Abstract
Background
Epidemiology studies have shown that ambient concentrations of ozone and fine particulate matter (PM2.5) are associated with increased emergency department (ED) visits and hospital admissions (HAs) for asthma.
Objective
Evaluate the impact of outdoor pollen, respiratory infections, and socioeconomic status (SES) on the associations between ambient ozone and PM2.5 and asthma HAs in New York City.
Methods
Daily ozone, PM2.5, meteorological factors, pollen, and hospitalization records during 1999 to 2009 were obtained for New York City residents. Daily counts of HAs for asthma and respiratory infections were calculated for all-age and specific age groups, and for high- and low-SES communities. Generalized additive models were used to examine ambient concentrations of ozone and PM2.5 and asthma HAs, potential confounding effects of outdoor pollen and HAs for respiratory infections, and potential effect modification by neighborhood SES.
Results
Both ozone and PM2.5 were statistically significantly associated with increased asthma HAs in children aged 6–18 years (per 10 ppb increase in ozone: RR = 1.0203, 95% CI: 1.0028–1.0382; per 10 μg/m3 increase in PM2.5: RR = 1.0218, 95% CI: 1.0007–1.0434), but not with total asthma HAs, or asthma HAs in other age groups. These associations were stronger for children living in the high-SES areas. Adjustment for respiratory infection HAs at various lags did not result in changes greater than 10% in the risk estimates for either ozone or PM2.5. In contrast, adjustment for outdoor pollen generally attenuated the estimated RRs for both ozone and PM2.5.
Conclusions
Ambient ozone and PM2.5 are associated with asthma HAs in school-age children, and these associations are not modified by SES. HAs for respiratory infections do not appear to be a confounder for observed ozone- and PM2.5-asthma HAs associations, but pollen may be a weak confounder.
Introduction
A number of epidemiology studies have reported positive associations between asthma exacerbation and ambient concentrations of ozone and fine particulate matter (PM2.5), measured as emergency department (ED) visits or hospital admissions (HAs) for asthma (e.g., [1–6]), and that children may be particularly susceptible to the effects of air pollution (e.g., see [7–10]). Many of these studies may have been vulnerable to confounding by time-varying factors such as temperature, outdoor pollen, and the start of the school year. Various methods have been developed to mitigate the effect of such confounding on effect estimates, but residual confounding remains an important source of uncertainty. Because the magnitude of associations between short-term air pollution and health effects are small, any residual confounding–even if small–could have had a substantial impact on the interpretation of study findings [11–13].
Outdoor pollen and upper respiratory infections are strong risk factors for asthma exacerbation [4, 14–19], and both exhibit short- and long-term changes over time that may correlate to some degree with temporal changes in air pollutants [16, 20]. In addition, concurrent exposures to both respiratory infections and inhaled allergens can greatly increase the risk of severe asthma exacerbations for children [21–23]. While some time series analyses of pediatric asthma and air pollution have accounted for potential confounding by pollen or upper respiratory infections with statistical adjustment for these variables (e.g., [1]), most analyses instead include a smooth function of calendar time as a surrogate measure of potential time-varying confounding. Although these confounding factors have been assessed in case-crossover designs [4, 24], to our knowledge, no time series studies have included a direct and thorough assessment of potential confounding by both factors, independently and in combination.
In addition, several recent studies reported that individual or community-level socioeconomic status (SES) modified the health effects of air pollution, and the observed effect modifications might be due to varying levels of psychosocial stress or access to healthcare resources [25–28]. We hypothesized that observed air pollution-asthma associations, as well as the potential confounding effects by respiratory infections or outdoor pollen, may vary by SES.
We conducted a time series study of asthma HAs and ambient concentrations of ozone and PM2.5 in New York City to determine whether results are confounded by outdoor pollen or upper respiratory infections, and whether neighborhood SES modifies the associations between air pollutants and asthma HAs with adjustment for potential confounding effects of pollen and respiratory infections.
Methods
Hospitalization data
We obtained hospitalization records from the New York Statewide Planning and Research Cooperative System (SPARCS) for the years 1999–2009. We identified asthma HAs by the International Statistical Classification of Diseases, 9th Revision (ICD-9) code (493), and excluded the asthma HAs that were elective admissions or had an unknown admission status. We calculated daily counts of asthma HAs for patients of all ages as well as for several age groups (under 6 years old, 6 to 18 years old, 19 to 49 years old, and 50 years old and older).
Similarly, we counted daily HAs for respiratory infections among patients of all ages as well as for children 6 to 18 years old (ICD-9: 460–466, 480–487), and daily HAs for influenza, specifically, for these age groups (ICD-9: 487). In our assessment of potential confounding by respiratory infections, we used log-transformed daily counts of HAs for respiratory infections (either all types or only influenza) as a surrogate measure of individual exposure to respiratory infections. Other epidemiology analyses of asthma have used such an ecological measure and demonstrated that it correlates strongly with short-term risk of asthma exacerbations (e.g., [20]).
Our study was approved by Chesapeake IRB (Columbia, MD).
Environmental data
The 8-hour maximum ozone and 24-hour average PM2.5 concentrations were downloaded from the United States Environmental Protection Agency (US EPA) Air Quality System (AQS, https://www.epa.gov/outdoor-air-quality-data). We selected all monitors located in New York State and within a 20-mile radius of the geographic center of New York City (40.74°N, 73.91°W). The data from all selected monitors with available measurements were averaged for each day from 1999 to 2009. For sensitivity analyses, we calculated alternative daily average concentrations of pollutants by varying the location of the city center (40.73°N, 73.99°W; 40.71°N, 73.92°W) or the selection radius (15–30 miles), as well as by including nearby New Jersey and Connecticut sites.
Hourly weather data for LaGuardia Airport (Queens, NY) were obtained from the National Centers for Environmental Information (http://www.ncdc.noaa.gov/orders/qclcd/).
