To the Editor
The Centers for Disease Control (CDC) estimates that 37% of all antibiotic use in hospitals may be inappropriate, and reducing unnecessary antibiotic prescribing is now considered an urgent national priority.1,2 In the US alone, asthma exacerbations lead to 1.8 million Emergency Department (ED) visits, and 400,000 hospitalizations annually.3 Although guidelines recommend against prescribing antibiotics during exacerbations of asthma in the absence of concurrent infection, little is known about the use of antibiotics in routine clinical practice.4,5
Methods
We conducted a retrospective study of hospitalizations in 2013 and 2014 at 577 US hospitals that participate in the Premier Alliance database. Patients ≥ 18 years were included if they had a principal diagnosis of asthma (ICD-9-CM codes 493.0x, 493.1x 493.9x 493.2x, 493.8x, 493.9x) or a principal diagnosis of acute respiratory failure (ICD-9-CM codes 518.81, 518.82, 518.84) combined with a secondary diagnosis of asthma. We excluded patients with an admitting or discharge diagnosis of bronchitis, emphysema, chronic obstructive pulmonary disease, or bronchiectasis. We also excluded patients with potential indications for antibiotics, including those with admitting or present-on-admission (POA) discharge diagnoses of sinusitis, pneumonia, urinary tract infection, skin and soft tissue infection, septicemia or sepsis, or fever; those hospitalized for pneumonia within 3 months of the index admission, or in whom blood or sputum cultures were obtained.
For each patient, we assessed receipt, type and timing of antibiotic therapy, and for each hospital computed a facility-specific rate of antibiotic treatment. We developed a hierarchical logistic regression model to identify independent patient and hospital factors associated with antibiotic treatment. In sensitivity analysis we further restricted the cohort by excluding patients with a diagnosis of infection regardless of POA status, those 55 and older, and patients with a diagnosis of tobacco use.
Results
Among 51,951 cases, the median age was 52 years, 70% were female, and 46% identified as White. (Table) Antibiotics were prescribed on the first hospital day in 41% of cases, and at any point during the hospitalization in 58% of cases. Median duration of inpatient antibiotic treatment was 3 days. The most commonly prescribed antibiotics were macrolides (19%), quinolones (16%), 3rd generation cephalosporins (9%) and tetracyclines (4%). Treatment rates varied across hospitals. (Figure)
Table 1.
Characteristics of patients hospitalized for asthma and independent factors associated with receipt of antibiotic treatment.
| Included patients, % | Patients receiving antibiotics on day 1, % | p-value | Adjusted OR (95%CI) | |
|---|---|---|---|---|
| Overall | N=51951 | 41 | ||
|
| ||||
| Age | <0.01 | |||
|
| ||||
| <40 | 25 | 35 | 0.8 (0.7–0.8) | |
| 40–65 | 53 | 42 | 0.9 (0.9–1.0) | |
| >65 | 22 | 46 | ref | |
|
| ||||
| Gender | <0.01 | |||
|
| ||||
| Female | 70 | 41 | – | |
| Male | 30 | 40 | – | |
| Race/Ethnicity | <0.01 | |||
| White | 46 | 46 | ref | |
| Black | 30 | 36 | 0.8 (0.7–0.8) | |
| Hispanic | 10 | 39 | 0.9 (0.9–1.0) | |
| Other | 14 | 36 | 0.9 (0.9–1.0) | |
|
| ||||
| Marital Status | <0.01 | |||
|
| ||||
| Married | 29 | 44 | – | |
| Single | 58 | 40 | – | |
| Other/Missing | 13 | 37 | – | |
|
| ||||
| Insurance | <0.01 | |||
|
| ||||
| Medicare | 35 | 45 | – | |
| Medicaid | 24 | 38 | – | |
| Private | 24 | 40 | – | |
| Uninsured | 13 | 38 | – | |
| Other/Unknown | 3 | 36 | – | |
|
| ||||
| Comorbidities | ||||
|
| ||||
| Hypertension | 53 | 43 | <0.01 | – |
| Diabetes | 28 | 43 | <0.01 | – |
| Obesity | 28 | 43 | <0.01 | 1.1 (1.0–1.1) |
| Fluid and electrolyte disorders | 20 | 43 | <0.01 | 1.1 (1.0–1.1) |
| Chronic pulmonary disease | 13 | 42 | 0.02 | – |
| Depression | 15 | 44 | <0.01 | – |
| Congestive heart failure | 13 | 41 | 0.48 | 0.8 (0.8–0.9) |
| Deficiency anemias | 10 | 40 | 0.24 | 0.9 (0.9–1.0) |
| Renal failure | 7 | 40 | 0.15 | 0.9 (0.8–0.9) |
|
| ||||
| Receipt of mechanical ventilation | ||||
|
| ||||
| Yes | 13 | 42 | 0.06 | – |
| No | 87 | 41 | – | |
|
| ||||
| Chronic obstructive asthma (493.2x) | <0.01 | |||
|
| ||||
| No | 62 | 36 | ref | |
| Yes | 38 | 49 | 1.6 (1.5–1.7) | |
| Hospital Characteristics | ||||
|
| ||||
| Bed Size | <0.01 | |||
|
| ||||
| Small, <200 | 19 | 48 | – | |
| Medium, 200–400 | 38 | 43 | – | |
| Large, >400 | 43 | 36 | – | |
|
| ||||
| Region | <0.01 | |||
|
| ||||
| South | 10 | 43 | ref | |
| Midwest | 23 | 40 | 0.8 (0.7–1.0) | |
| Northeast | 20 | 32 | 0.6 (0.5–0.7) | |
| West | 48 | 45 | 0.8 (0.6–0.9) | |
|
| ||||
| Rural/Urban Status | <0.01 | |||
|
| ||||
| Urban | 89 | 40 | – | |
| Rural | 11 | 50 | – | |
|
| ||||
| Teaching Status | <0.01 | |||
|
| ||||
| Non-Teaching | 58 | 46 | ref | |
| Teaching | 42 | 34 | 0.7 (0.6–0.8) | |
Figure 1. Antibiotic prescribing rates across hospitalsa included in the study.
