Abstract
Objective
While fruit and vegetable (F&V) consumption is associated with lower risk of coronary heart disease and stroke, its association with peripheral artery disease (PAD) is less certain. We thus sought to characterize F&V intake and investigate the association between F&V consumption and presence of PAD in a large community sample.
Approach and Results
Self-referred participants at >20,000 US sites who completed medical and lifestyle questionnaires were evaluated by screening ankle brachial indices (ABI) for PAD (ABI≤0.9).
Among 3,696,778 individuals, mean age was 64.1±10.2 years and 64.1% were female. Daily consumption of ≥3 servings of F&V was reported by 29.2%. Increasing age, female sex, white race, never smoking, being currently married, physical activity, increasing income, and frequent consumption of fish, nuts and red meat, were positively associated with daily consumption of F&V. After multivariable adjustment there was a stepwise inverse association between F&V intake and PAD. Participants reporting daily intake of ≥3 servings of F&V had 18% lower odds of PAD than those reporting less than monthly consumption. In unadjusted and multivariable-adjusted models, the inverse association with F&V became stronger as ABI decreased. When stratified by smoking status, the association was present only among those subjects who currently or formerly smoked tobacco.
Conclusions
Our study demonstrates an inverse association of F&V consumption with prevalent PAD and low overall low F&V consumption. These observations suggest the need to further efforts to increase F&V consumption and for more rigorous evaluation of the role of F&V in PAD prevention.
Keywords: peripheral arterial disease, fruits and vegetables, nutrition
Subject codes: Peripheral Vascular Disease, Diet and Nutrition, Risk Factors, Lifestyle
Introduction
Fruits and vegetables have long been regarded as essential to a healthy diet. The United States Department of Agriculture/United States Health and Human Services Dietary Guidelines for Americans recommend the consumption of at least 4.5 cups of fruits and vegetables combined daily.1, 2 Despite multiple public education campaigns, few American adults report consuming fruits and vegetables at suggested levels.3 Further, particular groups, including men, members of ethnic minorities and those with low socioeconomic status average lower levels of consumption.4–8
Formal recommendations related to fruit and vegetable consumption owe partly to observed associations of the foods with reduced risk of cancer (associations recent prospective studies have found to be much weaker than earlier research suggested9) and overall mortality.10, 11 Findings of benefit with fruit and vegetable consumption have been more congruous in cardiovascular disease, although there are suggestions of differences by vascular territory. For example, inverse associations of fruit and vegetable intake with coronary heart disease have been regularly observed,11, 12 although smaller studies have failed to show significant correlations.13 Reductions in risk of stroke are consistent,14 and potentially of greater magnitude than for coronary heart disease.15 Finally, a recent study of abdominal aortic aneurysm found an inverse association of the condition with fruit, but not vegetable, consumption.16
Despite the wealth of investigation into dietary composition and coronary heart disease and stroke risk, there has been limited investigation on dietary composition and peripheral artery disease (PAD), leading to calls for assessment of dietary components as they relate specifically to PAD.17 Recently, an intervention to encourage adherence to a Mediterranean diet pattern was demonstrated to successfully reduce incident PAD.18 However, the intervention did not focus on fruits and vegetables, and intake of these foods did not significantly differ between treatment and control groups, so a role for these specific foods in PAD prevention could not be assessed. With this in mind, we sought to investigate an association between fruit and vegetable consumption and presence of PAD, in a large community-based sample of nearly 3.7 million American adults. We secondarily sought to study reported fruit and vegetable consumption in this sample.
Material and Methods
Materials and Methods are available in the online-only Data Supplement.
Results
Among 3,696,778 unique individuals, mean age was 64.1±10.2 years, 64.1% were female and 89.1% were white. There were 233,958 (6.3%) cases of PAD as defined by ABI ≤0.9 or history of lower extremity revascularization procedure. As noted previously, the prevalence of different cardiovascular risk factors in this sample was similar to that of the general US adult population.19 Characteristics of the respondents categorized by reported frequency of fruit and vegetable consumption are presented in Table 1. Nearly half of the sample reported consuming at least three servings of fruits and vegetables on fewer than half the days of a week.
Table 1.