To estimate daily exposures to various types of outdoor aeroallergens, we relied on measurements of outdoor pollen concentrations for 2002–2006 compiled at the Fordham University's Louis Calder Biological Station in Armonk, NY, provided to us by the manager of the monitoring center. Details of the experimental technique used for sample collection and measurement of various genera of pollen are described elsewhere [29, 30]. We log-transformed daily concentrations (grains per cubic meter) for tree, weed, and total pollen, and created an indicator variable for outdoor pollen if daily concentrations exceeded the 5th percentile of the concentration distribution. This dichotomized approach is based on studies of asthma morbidity and pollen exposure that show that very low concentrations of pollen are sufficient to greatly increase the risk of asthma exacerbation [17]. Because pollen data were only measured from March through October, and there were no records for some days, we imputed the missing values using the approach described by Gleason et al. [4]. Briefly, a day with missing pollen counts was assigned the pollen counts from the previous day for up to three consecutive days with missing values. If there were more than three consecutive days with missing pollen values, the remainder of the days were given the pollen value from the succeeding day. The log-transformed pollen concentrations from November through February were set to 0.
Census data and stratification by SES
We stratified the counts of asthma HAs by neighborhood SES. We used patient billing US Postal Service (USPS) ZIP codes (missing for only 2.78% of records) as an approximation of ZIP Code Tabulation Areas (ZCTA), which are areal representations of USPS ZIP codes developed by the US Census Bureau for linkage to census data. We linked patient ZIP codes to census tracts using US Census Bureau 2010 databases, and then to the percentages of households in the census tract with incomes below the poverty level in the 2006–2010 five-year census. If a ZIP code matched to more than one census tract, the percentages of households in poverty for all tracts were averaged and assigned to that ZIP code. In a separate analysis, we identified each patient as living in either a relatively high or low SES ZIP code area using a cut-off of 20% of families in poverty, similar to the approach used in recent analyses of SES and asthma [28, 31].
Statistical analysis
We assessed associations between daily counts of asthma HAs and ambient ozone or PM2.5 concentrations using generalized additive regression models adjusted for various potential confounders, following the approach of similar studies [3, 13]. We scaled all results to represent relative risks (RRs) of asthma HAs per 10 parts per billion (ppb) increase in ozone or 10 μg/m3 increase in PM2.5.
Our main analyses included adjustment for federal holidays, the day of the week, the beginning of the school year (September [32]), temperature, very hot and humid conditions (defined as average temperature greater than 78 degrees and relative humidity greater than 80%), and temporal trends (Eq 1). For the temporal relationship between exposure and outcome, we analyzed the average pollutant concentrations on the same day and one day prior to the day of asthma HA (i.e., lag 0–1). We calculated associations using all data between 1999 and 2009, as well as data restricted to the warm season (April through August) because ozone and PM2.5 concentrations are generally higher during the warm season and warm season associations are often stronger than those observed in the cold season or across the whole year (e.g., [1, 4, 9, 24, 33]).
| (Eq 1) |
where:
E(Yt) is the expected count of asthma HAs on day t,
is the ozone or PM2.5 average daily concentrations on day t and one day prior,
DOWt is a categorical variable with seven levels specifying the day of the week on day t,
IHHt is an indicator variable that equals 1 on very hot and humid days (i.e., average temperature > 80°F and relative humidity > 80%), and otherwise 0,
Holidayt is an indicator variable that equals 1 if day t is a federal holiday, and otherwise 0,
Schoolt is an indicator variable that equals 1 if day t is in September, and otherwise 0,
ns(timet, 12 df/year) is a cubic spline function of time with twelve knots per year to control for temporal trends,
is a cubic spline function of the current-day average temperature with 3 degrees of freedom,
is a cubic spline function of the average temperature over the last two days with 3 degrees of freedom, and
Yt−1,Yt−2,Yt−3,Yt−4 are lag 1, lag 2, lag 3, and lag 4 day of asthma HAs counts on day t.
In sensitivity analyses, we evaluated whether results from our main analyses were robust against variations in model specifications, including by varying the degrees of freedom in temporal trends and varying the form of the temperature and humidity covariates (i.e., using maximum or minimum instead of average). We also tested whether the observed associations in our main analyses varied when alternative daily average concentrations of pollutants were used.
We repeated all analyses with the inclusion of residents' exposure to respiratory infections or ambient pollen, and we determined whether adjustment for these factors affected main effect estimates between air pollutants and daily asthma HAs. To assess confounding by respiratory infections, we adjusted for the HAs for total respiratory infections or for influenza among school-age children (6–18 years) at various lags (i.e., lag 0–1, lag 2–3, lag 4–6, lag 0–6). We evaluated confounding by ambient pollen by adjusting for outdoor tree, weed, or total pollen, either as a continuous variable or a binary variable, at various lags (i.e., lag 0–1, lag 2–3, lag 4–6, lag 0–6).
We also explored whether respiratory infections and pollen confound associations between air pollution and asthma HAs synergistically; that is, whether controlling for periods of both high respiratory infections and high pollen exposure affect the magnitude of associations between air pollution and asthma. To do so, we chose the ambient pollen and respiratory infection variables that have the strongest confounding effects on the main model, and repeated the main analysis for each pollutant with the inclusion of both factors, as well as their interaction term.
Finally, we evaluated whether SES modified the observed air pollution-asthma HAs associations, by including an indicator variable for patients living in relatively high- or low-SES neighborhoods and an interaction term between the indicator variable and the air pollutant in the main model. In an exploratory analysis, we also evaluated the confounding effect of outdoor pollen separately in the high- and low-SES communities.
