Abstract
Objective: To evaluate the patterns of e-Health use over a four-year period and the characteristics of users.
Design: Longitudinal, population-based study (1999–2002) of members of a prepaid integrated delivery system. Available e-Health services included ordering prescription drug refills, scheduling appointments, and asking medical questions.
Measurements: Rates of known access to e-Health services, and of e-Health use each quarter.
Results: The number of members with known e-Health access increased from 51,336 (1.6%) in 1999 to 324,522 (9.3%), in 2002. The percentage of households in which at least one person in the household had access increased from 2.7% to 14.1%. Among the subjects with known access, the percentage of subjects that used e-Health at least once increased from 25.7% in 1999 to 36.2% in 2002. In the multivariate analysis, subjects who had a low expected clinical need, were nonwhite, or lived in low socioeconomic status (SES) neighborhoods were less likely to have used e-Health services in 2002. Disparities by race/ethnicity and SES persisted after controlling for access to e-Health and widened over time.
Conclusion: Access to and use of e-Health services are growing rapidly. Use of these services appears to be greatest among persons with more medical need. The majority of subjects, however, do not use any e-Health services. More research is needed to determine potential reasons for disparities in e-Health use by race/ethnicity and SES as well as the implications of these disparities on clinical outcomes.
Introduction
New forms of electronic health care services (e-Health) have tremendous potential for improving the quality and efficiency of health care.1,2,3,4,5,6,7 These innovations in care delivery also could exacerbate disparities in access to care across racial/ethnic or economic groups or between the technologically sophisticated and naïve. As health systems begin providing these new e-Health services, it is important that we evaluate the use of this innovation to understand its benefits, costs, and potential for unintended consequences. Currently, there are limited quantitative data on the patterns of e-Health use or the characteristics of users over time.
The few existing reports suggest that early adopters of e-Health services are not representative of the general population and that there may be a digital divide across racial/ethnic and economic groups.8 These reports, however, tend to rely on self-reported data without independent confirmation and focus on general use of the Internet rather than use of specific services. Even fewer studies provide data on e-Health use that is linked to other medical care for the patient. Detailed quantitative data on use of e-Health services within the context of patients' existing medical care would be valuable for understanding the magnitude of potential effects and for identifying problem areas as health care decision makers develop, implement, and refine their information technology strategies.4
We conducted a longitudinal, population-based evaluation of the use of e-Health services in a large, integrated delivery system (IDS). We hypothesized that use of these services would increase rapidly over time. We also hypothesized that there would be significant variation in e-Health use across patient sociodemographic characteristics during the initial time period, but that any digital divide would narrow over time as a greater percentage of health system members started using the services and after adjusting for access to these Web-based services.
Methods
Design, Setting, and Population
Kaiser Permanente–Northern California (KPNC) is an IDS serving Northern California. More than three million members receive comprehensive medical care through 18 medical centers with attached outpatient facilities, and 14 freestanding outpatient facilities. This longitudinal population study included all persons who were KPNC members at any point in time between January 1999 and December 2002. We examined each member's ability to access the e-Health services and actual use of services over a four-year period (1999–2002). We obtained all data from KPNC automated databases and the 2000 U.S. Census. The IDS databases include information on e-Health access and use, membership status, individual sociodemographic characteristics, chronic conditions, and comorbidity status. The KPNC Institutional Review Board approved the study.
Electronic Health (e-Health) Services
To use any of the e-Health services, members must register for access by requesting a secure password-protected account through a Web site. After receiving a request and verifying the information, the IDS sent a randomly generated personal identification number (PIN) to the member's home address. Members then created a personal password after entering the PIN on the Web site. Using their password and medical record number, subjects could use any of the e-Health services either for themselves (personal use) or for another member for whom they had the correct medical record number (proxy use).