Characteristics of study population undergoing vascular screening exams at over 20,000 US sites between 2003 and 2008 categorized by reported frequency of consumption of at least three servings of fruits and vegetables.
| Less than once/month | Once/week - once/month | 2–3 times/week | 4 – 5 times/week | Daily | |
|---|---|---|---|---|---|
| n (%) | 250,648 (7.1%) | 532,731 (15.0%) | 921,000 (25.9%) | 811,518 (22.9%) | 1,035,194 (29.2%) |
| Age (years) ± SD | 62.8 ± 10.9 | 62.1 ± 10.8 | 62.8 ± 10.7 | 63.7± 10.3 | 65.4 ± 10.2 |
| Male | 124473 (51.1%) | 236201 (45.6%) | 345319 (38.6%) | 259184 (32.8%) | 372817 (27.1%) |
| Race/Ethnicity | |||||
| White | 210442 (84.0%) | 452247 (84.9%) | 785533 (85.3%) | 708381 (87.3%) | 903693 (87.3%) |
| Black | 7863 (3.1%) | 17601 (3.3%) | 30677 (3.3%) | 22947 (2.8%) | 25684 (2.5%) |
| Hispanic | 6920 (2.8%) | 14274 (2.7%) | 23211 (2.5%) | 16421 (2.0%) | 21077 (2.0%) |
| Asian | 4929 (2.0%) | 10628 (2.0%) | 18448 (2.0%) | 13554 (1.7%) | 18803 (1.8%) |
| BMI (kg/m2) ± SD | 28.1 ± 5.7 | 28.3 ± 5.8 | 28.1 ± 5.8 | 27.7 ± 5.7 | 27.2 ± 5.7 |
| Hypertension | 119144 (48.6%) | 252040 (48.3%) | 436926 (48.5%) | 379978 (47.8%) | 483730 (47.8%) |
| Diabetes | 27294 (10.9%) | 56317 (10.6%) | 99485 (10.8%) | 86360 (10.6%) | 116133 (11.2%) |
| Hypercholesterolemia | 135670 (54.1%) | 289122 (54.3%) | 499517 (54.2%) | 438844 (54.1%) | 544476 (52.6%) |
| Family history of CVD | 57618 (25.2%) | 124021 (25.5%) | 216205 (25.7%) | 191083 (25.7%) | 238406 (25.2%) |
| Current smokers | 82123 (33.4%) | 155148 (29.7%) | 233283 (25.8%) | 184636 (23.2%) | 215794 (21.3%) |
| Sedentary lifestyle | 132092 (55.1%) | 252310 (49.4%) | 360859 (40.8%) | 263035 (33.6%) | 269051 (26.9%) |
| Marital status | |||||
| Married | 66.6% | 68.1% | 68.9% | 70.6% | 70.1% |
| Divorced | 10.4% | 10.2% | 9.5% | 8.7% | 8.0% |
| Single | 10.7% | 9.6% | 8.7% | 7.6% | 7.4% |
| Widowed | 12.3% | 12.1% | 13.0% | 13.1% | 14.5% |
| Daily nut consumption | 7.0% | 6.5% | 9.2% | 14.1% | 26.1% |
| Daily fish consumption | 1.3% | 0.8% | 0.9% | 1.3% | 4.9% |
| Daily red meat consumption | 8.6% | 6.3% | 6.2% | 5.9% | 8.7% |
| Daily fast food consumption | 2.2% | 1.5% | 1.1% | 0.7% | 1.0% |
BMI – body mass index; CVD – cardiovascular disease; SD – standard deviation
Fruit and Vegetable Consumption
The proportion of participants reporting daily consumption of at least three servings of fruits and vegetables daily differed markedly by age, sex, and race/ethnicity (Supplemental Figures IA and IB). Older white women were most likely to consume ≥3 servings of fruits and vegetables daily. In contrast, younger black men were the least likely to report daily consumption of ≥3 servings of fruits and vegetables.
There was notable variation in fruit and vegetable consumption frequency by region (Supplemental Table I) and state (Supplemental Table II) of residence, and mean income of zip-code provided by the respondent (Supplemental Table III). The Pacific region had the greatest proportion of respondents reporting intake of at least three servings of fruits and vegetables on most days of the week, while less than half of subjects from South Central states reported consumption on most days of the week. The least frequent daily consumption of fruits and vegetables was reported in Mississippi (21.5%), Louisiana (22.0%), Oklahoma (23.5%), Arkansas (24.0%), and Alabama (24.7%).
We built a logistic regression model to assess which of the 16 variables listed above were predictive of daily intake of at least three servings of fruits and vegetables. Increasing age, female sex, non-sedentary lifestyle, increasing income, and frequent consumption (most days of the week) of fish, nuts and red meat, were positively associated with daily consumption of fruits and vegetables. Non-white race, current or former smoking, being currently unmarried, and frequent consumption of fast food were inversely associated with daily intake of at least three servings of fruits and vegetables (Supplemental Table IV). The area under the receiver operating curve of this model was 0.693. The p-value for goodness of fit testing was 0.59.