All statistical analyses were conducted with SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Daily counts of HAs for asthma and respiratory infections, daily ambient ozone, PM2.5, pollen concentrations, and daily temperatures in New York City are presented in Table 1 and S1 Table. There were a total of 295,497 (average daily count of 73.5) asthma HAs in New York City from 1999 to 2009, which included 113,144 (38.3%) patients who lived in high SES communities (mean daily counts = 28.2) and 179,743 (60.8%) who lived in low SES communities (mean daily counts = 44.7). Daily counts of respiratory infection HAs ranged from 0 to 534, with an average of 156.4. Daily pollen concentrations ranged from 0 to 16,425.2 grains/m3, with a mean of 234.6 grains/m3. Average daily concentrations of ozone and PM2.5 were 30.7 ppb and 13.8 μg/m3, respectively. Both ozone and PM2.5 were significantly correlated with temperatures and total weed pollens (S2 Table).
Table 1. Daily hospital admissions for asthma and upper respiratory infections, air pollutants, outdoor pollen, and temperature in New York City, from 1999 to 2009.
| Percentile | ||||||
|---|---|---|---|---|---|---|
| Mean (SD) | Min | 25th | 50th | 75th | Max | |
| Hospital Admissions for Asthma (N) | ||||||
| Total | 73.54 (22.39) | 0 | 57 | 74 | 88 | 175 |
| Age < 6 years | 17.39 (8.39) | 0 | 11 | 17 | 22 | 70 |
| Age 6–18 years | 12.02 (7.37) | 0 | 6 | 11 | 16 | 60 |
| Age 19–49 years | 19.57 (6.86) | 0 | 15 | 19 | 24 | 62 |
| Age 50+ years | 24.56 (24.56) | 0 | 19 | 24 | 29 | 66 |
| High SES | 28.16 (9.66) | 0 | 22 | 28 | 34 | 75 |
| Low SES | 44.73 (14.40) | 0 | 34 | 44 | 54 | 107 |
| Hospital Admissions for Upper Respiratory Infections (N) | ||||||
| ;Total | 156.35 (48.68) | 0 | 123 | 151 | 181 | 534 |
| Age < 6 years | 36.49 (21.17) | 0 | 20 | 32 | 47 | 124 |
| Age 6–18 years | 7.50 (4.04) | 0 | 5 | 7 | 10 | 43 |
| Age 19–49 years | 24.74 (8.43) | 0 | 19 | 24 | 29 | 75 |
| Age 50+ years | 87.62 (26.30) | 0 | 72 | 85 | 99 | 333 |
| High SES | 85.69 (27.23) | 0 | 68 | 82 | 98 | 308 |
| Low SES | 68.09 (23.19) | 0 | 51 | 66 | 81 | 217 |
| Air Pollutants | ||||||
| 8-hour max ozone (ppb) | 30.73 (16.90) | 2.00 | 18.60 | 28.00 | 39.90 | 105.40 |
| 24-hour average PM2.5 (μg/m3) | 13.76 (8.25) | 2.13 | 7.67 | 11.66 | 17.70 | 80.70 |
| Outdoor Pollena (grains/m3) | ||||||
| Total pollen | 234.55 (825.79) | 0 | 4.42 | 15.80 | 92.80 | 16,425.15 |
| Total tree pollen | 223.83 (822.24) | 0 | 0.00 | 4.42 | 73.82 | 16,405.35 |
| Total weed pollen | 4.81 (10.48) | 0 | 0.00 | 0.00 | 5.40 | 114.90 |
| Temperature (°F) | ||||||
| Daily average temperature | 55.78 (17.04) | 8.80 | 42.10 | 55.80 | 71.00 | 93.00 |
| Daily minimum temperature | 49.67 (16.67) | 2.00 | 37.00 | 50.00 | 65.00 | 86.00 |
| Daily maximum temperature | 62.18 (17.95) | 16.00 | 48.00 | 62.10 | 78.00 | 101.00 |
PM2.5 = Fine Particulate Matter; ppb = Parts Per Billion; SD = Standard Deviation; SES = Socioeconomic Status; μg/m3 = Microgram Per Cubic Meter.
(a) Pollen data are available from March to October, 2002–2006.
Adjusted RRs for total and age-specific asthma HAs associated with ozone and PM2.5 concentrations at lag 0–1 day are presented in Table 2. In all-year analyses, increases in ozone and PM2.5 concentrations were statistically significantly associated with increased asthma HAs in children aged 6–18 years (ozone: RR = 1.0203, 95% confidence interval [CI]: 1.0028–1.0382; PM2.5: RR = 1.0218, 95% CI: 1.0007–1.0434) but not with total asthma HAs or asthma HAs in other age groups. The point estimates for the two pollutants and asthma HAs in school-age children appeared to be slightly stronger for warm-season analyses (ozone: RR = 1.0271, 95% CI: 1.0039–1.0508; PM2.5: RR = 1.0469, 95% CI: 1.0094–1.0858). We also conducted a series of sensitivity analyses with different model and covariate specifications (S3 Table). In general, the effect estimates for ozone and PM2.5 were robust to various specifications of temporal and meteorological variables. The results also did not change when we used alternative daily average concentrations of pollutants (S4 Table).
