Abstract
Background: The Secretary of Health and Human Services recently released a report calling for the nation to create a national health information network (NHIN) that would interconnect Regional Health Information Organizations (RHIOs). These RHIOs, which others have called Local or Regional Health Information Infrastructures (LHII), would in turn interconnect local as well as national health information resources. Little data exist about the activities taking place in communities to create LHIIs.
Approach: The authors analyzed data that communities submitted in response to a request for capabilities issued by the Foundation for eHealth as part of their Connecting Communities for Better Health program using descriptive statistics and subjective evaluation.
Impression: The authors analyzed data from 134 responses from communities in 42 states and the District of Columbia. Communities are enthusiastic about moving forward with health information exchange to create LHIIs to improve the efficiency, quality, and safety of care. They have identified significant local sources of investment and plan to use some clinical data standards but not as broadly as was expected. The communities have not yet developed the specific technical approaches or the sustainable business models that will be required. Many communities are interested in creating an LHII and are developing the leadership commitment needed to translate that interest into an operational reality. Clinical information standards can be incorporated into a community's plans as often as they need to be. Communities have to overcome funding issues, develop deeper understanding of the technical and organizational issues, and aggressively share their learning to succeed within their community and to help other communities succeed.
The Relevance of Health Information Exchange
Experts have identified health information technology as a key tool in addressing the major challenges that health care faces in efficiency, safety, and quality.1,2,3 The Administration has shown its commitment to health information technology by establishing the office of the National Health Information Technology Coordinator, creating a “Strategic Framework for Action” and providing $139 million in funding for health information technology programs through the Agency for Healthcare Research and Quality. There is also growing consensus among Congressional leaders about the essential role that health information technology can play to address health care challenges as reflected in legislation introduced over the last two years.
Achieving the full benefit of health information technology, including provider order entry, disease management, and clinical decision support, requires clinical data. Much of the clinical data practitioners need comes from “outside” the practitioner's organization4 and the best way to obtain these “outside data” is from an interconnected health information infrastructure rather than trying to create point-to-point, unique connections to each laboratory, radiology center, or referring provider directly. In November 2001, the National Committee on Vital and Health Statistics (NCVHS) called for the creation of a National Health Information Infrastructure (NHII). In July 2004, the Department of Health and Human Services released a Strategic Framework report entitled The Decade of Health Information Technology: Delivering Consumer-centric and Information-Rich Health Care that calls for the creation of a “national health information network” to enable nationwide interoperability as well as “regional health information organizations” (RHIOs), which would provide local leadership, oversight, fiduciary responsibility, and governance for the development, implementation, and application of secure health information exchange across care settings. Others have referred to these organizations as regional or local health information infrastructures that would be the foundation for an interconnected infrastructure of systems, clinical data standards, networks, procedures, and laws that would be required for medical care based on electronic, as opposed to today's primarily paper, records as part of the NHII.5 As policymakers consider the alternatives for nationwide implementation of interoperable health information technology in both the public and private sectors and the state, regional, or local health information exchange organizations that would support it, they have access to almost no objective information about the principles related to the creation and operation of health information exchange organizations and the readiness of communities to create them.
Many experts believe that the NHII will be created by interconnecting a large number of state, regional, or locally based health information exchange organizations not only because most health care is local but also because this approach makes the problem more manageable. Such organizations provide many of the functions and infrastructure of the NHII but for a single region or other nongeographic community rather than for the entire nation. In addition, such organizations in turn provide the infrastructure for connecting patients, providers, hospitals, and health care institutions locally.
This is not an entirely new concept. The Community Health Information Networks (CHINs) of the 1990s were an early attempt to create interoperability at the local level. Many of them failed. The reasons they failed include inadequate buy-in and conflicting missions, lack of trust, the need for centralized databases and desire for control, data ownership issues, lack of financing, and the high cost of network technology. Subsequently, a few communities have created pilot or operational health information exchange organizations. Indianapolis, IN6,7 has created an operational health information infrastructure, while others, including the Santa Barbara County Care Data Exchange, have piloted them (Santa Barbara County, CA8,9). Improvements in hardware, software, network technology, and clinical information standards have eliminated some of the barriers to creating health information organizations. The Senior Advisor, National Health Information Infrastructure in the Department of Health and Human Services, recently completed an analysis of these efforts from an organizational change perspective.10
It is important to understand the level of interest and activity in creating health information organizations across the United States because they will probably be one of the key building blocks of the NHII. Using data from a national program created to foster health information exchange (HIE), we have created a profile of communities that are attempting to create interoperability through health information organizations.
