Abstract
Objective
To describe the characteristics of children seeking emergency care for firearm injuries within the PECARN network, and assess the influence of both individual and neighborhood factors on firearm-related injury risk.
Methods
This was a retrospective, multicenter cross-sectional analysis of children (<19-years-old) presenting to 16 pediatric EDs (2004–2008). ICD-9-CM E-codes were used to identify and categorize firearm injuries by mechanism/intent. Neighborhood variables were derived from home address data. Multivariable analysis examined the influence of individual and neighborhood factors on firearm-related injuries as compared to non-firearm ED visits. Injury recidivism was assessed.
Results
1,758 pediatric ED visits for firearm-related injuries were analyzed. Assault (51.4%, n=904) and unintentional injury (33.2%, n=584) were the most common injury mechanisms. Among children with firearm injuries, 68.3% were older adolescents (15–19 years-old), 82.3% male, 68.2% African-American, and 76.3% received public insurance/were uninsured. Extremity injuries were most common (75.9%), with 20% sustaining injuries to multiple body regions, 48.1% requiring admission, and 1% ED mortality. Multivariable analysis identified firearm injury risk factors, including adolescent age (p<0.001), male gender (p<0.001), non-Caucasian race/ethnicity (p<0.001), public payer/uninsured status (p<0.001), and higher levels of neighborhood disadvantage (p<0.001). Among children with firearm injuries, 12-month ED recidivism for any reason was 22.4%, with <1% returning for another firearm injury.
Conclusion
Among children receiving ED treatment within the PECARN network, there are distinct demographic and neighborhood factors associated with firearm injuries. Among younger children (<10 years old), unintentional injuries predominate, while assault-type injuries were most common among older adolescents. Overall, among this PECARN patient population, male adolescents living in neighborhoods characterized by high-levels of concentrated disadvantage had an elevated risk for firearm injury. Public health efforts should focus on developing and implementing initiatives addressing risk factors at both the individual and community level, including ED-based interventions to reduce the risk for firearm injuries among high-risk pediatric populations.
Keywords: Firearm Injury, Pediatric Emergency Department, Youth
INTRODUCTION
Despite comparable overall rates for suicide and non-lethal violence, the U.S. continues to have the highest pediatric firearm fatality rate of all high-income, industrialized nations.1,2 In 2013, firearm-related injuries were the 2nd leading cause of death among U.S. children (0–19 years old), responsible for 2,396 fatalities nationwide.3 Firearms are responsible for nearly 20% of all fatal injuries among children in the United States.3,4 Among older youth (15–19 years old), firearms are responsible for as many as 25% of all deaths annually, disproportionately affecting African-American children,3,4 where firearm homicide has been the leading cause of death for over a decade.3 Despite a decline since peaking in 1994, pediatric firearm fatality rates in the United States (3.27 deaths/100,000) have remained unchanged since 2003, and current firearm fatality rates have surpassed rates for the leading cause of death among children, motor vehicle crash injury, in six states.3
While population-based epidemiological data5 has provided insight into the burden of fatal firearm injuries, less research has focused on non-fatal firearm injures among pediatric patients receiving emergency department (ED) treatment. Non-fatal firearm injuries among adolescents occur at a rate three times that of the general population3,6 and over 12,000 children were injured seriously enough by firearm injuries to require ED treatment in 2012.3,6,7 The long-term morbidity resulting from such injuries is substantial, with nearly 50% of all children hospitalized after a firearm injury sustaining a long-term disability requiring rehabilitative care.8 The economic costs associated with firearm-related injuries is high, with 2010 cost estimates for all U.S. firearm injuries approaching 174 billion dollars annually.9
Recent ED- and hospital-based research has focused on firearm injuries among higher risk subsamples, including assault-injured youth,10–13 injured children requiring hospital admission14,15 and those transported by emergency medical services (EMS) after a firearm injury.16 Only one prior ED-based study has examined the pediatric ED population as a whole; however, this study was limited by the narrow set of socio-demographic factors available in the dataset and the inability to examine subpopulations of injury by intent.17 Further, no recent epidemiological studies have examined the influence of neighborhood socio-economic factors on patterns of firearm-related injury or examined firearm injury recidivism among this population. Given the paucity of prior literature in this area, such data are critical to informing public health and ED-initiated injury prevention efforts among high-risk populations.
To address the current gaps in literature on non-fatal firearm injuries among children and to inform public health efforts, we examined a multicenter administrative database of pediatric ED visits compiled by the Pediatric Emergency Care Applied Research Network (PECARN). Primary study objectives were: 1) to describe the characteristics of children seeking emergency care for a firearm injury within the PECARN network; and, 2) to understand the relative influence of individual and neighborhood factors on the risks for pediatric firearm-related injuries.
METHODS
Study Design/Primary Data Source
This study analyzed secondary data collected as part of the PECARN core data project. The project annually collects and aggregates administrative data from participating network hospitals.18 The dataset has information, including a unique patient identifier, that allows for longitudinal tracking of patients. Analyses were conducted utilizing data from 2004–2008 as both clinical and home address data were available during this timeframe.
Hospital Settings
Sixteen PECARN hospitals were included. Hospital inclusion was based on the availability of administrative data for all study years (2004–2008), and the assignment of International Statistical Classification of Diseases 9th revision clinical modification (ICD-9-CM) E-codes to ≥80% of all injury-related visits (i.e., ICD-9-CM Codes 800-995.9).19 Of the 16 pediatric EDs included in this analysis, 8 are freestanding children’s hospital EDs, 6 are separate pediatric EDs within a general ED, and two are general EDs where providers deliver care to adults and children. EDs included in this analysis are concentrated in the Midwest (n=6), mid-Atlantic (n=5), and northeast (n=3) with two hospitals located in the western US. Annual ED census at sites ranges from 10,437 to 84,301. Of the 16 sites, twelve are recognized as Level-1 pediatric trauma centers by either the American College of Surgeons or regional designation.