Table 2. Relative risksa of hospital admissions for asthma per 10 ppb increase in ozone concentrations or per 10 μg/m3 increase in PM2.5 concentrations in New York City, from 1999 to 2009.
| Hospital Admissions for Asthma | All Year | Warm Season | ||||||
|---|---|---|---|---|---|---|---|---|
| Ozone | PM2.5 | Ozone | PM2.5 | |||||
| RR (95% CI) | p-value | RR (95% CI) | p-value | RR (95% CI) | p-value | RR (95% CI) | p-value | |
| Total | 1.0066 | 0.1 | 1.0053 | 0.3 | 1.0068 | 0.2 | 1.0132 | 0.1 |
| (0.9988, 1.0145) | (0.9957, 1.015) | (0.9969, 1.0167) | (0.9974, 1.0294) | |||||
| Age < 6 years | 1.0001 | 1.0 | 1.0096 | 0.2 | 0.9964 | 0.7 | 1.0208 | 0.1 |
| (0.9870, 1.0133) | (0.9936, 1.0259) | (0.9795, 1.0137) | (0.993, 1.0491) | |||||
| Age 6–18 years | 1.0203 | 0.02 | 1.0218 | 0.04 | 1.0271 | 0.02 | 1.0469 | 0.01 |
| (1.0028, 1.0382) | (1.0007, 1.0434) | (1.0039, 1.0508) | (1.0094, 1.0858) | |||||
| Age 19–49 years | 1.0112 | 0.07 | 0.9952 | 0.5 | 1.0149 | 0.05 | 1.0156 | 0.2 |
| (0.9991, 1.0234) | (0.9805, 1.0101) | (0.9998, 1.0302) | (0.9917, 1.04) | |||||
| Age 50+ years | 0.9992 | 0.9 | 1.0035 | 0.6 | 0.9987 | 0.9 | 0.9948 | 0.6 |
| (0.9881, 1.0104) | (0.9897, 1.0175) | (0.9851, 1.0125) | (0.973, 1.0171) | |||||
CI = Confidence Interval; d.f. = Degree of Freedom; PM2.5 = Fine Particulate Matter; ppb = Parts Per Billion; RR = Relative Risk; μg/m3 = Microgram Per Cubic Meter.
(a) Relative risks were estimated from generalized additive models for lag 0–1 day air pollutants with adjustment for cubic splines of calendar time (12 d.f. per year), cubic splines of same-day temperature (3 d.f.), cubic splines of lag 1–2 day temperature (3 d.f.), start of school, very hot and humid day, day of the week, and public holidays.
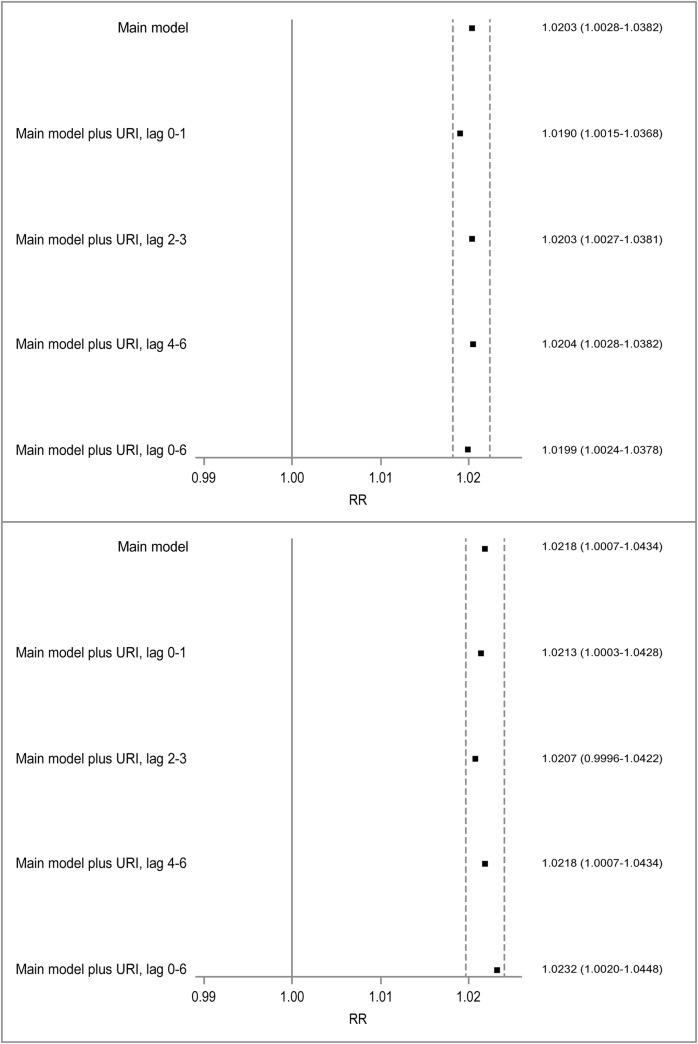
We evaluated potential confounding of observed associations between asthma HAs in children aged 6–18 years and ozone and PM2.5 by respiratory infections (Fig 1). Adjustment for respiratory infection HAs at various lags resulted in minimal changes (<10%) in the risk estimates for both ozone and PM2.5, indicating respiratory infections did not materially confound the observed associations. Using HAs for influenza instead of all respiratory infections (S1 Fig) did not change the results in any significant way. Adjustment for respiratory infection HAs in children aged 6–18 years old instead of respiratory infections for all ages also did not change the results (S2 Fig).
Fig 1. Confounding effects of hospital admissions for Upper Respiratory Infections (URI) on the associations between asthma hospital admissions in school-age children and ozone (top) and PM2.5 (bottom).