Peripheral Arterial Disease
After multivariable adjustment for age, sex, race/ethnicity and clinical risk factors, a stepwise inverse association between fruit and vegetable intake with the prevalence of PAD was apparent (Table 2, Figure 1A, P for trend <0.001). Additional adjustment for income and dietary components other than fruits and vegetables resulted in minimal attenuation of the association (P for goodness of fit = 0.12). The association persisted, but was found to be slightly more pronounced in men (p < 0.01) when adjusted analyses were stratified by sex (Supplemental Table V). Stratification of the sample by cigarette smoking status (current, former, never), demonstrated that the inverse association of increasing fruit and vegetable consumption with PAD was limited to subjects who currently or formerly smoked (Table 3).
Table 2.
Odds ratio for PAD (as defined by ABI <0.9 or prior revascularization) by fruit and vegetable intake relative to less than once/month consumption of at least three servings of fruits and vegetables
| Less than once/month | Once/week - Once/month | 2 – 3 times/week | 4 – 5 times/week | Daily | |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Unadjusted | 1.0 | 0.85 (0.83 – 0.86) | 0.81 (0.80 – 0.83) | 0.78 (0.76 – 0.79) | 0.83 (0.81 – 0.84) |
| Adjusted for age, sex, race/ethnicity | 1.0 | 0.86 (0.84 – 0.88) | 0.78 (0.77 – 0.79) | 0.71 (0.69 – 0.72) | 0.68 (0.67 – 0.69) |
| Adjusted for age, sex, race/ethnicity, clinical risk factors | 1.0 | 0.89 (0.87 – 0.91) | 0.84 (0.83 – 0.86) | 0.80 (0.78 – 0.81) | 0.80 (0.79 – 0.82) |
| Adjusted for age, sex, race/ethnicity, clinical risk factors, income | 1.0 | 0.89 (0.87 – 0.91) | 0.84 (0.83 – 0.86) | 0.80 (0.78 – 0.82) | 0.81 (0.79 – 0.82) |
| Adjusted for age, sex, race/ethnicity, clinical risk factors, income, diet | 1.0 | 0.89 (0.87 – 0.91) | 0.84 (0.83 – 0.86) | 0.80 (0.79 – 0.82) | 0.81 (0.79 – 0.83) |
ABI – ankle-brachial index, BMI – Body Mass Index (kg/m2), CI – Confidence Interval, OR – Odds ratio, PAD – Peripheral Arterial Disease, SES – socioeconomic status
Clinical risk factors include: diabetes, hypertension, hypercholesterolemia, sedentary lifestyle, tobacco use (current, former, never), family history of vascular disease and BMI (as a continuous variable)
Diet includes consumption of nuts, fish, red meat
Figure 1A.
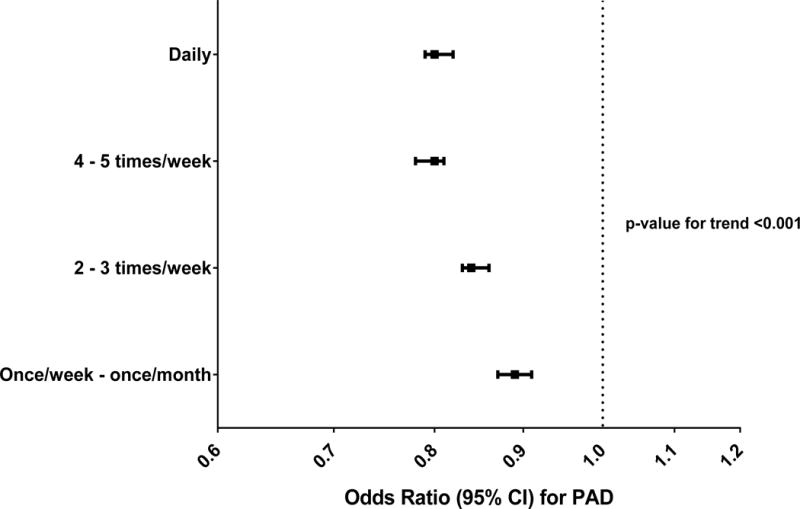
Adjusted odds ratios for any PAD (ABI < 0.9) by fruit and vegetable intake relative to less than once/month consumption of at least three servings of fruits and vegetables.
Adjusted model includes: diabetes, hypertension, hypercholesterolemia, sedentary lifestyle, tobacco use (current, former, never), family history of vascular disease, BMI (as a continuous variable) and consumption of nuts, fish and red meat.
Table 3.