During the study, KPNC members could use a Web-based secure portal (www.kponline.org) to request routine primary care visit appointments and order refills of prescription drugs. Members also could ask semistructured medical or prescription drug questions. Within 24 hours, a nurse would respond to medical questions, and a pharmacist would respond to drug questions. The advice nurse also had access to patients' lists of prescription drugs and clinical response templates. The advice nurse and pharmacist services were available in 1999 and did not change during the study period. The appointment request service also started in 1999; in the fourth quarter of 2001, the service changed to allow real-time scheduling of primary care appointments. The online refill service started in January 2001. For the fourth quarter of 2002, we only had use data for the appointment scheduling service and the drug refill service. Use of these services accounted for approximately 96% of total use over the first three quarters of 2002. There was no electronic medical record with patient access during the study period.
Measures of Access and Use
To measure known access, we determined the number of subjects who had requested a PIN, i.e., used the Web site to request an account, or who used an e-Health service through a proxy during each quarter of the study period. In addition, we had four variations in the definition of access: (a) subjects who had requested a PIN only; (b) subjects who used their PIN to create a personal password; (c) subjects who had a family member who requested a PIN; and (d) subjects who had a family member who either had requested a PIN or had used an e-Health service through a proxy. We used these definitions to assess the range of subjects who were likely to have had online access. We defined a household as all the members sharing the same primary insurance account number. In this article, we present the data using the first access definition; we also provide a graph using the household definition (d), which provides an upper bound for subjects with known access. The relationships between individual characteristics and access or use did not change when we used the other definitions.
To measure current use, we calculated the number of subjects who used any of the available e-Health services during each quarter of the study period. To determine cumulative use, we calculated the number of subjects who used any service during the current or any previous quarter during the study period. To determine the proportion of users, we used the number of active IDS members during the relevant quarter as the denominator.
Individual Characteristics
We determined subjects' age (0–17, 18–29, 30–49, 50–64, 65–74, and 75+ years old) and insurance type during each study year. The three insurance types were Medicaid, Medicare, and commercial insurance. If the individual had dual status of Medicaid and Medicare, we classified the subject as having Medicaid. If an individual had both Medicare and employer-supplemented insurance, we classified the subject as having Medicare. We evaluated membership status in each quarter between 1999 and 2002. We assessed race/ethnicity using a combination of automated data on inpatient care and routine patient satisfaction surveys. If there were multiple records, we used the most recent information. We have incomplete race/ethnicity data because this information is not routinely collected on all members. We classified subjects with missing race/ethnicity information as unknown. We performed analyses in which we classified subjects with missing information as either white or nonwhite to assess the sensitivity of our analyses to the missing data.
To assess expected need for medical services, we created a dichotomous indicator of clinical need using a diagnosis-based index (prospective DxCG score), which has been adopted by the Centers for Medicare and Medicaid Services (CMS) for Medicare payment risk adjustment.9,10 For each year, we classified subjects with a DxCG score above the median as having a high expected need for medical services, i.e., expected clinical resource use. We also evaluated whether each subject was a member of the IDS's chronic disease registries in each year from 1999 to 2002 for five diseases: diabetes mellitus (DM), congestive heart failure (CHF), coronary artery disease (CAD), asthma, and hypertension (Htn). The disease registries use data on prescription drugs, laboratory results, outpatient diagnoses, and inpatient diagnoses to identify members with each chronic disease. Similarly, using the automated databases, we determined whether each subject had a regular primary care provider (PCP) in each year during the study period.