URI is included in the main model as log-transformed daily counts of all-age URI HA. Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
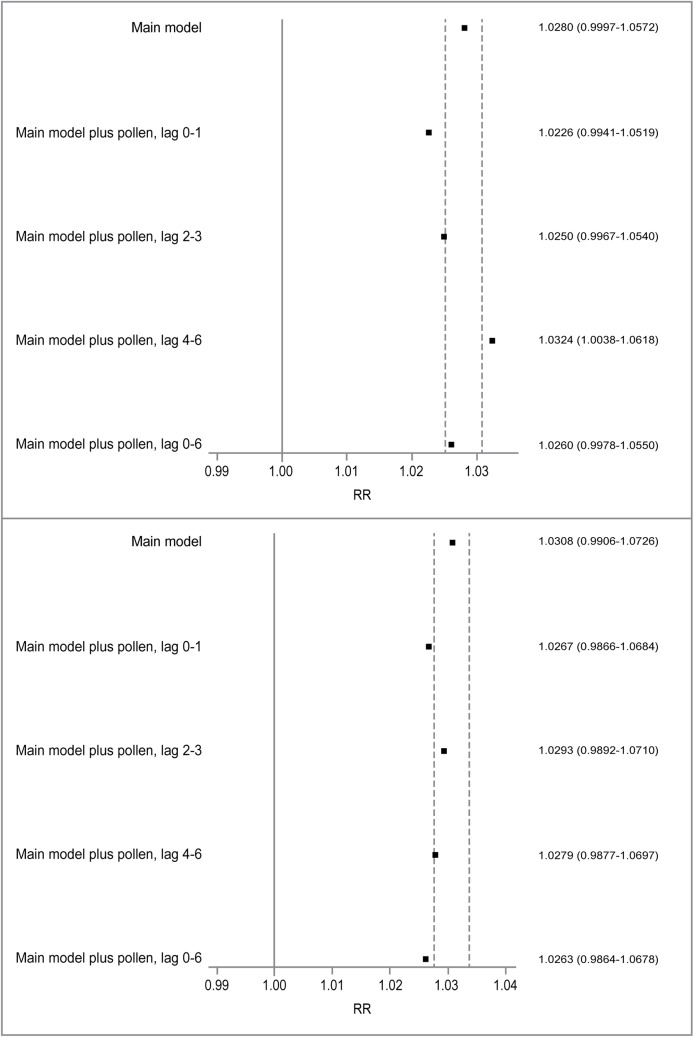
We next evaluated daily pollen levels as a potential confounder for the ozone- and PM2.5-asthma associations in children aged 6–18 years (Fig 2). We restricted our analysis to the warm seasons of 2002–2006 (when pollen data were available), and the main models yielded non-significant results for both ozone and PM2.5. Inclusion of log-transformed pollen counts as a linear term generally attenuated the estimated RRs for both ozone and PM2.5, except for pollen counts at lag 4–6 day, which resulted in an increased RR for ozone. The results did not change with the adjustment for outdoor pollen as a binary variable (S3 Fig). Using total weed pollen or total tree pollen instead of the total pollen led to the same conclusions (S4 Fig).
Fig 2. Confounding effects of outdoor pollen on the associations between asthma hospital admissions in school-age children and ozone (top) and PM2.5 (bottom).
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
We also evaluated the combined effect of respiratory infections and pollen on the results of our main analyses (S5 Fig). We only considered the lags of respiratory infections and pollen that had the largest observed confounding effect when evaluated independently (ozone: lag 0–1 for pollen, lag 0–1 for respiratory infections; PM2.5: lag 0–6 for pollen, lag 0–6 for respiratory infections). Inclusion of both respiratory infections and pollen, as well as their interaction term (pinteraction = 0.0522 and pinteraction = 0.0536 in the ozone and PM2.5 models, respectively), attenuated the estimated association between both pollutants and asthma HAs in children aged 6–18 years.
We next evaluated whether SES modifies the observed effects of ozone and PM2.5 on asthma HAs with adjustment for outdoor pollen. We selected pollen at lag 0–1 for the models of ozone and asthma HAs, and pollen at lag 0–6 for the models of PM2.5, because these were the lag times associated with the strongest confounding effects (Fig 2). As shown in Table 3, the observed associations between asthma HAs and the two pollutants, none of which were statistically significant, appeared to be similar between high- and low-SES communities.
Table 3. Relative risksa of hospital admissions for asthma per 10 ppb increase in ozone concentrations or per 10 μg/m3 increase in PM2.5 concentrations at Lag 0–1 in New York City, stratified by socioeconomic status, during warm seasons from 2002 to 2006.
| Asthma HAs | Warm season 02–06 | |||||
|---|---|---|---|---|---|---|
| Ozonea | PM2.5a | |||||
| High-SES | Low-SES | P of SES-ozone Interaction | High-SES | Low-SES | P of SES-PM2.5 Interaction | |
| All ages | 1.0025 | 1.0034 | 0.8509 | 1.0085 | 1.0145 | 0.5408 |
| (0.9902, 1.0148) | (0.9920, 1.0149) | (0.9887, 1.0286) | (0.9970, 1.0323) | |||
| Age < 6 y.o. | 1.003 | 0.9929 | 0.2626 | 0.9979 | 1.0103 | 0.4999 |
| (0.9804, 1.0261) | (0.9724, 1.0139) | (0.9616, 1.0356) | (0.9786, 1.0430) | |||
| Age 6–18 y.o. | 1.0269 | 1.0211 | 0.6326 | 1.0212 | 1.034 | 0.5897 |
| (0.9965, 1.0581) | (0.9935, 1.0495) | (0.9736, 1.0711) | (0.9935, 1.0762) | |||
| Age 19–49 y.o. | 0.9989 | 0.9979 | 0.8903 | 0.9985 | 1.0148 | 0.3255 |
| (0.9789, 1.0193) | (0.9795, 1.0166) | (0.9658, 1.0324) | (0.9863, 1.0441) | |||
| Age 50+ y.o. | 1.0023 | 1.0053 | 0.6645 | 1.0085 | 1.013 | 0.7568 |
| (0.9846, 1.0204) | (0.9882, 1.0226) | (0.9797, 1.0381) | (0.9863, 1.0404) | |||
d.f. = Degree of Freedom; PM2.5 = Fine Particulate Matter; ppb = Parts Per Billion; SES = Socioeconomic Status; μg/m3 = Microgram Per Cubic Meter.
(a) Relative risks were estimated from generalized additive models for outdoor pollen, lag 0–1 day air pollutants with adjustment for cubic splines of calendar time (12 d.f. per year), cubic splines of same-day temperature (3 d.f.), cubic splines of lag 1–2 day temperature (3 d.f.), start of school, very hot and humid day, day of the week, and public holidays.