Odds ratio for PAD (as defined by ABI <0.9 or prior revascularization) by fruit and vegetable intake relative to less than once/month consumption of at least three servings of fruits and vegetables – stratified by smoking status.
| Less than once/month | Once/week - Once/month | 2 – 3 times/week | 4 – 5 times/week | Daily | |
|---|---|---|---|---|---|
| Smoking status | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Current | 1.0 | 0.86 (0.83 – 0.89) | 0.78 (0.75 – 0.80) | 0.70 (0.68 – 0.73) | 0.65 (0.63 – 0.68) |
| Former | 1.0 | 0.87 (0.84 – 0.91) | 0.83 (0.80 – 0.86) | 0.79 (0.76 – 0.82) | 0.79 (0.76 – 0.82) |
| Never | 1.0 | 0.97 (0.93 – 1.01) | 0.98 (0.94 – 1.02) | 0.97 (0.93 – 1.01) | 1.02 (0.99 – 1.06) |
Model is adjusted for all variables incorporated into final model of Table 2.
Among all subjects with abnormal ABI, 73.2% (n = 121,389) had ABI 0.9 – 0.7, 19.7% (n = 32648) had ABI 0.7 – 0.5, and 7.1% (n = 11717) had ABI <0.5. The inverse association with fruit and vegetable intake was stronger with decreasing ABI in both crude and multivariable-adjusted models (Figure 1B).
Figure 1B.
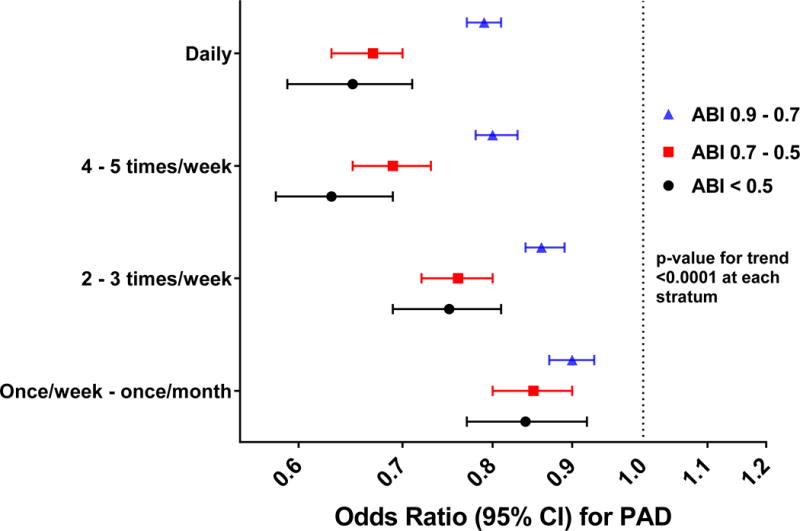
Adjusted odds ratios for increasingly abnormal ABI measures by fruit and vegetable intake relative to less than once/month consumption of at least three servings of fruits and vegetables.
Adjusted models include: diabetes, hypertension, hypercholesterolemia, sedentary lifestyle, tobacco use (current, former, never), family history of vascular disease, BMI (as a continuous variable) and consumption of nuts, fish and red meat.
Discussion
We present data from a self-referred sample of approximately 1.6% of all American adults in which we observed an association of greater frequency of consumption of fruits and vegetables with lower odds of prevalent PAD defined by abnormal ABI or history of prior lower extremity revascularization, but that a minority of participants reported consuming at least three servings of fruits and vegetables on a daily basis. Our adjusted analyses demonstrated a stepwise reduction in odds for PAD with increasing consumption of fruit and vegetables – associations which were stronger with increasingly abnormal ABI. Notably, this association was restricted to persons who were current or former cigarette smokers.
Unfortunately, our findings regarding fruit and vegetable consumption are in agreement with those of other, smaller surveys. Data from the 2007 – 2010 National Health and Nutrition Examination Surveys (NHANES) suggest that less than 20% of adult Americans consume fruits and vegetables at the United States Department of Agriculture’s recommended levels,8 with even lower prevalence found by the Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System.7 In our sample, 29.2% of subjects reported daily intake of at least three servings of fruits and vegetables daily, with just over half reporting this degree of consumption on most days of the week. Our state-level data is also very similar to that reported by the CDC,20 in which individuals living in Southern states reported less frequent fruit and vegetable consumption than did those residing in other regions. Further, our sample mirrored smaller cohorts in which men, blacks and relatively younger adults reported less frequent fruit and vegetable intake than did women and other races.4–7
The degree to which the American population as a whole, and certain segments in particular, fail to achieve guideline-directed fruit and vegetable consumption, has been recognized for more than three decades.21 While food consumption decisions are multifactorial (as supported by the modest value of our regression model to predict daily fruit and vegetable consumption), two recognized hurdles to increased consumption are availability and cost. Indeed, in our geographically diverse sample, we found both greater income, as well as frequent intake of other costly foods such as fish and red meat, to be strongly predictive of daily fruit and vegetable consumption.