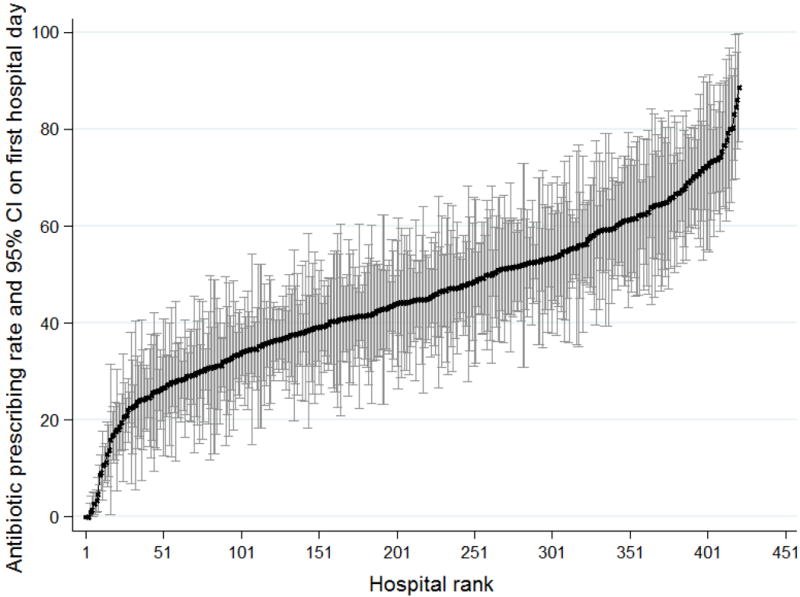
aLimited to 421 hospitals with at least 25 cases of asthma during the study period
Factors associated with lower chance of antibiotic treatment included younger age, Black race compared to White, heart failure, being treated at a teaching hospital or a hospital located in the Northeast or West compared to the South. Chronic obstructive asthma was associated with an increased likelihood of receiving antibiotic treatment. (Table) These results were robust in sensitivity analysis.
Discussion
In this large national sample we found that nearly 60% of patients hospitalized for asthma received antibiotics in the absence of documentation of an indication for antibiotic therapy. These findings build upon prior research restricted to US EDs that reported that 18–22% of patients with asthma were given a prescription for an antibiotic upon ED discharge.6
Potential explanations for this high rate of potentially inappropriate treatment include the challenge of differentiating bacterial from non-bacterial infections, distinguishing asthma from COPD in the acute care setting, and gaps in knowledge about the benefits of antibiotic therapy. Limitations of the study include the non-population-based sample, the possibility that concern about infection was not always accompanied by a billing diagnosis or culture specimen, and lack of information about antibiotic prescribing at discharge.
These findings suggest a significant opportunity to improve patient safety, reduce the spread of resistance, and lower spending through greater adherence to guideline recommendations. We hope these results prompt hospital-based clinicians to examine local treatment patterns, and attract the attention of professional societies and government agencies charged with promoting antimicrobial stewardship.
Acknowledgments
Source of Funding/Support
Dr. Stefan is supported by grant K01 (HL114631) from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Feemster is supported by grant K23 (HL111116) from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Feemster and Dr. Au receive support from the VA Health Services Research & Development.
Footnotes
Authors’ Contributions
Dr. Lindenauer conceived of the study and acquired the data. Drs. Lindenauer, Stefan, Feemster, Shieh, Carson, Au and Krishnan analyzed and interpreted the data. Dr. Lindenauer drafted the manuscript. All authors critically reviewed the manuscript for intellectual content. We certify that we have all participated sufficiently in the conception and design of this work, analysis, and interpretation of the data, as well as the writing of the manuscript to take public responsibility for it. We have all reviewed the final version of the manuscript and approve it for publication. The manuscript represents original work, is not under consideration elsewhere, and its contents have not been previously published.
Data Access and Responsibility
Dr. Lindenauer had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
Authors report no conflict of interest.
Disclaimer
The views expressed here are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Fridkin S, Baggs J, Fagan R, et al. Vital Signs: Improving Antibiotic Use Among Hospitalized Patients. Centers for Disease Control and Prevention; 2014. pp. 1–7. http://www.cdc.gov/mmwr/pdf/wk/mm63e0304.pdf. [Google Scholar]
- 2.The White House. National Action Plan for Combating Antibiotic-Resistant Bacteria. 2015 Mar; https://www.whitehouse.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf. Accessed January 25, 2016.
- 3.Centers for Disease Control and Prevention. FastStats; Asthma: http://www.cdc.gov/nchs/fastats/asthma.htm. Accessed December 30, 2015. [Google Scholar]
- 4.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma. 2015 http://www.ginasthma.org/documents/4. Accessed December 30, 2015.
- 5.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 6.Vanderweil SG, Tsai C-L, Pelletier AJ, et al. Inappropriate use of antibiotics for acute asthma in United States emergency departments. Acad Emerg Med Off J Soc Acad Emerg Med. 2008;15(8):736–743. doi: 10.1111/j.1553-2712.2008.00167.x. [DOI] [PubMed] [Google Scholar]