Case Definition
Eligible patients included all patients <19 years-old seeking ED care at one of the 16 hospitals. Patient visit type was identified using ICD-9-CM diagnostic codes.19 Firearm injuries, consistent with the CDC case definition20,21 were defined as any gunshot wound or penetrating injury from a weapon using a powder discharge to fire a projectile. This included firearm injuries resulting from handguns, hunting rifles, military firearms, and shotguns, but excluded those from air-powered BB, pellet-type guns and paint guns. For this analysis, firearm injuries were identified and classified based on having one of the following injury related ICD-9-CM/E-codes: 1) Intentional firearm assaults (E965.0–E965.4; E979.4); 2) Self-inflicted firearm injuries (E955.0–E955.4); 3) Unintentional firearm injuries (E922.0–E922.3; E922.8–E922.9), or 4) Undetermined firearm injuries (E985.0–E985.4). Firearm injuries resulting from legal intervention/war (E970; E991) were excluded due to small sample size (n=13). Of note, data on children who suffered a fatal firearm injury during the pre-hospital period is not captured within this hospital-based administrative dataset. Firearm type (handgun, shotgun, hunting rifle, military firearm, unspecified/other) was characterized from e-code data where available. Non-firearm related pediatric ED visits at the study hospitals served as the comparison group.
Individual Level Variables
Individual level data elements included demographics (age, race/ethnicity, gender) and insurance status (private payer, public payer, uninsured/other). Age was grouped as 0–4, 5–9, 10–14 and 15–19 years of age.14 Race/ethnicity was classified as African-American/Non-Hispanic, White/Non-Hispanic, Hispanic, or other. The other race/ethnicity category included American Indian/Alaskan Native, Asian American, and Native Hawaiian or Other Pacific Islanders.
Neighborhood Level Variables
Neighborhood level variables were derived using patient home address and corresponding census tract data from the 2000 U.S. census survey.22 Rurality was determined using zip codes, which were mapped to their corresponding rural-urban continuum code (RUCC) as defined at each decennial census. RUCCs are defined on a nine point scale and consistent with prior literature were collapsed as: 1) Metropolitan (RUCC 1–3; metropolitan areas with >250,000 people), 2) Urban non-metropolitan (RUCC 4–7; urban settings >2,500 people), and 3) Rural (RUCC 8–9; rural setting <2,500 people).23 As has been done in prior work24 and consistent with a concentrated neighborhood disadvantage measure constructed by Sampson et al,25 four neighborhood measures within the 2000 census tract data were also examined, including: 1) neighborhood poverty (defined as the % of households <150% of the poverty level); 2) the proportion of vacant housing units; 3) the proportion of female head of households; and 4) the proportion of African-American/Non-Hispanic households. The four variables were combined and standardized using principal component analysis to create a single continuous measure of neighborhood disadvantage [range 0–188] in which greater values represented more concentrated neighborhood disadvantage. Other important census-based measures previously identified by Sampson et al.,25 including public assistance, unemployment, and the number of children (<18 years-old) per household, were unavailable in the 2000 census and thus were unable to be included.
ED Visit Characteristics/Patient Outcomes
ED visit characteristics included mode of arrival (EMS/Walk-in/Other), hospital trauma center status, and ED length of stay. Length of stay (LOS) was calculated (in minutes) by subtracting the ED triage time from the ED discharge time and was capped at 24 hours (i.e., 1,440-min). Injury severity scores (ISS)26 were calculated using the sum of the squares of the three most severely injured body regions as determined by the abbreviated injury scale (AIS), an ordinal scale of injury severity ranging from 1 (minor) to 6 (not survivable). Maximal AIS severity scores for each body region (head, neck, face, thorax, spine, upper extremity, lower extremity, external/other) were derived by mapping ICD-9-CM codes associated with each visit to the corresponding AIS codes (1998 version) using ICDMAP-90 software. These codes were then manually revised to be consistent with the updated AIS 2005 and 2008 versions.27–29 A maximal AIS of 6 in any body region defaulted to an ISS=75. ED visit outcome was categorized as admit/transferred, death, discharged/left against medical advice, and other.
Data Analysis
Among the PECARN dataset, 56% of cases had complete data for all individual and neighborhood level variables. Among those cases with missing data, 78% were missing data for two variables or less among all of the individual, ED-visit, or neighborhood level variables examined. Multiple imputation using chained regressions was used to populate missing individual-level and ED visit measures.30–32 However, due to an inability to perform imputation for neighborhood level variables, those cases with missing neighborhood data (<10%) were excluded from bivariate and multivariable analyses. Descriptive statistics were calculated and compared by intent/mechanism of injury. Bivariate analyses compared unadjusted individual and neighborhood characteristics for patients presenting for a firearm-related injury to those of patients seeking care for non-firearm related reasons. Multivariable log-binomial regression was utilized to identify those individual and neighborhood factors associated with an increased likelihood of firearm injury as compared to patients presenting for other reasons. Parameters within the final model were chosen based on significance in the bivariate comparisons and included age, gender, race/ethnicity, insurance status, and neighborhood disadvantage. Finally, LinkSolv software was utilized to conduct probabilistic linkage and identify multiple ED visits for the same patient within and across PECARN hospitals for the 12-months preceding and following the index firearm injury visit. Return visits within 72 hours of the initial ED visit for a firearm injury were excluded from the recidivism analysis as these visits were presumed to be related to the initial firearm injury. Given the limitations of the database, preceding and return visits were limited to those available in the 2004–2008 study period. The database was managed and analyses were conducted using SAS (version 9.2, SAS Institute Inc., Cary, NC).
RESULTS
Sample Characteristics
A total of 1,758 ED visits for a firearm injury occurred among children (<19 years-old) at a PECARN study hospital (n=16) during the five-year study period (2004–2008). Among these ED visits, 93.4% (n=1,642) of children were between 10 and 18 years-old, 82.3% (n=1,447) were male, 68.2% (n=1,199) were African-American, 60.8% of cases arrived via ambulance (air/ground), and 86.7% were cared for in a Level-1 trauma center.
Among pediatric ED visits for firearm injuries (n=1,758), 9% (n=159) were missing home address data and were excluded from the descriptive and comparative neighborhood analyses (leaving n=1,599 for bivariate/multivariable analyses). Those children missing address data were noted to be slightly older [median age, IQR: 16 y/o (15; 17) vs. 15 y/o (14, 17), p=0.03] and were more likely to be male [89%-vs.-82%, p=0.03]. No significant differences were noted among those with and without address data with regards to race/ethnicity or insurance status.