Public marketing campaigns such as ‘5 A Day for Better Health’ and the current ‘Fruits and Veggies – More Matters’ have met with limited success in increasing consumption of fruits and vegetables by American adults.22 A large gap remains between goal and actual fruit and vegetable consumption, leading experts to advocate for multi-modality approaches to attain recommended consumption levels across the population.23 Our observation of the levels of fruit and vegetable intake in this large community-based sample highlights this divide. As the limited sensitivity and specificity of our regression model demonstrates, this is certainly a complex endeavor. However, our analyses provide evidence of the need to focus on the particularly low fruit and vegetable intake in certain groups, including non-whites, men, those living in Southern states, those with low incomes, and smokers.
In addition to confirming the overall low frequency of recommended levels of fruit and vegetable intake among American adults, we further observed an association of greater consumption with lower odds of prevalent PAD defined by ABI ≤0.9. Our adjusted analyses demonstrated a stepwise reduction in odds for PAD with increasing consumption of fruit and vegetables – associations which were stronger with more abnormal ABI measures.
Although a number of studies have found inverse associations of nutrients present in fruits and vegetables with prevalent PAD24–26 and incident claudication,27 to our knowledge, this is only the second assessment of an association specifically between fruit and vegetable consumption and PAD. The first was a report at year 12 of the Health Professionals Follow-Up Study.28 In that cohort, 295 cases of incident, symptomatic PAD had been confirmed in the approximately 44,000 men without diabetes or vascular disease at enrollment. In age-adjusted analyses, the investigators also found a step-wise reduction in risk for incident PAD by quintile of fruit and vegetable intake. However, when smoking and exercise were included in the models, this association was attenuated and no longer statistically significant in this sample with a low incidence of PAD (0.7%). In our very large sample with PAD (both symptomatic and asymptomatic defined by ABI ≤0.9) prevalence >6%, we detected a stepwise inverse association of fruit and vegetable consumption with prevalent PAD that persisted with correction for age, sex, race/ethnicity, smoking, physical activity, income and multiple other CVD risk factors, and was of greater magnitude with lower ABI.
When we stratified our sample by smoking status, we found that the inverse association of fruit and vegetable intake with PAD was limited to subjects who formerly or currently used tobacco (Table 3). This observation has precedence. In the above mentioned Health Professionals Follow-Up Study, the observed trend toward a reduced incidence of PAD with fruit and vegetable intake was present in active smokers, but not in a combined group of never and former smokers.28 Likewise, intake of nutrients prevalent in fruits and vegetables – β-carotene, vitamin C and lycopene – have been associated with reduced risk for developing claudication in male smokers,27 and an association of vitamin C consumption and ABI in the Edinburgh Artery Study was seen only in individuals who had smoked, not in those who had never smoked.29 An interaction of smoking with vitamin C intake and the risk of stroke has also been reported.30 Hypothesized mechanisms underlying reduced atherosclerosis with fruit and vegetable consumption generally involve action of micronutrients contained in the foods. Indeed, the prevailing explanation for the isolated associations in smokers is that antioxidant nutrients supplied via fruits and vegetables only manifest detectable disease-preventing effects in the setting of significant oxidative stress, as occurs with smoking. Within the pathophysiology of PAD, oxidative stress is felt to be important in both the initiation and progression of the disease,31 and increased antioxidant capacity may inhibit this process.
