.9 to 94.6) for the Maldives.
Understanding the drivers of successful progress in reducing maternal mortality, as well as the factors impeding progress are key to informed decision making for reducing the MMR in the post-MDG era. Box 1 summarizes country case studies.
BOX 1. Country examples of accelerated decline of maternal mortality.
Individual case studies have been carried out to analyse the drivers of MMR declines in various countries. In additional, collaborative initiatives such as Countdown to 2015, have published reports and country profiles for high burden countries to discuss coverage of care and its major determinants, including patterns of equity, policies, health system performance measures, and financial flows, at both the global and country levels to understand the underlying factors contributing to improvements in maternal (and newborn, child) health (21). Below, we highlight the achievements of three countries Bangladesh, Cambodia, and Rwanda.
In Bangladesh, a case study examined policy formulation and programme initiatives, availability and access to reproductive and maternal health services, and assessed changes in coverage of key reproductive health interventions. The study also examined relevant contextual factors such as education, access to information, and economic conditions (21, 22). Broadly, the analyses using survey data from 2001 and 2010 found that factors both directly linked to health services and those distal such as improved transportation, access to mobile technology (and thus communication channels for information and social assistance), as well as education and socio-economic status influence maternal health (21, 22). Notably, a near doubling in the proportion of girls with at least some secondary education is believed to be empowering, raising her potential for effective response to maternal complications as well as her ability to navigate the health care system (21, 22). The experience of Bangladesh notably demonstrates the need to look beyond the health care system when considering how to enact game-changing policies to reduce maternal mortality.
Between 1990 and 2015, both Cambodia and Rwanda had accelerated rates of reduction of maternal mortality. Cambodia reduced maternal mortality, with the ARR of 7.4% (5.6 to 8.7), and Rwanda, with an ARR of 6.0% (4.5 to 7.4). In Cambodia, access to health care was improved through heavy government investment in transport infrastructure and in health facilities, from local-level health posts and health centres to referral and national hospitals. Specifically in the area of reproductive, maternal and child health, innovative policies and programme responses have been among strategic priorities in Cambodia from the mid-2000s including a systematic programme to improve the utilization of maternal and newborn health services in public facilities whereby health centres started to operate 24 hours per day and maternity waiting houses and extended delivery rooms were added at health centers to make maternity services more accessible. The Cambodian Ministry of Health also adopted a strategy of increasing both the training of midwives and their absorption into the health system through targeted deployment. To further increase the proportion of births attended by a skilled midwife, financial incentives were offered to health workers. (23)
Rwanda’s substantial reductions in maternal mortality have been linked to a range of key policy and programme interventions. These include the strengthening of the health workforce and infrastructure by the Ministry of Health through the training and deploying of 45,000 community health workers (CHWs) nationwide, including at the village level. A national performance-based financing system incentivizes CHWs by rewarding them according to improvements on selected indicators, including the proportion of women delivering at health facilities. Rwanda also prioritized strong community involvement in the strengthening of the health workforce, allowing villages to elect the three individuals best suited to serve as their CHWs. Additionally, a comprehensive and community-based health insurance scheme has lowered financial thresholds for accessing maternal and child health services and thus expanded access to poorer populations. Finally, Rwanda has greatly strengthened its data collection system to improve priority-setting, planning, and resource allocation: all maternal and child health services have been integrated under one national monitoring and evaluation framework, a web-based Health Management Information System has been developed and deployed and maternal death reviews were scaled up. (24)
Together, these examples illustrate how expansion of service coverage and increasing the number of health care providers, setting standards of care, when referrals should be made, and training programmes for qualified health providers such as midwives helped to accelerate progress in reducing maternal mortality (21–25). These examples also demonstrate the need to balance quality of care and avoidance of over-medicalization in the quest to reduce maternal mortality. (25, 26)