Firearm Injuries at PECARN Hospitals
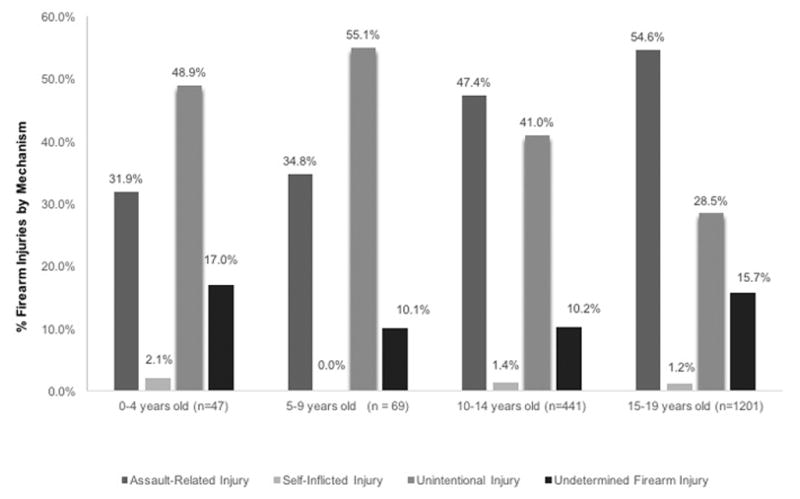
Table 1 provides descriptive characteristics for all ED visits among children evaluated for a firearm injury (n=1,758), with 51.4% (n=904) resulting from an intentional assault, 33.2% (n=584) from an unintentional injury, and 1.2% (n=21) from a self-inflicted injury. The method of injury for the remaining 14.2% (n=249) was unable to be determined from ICD-9-CM coding. Differences between method of firearm injury by age is presented in Figure 1 (p < 0.001), with unintentional injury most common among children <10 years old when compared with assault and self-inflicted type injuries. Among older youth (10–18 years-old), assault-type injuries were most common when compared with other mechanisms of injury. Children sustaining firearm assaults, unintentional type injuries, or undetermined injuries were more likely African-American than other races/ethnicities (p < 0.001). While numbers of self-inflicted injures were too small to characterize statistically, Caucasian children comprised the majority of those with self-inflicted firearm injuries when compared with other races/ethnicities. Among children sustaining a firearm injury, 63.3% were insured by a public payer, 23.7% by private insurance and 13.0% by self-pay/other forms of insurance. Children sustaining firearm assaults, unintentional firearm injuries, or those who had an undetermined type of firearm injury were more likely to have a public payer and/or be uninsured than have private insurance (p = 0.001). Among the small number of self-inflicted injuries, children were most likely to have private insurance (57.1%). Among those with available neighborhood data, 98.3% resided in a metropolitan setting. Neighborhood disadvantage was noted to be high among all firearm injury related mechanisms except those resulting from self-inflicted firearm injuries where neighborhood disadvantage was notably lower than other injury-related mechanisms (p < 0.001).
Table 1.
Descriptive characteristics of ED visits occurring among pediatric patients (<19 years-old) seeking emergency care at a PECARN study hospital for a firearm injury between 2004–2008
| Firearm Assault Injury (n = 904) | Self-inflicted Firearm Injury (n = 21) | Unintentional Firearm Injury (n = 584) | Undetermined Firearm Injury (n = 249) | |
|---|---|---|---|---|
|
| ||||
|
Individual Characteristics
| ||||
| Age (mean, sd) | 15.2 (2.9) | 14.7 (3.2) | 14.0 (3.6) | 15.1 (3.0) |
|
| ||||
| Gender (n, % male) | 735 (81.3) | 15 (71.4) | 485 (83.1) | 212 (85.1) |
|
| ||||
| Race/Ethnicity (n, %) | ||||
| African-American | 604 (66.8) | 4 (19.0) | 383 (65.6) | 208 (11.9) |
| Caucasian | 77 (8.6) | 10 (47.6) | 112 (19.2) | 14 (5.5) |
| Hispanic | 93 (10.3) | 4 (19.0) | 37 (6.3) | 11 (4.6) |
| Other, Non-Hispanic | 130 (14.4) | 3 (15.2) | 52 (8.9) | 16 (6.4) |
|
| ||||
| Insurance Type (n, %) | ||||
| Private Payer | 185 (20.5) | 12 (57.1) | 161 (27.6) | 58 (23.3) |
| Public Payer | 605 (66.9) | 7 (33.3) | 341 (58.4) | 160 (64.3) |
| Other/Uninsured | 114 (12.6) | 2 (9.5) | 82 (14.0) | 31 (12.4) |
|
| ||||
|
Medical Visit Characteristics
| ||||
| Mode of Arrival (n, %) | ||||
| EMS Air/Ground | 554 (61.3) | 17 (81.0) | 333 (57.0) | 164 (65.9) |
| Non-EMS/Walk-in | 342 (37.8) | 4 (19.0) | 244 (41.8) | 80 (32.1) |
| Other | 8 (0.9) | 0 (0.0) | 7 (1.2) | 5 (2.0) |
|
| ||||
| Disposition (n, %) | ||||
| Admit/Transfer | 438 (48.5) | 16 (76.2) | 254 (43.5) | 141 (56.6) |
| Death | 11 (1.2) | 1 (4.8) | 4 (0.7) | 2 (0.8) |
| Discharged/AMA | 451 (49.9) | 4 (19.0) | 316 (54.1) | 103 (41.4) |
| Other | 4 (0.4) | 0 (0.0) | 10 (1.7) | 3 (1.2) |
|
| ||||
| Trauma Center (n, %) | 729 (80.6) | 20 (95.2) | 546 (93.5) | 229 (92.0) |
|
| ||||
| ED LOS (mean, sd) | 280.1 (316.0) | 508.6 (557.0) | 278.7 (341.5) | 220.2 (209.5) |
|
| ||||
| ISS (median, IQR) | 1 (1, 5) | 1 (1, 125) | 1 (1, 4) | 1 (1, 4) |
| Range (excluding 99) | 0, 75 | 0, 29 | 0, 75 | 0, 26 |
|
| ||||
|
Neighborhood Characteristics
| ||||
| (n = 824) | (n = 17) | (n = 531) | (n = 227) | |
|
| ||||
| Poverty (mean %, SD) | 39.0 (12.4) | 16.7 (12.4) | 36.7 (17.6) | 41.0 (17.5) |
|
| ||||
| Vacant Units (mean %, SD) | 10.3 (6.9) | 6.3 (6.1) | 11.3 (7.2) | 10.7 (5.9) |
|
| ||||
| Female Head of Household (mean %, SD) | 28.8 (12.5) | 12.6 (9.7) | 27.1 (13.1) | 12.5 (13.0) |
|
| ||||
| African-American/Non-Hispanic (mean %, SD) | 54.0 (36.7) | 10.5 (21.9) | 52.0 (37.7) | 64.6 (32.6) |
|
| ||||
| Neighborhood Disadvantage Index | 73.0 (31.4) | 27.9 (20.6) | 70.1 (33.9) | 80.9 (31.2) |
|
| ||||
| Rurality (n, %) | ||||
| Metropolitan | 821 (99.6) | 14 (82.4) | 511 (96.2) | 226 (99.6) |
| Urban, Non-Metro | 3 (0.4) | 3 (17.7) | 19 (3.6) | 1 (0.4) |
| Rural | 0 (0.0) | 0 (0.0) | 1 (0.2) | (0.0) |
Note: ED: Emergency Department; EMS: Emergency Medical Services; AMA: Against Medical Advice; LOS: Length of Stay; ISS: Injury Severity Score; IQR: Inner Quartile Range
Figure 1.