Connecting Communities for Better Health
The eHealth Initiative Foundation (<www.ehealthinitiative.org>) launched the Connecting Communities for Better Health Program (CCBH) (<http://ccbh.ehealthinitiative.org/>) in cooperation with the Health Services and Resources Administration to assist communities that are attempting to develop health information organizations at either the state, regional, or local level. The goals of the CCBH Program are to:
Raise awareness and demonstrate the importance of health information exchange (HIE) and its impact on quality, safety, and efficiency to drive public and private sector interest in supporting communities who are engaged in such activities
Highlight the technical, financial, organizational, legal, and clinical challenges communities face in deploying health information exchange (HIE); mobilize community pioneers and national experts to develop tools and resources to address such challenges; and widely disseminate this information to provide support to these communities
Provide concrete assistance to communities through funding and technical support
Provide a communications vehicle (the Community Learning Network) that will enable communities and stakeholders to share information and take steps toward the use of IT and health information exchange
Request for Capabilities Development
The CCBH Program created a request for capabilities (RFC) instrument. The CCBH staff created the initial draft of the RFC instrument by developing questions to explore seven dimensions that an expert Review Panel had judged to be important determinants of a community's success in creating a health information exchange. The program staff circulated the draft questions to the expert Review Panel (Appendix 1) for review. The staff refined the RFC based on the Panel's feedback. The entire Technical Review Committee then discussed and revised the RFC. The final RFC (<http://www.connectingcommunities.org>) consisted of 37 questions including several multipart questions. There were 60 true/false data elements, 24 numeric elements and 32 fixed-length free text data elements (Appendix 2, available as an online data supplement at www.jamia.org).
Request for Capabilities Announcement/Advertising
The CCBH Program widely disseminated the RFC availability. We sent e-mails to 839 recipients representing individuals, government agencies, national associations, and national organizations interested in health information exchange (▶) who were encouraged to broadly disseminate this information to their membership. Two hundred one (201) of these individuals had a focus within a particular state. The staff posted information about the program on the eHealth Initiative Foundation and HRSA Telehealth Information Network Web sites, published it in the Federal Register, and made announcements at dozens of public meetings. Communities were motivated to respond because the CCBH Program only considered those who submitted proposals for financial support though communities were encouraged to submit a response even if they were not planning to seek support.
Table 1B.
Number of Replies and E-Mail Recipients (Replies/Recipients) Who Were Stakeholders in a Specific State or the District of Columbia Versus those Recipients With a National Scope of Interest
| AL | 2/1 | GA | 4/0 | MD | 5/5 | NJ | 2/2 | SC | 0/11 |
| AK | 2/0 | HI | 2/0 | MA | 1/20 | NM | 0/2 | SD | 1/0 |
| AZ | /0 | ID | 2/3 | MI | 10/6 | NY | 12/11 | TN | 4/9 |
| AR | 3/0 | IL | 3/3 | MN | 2/9 | NC | 4/11 | TX | 3/2 |
| CA | 13/31 | IN | 5/14 | MS | 0/1 | ND | 0/0 | UT | 0/6 |
| CO | 4/2 | IA | 2/2 | MO | 0/2 | OH | 9/3 | VT | 1/0 |
| CT | 2/5 | KS | 1/2 | MT | 2/0 | OK | 1/0 | VA | 1/0 |
| DE | 0/0 | KY | 1/3 | NE | 2/0 | OR | 1/6 | WA | 2/9 |
| DC | 3/3 | LA | 3/0 | NV | 0/0 | PA | 7/9 | WI | 1/3 |
| FL | 2/3 | ME | 0/2 | NH | 1/0 | RI | 1/0 | WV | 1/0 |
| WY | 0/0 |
Many more individuals in states became aware of the RFC through the 638 contacts to individuals, companies and organizations that had a national focus.
Table 1A.