Finally, we explored whether the confounding effects by pollen vary by lag time, air pollutant, or SES (S6 Fig). We evaluated the changes in effect estimates of ozone and PM2.5 with adjustment for outdoor pollen levels at different lag times in high- and low-SES communities separately. In general, the confounding effect of pollen at various lag times appeared to be slightly stronger for ozone in high-SES communities, and for PM2.5 in low-SES communities. However, with the exception of ozone with adjustment for pollen at lag 4–6 in low-SES communities, all of the effect estimates for ozone and PM2.5 were small in magnitude and not statistically significant.
Discussion
We conducted a time series analysis of ambient ozone and PM2.5 and daily counts of asthma HAs in New York City, and observed small elevations in the risk of asthma HAs among school-age children following elevated concentrations of pollutants. HAs for respiratory infections do not appear to be a confounder for observed air pollutant-asthma HAs associations, but pollen may be a weak confounder. SES did not appear to modify the observed associations between asthma HAs and air pollutants.
Our findings of increased asthma HAs associated with air pollutant exposures are consistent with several other time series studies. Recently, a meta-analysis of published epidemiology studies of air pollution and asthma HAs or ED visits reported a meta-RR of 1.008 (95% CI: 1.005–1.012; n = 42 studies) per 10 ppb increase in ozone and 1.025 (95% CI: 1.013–1.031; n = 20 studies) per 10 μg/m3 increase in PM2.5 for children [9]. Lim et al. [10] conducted a systematic review of PM2.5 exposure and reported a meta-RR of 1.048 (95% CI: 1.028–1.067) when pooling results of 26 studies of HAs and ED visits for pediatric asthma per 10 μg/m3 increase in PM2.5 exposure. Notably, both meta-analyses found a high degree of heterogeneity (>80%) among studies.
Some studies have observed evidence that respiratory infections confound associations between short-term air pollution exposure and asthma [1, 14, 20]. In contrast, we observed no compelling evidence that associations were confounded by HAs for respiratory infections in New York City. It is possible that daily counts of HAs for respiratory infections may not accurately represent the temporal patterns of residents' exposure to respiratory infections. Therefore, we cannot rule out confounding by respiratory infections in our study entirely.
Several studies have reported strong associations between outdoor pollen and other aeroallergens and asthma exacerbations [4, 17, 18, 30, 34], but only a few presented evidence that pollen may confound the associations between air pollution and asthma [4, 6]. In our analyses, pollen appeared to be a weak negative confounder for the associations between asthma HAs and ozone and PM2.5. However, the nature of confounding by pollen is complex due to several uncertainties. The risk of respiratory effects from pollen exposure varies significantly between individuals and is largely determined by allergic sensitization to the specific pollen genera [19]. Also, respiratory health risks can vary strongly by specific genera of pollen [4, 18]. Furthermore, there is uncertainty regarding the true shape of the dose-response relationship between pollen and respiratory effects [17] and the lag relationship between pollen exposure and health effects [4, 18]. Finally, the strength of the relationship between pollen and respiratory effects may change across the course of a pollen season, with risks declining later in the pollen season [30], which in turn could affect the confounding effect of pollen. Future analyses of pollen as a potential confounder for the associations between air pollutants and asthma should aim to account for these uncertainties.
Several researchers have hypothesized that low-resource individuals and communities are more vulnerable to the effects of air pollution [26, 28]. However, we did not observe strong evidence for interactions between air pollutants and SES in our analysis. Other published epidemiology studies have reported mixed results. For example, Wilhelm et al. [25] observed stronger associations between ozone and asthma among relatively high resource neighborhoods, while others found evidence of increased asthma susceptibility to air pollution in lower SES or otherwise lower resource communities [26, 27]. These mixed findings could be due to heterogeneous populations, local conditions, analytical uncertainties, such as the geographical resolution for estimates of SES (e.g., zip code vs. census tracts vs. census blocks), and whether any true effect modifications are linear. O'Lenick et al. [28], for example, observed a U-shaped relationship between the modification of asthma-air pollution associations by SES: associations were stronger in communities of both the lowest and highest quartiles of SES.
In an exploratory analysis, we observed slightly stronger confounding effects of pollen on the association between ozone and asthma HAs among school-age children in high-SES areas. We hypothesize that this may be because of differing access to healthcare resources and treatments for allergic airway diseases. For example, it has been shown that a child's vulnerability to respiratory effects of seasonal pollen exposure is affected by whether or not the child is taking asthma maintenance medication [17].
To our knowledge, ours is the first time series study of air pollution and asthma to examine potential confounding by pollen and respiratory infections, including an evaluation of combined effects of these two factors, and, specifically, an evaluation of whether the nature of confounding varies by neighborhood SES. Strengths of our study include the large sample size and our rigorous assessment of model specification in statistical analyses. We also used measurements of ambient pollen in New York City from a database of uniquely high-quality pollen data [30].
We also note several limitations of our analyses. As is the case for all time series air pollution analyses, our study is ecological in nature and provides limited insight into individual-level exposures and health risks. Because we relied on central site monitors to estimate population exposures to ambient air pollutants, there may be substantial exposure measurement error. The impact on health effect estimates likely depend on the amount and type of measurement errors [35, 36]. In addition, ambient pollen concentrations exhibit a high degree of geographic heterogeneity [37], thus pollen counts made at one location in New York City may not accurately represent true exposures across the study region. It is difficult to know how such spatial heterogeneity in ambient pollen concentrations impacted results.