A number of other mechanisms are also hypothesized to explain any protection from cardiovascular disease acquired with frequent fruit and vegetable consumption. One is through salicylic acid present in these foods.32 A reduction in blood pressure, demonstrated in several randomized, controlled trials is another.33, 34 Although improved serum lipid profiles associated with the substitution of fruit and vegetables for foods containing more fat and/or less fiber are also hypothesized to mediate inverse associations with atherosclerosis, high quality experimental support for this is lacking.35 The evidence for greater fruit and vegetable consumption to afford reduced weight similarly lacks a strong evidentiary foundation,36, 37 and seems contingent on the substitution of fruits and vegetables for more calorically-dense and fiber-poor foods.38
Limitations of our analysis include its cross-sectional nature that does not allow for assessment of longitudinal dietary consumption that is likely important in the development and progression of this chronic disease. Our survey instrument was not validated and left the definition of a “serving” to the determination of the participant. Further, the presence of a single question regarding fruit and vegetable consumption also does not allow for individual assessment of separate fruit or vegetable consumption with PAD prevalence, nor does it allow us to assess overall servings of fruits and vegetables consumed by a participant. This introduces the potential for “miscategorization” of participants with infrequent consumption of many servings of fruits and vegetables, as well as those with frequent consumption of slightly fewer than 3 servings of the foods. However, any miscategorization would serve to bias our observations toward the null – suggesting that our observed effect potentially underestimates the size of the actual effect of fruit and vegetable intake on PAD. Additionally, despite this limitation, our survey instrument likely provides ranking validity, and the five categories of consumption represent strata of overall fruit and vegetable intake. Further, there is some evidence that suggests that for the purposes of categorizing total consumption of foods, that the frequency of intake is more important the number of servings.39
Despite our correction for over a dozen established risk factors for atherosclerotic disease and other variables, there are likely confounders which were not measured in our limited survey. Specifically, our data do not allow for estimation of whole grain, alcohol, or total energy intake in our sample. Our survey also did not query use of vitamin supplements. Given the previously reported associations and mechanistic plausibility of greater fiber and/or antioxidant vitamin intake with PAD prevention, whole grain consumption and use of vitamin supplements are potential unmeasured confounders of our findings. The absence of total energy intake could also confound associations given that greater total energy intake correlates with greater consumption of multiple food groups. This potential association is borne out in the propensity for those subjects who reported consuming fruits and vegetables more frequently to also report more frequently consuming nuts and fish, but also red meat (Table 1). However, when analyses were restricted to those participants who reported eating nuts, fish and red meat at least four times weekly (as a surrogate for high energy intake), the inverse association of fruits and vegetables with PAD was unchanged (data not shown).
Finally, although one strength of our study is our objective outcome of PAD defined by an abnormal value (≤0.9) on directly measured ABI (rather than symptomatic PAD, which may occur in the minority of patients with abnormal ABI40), ABI is not as sensitive or specific as angiography for the diagnosis of PAD.41 One reason for impaired sensitivity in ABI is the predilection for elderly, diabetics, and patients with end stage renal disease to have elevated, rather than reduced ABI. However, the persistence of our findings when restricted to severely reduced ABIs, as well as with the exclusion of diabetics (data not shown), strengthens the confidence that can be assigned to our conclusions.
Nonetheless, the major strengths of our study are its inclusion of nearly 3.7 million subjects, and its demonstration of a clear inverse association of prevalent PAD, as defined by a directly-measured abnormal ABI, with fruit and vegetable intake, even with correction for multiple established PAD risk factors. These findings are restricted to subjects who have a history of tobacco use, in accordance with prior studies of antioxidant micronutrients and PAD, and thus are suggestive of a possible mechanism underlying the association.
Our study adds to the burgeoning literature regarding dietary consumption and PAD, emphasizing the necessity of further studies into diet and PAD specifically, so that dietary recommendations and interventions for reducing the burden of this disease can be established. This study also provides further evidence that fruit and vegetable consumption varies markedly by sex, race and region of the United States, but is universally poor. This observation supports the continued need for programs to improve the dietary patterns of all Americans.
Supplementary Material
Highlights.
There is a stepwise inverse association between fruit and vegetable intake and prevalence of PAD
The inverse association of fruit and vegetable intake with PAD is stronger with increasing severity of disease and restricted to current and former smokers
Fruit and vegetable intake at recommended levels is universally poor
Fruit and vegetable intake varies by demographics and geography
Acknowledgments
This work has utilized computing resources at the High Performance Computing Facility of the Center for Health Informatics and Bioinformatics at New York University Langone Medical Center.
Sources of Funding
Dr. Berger was partially funded by the National Heart and Lung Blood Institute of the National Institutes of Health (HL114978). Dr. Heffron was supported in part by T32 HL 098129 and KL2 TR001446.
Funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Abbreviations
- ABI
ankle-brachial index
- PAD
peripheral artery disease
Footnotes
Disclosures
There are no potential conflicts of interest. The authors gratefully acknowledge the participation and generosity of Life Line Screening (Cleveland, OH), who provided these data free of charge for the purposes of research and with no restrictions on its use for research or resultant publications.