Breakdown by E-Mail Recipient Category
| E-mail Recipient Type | Number |
|---|---|
| National Associations | 110 |
| Government Agencies | 57 |
| Individuals | 117 |
| National Organizations | 354 |
| State Focused | 201 |
| Total | 839 |
CCBH staff solicited responses to the RFC through public announcements, Web site postings, and e-mails to individuals representing national organizations, corporations with a national presence, government agencies, and individuals who they identified as having an interest in HIE. Many of these organizations broadcast the e-mail to their membership and posted information on their Web sites.
Respondents created accounts and entered information into Web-based forms created for the CCBH RFC and, when respondents saved the form, the system stored their responses in a database. The firm managing the Web site extracted the data from the underlying database as comma-delimited files, and CCBH staff converted it to an Access® database. CCBH staff then created additional coded entries for each community, based on their review of the respondents' text entries for questions about technical approach and respondent organizational type. CCBH did not attempt to validate the respondents' data in any way.
We used Microsoft Excel® to create data summaries using the program's descriptive statistical functions (count, sum, and standard deviations) and pivot table functions to explore the relationships between parameter pairs using cross tabulations of counts. In addition, we read all text responses a minimum of three times and recorded our global impressions.
Respondent Communities' Readiness for Health Information Exchange
Connecting Communities for Better Health Program received 134 RFC responses from 42 states and the District of Columbia that we judged sufficiently complete to include in the analysis. Communities that responded to the RFC had made substantial progress in organizing themselves to create a health information organization. Given the time and effort required to complete the RFC and the relatively advanced organizational stage that the RFC required, we believe there are likely to be two or three times as many communities that are interested in developing health information exchange but that did not complete an application. The communities that did respond represent a broad cross section of geography and organization types.
Respondents reported that almost a quarter (22%) of their HIE efforts were in a “beta” stage, 28% operating in pilot mode and 28% in general availability. They described the remaining 22% as being at other stages including conceptual. Of those respondents that described themselves as operational (64), only nine (9) could be described as operational on the basis of careful review of the full RFC response. While few communities were ready to create their HIE, the RFC asked a number of detailed questions about architecture, patient linking, and clinical information standards to better understand the technical approaches the communities were considering.
Organizational Phase
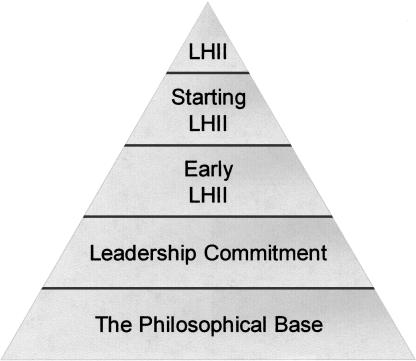
Dr. Nancy Lorenzi has proposed five organizational development stages in evolution of a health information exchange organization or “LHII” (▶).10 The majority of respondent communities were struggling to make the transition from a philosophical base to a leadership commitment stage.
Figure 1.
Developmental LHII stages.10
Almost all of the respondents described the problem they were trying to solve in terms of bringing more information and tools to providers to improve the quality and efficiency of care. Sometimes they focused on care for specific conditions, such as asthma or diabetes, or special populations but usually on a broader population.
Five percent of respondents were at the conceptual stage and had not yet created an organizational structure; 28% described themselves as a loose affiliation; and, 29% had a corporate structure. The remainder of respondents had various organizational structures including mixed models.
The most common type of organization that responded was “other” (28%), followed by hospitals (23%), provider organizations (16%), and academic medical centers (10%). Only 9% of proposals came from dedicated community health information exchange organizations and 2% from public health departments. The majority of respondents were organizations that described themselves as collaborations or coalitions that had evolved to solve local health care problems. These collaborations often were limited in scope, involving a few community health centers, a health department, and a hospital, for example. Such limited participation raises the question of how the HIEs could grow beyond the initial collaboration. Similarly, some respondents appeared to have a strong lead organization with a number of weaker organizations “tagging along.” While weaker organizations almost certainly benefit from a strong organization's leadership and resources in this model, it may be difficult to expand the group. Other strong organizations may not be willing to participate because they don't see a benefit and they will not be willing to take a secondary role.
There was often a long list of categories of organizations that were said to participate in the HIE, but the narrative text often failed to indicate how they would be involved. Their absence from the narrative may report an omission due to length restrictions but could also indicate that these organizations were interested and supportive, but the community had not really thought through the details of their involvement.