Among all children with firearm injuries, 18.6% had been seen and treated in the same ED for a medical or injury-related complaint during the preceding 12-months, with rates of preceding ED visits highest among those that eventually sought care for firearm assault (32.1%) as compared with other firearm injury mechanisms (p=0.001). Rates of visits within the proceeding 12-months for self-inflicted firearm injuries and unintentional firearm injuries were 0.2% and 7.9%, respectively.
While weapon type was unknown or unable to be determined in most cases (n=1,253; 71.3%), among those cases where firearm type was identified (n=505), handguns were the most common cause of firearm injury (n=366, 72.5%, 95% CI 70.4%, 74.6%).
Emergency Department Outcomes and Recidivism
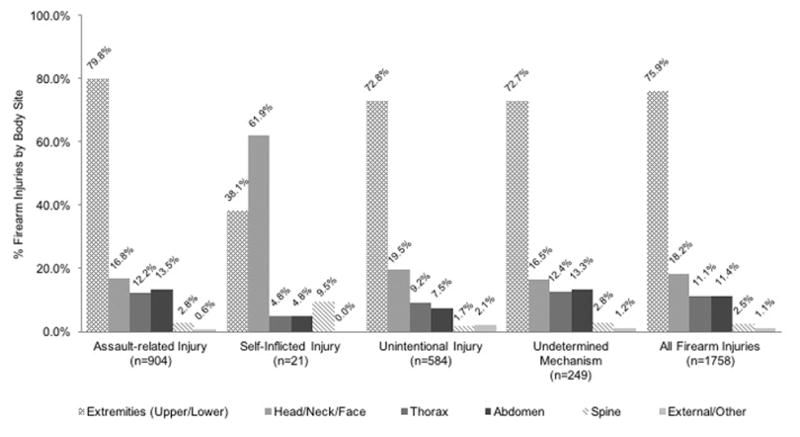
Among firearm injury visits, almost half (48.3%; n=849) of children suffered injuries severe enough to require hospital admission, with the highest admission rates noted among those with self-inflicted injuries when compared with the admission rates of other firearm-related injury mechanisms (p < 0.001). ED mortality following a firearm injury was 1% (n=18). Overall, 75.9% of children with firearm injuries sustained an extremity injury, 22.5% a thoraco-abdominal injury, 18.2% a head/neck or face injury, and 2.5% a spinal injury (Figure 2). The distribution of firearm injuries by body region was similar among those with assault, unintentional and undetermined injuries. In contrast, among those with self-inflicted injuries (Figure 2), head and neck injuries were the predominant injury type.
Figure 2.
Among children with firearm injuries, 22.4% (n=385) returned within the next 12-months for an ED visit for any reason (average number of ED visits=1.6), with <1% of the sample (n=13) returning for a second firearm injury, the majority among those sustaining an assault-injury (n=6) or unintentional firearm injury (n=7) at the index visit.
Multivariable Analysis
Table 2 presents the results of the unadjusted bivariate analysis comparing firearm-related injury visits to non-firearm related ED visits. Children with firearm injuries were more likely to be older (p<0.001), of non-Caucasian race/ethnicity (p<0.001) and were more likely covered by a public payer (p<0.001). Further, children sustaining firearm-related injuries were more likely to be from neighborhoods with higher level of socio-economic disadvantage (p<0.001). In the multivariable regression model, male gender, minority race/ethnicity, older aged youth and higher neighborhood disadvantage were found to be associated with increased risk of a firearm-related injury visit (Table 3).
Table 2.
Unadjusted bivariate comparison of individual and neighborhood characteristics of pediatric patients (< 19 years old) with a firearm injury as compared to a non-firearm related ED diagnosis at a PECARN study hospital, 2004–2008.