While country success stories provide practical guidance and inspiration for targeted interventions to reduce maternal mortality, country-specific studies also help to better understand major risk factors and potential solutions in any country with high maternal mortality levels so that directed action can be taken. A study in Tanzania suggested that the distance to a health clinic and quality of care were factors contributing to high maternal mortality outcomes. (27) For countries with high HIV prevalence, indirect AIDS maternal deaths have contributed to higher maternal mortality in the last two decades (see web appendix table 5, pp 109–124). Reflecting the effect of interventions, with the increase in anti-retroviral medication use, greater progress can be made in years to come in countries with generalized HIV/AIDS epidemics
Another potential factor that may hinder progress in reducing maternal mortality is an ongoing or emerging humanitarian crisis or fragile settings of conflict, post-conflict or disaster situations. (28) Further compounding this barrier, is that evidence and analyses of these events in these settings often remain anecdotal---collecting data on health outcomes in crisis situations is often not done. While comprehensive provision of maternal and child health interventions may be unrealistic to carry out in countries faced with conflict or natural disaster, targeted actions such as routine obstetric care during crises may still be possible and could reduce maternal mortality from preventable causes. (29)
In 2000 when the MDGs were endorsed, 98 countries had civil registration systems in place, 37 countries had nationally representative surveys conducted in the prior 5–7 years, and few specialized reports on maternal mortality existed. To overcome the limitations of data availability, statistical models have been used to make assessments on progress in maternal health. For the assessment of levels and trends in maternal mortality, we developed a new estimation approach which extended and improved upon the methodology used in past UN MMEIG publications to capture data-driven trends in all countries, while accounting for systematic and random errors in the data inputs. (6–8, 16) Validation exercises suggest that the new model is reasonably well calibrated.(16) In addition to an update to the methodology used for estimating maternal mortality, we also updated the MMEIG data base with over 200 new entries such that the current estimates are based on 2,608 observations corresponding to 3634 country-years of information in 171 countries and used updated estimates for covariates and the number of live births. Figure 1 in the web appendix provides an overview of differences between UN MMEIG estimates published in 2014 and these revised estimates, and decomposes differences into those due to new methods versus updated inputs. (11)
Despite the advances in modelling procedure and data base used, challenges remain regarding the estimation of maternal mortality and there are important limitations to our study. Estimating maternal mortality is challenging because of limited maternal mortality data availability. For example, for 9 out of 171 countries with empirical evidence, there are no data points from 2005 or later, and for 55 out of 171 countries, there is no information since 2010. Moreover, the substantial uncertainty surrounding observations due to random errors (including sampling and/or stochastic errors), as well as uncertainty due to systematic errors in reporting need to be accounted for.
The misclassification of maternal deaths in vital registration systems remains a great obstacle to accurate measurement of maternal mortality in higher income countries. While the addition of a “pregnancy check box” on ICD coding documents has improved death classification for maternal deaths, they continue to be classified outside of related ICD-10 codes. (8) Acknowledging these classification difficulties, countries such as Kazakhstan, Mexico, and Cuba have implemented specialized surveillance systems and administrative protocols to review and correct cause of death assignment before submission to vital statistical departments hence eliminating systematic misclassification errors. (30–32) If implemented in more countries, this would result in more accurate reporting and provide the basis for additional analyses of misclassification that may inform misclassification adjustments for countries without such systems.
In addition to the classification issues in VR data, another reporting issue relates to the impact of the evolving definition and conceptualization of what is a maternal death. During the MDG reporting period, countries with VR systems in place transitioned from ICD-9 to ICD-10. Whereas deaths reported by ICD-9 codes cannot be explicitly identified by timing, ICD-10 introduced the concept of “late maternal deaths”; those that occur after 42 days but up to 1 year after the end of a pregnancy. Since the introduction of these late maternal death codes (O96 and O97), a rise in number late maternal deaths as well as increasing cases of near-miss cases and maternal morbidity has been observed and described by the “obstetric transition” phenomenon (33). While improvements in health care likely contribute to this phenomenon, the potential contribution of changes in reporting also warrants further investigation. Measurement considerations are especially relevant for the release of the 11th revision of the ICD, which is anticipated in 2018, and will be implemented in countries through the latter half of the SDG monitoring period.