The RFC asked each respondent to identify a lead organization that would serve as an administrative home for the effort. The types of organizations identified as the lead were very diverse. Hospitals accounted for 23% of responses, provider organizations for 16%, academic health centers for 10%, community HIE organizations for 9%, and “other” for 29%. Professional societies, payers, government, and health departments accounted for less than 5% each. While some clinicians are involved with the community's proposed projects, with rare exceptions, engaging the “rank and file” clinicians remains to be done.
While only 24% of respondents were organized by physician groups, clinicians were cited to be heavily involved at all stages of nearly all the projects, including serving on advisory committees and leading or driving a number of strategies, including requirements development, clinical process change, usability testing, and training and feedback.
Technical Approaches
Database architectures ranged from personal health records (2%) to peer-to-peer (20%), federated databases (3%), and centralized databases (54%). A substantial fraction of respondents (18%) had not yet selected an approach, and 3% were transmitting but not storing video. Some respondents focused on the network connectivity as a critical component of their HIE.
Whereas one reason the CHINs failed was their emphasis on centralized databases, the most common technologic approach the respondents proposed was still a centralized database.11 There are obvious reasons for choosing a centralized database, especially early in an HIE's development to reduce the costs by reducing technical complexity. On the other hand, the few successful examples of health information exchange organizations use federated databases to avoid concerns over data ownership or control and to allow for easier expansion. Starting with a centralized database may be a reasonable initial strategy for a community just starting an HIE if the participants have a high degree of trust and proper management arrangements.
Respondents planned to use a master patient index that links identifiers in different systems 15% of the time and a unique ID 22% of the time. Twelve percent (12%) thought they did not need to do any patient matching. Thirteen percent thought patient matching was not applicable. Other approaches included biometrics (2%), human matching (4%), and hardware tokens (2%). The planned approaches to linking patient data from multiple sources varied considerably, and some respondents did not address how they would overcome challenges resulting from these approaches implying that they may not recognize these barriers. It was not clear, for example, when respondents planned to use an MPI in the “traditional” fashion—performing the look-up and linking when a participant registers a patient in a clinical application—and when they planned to rely on deterministic or probabilistic matching algorithms that developers might build into these products. The most common (31%) approach planned for patient matching was to use four or more data fields for a patient, commonly social security, last name, first name, and date of birth, to match patients from different sources. Deterministic matching approaches were more common than probabilistic approaches.
Data and Standards
More than 80% of respondents' projects were to include inpatient, outpatient, primary care, and specialty care organizations in their HIE efforts, and more than 50% of projects were to include a broad variety of participating data sources including laboratories, health departments, and school-based clinics. While the respondents specifically identified the types of participants that would be included in their HIE, the narrative descriptions often failed to describe how they would be involved. These omissions may have resulted from length restrictions placed on the narrative descriptions. More than 70% of respondents' projects were to use ambulatory visit data, inpatient discharge data, emergency department visit data, and laboratory data. Only 35% of projects were to use prescription data. As expected, respondents planned to incorporate data generated from specialists, diagnostics, and therapeutic interventions, such as gastroenterology and pulmonology data, less commonly.
Communities proposed to implement a broad array of functionality (▶). A majority planned a repository (78%), results delivery (74%), and reminders (71%). Only 6% proposed personal health record functionality. The RFC did not allow the communities to explain how they would implement these functions in detail, but our overall impression was that they were overly ambitious—planning to implement several different kinds of functionality right away rather than focusing on a few that would allow them to get started without overwhelming them.
Table 2.
The RFC Questions Were Created to Characterize Communities Along Seven Dimensions (in Alphabetical Order)
| RFC Question Categories |
|---|
| Clinical component |
| Demonstration of community commitment and leadership |
| Matching funds |
| Overall technical readiness |
| Plans for sustainable business model |
| Use of data standards |
| Use of replicable and scalable tools |
Given the heavy emphasis that CCBH placed on using clinical data standards in the RFC, we were surprised and disappointed that only half of the respondents proposed to use appropriate data coding standards outside of ICD-9 and CPT-4 codes for encounter data. Mirroring the focus on encounter data from hospitals, EDs, and ambulatory care sites, the respondents planned to use ICD-9 (82%) and CPT-4 (73%) more frequently than other data coding standards. Other code systems such as LOINC (38%), SNOMED (41%), and NDC (48%) were planned for fewer HIE projects. While standard codes such as LOINC are not in widespread use in clinical systems, and we might not expect it to be used in the majority of proposals, others such as NDC are in widespread use and still are not included in a majority of proposals. The modest proportion of proposals using appropriate clinical data standards is concerning because it implies that many respondents have a poor grasp of the central role that clinical standards play in health information exchange.