| Firearm-related ED visits (n = 1,599) | Non-firearm ED visits (n = 2,833,345) | RR (95% CI) | |
|---|---|---|---|
|
| |||
|
Individual Characteristics
| |||
| Age Group (n, %) | |||
| 0 – 4*** | 42 (2.6) | 1,478,240 (52.2) | Ref |
| 5 – 9*** | 66 (4.1) | 550,687 (19.4) | 4.2 (2.9, 6.2) |
| 10–14*** | 414 (25.9) | 456,016 (16.1) | 31.9 (23.2, 43.9) |
| 15 – 18*** | 1,077 (67.4) | 348,402 (12.3) | 108.5 (79.7, 147.6) |
|
| |||
| Male Gender (n, %)*** | 1,306 (81.7) | 1,520,076 (53.7)) | 3.9 (3.4, 4.4) |
|
| |||
| Race (n, %) | |||
| Caucasian | 192 (12.0) | 995,897 (35.2) | Ref |
| African-American*** | 1,103 (69.0) | 1,203,008 (42.5) | 4.8 (3.9, 5.8) |
| Hispanic ** | 126 (7.9) | 448,088 (15.8) | 1.5 (1.1, 1.9) |
| Other, Non-Hispanic*** | 178 (11.1) | 186,353 (6.6) | 5.0 (3.7, 6.6) |
|
| |||
| Public Payer (n, %) | |||
| Private Payer | 376 (23.5) | 1,011,791 (35.7) | Ref |
| Public Payer*** | 1,019 (63.7) | 1,633,911 (57.6) | 1.7 (1.5,1.9) |
| Other/Uninsured*** | 204 (12.8) | 187,643 (6.6) | 2.9 (2.4,3.5) |
|
| |||
|
Neighborhood Characteristics
| |||
| Metropolitan (n, %) | 1,572 (98.3) | 2,780,630 (98.1) | 0.9 (0.6, 1.3) |
|
| |||
| Poverty (mean %, SD)*** | 38.3 (17.1) | 27.0 (18.0) | 1.37 (1.34, 1.40) |
|
| |||
| Vacant Housing Units (mean %, SD)*** | 10.6 (6.9) | 8.4 (6.9) | 1.44 (1.36, 1.52) |
|
| |||
| Female Head of Household (mean %, SD)*** | 28.6 (12.9) | 20.5 (12.4) | 1.55 (1.50, 1.60) |
|
| |||
| Black/Non-Hispanic (mean %, SD)*** | 54.4 (36.9) | 34.8 (36.2) | 1.15 (1.13, 1.16) |
|
| |||
| Neighborhood Disadvantage Index*** | 72.7 (32.6) | 50.7 (33.6) | 1.19 (1.17, 1.21) |
p<0.05
p<0.01
p<0.001
Note: The RR calculation for the Neighborhood Disadvantage Index is based on a 10 point change in the index scale.
Table 3.
Multivariable model examining individual and neighborhood characteristics predicting a pediatric (<19 years old) ED visit for a firearm related injury at a PECARN study hospital, 2004–2008. (n=1599)
| Socio-demographic Risk Factor | Relative Risk (95% CI) |
|---|---|
| Age | |
| 0 – 10 | Ref |
| 11 – 14*** | 16.8 (13.8, 20.4) |
| 15 – 18*** | 54.6 (45.7, 65.3) |
| Male Gender*** | 5.2 (4.5, 5.9) |
| Race | |
| White | Ref |
| Black*** | 2.5 (2.0, 3.2) |
| Hispanic** | 1.6 (1.2, 2.1) |
| Other, Non-Hispanic*** | 4.9 (3.7, 6.7) |
| Payer | |
| Private | Ref |
| Public*** | 1.4 (1.2, 1.6) |
| Other/Uninsured*** | 1.9 (1.6, 2.4) |
| Neighborhood Disadvantage Index*** | 1.11 (1.09, 1.13) |
p<0.05
p<0.01
p<0.001
Note: The RR calculation for the Neighborhood Disadvantage Index is based on a 10 point change in the index scale.
DISCUSSION
While the overall incidence of firearm injuries has declined since the early 1990s, little additional progress has been made in over a decade and firearm injuries remain a leading preventable cause of pediatric morbidly and mortality. Recent epidemiological research14,16,17,33 has focused on defining the incidence and trends in firearm-related injuries among children to better understand the characteristics of such injuries and to inform injury prevention efforts. Our multisite study adds to the literature as it is one of the largest studies to date to describe the characteristics of children with firearm injuries, especially those sustaining non-fatal firearm injuries, and it is the first to examine the relative influence of individual and neighborhood factors on firearm injury risk among a cohort of children seeking ED care.
Our data highlight several findings important to ED-based public health efforts. First, study data demonstrate that children presenting to pediatric EDs with firearm injuries are a diverse and heterogeneous population, with injury mechanisms that vary by age and sex. While assault-type injuries were the most common firearm injury observed among adolescents, unintentional injuries were the most common injury among younger children (<10 years-old) in our sample. Prior research highlights that 38% of U.S. households with children have a firearm,34 with 43% reporting that the firearm is stored unlocked.35 This, combined with research demonstrating that children as young as 3–4 years of age are strong enough to pull a trigger36 and that as many as half of unintentional firearm injuries result from a child finding and playing with a loaded firearm in the home,37 underscores the need for better prevention efforts addressing firearm access, especially among younger populations. Further, while similar to prior studies,14,38,39 male sex was overwhelmingly associated with firearm injuries, especially assault-type and unintentional injuries, it is important to note that 20–30% of the children in our sample were female, highlighting the need to develop tailored ED- and public health interventions that can be applied to both sexes.
While self-inflicted injuries were the least common firearm injury in our sample, they were noted to have the highest rates of hospital admission and ED mortality. This is consistent with prior literature demonstrating the high case fatality rate associated with self-inflicted firearm injuries.40 Prior literature has highlighted the importance of restricting lethal means access among at-risk teens and has identified that safe firearm storage can be an effective means of preventing unintentional firearm shootings and suicide attempts among children.41 Physician counseling and anticipatory guidance have also been shown to be effective increasing safe storage practices,41–43 with one prior study finding that 64% of parents made safer firearm storage changes after receiving such counseling and 12% opted to remove a firearm from their home.44 In light of this, there is likely a larger role for physician-based counseling of at-risk youth in ED and primary care settings. It is important to note, however, that physician inquiries about firearm ownership have recently been restricted in several states.45 Although this limits the ability of physicians to focus counseling efforts among high-risk families that own firearms, physicians are still able to discuss safe firearm storage practices with all families as a universal safety measure (e.g., similar to seatbelts). Decreases in unintentional and self-inflicted firearm injuries have also been noted in states enacting child access prevention laws that impose criminal liability on adults negligently storing firearms.46–49 Given that over a third of the injuries in our sample resulted from unintentional or self-inflicted causes, expanding the role for public policies that address child access, research examining the effectiveness of technological interventions to improve firearm safety (e.g., smart guns), and addressing concerns about the role of focused physician counseling in routine practice, is critical to reducing the incidence of such injuries.
Our findings also highlight the substantial contribution that firearm injuries make to the problem of health disparities, both at the individual and neighborhood level. In our ED sample, minority adolescents were at the highest risk for firearm injuries, with most resulting from interpersonal violence. This is consistent with data demonstrating that firearm homicides are the leading cause of African-American youth mortality and that among African-American youth, firearm injuries occur at a rate eight times that of Caucasian youth.3,7 Such violence disparities are often attributed to multiple neighborhood-level factors, including poverty, neighborhood disorganization, family disruption, low economic opportunity, and a high concentration of firearms, especially illegal firearms.50–53 Consistent with this research, we found that children within our sample from communities with high levels of socio-economic disadvantage or those requiring Medicaid or lacking insurance (a proxy for socio-economic status) were at the highest risk for firearm injuries. Taken together, this suggests that while firearm injury prevention efforts should be applied universally, there must also be a particular focus on addressing the intentional violent injury risk that exists for minority adolescent populations in low-resource neighborhoods with high levels of community violence.