References
- 1.US Department of Health and Human Services and US Department of Agriculture. Dietary Guidelines for Americans 2015 – 2020. 8th. Washington, DC: U.S. Government Printing office; 2015. [Google Scholar]
- 2.US Department of Health and Human Services and US Department of Agriculture. Dietary Guidelines for Americans, 2005. 6th. Washington, DC: U.S. Government Printing Office; 2005. [Google Scholar]
- 3.US Department of Health and Human Services and Centers for Disease Control and Prevention. Adults Meeting Fruit and Vegetable Intake Recommendations - United States, 2013. Morbidity and Mortality Weekly Report. 2015;64(26):709–713. [PMC free article] [PubMed] [Google Scholar]
- 4.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J Acad Nutr Diet. 2012;112(5):624–635.e6. doi: 10.1016/j.jand.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Storey M, Anderson P. Income and race/ethnicity influence dietary fiber intake and vegetable consumption. Nutr Res. 2014;34(10):844–850. doi: 10.1016/j.nutres.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 6.Dubowitz T, Heron M, Bird CE, Lurie N, Finch BK, Basurto-Davila R, Hale L, Escarce JJ. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008;87(6):1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore LV, Dodd KW, Thompson FE, Grimm KA, Kim SA, Scanlon KS. Using Behavioral Risk Factor Surveillance System Data to Estimate the Percentage of the Population Meeting US Department of Agriculture Food Patterns Fruit and Vegetable Intake Recommendations. Am J Epidemiol. 2015;181(12):979–988. doi: 10.1093/aje/kwu461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Cancer Institute. Usual Dietary Intakes: Food Intakes, U.S. Population, 2007–10. Epidemiology Research Program Web site. 2015 May 20; Updated. [Google Scholar]
- 9.Boffetta PCE, Wichmann J, Ferrari P, et al. Fruit and vegetable intake and overall cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) J Natl Cancer Inst. 2010;102(8):529–537. doi: 10.1093/jnci/djq072. [DOI] [PubMed] [Google Scholar]
- 10.Bellavia ALS, Bottai M, Wolk A, Orsini N. Fruit and vegetable consumption and all-cause mortality: a dose-response analysis. Am J Clin Nutr. 2013;98(2):454–459. doi: 10.3945/ajcn.112.056119. [DOI] [PubMed] [Google Scholar]
- 11.Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. doi: 10.1136/bmj.g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hung HCJK, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Colditz GA, Rosner B, Spiegelman D, Willett WC. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96(21):1577–1584. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 13.Dauchet LAP, Dallongeville J. Fruits, vegetables and coronary heart disease. Nat Rev Cardiol. 2009;6(9):599–608. doi: 10.1038/nrcardio.2009.131. [DOI] [PubMed] [Google Scholar]
- 14.Hu DHJ, Wang Y, Zhang D, Qu Y. Fruits and Vegetables Consumption and Risk of Stroke: A Meta-Analysis of Prospective Cohort Studies. Stroke. 2014;45:1613–1619. doi: 10.1161/STROKEAHA.114.004836. [DOI] [PubMed] [Google Scholar]
- 15.He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21(9):717–728. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- 16.Stackelberg O, Bjorck M, Larsson SC, Orsini N, Wolk A. Fruit and vegetable consumption with risk of abdominal aortic aneurysm. Circulation. 2013;128(8):795–802. doi: 10.1161/CIRCULATIONAHA.112.000728. [DOI] [PubMed] [Google Scholar]
- 17.Brostow DPHA, Collins TC, Kurzer MS. The role of nutrition and body composition in peripheral arterial disease. Nat Rev Cardiol. 2012;9:634–643. doi: 10.1038/nrcardio.2012.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz-Canela M, Estruch R, Corella D, Salas-Salvado J, Martinez-Gonzalez MA. Association of Mediterranean diet with peripheral artery disease: the PREDIMED randomized trial. JAMA. 2014;311(4):415–417. doi: 10.1001/jama.2013.280618. [DOI] [PubMed] [Google Scholar]
- 19.Savji NRC, Skolnick AH, Guo Y, Adelman MA, Riles T, Berger JS. Association between advanced age and vascular disease in different arterial territories: a population database of over 3.6 million subjects. J Am Coll Cardiol. 2013;61(16):1736–1743. doi: 10.1016/j.jacc.2013.01.054. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Chronic Disease Prevention and Health Promotion and Department of Nutrition, Physical Activity, and Obesity. State Indicator Report on Fruits and Vegetables. 2013:1–16. [Google Scholar]