When the categories of data included in the HIE are compared with the vocabulary standards that are going to be used in the project, we were surprised to find that for laboratory, prescription, and pathology data only 50% of respondents planned to use the appropriate standards. More than 95% of respondents planning to include inpatient, outpatient, or emergency room data plan to use relevant vocabulary standards. Only half of respondents planned to use X12 messages for enrollment and claims.
Eighty-three percent (83%) of respondents planned to use HL7 messaging in their HIE. They planned to use other messaging standards, including DICOM (40%), NCPDP (32%) and X12 (39%), in fewer HIEs. Several respondents planned to use XML-based messaging but did not identify the standard they would use.
Initial Funding and Sustainability
Respondents had, on average, identified approximately $1,500,000 in local funding that was available to support their HIE project (▶). Almost one third (32%) of respondents, however, had not identified any funding. Nonprofit organizations were the most commonly identified source of funding (37%); philanthropic organizations were the next most common (23%). Federal source (22%), HIE organizations (18%), states (17%), private sources (12%), and others (11%) were less-frequent sources (▶). Interestingly, the amount of money respondents expected to obtain from “other” sources was highest at $2,000,000 on average. They looked to states for the smallest amount of funding seeking $100,000 on average. ▶ details the expected sources and amounts of initial capitalization that the respondents expect. In total, the respondents identified $203,000,000 in initial funding available to capitalize their HIE efforts with the majority of those funds coming from other sources and nonprofits while they expect approximately 10% to come from federal sources.
Table 3.
Functions Communities Plan to Provide Through their HIE
| Functionality Category | Communities Planning (%) |
|---|---|
| Personal health record | 6 |
| Patient order | 29 |
| Other | 35 |
| Patient e-mail | 36 |
| Electronic laboratory reporting for public health | 44 |
| Alerts | 45 |
| Public health surveillance | 46 |
| Case management | 52 |
| Quality reporting | 56 |
| Enrollment | 61 |
| Office electronic medical records | 62 |
| Consultations | 68 |
| Reminders | 71 |
| Result delivery | 74 |
| Repository | 78 |
Table 4.
Expected Sources and Amounts of Initial Capitalization Sources
| Source | Proportion of Respondents (%) | Average Expected Amount (Thousands) |
|---|---|---|
| Federal programs | 21 | $600 |
| State government | 16 | $200 |
| Philanthropies | 23 | $800 |
| HIE organizations | 19 | $550 |
| Nonprofit (including hospitals) | 36 | $1,300 |
| Private sources | 13 | $300 |
| Other source | 12 | $2,000 |
| No source identified | 32 |
Once operational, 60% of respondents expected sources other than subscriber fees, source fees, grants, or fees from payers to be important revenue sources accounting for 63% of their income. Subscribers were the second most commonly mentioned source of revenue (45%) accounting for 52% of total revenues. Revenue from data sources (20%), government (20%), and pay-for-performance programs (18%) were less-often cited by respondents who expected them to account for 22%, 28%, and 30% of total revenues, respectively. The most common source of revenues that communities anticipated building on was “other”—revenue other than subscriber fees, local government support, data source fees, or pay-for-performance revenues.
A minority of respondents plan to move forward with their HIE even if they do not receive funding from the CCBH program, but the majority of projects will not move forward without external funding. Despite impressive local commitments, there is a funding gap. Collectively, the 134 proposed projects would require $1.2 billion to complete, or an average of $11 million each over three years. The size of the proposed projects varied greatly.
Limitations
We need to be cautious when we interpret the results for two reasons. First, while the CCBH program broadly disseminated information about the request for capabilities and encouraged any community thinking about developing a health information exchange to reply, not every community responded. Second, because responses to the RFC were the basis for an invitation to submit a Request for Proposal for funding, communities may have been optimistic in their responses to the RFC.