The finding that almost 20% of assault-injured youth were seen in the same ED within the preceding year highlights the opportunity for emergency physicians to engage in primary and secondary prevention efforts among these traditionally hard-to-reach youth. Further, recent studies highlighting the cyclical and chronic nature of intentional violence among urban youth,54,55 as well as our finding that 13 children sustaining a firearm assault-type injury in our sample suffered another firearm injury within the next 12 months highlights the potential utility of EDs incorporating violence prevention into standard medical practice. This is especially critical for the almost 50% of firearm assaults that are discharged from the ED and do not have access to in-patient hospital-based violence prevention and mental health services. Prior research has demonstrated the potential effectiveness of ED and hospital-based interventions that address violence-related factors (e.g., anger management, conflict resolution) along with co-occurring risk factors (e.g., substance use, PTSD) to decrease future violence risk and weapon-related behaviors.56–58 As the evidence base grows for such interventions, incorporating them into the standard-of-care for high-risk youth and linking them to on-going community interventions (e.g., CeaseFire, Safe Streets)59,60 may decrease the high rates of violence, as well as the health disparities, observed among high-risk ED populations.
It is important to note that over 20% of our sample sustained a head, neck or spinal injury, with the rates highest among children with self-inflicted firearm injuries. Such injuries underscore the impact that a firearm event can have on long-term health, as they are often neurologically devastating and in prior studies have been shown to have the highest association with long-term disability and rehabilitation costs.8 Further, 20% of the children within our sample sustained injuries to multiple body regions, with rates of polytrauma highest among youth with assault injuries. This finding, which is more often associated with high-force blunt motor vehicle crash trauma rather than assault injuries, may increase the complexity and duration of the acute treatment period.8 Over three quarters of the sample sustained an extremity wound. Such injuries are often associated with the need for multiple complex orthopedic surgeries61 and are associated with significant short-term disability, including the likelihood of decreased mobility at the time of hospital discharge and the need to modify routine activities of daily living.8 Cost data was not available in our dataset and further research is needed to characterize these acute and long-term costs. In addition, while medical care for firearm injuries has typically focused on the physical injury, more research is needed to develop the best practices to improve the long term mental health of children sustaining firearm injuries (e.g., PTSD), as well as to provide necessary services to family members.
Limitations should be noted. First, this is a secondary analysis using administrative data from PECARN EDs. Further, given that most PECARN hospitals are urban trauma centers in the Northeast, Midwest and Mid-Atlantic regions, findings may not generalize to community/rural settings. Second, study data is from 2004–2008 as this is when neighborhood data was available for the PECARN population; however, given the paucity of prior neighborhood-level data in prior studies and a lack significant changes to firearm-related mortality during the past ten years, findings are likely relevant to addressing current neighborhood factors on this topic. Third, no data was available on pre-hospital mortality. Prior research has identified that a third of children die at the scene,16 and thus our study likely underestimates the total burden of disease. Fourth, the small number of self-inflicted injuries limits conclusions about this injury type. In addition, the number of undetermined injuries (14%) in the sample limits a complete understanding of the underlying mechanisms characterizing firearm injuries in this population. Fifth, recidivism rates do not account for ED visits outside of PECARN or those among patients over 18. Thus, recidivism estimates likely underestimates the true incidence of repeat firearm injury. Finally, while multiple imputation, which has been shown to limit missing data bias,32,62–65 was utilized to address individual-level missing data, this was unable to be done for neighborhood data, potentially introducing bias.
CONCLUSION
This study offers insight into the burden of pediatric firearm injuries encountered in ED settings, the diversity of causes for such injuries, and the associated ramifications. ED physicians have a key responsibility within the medical system for identifying children who may be at-risk for firearm injuries and intervening with available prevention strategies, including behavioral counseling (e.g., safe storage) where appropriate, as well as referral to available community resources for at-risk youth. Many communities will have gunlocks and safe storage aids free to families and ED providers can encourage the dissemination of such resources to their at-risk patients. Finally, ED physicians can work within their professional organizations to promote greater research into effective prevention programs and can serve as advocates for implementing programs in their communities that help to improve firearm safety and safe storage, and reduce the burden of firearm injury among pediatric populations.
Acknowledgments
The authors wish to acknowledge Wendi Mohl for her assistance in manuscript preparation.
Abbreviations
- PECARN
Pediatric Emergency Care Applied Research Network
- ICD9
International Classification of Diseases, Ninth Revision, Clinical Modification
- E-code
External cause of Injury Code
- ISS
Injury Severity Score
- AIS
Abbreviated Injury Score
- PCDP
PECARN Core Data Project
- EMS
Emergency Medical Services
Footnotes
Prior Presentations: None
Funding Sources/Disclosures: This project is supported in part by the Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB), Emergency Medical Services for Children (EMSC) Network Development Demonstration Program under cooperative agreement number U03MC00008, and is partially support by MCHB cooperative agreements: U03MC00001, U03MC00003, U03MC00006, U03MC00007, U03MC22684 U03MC22685. In addition, this project was also supported, in part, by NIH/NIDA K23DA03934. The information, content, views and conclusions in the manuscript are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. Dr. Carter authored the first draft of this manuscript. No honoraria, grants or other form of payment were received from any of the co-authors for producing this manuscript.
References
- 1.Richardson EG, Hemenway D. Homicide, suicide, and unintentional firearm fatality: comparing the United States with other high-income countries, 2003. Journal of Trauma and Acute Care Surgery. 2011;70:238–43. doi: 10.1097/TA.0b013e3181dbaddf. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine of the National Academies. Priorities for research to reduce the threat of firearm-related violence. 2013 doi: 10.7205/MILMED-D-15-00568. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention and Control. [Accessed Sep 5, 2016];2015 at http://www.cdc.gov/injury/wisqars/index.html.