We obtained neighborhood socioeconomic status (SES) information from the 2000 U.S. Census at the block group level. We used MapMarker Plus Version 8.3.0.37 to create geocodes based on the member's address. We linked each member to his or her census-block group, i.e., subdivisions of the census tracts, which contain an average of 1,000 inhabitants. For patients with missing addresses or without geocodes (3.6%), we recorded the census-block group as missing data. We then created a dichotomous indicator of low SES (yes/no) based on the 2000 census-block group data. We defined a census-block group as low SES when ≥20% of residents had household incomes below the federal poverty level or when ≥25% of residents 25 years and older had less than a high-school education.11
Statistical Analysis
We used bivariate and multivariate logistic regression models to assess access to and use of e-Health services at both the individual and household levels. Patient-related independent variables included age category, gender, race/ethnicity, neighborhood SES, and having a high expected need for medical services (DxCG comorbidity score). System-related independent variables included having a PCP and insurance type. We examined e-Health access and use in relation to each of these variables in bivariate analyses among all active KP members, as well as use among members with known access. We then included the independent variables in multivariate logistic regression models for each study year. We repeated all analyses using indicators for five chronic diseases, instead of the DxCG score. We also repeated all analyses in subjects continuously enrolled as of January 1999, i.e., a fixed cohort, to better control for time of exposure to KPNC's e-Health services. The results were similar for all analyses across these methods and for each year. Given these similarities, we present only the models for 2002 using the DxCG score and using the dynamic population (i.e., subjects could leave and enter throughout the study), which represent the most current data and best reflect the actual levels of use.
Finally, we used logistic regression models to examine trends in use during the four-year study period among groups of patients with different races/ethnicities, adjusting for our covariates. We modeled quarterly use in a logistic regression model, using the explanatory variables of race/ethnicity, time (from 1 to 16), time-squared, and an interaction term between race/ethnicity and time, and adjusted for covariates. We used a generalized estimating equations approach with a first-order autoregressive covariance structure to account for the potential correlation between time points of a common trend. We conducted a similar analysis for patients by SES. We performed all analyses using SAS version 8.2.
Role of the Funding Sources and the Health System
The Internet Services Group, which managed KP's e-Health services, assisted in the data collection and initial study design. Neither the health system nor the funding agency had a role in the analysis, interpretation of data, or the decision to submit this article for publication. The views expressed in this article represent the views of the authors and do not represent the views of AHRQ, the federal government, the University of California, or KP.
Results
Individual Characteristics and e-Health: Access and Use
In 2002, there were 3,482,152 members in the IDS, compared with 3,213,571 members in 1999. Of the members in 2002, 324,522 (9.3% of all subjects) had documented e-Health access, i.e., they had known access either because they went online for an account or had used services through another subject's (proxy) account; this represents a 632% increase (= 324,522/51,336) in the number of subjects with known access compared with 1999 (n = 51,336; 1.6%).
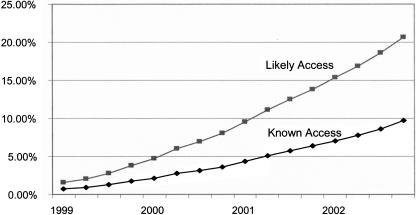
▶ depicts the percentage of subjects with known access in each quarter between 1999 and 2002 (lower curve). The graph also depicts the percentage of subjects who had known household access (upper curve), i.e., they were members of a household in which at least one member had known access. Given that the IDS permitted members to use e-Health services through a proxy, the household estimate provides an approximate upper boundary of subjects with ready access to e-Health services.
Figure 1.
Access to e-Health services over time (1999–2002). Access to e-Health services over time using two definitions of access. The lower curve (diamonds) indicates the percentage of subjects with known access, i.e., either having gone online to request an account or having prior use of e-Health services through another member's account (proxy). The upper curve (squares) indicates the percentage of subjects who likely had access through their household, i.e., at least one member of the household had known access. We calculated access (%) as the number of subjects with access divided by the number of subjects who were active IDS members in each quarter.