For countries without well-functioning VR systems, well-designed research studies and surveillance systems can collect data to undertake cause-specific analyses of mortality to assess the proportion of deaths that are due to maternal causes. (35) However, many countries rely on the reporting of pregnancy-related mortality for estimating maternal mortality, which is challenging because of limited availability of data which allow for a detailed analysis of how pregnancy-related mortality compares to maternal mortality at the national level, and by the additional challenge of defining and estimating which proportion of pregnancy-related AIDS deaths should be counted as maternal deaths due to the aggravating effect of the pregnancy. (8, 35) Recent subnational studies, such as the one carried out by the INDEPTH surveillance network may also provide new insights for estimates. (35) The extent of under- or over-reporting of proportion of pregnancy-related deaths is another uncertain factor. While past studies suggested the underreporting of pregnancy-related PMs (11), a recent study in a demographic surveillance site in Senegal found that the proportion of pregnancy-related deaths was over-reported when using a DHS questionnaire, and that a siblings’ survival calendar may provide a better instrument for measuring pregnancy-related mortality. (36) Further studies are needed to test the validity of these findings in other settings. More generally, to improve maternal mortality estimates, future endeavours related to maternal health monitoring should take into account how data are collected and determine mechanisms to “standardize” data in order to minimize reporting biases (9).
In addition to the limitations due to maternal mortality data issues, the dependency of the maternal mortality estimation on the estimation of adult female mortality as well as the number of births, implies that the challenges and limitations that apply to the estimation of these two indicators are also applicable to maternal mortality estimation. (12, 13) Longer term, uncertainty assessments should include the uncertainty in related indicators such as covariates, all-cause deaths and births. A further limitation is the need to rely on predictor covariates whenever empiric country observations are lacking. Compounding this limitation is the challenge in constructing time series of covariates that are comparable across countries and within countries over time. Doing so for one of the predictor covariates used, skilled birth attendance, is particularly challenging due to issues with definition as well as reporting. (37–40) Given the great uncertainty in maternal mortality indicators, more attention need to be given to the presentation and interpretation of uncertainty intervals. In addition, users of MMR estimates should be warned against post-hoc analyses for countries with limited data, such as correlating the MMR estimates with coverage indicators, given the great uncertainty surrounding the MMR estimates and the covariate-driven estimation approach.
Differences exist between the UN MMEIG MMR estimates and those produced by the Global Burden of Disease study 2013. (41) Table 6 in the web appendix provides an overview of differences in global and regional maternal deaths in 1990 and 2013 and figure 3 in the web appendix shows a comparison of country estimates. Globally, the GBD 2013 study estimated that there were 374,000 number of deaths in 1990, which is much lower than the 532,000 (496,000 to 590,000) maternal deaths estimated by the UN MMEIG. Large differences are observed in Southern Asia and Sub-Saharan Africa. For 2013, differences are smaller: the GBD study estimates 292,000 deaths compared to 315,000 (303,000 to 356,000) deaths estimated in this study. Differences in estimates may be due to differences in estimates of all-cause deaths: all-cause mortality estimates are much lower in the GBD study, as compared to all-cause mortality used by UN MMEIG for the great majority of countries in sub-Saharan Africa in 1990, and GBD all-cause mortality estimates may be subject to underestimation for those countries where estimation relies largely on DHS sibling histories. (42) Other explanations for differences in estimates include differences in the preprocessing of input data (i.e. VR and DHS data), differences in the estimates of the number of births (GBD 2013 used births from the World Population Prospects 2012 revision while the UN MMEIG used birth estimates from the World Population Prospects 2015) as well as differences in the models and covariates used for estimating maternal mortality outcomes. More analysis is necessary to better understand the contribution of the various differences in modeling to the differences in estimates at the country and regional level.
While transitioning from MDG 5 monitoring to the discussion of maternal mortality related targets for the SDGs, a vision of ending all preventable maternal deaths has emerged. (43) While it is recognized that even in the best of circumstances, maternal deaths may still occur, in a world without preventable maternal deaths, everything that could be done to avoid a maternal death is done and is done appropriately. Working towards this aim, the SDG target of reducing global maternal mortality to less than 70 deaths per 100,000 live births by 2030 has been proposed as part of the SDG outcome document. (9, 10) Our projections suggest that the achievement of the SDG maternal mortality target would result in 60.1% fewer maternal deaths in the year 2030, and 1.4 million fewer deaths cumulatively from 2016 to 2030, as compared to a projection to 2030 based on an ARR of 2.9%, as estimated for a typical country during 2000–2010. The ARR required to achieve the SDGs (7.5%) is higher than the ARR which would have led to achievement of the MDGs (5.5%).