- 4.Dowd M, Sege R. Council on Injury, Violence, and Poison Prevention Executive Committee; American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2012;130:e1416–e23. doi: 10.1542/peds.2012-2481. [DOI] [PubMed] [Google Scholar]
- 5.Karch DL, Dahlberg LL, Patel N. Surveillance for violent deaths—National violent death reporting system, 16 States, 2007. MMWR Surveill Summ. 2010;59:1–50. [PubMed] [Google Scholar]
- 6.Martin CA, Unni P, Landman MP, et al. Race disparities in firearm injuries and outcomes among Tennessee children. Journal of pediatric surgery. 2012;47:1196–203. doi: 10.1016/j.jpedsurg.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 7.Pressley JC, Barlow B, Kendig T, Paneth-Pollak R. Twenty-year trends in fatal injuries to very young children: the persistence of racial disparities. Pediatrics. 2007;119:e875–84. doi: 10.1542/peds.2006-2412. [DOI] [PubMed] [Google Scholar]
- 8.DiScala C, Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics. 2004;113:1306–12. doi: 10.1542/peds.113.5.1306. [DOI] [PubMed] [Google Scholar]
- 9.Miller TR. The cost of firearm violence. Calverton, MD: Children’s Safety Network; 2012. [Google Scholar]
- 10.Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133:e96–e105. doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sege RD, Kharasch S, Perron C, et al. Pediatric violence-related injuries in Boston - Results of a city-wide emergency department surveillance program. Arch Pediat Adol Med. 2002;156:73–6. doi: 10.1001/archpedi.156.1.73. [DOI] [PubMed] [Google Scholar]
- 12.Cheng TL, Wright JL, Fields CB, et al. Violent injuries among adolescents: declining morbidity and mortality in an urban population. AnnEmergMed. 2001;37:292–300. doi: 10.1067/mem.2001.111763. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham RM, Murray R, Walton MA, et al. Prevalence of past year assault among inner-city Emergency Department patients. Ann Emerg Med. 2009;53:814–23. doi: 10.1016/j.annemergmed.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leventhal JM, Gaither JR, Sege R. Hospitalizations due to firearm injuries in children and adolescents. Pediatrics. 2014;133:219–25. doi: 10.1542/peds.2013-1809. [DOI] [PubMed] [Google Scholar]
- 15.Rowhani-Rahbar A, Zatzick D, Wang J, et al. Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: a cohort study. Annals of Internal Medicine. 2015;162:492–500. doi: 10.7326/M14-2362. [DOI] [PubMed] [Google Scholar]
- 16.Newgard CD, Kuppermann N, Holmes JF, et al. Gunshot injuries in children served by emergency services. Pediatrics. 2013;132:862–70. doi: 10.1542/peds.2013-1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Srinivasan S, Mannix R, Lee LK. Epidemiology of pediatric firearm injuries in the USA, 2001–2010. Archives of Disease in Childhood. 2014;99:331–5. doi: 10.1136/archdischild-2013-304642. [DOI] [PubMed] [Google Scholar]
- 18.Alpern ER, Stanley RM, Gorelick MH, et al. Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. PediatrEmergCare. 2006;22:689–99. doi: 10.1097/01.pec.0000236830.39194.c0. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization, Practice Management Information Corporation. ICD-9-CM: International Classification of Diseases, 9th Revision: Clinical Modification: PMIC, Practice Management Information Corporation. 1998. [Google Scholar]
- 20.Centers for Disease Control and Prevention. Recommended framework for presenting injury mortality data. MMWR: Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports/Centers for Disease Control. 1997;46:1–30. [PubMed] [Google Scholar]
- 21. [Accessed Nov 1, 2014];Matrix of ICD-9/iCD-9-CM E-code Groupings. at http://www.cdc.gov/injury/wisqars/ecode_matrix.html.
- 22.Census 2000 Gateway. 2002 at http://www.census.gov/main/www/cen2000.html.
- 23.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in US epidemiologic studies. Journal of Urban Health. 2006;83:162–75. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goldstick JE, Lipton RI, Carter P, et al. The effect of neighborhood context on the relationship between substance misuse and weapons aggression in urban adolescents seeking ED care. Substance Use & Misuse. 2015;50:674–84. doi: 10.3109/10826084.2014.998235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 26.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 27.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses: validation of an ICD-9CM to AIS-85 conversion table. Medical Care. 1989;27:412–22. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Durbin DR, Localio AR, MacKenzie EJ. Validation of the ICD/AIS MAP for pediatric use. Injury Prevention. 2001;7:96–9. doi: 10.1136/ip.7.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Association for the Advancement of Automotive Medicine. Abbreviated Injury Scale (AIS), 2005 Update. Des Plaines, Illinois: AAAM; 2008. [Google Scholar]
- 30.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–96. [Google Scholar]
- 31.Haukoos JS, Newgard CD. Advanced statistics: missing data in clinical research—part 1: an introduction and conceptual framework. AcadEmergMed. 2007;14:662–8. doi: 10.1197/j.aem.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 32.Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research—part 2: multiple imputation. AcadEmergMed. 2007;14:669–78. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 33.Hendry PL, Suen A, Kalynych CJ, Lott M, Paul J, Smotherman C. A 6-year retrospective review of pediatric firearm injuries: Do patients< 14 years of age differ from those 15–18 years of age? Journal of Trauma and Acute Care Surgery. 2014;77:S41–S5. doi: 10.1097/TA.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 34.Hepburn L, Miller M, Azrael D, Hemenway D. The US gun stock: results from the 2004 national firearms survey. Injury Prevention. 2007;13:15–9. doi: 10.1136/ip.2006.013607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schuster MA, Franke TM, Bastian AM, Sor S, Halfon N. Firearm storage patterns in US homes with children. AmJPublic Health. 2000;90:588. doi: 10.2105/ajph.90.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naureckas SM, Galanter C, Naureckas ET, Donovan M, Christoffel KK. Children’s and women’s ability to fire handguns. Arch Pediat Adol Med. 1995;149:1318–22. doi: 10.1001/archpedi.1995.02170250024003. [DOI] [PubMed] [Google Scholar]