In conclusion, we found that ambient ozone and PM2.5 are associated with asthma HAs among school-age children in New York City, and these associations did not vary by SES. HAs for respiratory infections do not appear to be a confounder for observed ozone- and PM2.5-asthma HAs associations, but there is some evidence that pollen may be a weak confounder. Future studies should consider confounding by pollen when evaluating air pollution and respiratory morbidity.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
URI is adjusted by adding log-transformed daily URI counts for school-aged children into the main model. Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model. Outdoor pollen is defined as daily counts of > 5th percentile.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Acknowledgments
We thank Dr. Guy Robinson at Fordham University for providing the pollen and aeroallergen data. We also thank the following Gradient staff: Dr. Yanxu Zhang for contributions to conditioning the air pollutants data, Dr. Thuy Lam for reviewing SAS code, and Ms. Jasmine Lai, Ms. Laura Smith, and Ms. Jessica Goldstein for editorial support.
Data Availability
The data on hospital admissions for asthma and respiratory infections cannot be made publicly available in order to protect private information of the patients. We obtained the asthma hospitalization data from the New York State Department of Health. These restrictions prohibit us from making the minimal data set publicly available. Requests for access to the data can be made to New York State Department of Health (Email: sparcs.requests@health.nv.gov; URL: http://www.health.ny.gov/statistics/sparcs/).
Funding Statement
The work reported in this paper was conducted by the authors during the normal course of their employment, with funding provided by the Exxonmobil Biomedical Sciences, Inc. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, Waller LA, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am. J. Respir. Crit. Care Med. 2010; 182(3): 307–316. doi: 10.1164/rccm.200908-1201OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tolbert PE, Mulholland JA, MacIntosh DL, Xu F, Daniels D, Devine OJ, et al. Air quality and pediatric emergency room visits for asthma in Atlanta, Georgia. Am. J. Epidemiol. 2000; 151(8): 798–810. [DOI] [PubMed] [Google Scholar]
- 3.Ito K, Thurston GD, Silverman RA. Characterization of PM2.5, gaseous pollutants, and meteorological interactions in the context of time-series health effects models. J. Expo. Sci. Environ. Epidemiol. 2007; 17(Suppl. 2): S45–S60. [DOI] [PubMed] [Google Scholar]
- 4.Gleason JA, Bielory L, Fagliano JA. Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in New Jersey: A case-crossover study. Environ. Res. 2014; 132: 421–429. doi: 10.1016/j.envres.2014.03.035 [DOI] [PubMed] [Google Scholar]
- 5.Evans KA, Halterman JS, Hopke PK, Fagnano M, Rich DQ. Increased ultrafine particles and carbon monoxide concentrations are associated with asthma exacerbation among urban children. Environ. Res. 2014; 129: 11–19. doi: 10.1016/j.envres.2013.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheffield PE, Zhou J, Shmool JL, Clougherty JE. Ambient ozone exposure and children's acute asthma in New York City: A case-crossover analysis. Environ. Health 2015; 14: 25 doi: 10.1186/s12940-015-0010-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US EPA. Integrated Science Assessment for Particulate Matter (Final). 2009; Office of Research and Development. National Center for Environmental Assessment (NCEA)—RTP Division, EPA/600/R-08/139F. 2,228p., December.
- 8.US EPA. Integrated Science Assessment for Ozone and Related Photochemical Oxidants (Final). 2013; National Center for Environmental Assessment (NCEA), EPA/600/R–10/076F. 1,251p., February.
- 9.Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: A systematic review and meta-analysis. PLoS ONE 2015; 10(9): e0138146 doi: 10.1371/journal.pone.0138146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim H, Kwon HJ, Lim JA, Choi JH, Ha M, Hwang SS, et al. Short-term effect of fine particulate matter on children's hospital admissions and emergency department visits for asthma: A systematic review and meta-analysis. J. Prev. Med. Public Health 2016; 49(4): 205–219. doi: 10.3961/jpmph.16.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lumley T, Sheppard L. Assessing seasonal confounding and model selection bias in air pollution epidemiology using positive and negative control analyses. Environmetrics 2000; 11: 705–717. [Google Scholar]
- 12.Bell ML, Samet JM, Dominici F. Time-series studies of particulate matter. Annu. Rev. Public Health 2004; 25: 247–280. doi: 10.1146/annurev.publhealth.25.102802.124329 [DOI] [PubMed] [Google Scholar]
- 13.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013; 42(4): 1187–1195. doi: 10.1093/ije/dyt092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rabinovitch N, Zhang L, Murphy JR, Vedal S, Dutton SJ, Gelfand EW. Effects of wintertime ambient air pollutants on asthma exacerbations in urban minority children with moderate to severe disease. J. Allergy Clin. Immunol. 2004; 114(5): 1131–1137. doi: 10.1016/j.jaci.2004.08.026 [DOI] [PubMed] [Google Scholar]
- 15.Forno E, Celedon JC. Health disparities in asthma (Editorial). Am. J. Respir. Crit. Care Med. 2012; 185(10): 1033–1035. doi: 10.1164/rccm.201202-0350ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eggo RM, Scott JG, Galvani AP, Meyers LA. Respiratory virus transmission dynamics determine timing of asthma exacerbation peaks: Evidence from a population-level model. Proc. Natl. Acad. Sci. USA 2016; doi: 10.1073/pnas.1518677113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DellaValle CT, Triche EW, Leaderer BP, Bell ML. Effects of ambient pollen concentrations on frequency and severity of asthma symptoms among asthmatic children. Epidemiology 2012; 23(1): 55–63. doi: 10.1097/EDE.0b013e31823b66b8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Darrow LA, Hess J, Rogers CA, Tolbert PE, Klein M, Sarnat SE. Ambient pollen concentrations and emergency department visits for asthma and wheeze. J. Allergy Clin. Immunol. 2012; 130(3): 630–638. doi: 10.1016/j.jaci.2012.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canova C, Heinrich J, Anto JM, Leynaert B, Smith M, Kuenzli N, et al. The influence of sensitisation to pollens and moulds on seasonal variations in asthma attacks. Eur. Respir. J. 2013; 42(4): 935–945. doi: 10.1183/09031936.00097412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van der Zee SC, Hoek G, Boezen MH, Schouten JP, van Wijnen JH, Brunekreef B. Acute effects of air pollution on respiratory health of 50–70 yr old adults. Eur. Respir. J. 2000; 15(4): 700–709. [DOI] [PubMed] [Google Scholar]