While the pay-off of achieving the SDG target is clear based on the projected reduction in number of maternal deaths, much work is needed at the country-level to accomplish this ambitious goal in the coming 15 years. Continued research on what efforts and innovations have the greatest impact to maternal mortality reductions will aid resource allocation and priority setting. The required acceleration will not be possible without a combination of interventions and actions taken, along the lines of the concerted efforts taken by countries that succeeded in bringing about a substantial maternal mortality decline in a short period of time. While each country context will be different, the Ending Preventable Maternal Mortality Strategy suggests for adaptive, highly effective interventions to improve women’s health, before, during, and after pregnancy. (9) Future discussion on interventions must be informed by the content and quality of the care provided; efforts to define and delineate what constitutes “high quality” care, which would be expected to decrease mortality and morbidity, are underway (44). These strategies are complemented by analyses such as LiST and the One Health Tool, which provide insight on the cost-effectiveness and impact on mortality reduction. (45, 46) Achievement of the target will also require the strengthening of robust information systems to monitor progress and inform priority-setting, planning, and resource allocation. The importance of high quality data, specifically on cause of death, to inform decision making and to ultimately reduce maternal mortality is highlighted in the UN Global Strategy for Women’s, Children’s and Adolescents Health-thus putting data collection at the center of political attention. (47, 48)
While the activities and resources needed to accomplish the SDG target may seem overwhelmingly ambitious, current evidence suggests that ten countries-including Cambodia and Rwanda-experienced rates of reduction that exceeded those necessary for the required SDG target. Moreover, a world where millions of preventable maternal deaths continue to occur on an annual basis is not acceptable as an alternative scenario. Hence, the time for action is now.
Supplementary Material
PANEL: Research in context.
Evidence before this study
All publicly available data on maternal mortality are compiled on a regular basis by the United Nations Maternal Mortality Inter-agency Group (UN MMEIG) to improve monitoring of progress towards maternal survival goals, and to enhance the capacity of countries to produce timely estimates of maternal mortality. (6–8) Prior to this study, the global database contained 2374 records and UN MMEIG estimates of maternal mortality levels and trends were constructed using that data base and a multilevel regression model for countries without sufficient high-quality information from vital registration systems. (8)
Added value of this study
This study extended the existing UN MMEIG global database by including 234 additional records. We developed a modelling approach that extends and improves upon the methodology used in prior studies, to construct estimates for 183 countries that capture data-driven trends in all countries, while accounting for systematic and random errors in the observations. (16)
For the first time, this study publishes country-specific MMR estimates up to the MDG target year (2015) and assesses achievements in reducing the MMR between 1990 and 2015. Globally, we estimated that the MMR declined from 385 deaths per 100,000 live births (80% uncertainty interval ranges from 359 to 427) in 1990 to 216 (207 to 249) in 2015. Scenario-based projections from 2016 to 2030 provide insights into the future burden of maternal deaths: in the next 15 years, 3.9 million women would die from a maternal cause of death if each country would continue to reduce its MMR at an annual rate of reduction of 2.9%, which is the median outcome of country-specific rates of reductions estimated from 2000 to 2010. Under the SDG target, the total number of projected cumulative deaths between 2016 and 2030 is 2.5 million, hence 1.4 million lower than the scenario based on a continuation of recent rates of change.
Implications of all the available evidence
With the vision of ending preventable maternal deaths and the mission to reduce the global MMR to 70 deaths per 100,000 in the next 15 years, urgent action is needed to accelerate progress, in particular in countries with substantial maternal mortality burdens. Future action may be guided by past successes in countries with successful concerted efforts to reduce the MMR. Future research on what efforts contribute most effectively to maternal mortality reductions will aid resource allocation and priority setting.