- 37.Wintemute GJ, Teret SP, Kraus JF, Wright MA, Bradfield G. When children shoot children: 88 unintended deaths in California. JAMA. 1987;257:3107–9. doi: 10.1001/jama.257.22.3107. [DOI] [PubMed] [Google Scholar]
- 38.Eber GB, Annest JL, Mercy JA, Ryan GW. Nonfatal and fatal firearm-related injuries among children aged 14 years and younger: United States, 1993–2000. Pediatrics. 2004;113:1686–92. doi: 10.1542/peds.113.6.1686. [DOI] [PubMed] [Google Scholar]
- 39.Snyder AK, Chen LE, Foglia RP, Dillon PA, Minkes RK. An analysis of pediatric gunshot wounds treated at a level I pediatric trauma center. Journal of Trauma and Acute Care Surgery. 2003;54:1102–6. doi: 10.1097/01.TA.0000063479.92520.2E. [DOI] [PubMed] [Google Scholar]
- 40.Elnour AA, Harrison J. Lethality of suicide methods. Injury Prevention. 2008;14:39–45. doi: 10.1136/ip.2007.016246. [DOI] [PubMed] [Google Scholar]
- 41.Grossman DC, Stafford HA, Koepsell TD, Hill R, Retzer KD, Jones W. Improving firearm storage in Alaska native villages: a randomized trial of household gun cabinets. AmJPublic Health. 2012;102:S291–S7. doi: 10.2105/AJPH.2011.300421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barkin SL, Finch SA, Ip EH, et al. Is office-based counseling about media use, timeouts, and firearm storage effective? Results from a cluster-randomized, controlled trial. Pediatrics. 2008;122:e15–e25. doi: 10.1542/peds.2007-2611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McGee KS, Coyne-Beasley T, Johnson RM. Review of evaluations of educational approaches to promote safe storage of firearms. Injury Prevention. 2003;9:108–11. doi: 10.1136/ip.9.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Albright TL, Burge SK. Improving firearm storage habits: impact of brief office counseling by family physicians. The Journal of the American Board of Family Practice. 2003;16:40–6. doi: 10.3122/jabfm.16.1.40. [DOI] [PubMed] [Google Scholar]
- 45.Weinberger SE, Lawrence HC, III, Henley DE, Alden ER, Hoyt DB. Legislative interference with the patient–physician relationship. New England Journal of Medicine. 2012;367:1557–9. doi: 10.1056/NEJMsb1209858. [DOI] [PubMed] [Google Scholar]
- 46.Hepburn L, Azrael D, Miller M, Hemenway D. The effect of child access prevention laws on unintentional child firearm fatalities, 1979–2000. Journal of Trauma and Acute Care Surgery. 2006;61:423–8. doi: 10.1097/01.ta.0000226396.51850.fc. [DOI] [PubMed] [Google Scholar]
- 47.Becher EC, Christakis NA. Firearm injury prevention counseling: are we missing the mark? Pediatrics. 1999;104:530–5. doi: 10.1542/peds.104.3.530. [DOI] [PubMed] [Google Scholar]
- 48.Chapman S, Alpers P, Agho K, Jones M. Australia’s 1996 gun law reforms: faster falls in firearm deaths, firearm suicides, and a decade without mass shootings. Injury Prevention. 2006;12:365–72. doi: 10.1136/ip.2006.013714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Webster DW, Vernick JS, Zeoli AM, Manganello JA. Association between youth-focused firearm laws and youth suicides. Jama. 2004;292:594–601. doi: 10.1001/jama.292.5.594. [DOI] [PubMed] [Google Scholar]
- 50.Blumstein A. Youth, guns, and violent crime. The future of children. 2002:39–53. [PubMed] [Google Scholar]
- 51.Carter PM, Walton MA, Newton MF, et al. Firearm possession among adolescents presenting to an urban Emergency Department for assault. Pediatrics. 2013;132:213–21. doi: 10.1542/peds.2013-0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Office of the Surgeon General. Youth violence: A report of the Surgeon General. Rockville, MD: US Department of Health and Human Services; 2001. [PubMed] [Google Scholar]
- 53.Cunningham R, Knox L, Fein J, et al. Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009;53:490–500. doi: 10.1016/j.annemergmed.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 54.Cunningham RM, Carter PM, Ranney M, et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA pediatrics. 2015;169:63–70. doi: 10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carter PM, Walton MA, Roehler DR, et al. Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics. 2015;135:805–15. doi: 10.1542/peds.2014-3572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zatzick D, Russo J, Lord SP, et al. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial. JAMA pediatrics. 2014;168:532–9. doi: 10.1001/jamapediatrics.2013.4784. [DOI] [PubMed] [Google Scholar]
- 57.Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304:527–35. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cunningham RM, Chermack S, Zimmerman MA, et al. Brief Motivational Interviewing Intervention for Peer Violence and Alcohol Use in Teens: One Year Follow-up. Pediatrics. 2012;129:1083–90. doi: 10.1542/peds.2011-3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Braga AA, Kennedy DM, Waring EJ, Piehl AM. Problem-oriented policing, deterrence, and youth violence: An evaluation of Boston’s Operation Ceasefire. J Res Crime Delinq. 2001;38:195–225. [Google Scholar]
- 60.Webster DW, Whitehill JM, Vernick JS, Curriero FC. Effects of Baltimore’s safe streets program on gun violence: A replication of Chicago’s CeaseFire Program. Journal of Urban Health. 2013;90:27–40. doi: 10.1007/s11524-012-9731-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arslan H, Subasi M, Kesemenli C, Kapukaya A, Necmioğlu S, Kayıkçı C. Problem fractures associated with gunshot wounds in children. Injury. 2002;33:743–9. doi: 10.1016/s0020-1383(02)00122-5. [DOI] [PubMed] [Google Scholar]
- 62.van der Heijden GJ, Donders ART, Stijnen T, Moons KG. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: a clinical example. Journal of Clinical Epidemiology. 2006;59:1102–9. doi: 10.1016/j.jclinepi.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 63.Crawford SL, Tennstedt SL, McKinlay JB. A comparison of analytic methods for non-random missingness of outcome data. Journal of Clinical Epidemiology. 1995;48:209–19. doi: 10.1016/0895-4356(94)00124-9. [DOI] [PubMed] [Google Scholar]
- 64.Joseph L, Bélisle P, Tamim H, Sampalis JS. Selection bias found in interpreting analyses with missing data for the prehospital index for trauma. Journal of Clinical Epidemiology. 2004;57:147–53. doi: 10.1016/j.jclinepi.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 65.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. AcadEmergMed. 2006;13:314–24. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]