Outlook
There is an exciting level of interest in health information exchange. This interest is present in almost every state, in urban and rural settings, and in many different types of organizations. These communities will need more than interest to succeed, however, and the excitement could easily wane if there is no progress in the next several years. With continued strong leadership, clear guidance regarding standards and architectures, appropriate sharing of information, and financial models that will assure sustainability, we can capitalize on the excitement and make substantive progress toward creating local health information exchanges.
Appendix 1. Review Panel Members
Philanthropies
Carol Diamond, MD, MPH, Markle Foundation
Sam Karp, California Healthcare Foundation
John Lumpkin, MD, MPH, Robert Wood Johnson Foundation
Private Sector
David Brailer, MD, PhD, HealthTech*
Francois deBrantes, General Electric Corporate Benefits
Seth Foldy, MD, City of Milwaukee Public Health Department
John Glaser, PhD, Partners HealthCare System
Martin Harris, MD, Cleveland Clinic
Blackford Middleton, MD, Center for Information Technology Leadership
Russ Ricci, MD, HealthSTAR Communications
Helga Rippen, MD, PhD, RAND
Jonathan Teich, MD, PhD, Brigham & Womens Hospital, HealthVision
Federal Agencies
Claire Broome, MD, Centers for Disease Control and Prevention
Carol Haberman, Health Resources and Services Administration
Eduardo Ortiz, MD, Agency for Healthcare Research and Quality
Dena Puskin, Health Resources and Services Administration
Bill Rollow, MD, Centers for Medicare and Medicaid Services
Bill Yasnoff, MD, PhD, National Health Information Infrastructure, Department of Health and Human Services
Scott Young, MD, Agency for Healthcare Research and Quality
Supplementary Material
Presented in part at the eHealth Initiative Annual Meeting, Washington, DC, December 16, 2003.
Supported by Contract # 1D1B TH01027-01-00 from the Health Services Research Administration.
Footnotes
currently National Coordinator for Health Information Technology
References
- 1.Institute of Medicine. Fostering Rapid Advances in Healthcare: Learning from System Demonstrations. Washington, DC: National Academy Press; 2002.
- 2.Detmer D. Building the national health information infrastructure or personal health, health care services, public health and research. BMC Medical Informatics and Decision Making. 2003, 3(1). Available at: http://www.biomedcentral.com/1427-6947/3/1. Accessed Mar 16, 2004. [DOI] [PMC free article] [PubMed]
- 3.Institute of Medicine. Fostering Rapid Advances in Health Care: Learning from System Demonstrations. November 19, 2002. Washington, DC; National Academy Press, 2002. [PubMed]
- 4.Overhage JM, McDonald CJ. Patient Information Management Systems in ACP. Guide to Computers in Medicine. In: Oshcroft J, editor. Computers in Clinical Practice: Managing Patients, Information and Communication. Philadelphia: American College of Physicians, 1995.
- 5.Yasnoff WA, Humphreys BL, Overhage JM, et al. Consensus action agenda for achieving the National Health Information infrastructure. J Am Med Inform Assoc. 2004;11(4):332–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Overhage JM, Tierney WM, McDonald CJ. Design and implementation of the Indianapolis Network for Patient Care and Research. Bulletin of the Medical Library Association. 1995;83(1):48–56. [PMC free article] [PubMed] [Google Scholar]
- 7.Overhage JM, Dexter PR, Perkins SM, et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med. 2002;39(1):14–23. [DOI] [PubMed] [Google Scholar]
- 8.Brailer DJ. Connection tops collection. Peer-to-peer technology lets caregivers access necessary data, upon request, without using a repository. Health Management Technology. 2001;22(8):28–9. [PubMed] [Google Scholar]
- 9.Anonymous. Moving Toward Electronic Health Information Exchange: Interim Report on the Santa Barbara County Data Exchange California Healthcare Foundation, July 2003.
- 10.Lorenzi N. Strategies for Creating Successful Local Health Information Infrastructure Initiatives. Report to the Senior Advisor, National Health Information Infrastructure. Washington, DC: Department of Health and Human Services; 2003.
- 11.MacDonald K, Metzger J. First Consulting Group, Connecting Communities: Strategies for Physician Portals and Regional Data Sharing—Including Results from a Recent Survey by the College of Healthcare Information Management Executives (CHIME), March 2004.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.