Acknowledgments
We thank the numerous survey participants and the staff involved in the collection and publication of the data that we analysed. We also thank country focal points and participants of regional workshops on maternal mortality estimation for their comments and provision of additional data sources. We are grateful to Jeff Eaton, Bilal Barakat and Emily Peterson for discussion of the study and/or comments on prior versions of the manuscript and to Nobuko Mizoguchi for preparing the census input data. We thank Maria Barreix and Karin Stein for assistance with translation and manuscript preparation.
Footnotes
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the institutions to which the authors are affiliated.
Conflict of interest statement
We declare that we have no conflicts of interest.
Contributors
LA and SZ developed the statistical model and analysed model results. DH and CM provided statistical support and inputs to the model development. DC, DH, DMF, AG and AM constructed input data sets. LA, DC, DH and LS prepared the first draft of the manuscript. All authors reviewed results and provided inputs and comments to the paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Leontine Alkema, University of Massachusetts Amherst, Amherst, USA.
Doris Chou, World Health Organization, Geneva, Switzerland.
Daniel Hogan, World Health Organization, Geneva, Switzerland.
Sanqian Zhang, Harvard University, Cambridge, USA.
Ann-Beth Moller, World Health Organization, Geneva, Switzerland.
Alison Gemmill, University of California, Berkeley, USA.
Doris Ma Fat, World Health Organization, Geneva, Switzerland.
Ties Boerma, World Health Organization, Geneva, Switzerland.
Marleen Temmerman, World Health Organization, Geneva, Switzerland.
Colin Mathers, World Health Organization, Geneva, Switzerland.
Lale Say, World Health Organization, Geneva, Switzerland.
Saifuddin Ahmed, Johns Hopkins University.
Mohamed Ali, World Health Organization, Eastern Mediterranean Regional Office, Cairo, Egypt.
Agbessi Amouzou, United Nations Children’s Fund, New York, USA.
David Braunholtz, Consultant.
Peter Byass, Umeå University, Umeå, Sweden and University of the Witwatersrand, Johannesburg, South Africa.
Liliana Carvajal-Velez, United Nations Children’s Fund, New York, USA.
Victor Gaigbe-Togbe, United Nations Population Division, New York, USA.
Patrick Gerland, United Nations Population Division, New York, USA.
Edilberto Loaiza, UNFPA, New York, USA.
Samuel Mills, The World Bank, Washington DC, USA.
Namuunda Mutombo, African Population and Health Research Center, Nairobi, Kenya.
Holly Newby, United Nations Children’s Fund, New York, USA.
Thomas W. Pullum, DHS.
Emi Suzuki, The World Bank, Washington DC, USA.
References
- 1.UN General Assembly. United Nations Millennium Declaration, Resolution Adopted by the General Assembly; 18 September 2000; [accessed 14 September 2015]. A/RES/55/2. [Google Scholar]
- 2.WHO, UNICEF. Revised 1990 estimates of maternal mortality: a new approach by WHO and UNICEF. Geneva: World Health Organization; 1996. [Google Scholar]
- 3.WHO, UNICEF, UNPFA. Maternal mortality in 1995: estimates developed by WHO, UNICEF, UNFPA. Geneva: World Health Organization; 2001. [Google Scholar]
- 4.WHO, UNICEF, UNFPA. Maternal mortality in 2000: estimates developed by WHO, UNICEF and UNFPA. Geneva: World Health Organization; 2003. [Google Scholar]