- 21.Patterson BH, Block G, Rosenberger WF, Pee D, Kahle LL. Fruit and vegetables in the American diet: data from the NHANES II survey. Am J Public Health. 1990;80(12):1443–1449. doi: 10.2105/ajph.80.12.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rekhy R, McConchie R. Promoting consumption of fruit and vegetables for better health. Have campaigns delivered on the goals? Appetite. 2014;79:113–123. doi: 10.1016/j.appet.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 23.Thomson CA, Ravia J. A systematic review of behavioral interventions to promote intake of fruit and vegetables. J Am Diet Assoc. 2011;111(10):1523–1535. doi: 10.1016/j.jada.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 24.Klipstein-Grobusch K, den Breeijen JH, Grobbee DE, Boeing H, Hofman A, Witteman JC. Dietary antioxidants and peripheral arterial disease: the Rotterdam Study. Am J Epidemiol. 2001;154(2):145–149. doi: 10.1093/aje/154.2.145. [DOI] [PubMed] [Google Scholar]
- 25.Lane JS, Magno CP, Lane KT, Chan T, Hoyt DB, Greenfield S. Nutrition impacts the prevalence of peripheral arterial disease in the United States. J Vasc Surg. 2008;48(4):897–904. doi: 10.1016/j.jvs.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 26.Wilmink AB, Welch AA, Quick CR, Burns PJ, Hubbard CS, Bradbury AW, Day NE. Dietary folate and vitamin B6 are independent predictors of peripheral arterial occlusive disease. J Vasc Surg. 2004;39(3):513–516. doi: 10.1016/j.jvs.2003.09.046. [DOI] [PubMed] [Google Scholar]
- 27.Tornwall ME, Virtamo J, Haukka JK, Aro A, Albanes D, Huttunen JK. Prospective study of diet, lifestyle, and intermittent claudication in male smokers. Am J Epidemiol. 2000;151(9):892–901. doi: 10.1093/oxfordjournals.aje.a010293. [DOI] [PubMed] [Google Scholar]
- 28.Hung HCMA, Willett W, Ascherio A, Rosner BA, Rimm E, Joshipura KJ. The association between fruit and vegetable consumption and peripheral arterial disease. Epidemiology. 2003;14:659–665. doi: 10.1097/01.ede.0000086882.59112.9d. [DOI] [PubMed] [Google Scholar]
- 29.Donnan PT, Thomson M, Fowkes FG, Prescott RJ, Housley E. Diet as a risk factor for peripheral arterial disease in the general population: the Edinburgh Artery Study. Am J Clin Nutr. 1993;57:917–921. doi: 10.1093/ajcn/57.6.917. [DOI] [PubMed] [Google Scholar]
- 30.Voko Z, Hollander M, Hofman A, Koudstaal PJ, Breteler MM. Dietary antioxidants and the risk of ischemic stroke: the Rotterdam Study. Neurology. 2003;61:1273–1275. doi: 10.1212/01.wnl.0000090458.67821.a3. [DOI] [PubMed] [Google Scholar]
- 31.Violi F, Loffredo L, Marcoccia A. Antioxidants in peripheral arterial disease. Curr Drug Targets Cardiovasc Haematol Disord. 2004;4:289–294. doi: 10.2174/1568006043336212. [DOI] [PubMed] [Google Scholar]
- 32.Spadafranca A, Bertoli S, Fiorillo G, Testolin G, Battezzati A. Circulating salicylic acid is related to fruit and vegetable consumption in healthy subjects. Br J Nutr. 2007;98:802–806. doi: 10.1017/S0007114507744422. [DOI] [PubMed] [Google Scholar]
- 33.John JH, Ziebland S, Yudkin P, Roe LS, Neil HA. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomised controlled trial. Lancet. 2002;359(9322):1969–1974. doi: 10.1016/s0140-6736(02)98858-6. [DOI] [PubMed] [Google Scholar]
- 34.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 35.Hartley L, Igbinedion E, Holmes J, Flowers N, Thorogood M, Clarke A, Stranges S, Hooper L, Rees K. Increased consumption of fruit and vegetables for the primary prevention of cardiovascular diseases. Cochrane Database Syst Rev. 2013;6:Cd009874. doi: 10.1002/14651858.CD009874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tohill BC, Seymour J, Serdula M, Kettel-Khan L, Rolls BJ. What epidemiologic studies tell us about the relationship between fruit and vegetable consumption and body weight. Nutr Rev. 2004;62(10):365–374. doi: 10.1111/j.1753-4887.2004.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 37.Ledoux TA, Hingle MD, Baranowski T. Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev. 2011;12(5):e143–150. doi: 10.1111/j.1467-789X.2010.00786.x. [DOI] [PubMed] [Google Scholar]
- 38.Mytton OT, Nnoaham K, Eyles H, Scarborough P, Ni Mhurchu C. Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health. 2014;14:886. doi: 10.1186/1471-2458-14-886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ashfield-Watt PA, Welch AA, Day NE, Bingham SA. Is ‘five-a-day’ an effective way of increasing fruit and vegetable intakes? Public Health Nutr. 2004;7:257–261. doi: 10.1079/PHN2003524. [DOI] [PubMed] [Google Scholar]
- 40.Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 41.Xu D, Zou L, Xing Y, Hou L, Wei Y, Zhang J, Qiao Y, Hu D, Xu Y, Li J, Ma Y. Diagnostic value of ankle-brachial index in peripheral arterial disease: a meta-analysis. Can J Cardiol. 2013;29:492–498. doi: 10.1016/j.cjca.2012.06.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