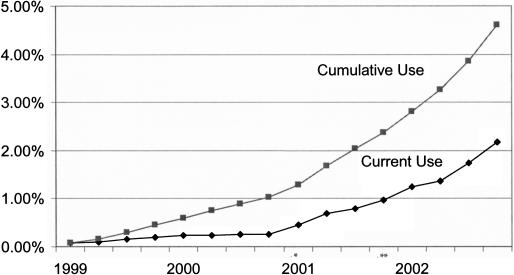
There were 117,174 subjects (3.4% of all subjects and 35.9% of subjects with known access) who used e-Health services at least once during 2002, an 884% increase (= 117,174/13,261) in the number of subjects compared with 1999 (n = 13,261; 0.4% of all subjects and 25.7% of subjects with known access). ▶ depicts the percentage of all members who had any e-Health service use during the study and in each quarter between 1999 and 2002. The figure also displays the introduction dates of new e-Health services during the study. In addition to the increase in the percentage of subjects with any use, the mean number of uses per year among users also increased from 1.5 to 3.9 uses/year/subject between 1999 and 2002 (1.5, 1.6, 3.1, and 3.9 per year, respectively; p < 0.0001). Similarly, the percentage of users with four or more uses in a single year also increased from 4.6% to 29.6% (p < 0.0001) over the four-year period. By the end of the study period, the appointment scheduling service had the largest number of users (n = 31,158 in the third quarter of 2002), followed by the drug refill service (n = 29,469), medical advice service (n = 4,039), and pharmacy advice service (n = 888).
Figure 2.
e-Health users (1999–2002). The definition of current users (calculated as a percentage) is the number of subjects who have used any e-Health service in each quarter divided by the total number of subjects in the quarter (diamonds in lower curve). The definition of cumulative users (calculated as a percentage) is the number of subjects who have ever used any e-Health service during the study divided by the total number of subjects in the quarter (squares in upper curve). *Introduction of a prescription drug refill service in first quarter of 2001. **Introduction of real-time online appointment scheduling in fourth quarter of 2001.
▶ lists the individual characteristics of the subjects in 2002. The table also describes the number and percentage of subjects with each characteristic who had known access to and who had used e-Health services at least once during 2002. As expected, there were variations in the percentage of subjects with use and known access across individual characteristics in the bivariate analyses. For example, use was most common in subjects age 50–64 years, followed by subjects age 65–74 and 30–49 years. Use also was more common among female subjects, subjects with a chronic disease, subjects with a high expected need for clinical services, subjects with a PCP, subjects living in a high SES neighborhood, and subjects with Medicare insurance (p < 0.0001 for all differences). Finally, use was most common among whites, followed by other race/ethnicity, Asians, blacks, and Hispanics. Similar relationships were observed between individual characteristics and use of e-Health services, among subjects with known access to these services.
Table 1.
Subjects with Known Access to and Who Used e-Health Services by Individual Characteristics (2002)
| Total (N) | Known Access |
Used |
|||
|---|---|---|---|---|---|
| Characteristics | N | % | N | % | |
| Total no. | 3,482,152 | 324,522 | 9.3 | 117,174 | 3.4 |
| Age, yr | |||||
| 0–17* | 829,006 | 22,509 | 2.7 | 9,898 | 1.2 |
| 18–29* | 564,526 | 52,910 | 9.4 | 15,807 | 2.8 |
| 30–49 (R) | 1,072,438 | 127,919 | 11.9 | 41,009 | 3.8 |
| 50–64* | 607,640 | 82,182 | 13.5 | 33,802 | 5.6 |
| 65–74* | 228,060 | 26,203 | 11.5 | 11,497 | 5.0 |
| 75+* | 180,482 | 12,799 | 7.1 | 5,161 | 2.9 |
| Gender | |||||
| Male | 1,700,950 | 113,324 | 6.7 | 37,065 | 2.2 |
| Female* | 1,781,202 | 211,198 | 11.9 | 80,109 | 4.5 |
| Ethnicity | |||||
| White (R) | 1,076,163 | 154,270 | 14.3 | 61,130 | 5.7 |