- 21.Eggleston PA. Complex interactions of pollutant and allergen exposures and their impact on people with asthma. Pediatrics 2009; 123: S160–S167. doi: 10.1542/peds.2008-2233F [DOI] [PubMed] [Google Scholar]
- 22.Murray CS, Poletti G, Kebadze T, Morris J, Woodcock A, Johnston SL, et al. Study of modifiable risk factors for asthma exacerbations: Virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax 2006; 61(5): 376–382. doi: 10.1136/thx.2005.042523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kloepfer KM, Gern JE. Virus/allergen interactions and exacerbations of asthma. Immunol. Allergy Clin. North Am. 2010; 30(4): 553–563. doi: 10.1016/j.iac.2010.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Villeneuve PJ, Chen L, Rowe BH, Coates F. Outdoor air pollution and emergency department visits for asthma among children and adults: A case-crossover study in northern Alberta, Canada. Environ. Health 2007; 6: 40 doi: 10.1186/1476-069X-6-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilhelm M, Qian L, Ritz B. Outdoor air pollution, family and neighborhood environment, and asthma in LA FANS children. Health Place 2009; 15(1): 25–36. doi: 10.1016/j.healthplace.2008.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yap PS, Gilbreath S, Garcia C, Jareen N, Goodrich B. The influence of socioeconomic markers on the association between fine particulate matter and hospital admissions for respiratory conditions among children. Am. J. Public Health 2013; 103(4): 695–702. doi: 10.2105/AJPH.2012.300945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strickland MJ, Klein M, Flanders WD, Chang HH, Mulholland JA, Tolbert PE, et al. Modification of the effect of ambient air pollution on pediatric asthma emergency visits: Susceptible subpopulations. Epidemiology 2014; 25(6): 843–850. doi: 10.1097/EDE.0000000000000170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Lenick CR, Winquist A, Mulholland JA, Friberg MD, Chang HH, Kramer MR, et al. Assessment of neighbourhood-level socioeconomic status as a modifier of air pollution-asthma associations among children in Atlanta. J. Epidemiol. Community Health 2016; doi: 10.1136/jech-2015-206530 [DOI] [PubMed] [Google Scholar]
- 29.Sheffield PE, Weinberger KR, Ito K, Matte TD, Mathes RW, Robinson GS, et al. The association of tree pollen concentration peaks and allergy medication sales in New York City: 2003–2008. ISRN Allergy 2011; 2011: 537194. doi: 10.5402/2011/537194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ito K, Weinberger KR, Robinson GS, Sheffield PE, Lall R, Mathes R, et al. The associations between daily spring pollen counts, over-the-counter allergy medication sales, and asthma syndrome emergency department visits in New York City, 2002–2012. Environ. Health 2015; 14: 71 doi: 10.1186/s12940-015-0057-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. J. Allergy Clin. Immunol. 2015; doi: 10.1016/j.jaci.2014.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnston NW, Johnston SL, Duncan JM, Greene JM, Kebadze T, Keith PK, et al. The September epidemic of asthma exacerbations in children: A search for etiology. J. Allergy Clin. Immunol. 2005; 115(1): 132–138. doi: 10.1016/j.jaci.2004.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jalaludin B, Khalaj B, Sheppeard V, Morgan G. Air pollution and ED visits for asthma in Australian children: A case-crossover analysis. Int. Arch. Occup. Environ. Health 2008; 81(8): 967–974. doi: 10.1007/s00420-007-0290-0 [DOI] [PubMed] [Google Scholar]
- 34.Dales RE, Cakmak S, Judek S, Coates F. Tree pollen and hospitalization for asthma in urban Canada. Int. Arch. Allergy Immunol. 2008; 146(3): 241–247. doi: 10.1159/000116360 [DOI] [PubMed] [Google Scholar]
- 35.Goldman GT, Mulholland JA, Russell AG, Strickland MJ, Klein M, Waller LA, et al. Impact of exposure measurement error in air pollution epidemiology: Effect of error type in time-series studies. Environ. Health 2011; 10:61 doi: 10.1186/1476-069X-10-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rhomberg LR, Chandalia JK, Long CM, Goodman JE. Measurement error in environmental epidemiology and the shape of exposure-response curves. Crit. Rev. Toxicol. 2011; 41(8):651–671. doi: 10.3109/10408444.2011.563420 [DOI] [PubMed] [Google Scholar]
- 37.Dvorin DJ, Lee JJ, Belecanech GA, Goldstein MF, Dunsky EH. A comparative, volumetric survey of airborne pollen in Philadelphia, Pennsylvania (1991–1997) and Cherry Hill, New Jersey (1995–1997). Ann. Allergy Asthma Immunol. 2001; 87(5): 394–404. doi: 10.1016/S1081-1206(10)62921-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
URI is adjusted by adding log-transformed daily URI counts for school-aged children into the main model. Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model. Outdoor pollen is defined as daily counts of > 5th percentile.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Squares are point estimates for relative risks of asthma hospital admissions associated with increases in air pollutants. The dashed lines represent ±10% changes in the point estimates from the main model.
(DOCX)
Data Availability Statement
The data on hospital admissions for asthma and respiratory infections cannot be made publicly available in order to protect private information of the patients. We obtained the asthma hospitalization data from the New York State Department of Health. These restrictions prohibit us from making the minimal data set publicly available. Requests for access to the data can be made to New York State Department of Health (Email: sparcs.requests@health.nv.gov; URL: http://www.health.ny.gov/statistics/sparcs/).