- 5.WHO, UNICEF, UNFPA, The World Bank. Estimates developed by WHO, UNICEF and UNFPA. Geneva: World Health Organization; 2007. Maternal mortality in 2005. [Google Scholar]
- 6.WHO, UNICEF, UNFPA, The World Bank. Trends in maternal mortality: 1990 to 2008. Geneva: World Health Organization; 2010. [Google Scholar]
- 7.WHO, UNICEF, UNFPA, The World Bank. Trends in maternal mortality: 1990 to 2010. Geneva: World Health Organization; 2012. [Google Scholar]
- 8.WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Trends in maternal mortality: 1990 to 2013. Geneva: World Health Organization; 2014. [Google Scholar]
- 9.Strategies toward ending preventable maternal mortality (EPMM) Geneva: World Health Organization; 2015. [Google Scholar]
- 10.https://sustainabledevelopment.un.org
- 11.Stanton C, Abderrahim N, Hill K. An assessment of DHS maternal mortality indicators. Studies in Family Planning. 2000;31:111–23. doi: 10.1111/j.1728-4465.2000.00111.x. [DOI] [PubMed] [Google Scholar]
- 12.Life tables for WHO Member States 1990–2012. Geneva: World Health Organization; 2014. [Google Scholar]
- 13.World Population Prospects: The 2015 Revision. New York: United Nations Population Division; 2015. [Google Scholar]
- 14.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2013. [Google Scholar]
- 15.Wilmoth J, et al. A new method for deriving global estimates of maternal mortality. Stat Politics Policy. 2012;3(2):1–38. doi: 10.1515/2151-7509.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alkema L, Zhang S, Chou D, Gemmill A, Moller AB, Ma Fat D, Say L, Mathers C, Hogan D. A Bayesian approach to the global estimation of maternal mortality. (under review) This paper has been submitted as a supplement to this manuscript and will be available through Arxiv at the time of publication. [Google Scholar]
- 17.Wilmoth J. The lifetime risk of maternal mortality: concept and measurement. Bulletin of the World Health Organization. 2009;87:256–62. doi: 10.2471/BLT.07.048280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical model. New York: Cambridge University Press; 2007. [Google Scholar]
- 19.Plummer M, editor. JAGS: A Program for Analysis of Bayesian Graphical Models Using Gibbs Sampling. The third international workshop on 'Distributed Statistical Computing; 2003; Vienna, Austria. [Google Scholar]
- 20.R: A language and environment for statistical computing [Internet] R Foundation for Statistical Computing; 2014. Available from: http://www.R-project.org/ [Google Scholar]
- 21.A Decade of Tracking Progress for Maternal Newborn and Child Survival-The2015 Report-Conference Draft. Geneva: World Health Organization; 2015. [Google Scholar]
- 22.El Arifeen S, Hill K, Ahsan KZ, Jamil K, Nahar Q, Streatfield PK. Maternal mortality in Bangladesh: a Countdown to 2015 country case study. The Lancet. 2014;384(9951):1366–74. doi: 10.1016/S0140-6736(14)60955-7. [DOI] [PubMed] [Google Scholar]
- 23. [accessed 8 August 2015];Cambodia reduces maternal mortality: WPRO. Available from: http://www.wpro.who.int/about/administration_structure/dhs/story_cambodia_reduces_maternal_mortality/en/
- 24.Worley H. [accessed 8 August 2015];Rwanda's Success In Improving Maternal Health: Population Reference Bureau. 2015 Available from: http://www.prb.org/Publications/Articles/2015/rwanda-maternal-health.aspx.