| Black* | 148,272 | 10,186 | 6.9 | 3,261 | 2.2 |
| Hispanic* | 258,579 | 14,225 | 5.5 | 4,529 | 1.8 |
| Asian* | 243,705 | 23,873 | 9.8 | 8,244 | 3.4 |
| Other race/ethnicity* | 84,735 | 8,644 | 10.2 | 2,945 | 3.5 |
| Unknown race/ethnicity* | 1,670,698 | 113,324 | 6.8 | 37,065 | 2.2 |
| History of CAD* | 89,013 | 11,464 | 12.9 | 5,076 | 5.7 |
| No history of CAD | 3,393,139 | 313,058 | 9.2 | 112,098 | 3.3 |
| History of heart failure* | 38,216 | 4,226 | 11.1 | 1,794 | 4.7 |
| No history of heart failure | 3,443,936 | 320,296 | 9.3 | 115,380 | 3.4 |
| History of hypertension* | 413,503 | 55,303 | 13.4 | 25,027 | 6.1 |
| No history of hypertension | 3,068,649 | 269,219 | 8.8 | 92,147 | 3.0 |
| History of diabetes mellitus* | 185,022 | 24,158 | 13.1 | 10,539 | 5.7 |
| No history of diabetes mellitus | 3,297,130 | 300,364 | 9.1 | 106,635 | 3.2 |
| History of asthma* | 345,537 | 41,684 | 12.1 | 16,319 | 4.7 |
| No history of asthma | 3,136,615 | 282,838 | 9.0 | 100,855 | 3.2 |
| High expected clinical need (DxCG)* | 1,735,169 | 198,360 | 11.4 | 75,967 | 4.4 |
| Low expected clinical need (DxCG) | 1,746,983 | 126,162 | 7.2 | 41,207 | 2.4 |
| Have a regular PCP* | 2,229,353 | 280,532 | 12.6 | 101,821 | 4.6 |
| No regular PCP | 1,252,799 | 43,990 | 3.5 | 15,353 | 1.2 |
| Live in low SES neighborhood* | 908,595 | 51,858 | 5.7 | 17,584 | 1.9 |
| Live in high SES neighborhood | 2,448,489 | 268,734 | 11.0 | 98,416 | 4.0 |
| Commercial insurance (R) | 3,043,374 | 286,425 | 9.4 | 101,033 | 3.3 |
| Medicaid insurance* | 61,147 | 1,900 | 3.1 | 646 | 1.1 |
| Medicare insurance* | 377,631 | 36,197 | 9.6 | 15,495 | 4.1 |
(R) = reference group, indicated when relevant; CAD = coronary artery disease; DxCG = comorbidity score; PCP = primary care provider; SES = socioeconomic status.
p-Value < 0.0001 in bivariate logistic regression models, sociodemographic, clinical, and insurance characteristics of subjects in 2002. We defined subjects as having known e-Health access if they either had gone online to request an account or had used services through another subject's account (proxy use). We defined subjects as having used e-Health services if they had used any of the services at least once during the year. All percentages are row percentages, i.e., within each characteristic, the number of subjects with access/use out of the total number of subjects with that characteristic. In addition, 3.6% of subjects either did not have an address or had an address without a corresponding geocode, which we classified as missing.
Households and e-Health: Access and Use
There were 1,926,298 IDS households in 2002 compared with 1,720,538 households in 1999. Of the households in 2002, 271,479 (14.1% of all households) had at least one member with known access, an increase of 576% (= 271,479/47,144) from 1999 (n = 47,144; 2.7% of all households). Similarly, 90,095 households had at least one member who used e-Health services during the year (4.7% of all households and 33.2% of households with known access); this represented an increase of 788% (= 90,095/11,430) from 1999 (n = 11,430; 0.66% of all households, and 24.2% of households with known access).
▶ lists the characteristics of households in the IDS. In bivariate analyses, households living in high SES neighborhoods were more likely to have known access and e-Health use (access: odds ratio [OR] = 1.91, 95% confidence interval (CI) = 1.89–1.93; use: OR = 1.97, 95% CI = 1.94–2.00), as were households with at least one member with a high expected need for clinical services (access: OR = 1.39, 95% CI = 1.37–1.40; use: OR = 1.57, 95% CI = 1.54–1.59). Households with children were slightly more likely to have access (OR = 1.17, 95% CI = 1.16–1.18).