- 25.Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. The Lancet. 384(9949):1215–25. doi: 10.1016/S0140-6736(14)60919-3. [DOI] [PubMed] [Google Scholar]
- 26.Souza JP, Tunçalp Ö Vogel JP, Bohren M, Widmer M, Oladapo OT, Say L, Gülmezoglu AM, Temmerman M. Obstetric transition: the pathway towards ending preventable maternal deaths. BJOG. 2014;121(Suppl 1):1–4. doi: 10.1111/1471-0528.12735. [DOI] [PubMed] [Google Scholar]
- 27.Hanson C, et al. Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. Lancet Global Health. 2015;3(7):e387–95. doi: 10.1016/S2214-109X(15)00048-0. [DOI] [PubMed] [Google Scholar]
- 28.OECD. States of Fragility 2015: Meeting Post-2015 Ambitions. Paris: OECD Publishing; 2015. [Google Scholar]
- 29.Report of the Office of the United Nations High Commissioner for Human Rights on preventable maternal mortality and morbidity and human rights. Geneva: 2010. [Google Scholar]
- 30.Ministry of Health Cuba. Maternal mortality country consultation. 2015. [Google Scholar]
- 31.Commission CCA. Finds of a confidential audit of maternal mortality rates in the Republic of Kazakhstan 2011–2013. Astana: Ministry of Health, Kazakhstan; 2014. [Google Scholar]
- 32.Busqueda intencionada de muertes maternas en México - Informe 2011. Ministry of Health; Mexico: 2013. [Google Scholar]
- 33.Souza JP, Tunçalp Ö Vogel JP, Bohren M, Widmer M, Oladapo OT, Say L, Gülmezoglu AM, Temmerman M. Obstetric transition: the pathway towards ending preventable maternal deaths. BJOG. 2014;121(Suppl 1):1–4. doi: 10.1111/1471-0528.12735. [DOI] [PubMed] [Google Scholar]
- 34.Streatfield PK, et al. Cause-specific mortality in Africa and Asia: evidence from INDEPTH health and demographic surveillance system sites. [Date accessed: 23 Aug. 2015];Global Health Action, [Sl] 2014 Oct;7 doi: 10.3402/gha.v7.25362. Available at: < http://www.globalhealthaction.net/index.php/gha/article/view/25362>. http://dx.doi.org/10.3402/gha.v7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Helleringer S, et al. Improving survey data on pregnancy-related deaths in low and middle-income countries: a validation study in Senegal. Trop Med Int Health. 2015 Aug 7; doi: 10.1111/tmi.12583. [DOI] [PubMed] [Google Scholar]
- 36.WHO. Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. World Health Organization; Geneva: 2004. [Google Scholar]
- 37.Harvey SA, Blandón YCW, McCaw-Binns A, Sandino I, Urbina L, Rodríguez C, et al. and the Nicaraguan maternal and neonatal health quality improvement group. Are skilled birth attendants really skilled? A measurement method, some disturbing results and a potential way forward. Bull World Health Organ. 2007;85:783–790. doi: 10.2471/BLT.06.038455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adegoke A, Utz B, Msuya SE, van den Broek N. Skilled Birth Attendants: who is who? A descriptive study of definitions and roles from nine Sub Saharan African countries. PLoS One. 2012;7:e40220. doi: 10.1371/journal.pone.0040220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Das J, Holla A, Das V, Mohanan M, Tabak D, Chan B. In urban and rural India, a standardized patient study showed low levels of provider training and huge quality gaps. Health Aff (Millwood) 2012;31:2774–2784. doi: 10.1377/hlthaff.2011.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Jan 10;385(9963):117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gerland P, Masquelier B, Helleringer S, Hogan D, Mathers CD. Maternal mortality estimates. The Lancet. 2014;384(9961):2211. doi: 10.1016/S0140-6736(14)62424-7. [DOI] [PubMed] [Google Scholar]
- 42.Bustreo F, Lale S, Koblinsky M, Pullum TW, Temmerman M, Pablos-Méndez A. Ending preventable maternal deaths: the time is now. Lancet Glob Health. 2013;1(4):e176–7. doi: 10.1016/S2214-109X(13)70059-7. [DOI] [PubMed] [Google Scholar]
- 43.Tuncalp Ö, Kristensen F, Temmerman M, Bustreo F, Were WM, MacLennan C, et al. Quality of care for pregnant women and newborns-the WHO vision. BJOG : an international journal of obstetrics and gynaecology. 2015;122(8):1045–9. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.One Health Tool. Available from: http://www.who.int/choice/onehealthtool/en/
- 45.Pollard S, Mathai M, Walker N. Estimating the impact of interventions on cause-specific maternal mortality: a Delphi approach. BMC Public Health. 2013;13(Suppl 3):S12. [Google Scholar]
- 46.Chou D, Daelmans B, Jolivet RR, Kinney M, Say L. Ending preventable maternal and newborn mortality and stillbirths. BMJ. 2015;351:h4255. doi: 10.1136/bmj.h4255. [DOI] [PubMed] [Google Scholar]
- 47.UN Secretary-General. Global Strategy for Women's, Children's and Adolescent Health: 2016–2030. New York: United Nations; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.