Table 2.
Families with Known Access to and with Use of e-Health Services by Individual Characteristics (2002)
| Total (N) | Known Access |
Used |
|||
|---|---|---|---|---|---|
| Characteristics | N1 | (%N1/N) | N2 | (%N2/N) | |
| Total no. of families | 1,926,298 | 271,479 | 14.1 | 90,095 | 4.7 |
| Families living in low SES neighborhood | |||||
| Yes* | 549,943 | 50,094 | 9.1 | 15,542 | 2.8 |
| No | 1,376,355 | 221,385 | 16.1 | 74,553 | 5.4 |
| Families with ≥1 family member < 18 yr old | |||||
| Yes* | 488,944 | 75,926 | 15.5 | 20,929 | 4.3 |
| No | 1,437,354 | 195,553 | 13.6 | 69,166 | 4.8 |
| Families with ≥1 family member ≥65 yr old | |||||
| Yes* | 354,262 | 37,370 | 10.5 | 15,011 | 4.2 |
| No | 1,572,036 | 234,109 | 14.9 | 75,084 | 4.8 |
| Families with ≥1 family member with a high expected clinical need (DxCG) | |||||
| Yes* | 1,307,443 | 200,068 | 15.3 | 68,900 | 5.3 |
| No | 618,855 | 71,411 | 11.5 | 21,195 | 3.4 |
Sociodemographic and clinical characteristics of families in the integrated delivery system first available information during the given year (age is calculated at the end of the given year). The definition of access to e-Health services is having a household member with known access, i.e., either having gone online to request an account or having prior use of e-Health services through a member with an account (proxy). All percentages are row percentages, i.e., for each characteristic, the number of subjects with access/use out of the total number of subjects with that characteristic.
SES = socioeconomic status; DxCG = comorbidity score; N1 = subjects with known access; N2 = subjects with use of e-Health services.
p-Value < 0.0001 in bivariate logistic regression models.
Characteristics Associated with e-Health Use
▶ depicts the individual characteristics associated with e-Health use in 2002. In these multivariate models, subjects who were female, had a high expected need for clinical services or had a regular PCP were significantly more likely to use e-Health services. Subjects who were age 50–64 years also were more likely to use services compared with the reference group of subjects age 30–49 years. In contrast, subjects age 75 years or older were least likely to use services, followed by subjects age 17 years or younger, age 65–74, and age 18–29 years. Similarly, subjects with Medicaid were significantly less likely to use services, as were subjects with Medicare, when compared with subjects with commercial insurance.
Table 3.
Association of e-Health Service Use and Individual Characteristics in 2002
| All Subjects |
Subjects with Known Access |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age, yr | ||||
| 0–17 | 0.84 | 0.81–0.87 | 2.41 | 2.31–2.52 |
| 18–29 | 0.94 | 0.93–0.96 | 0.97 | 0.94–0.99 |
| 30–49 | Reference Group | Reference Group | ||
| 50–64 | 1.11 | 1.09–1.13 | 1.37 | 1.35–1.40 |
| 65–74 | 0.89 | 0.85–0.92 | 1.38 | 1.32–1.45 |
| 75+ | 0.45 | 0.43–0.47 | 1.16 | 1.09–1.23 |
| Gender | ||||
| Male | Reference Group | Reference Group | ||
| Female | 1.17 | 1.16–1.19 | 1.08 | 1.07–1.10 |
| Race/ethnicity | ||||
| White | Reference Group | Reference Group | ||
| Black | 0.44 | 0.42–0.46 | 0.77 | 0.74–0.80 |
| Hispanic | 0.38 | 0.37–0.39 | 0.78 | 0.75–0.81 |
| Asian | 0.63 | 0.61–0.64 | 0.88 | 0.85–0.90 |
| Other race/ethnicity | 0.64 | 0.62–0.67 | 0.83 | 0.79–0.87 |
| Unknown race/ethnicity | 0.49 | 0.48–0.50 | 0.89 | 0.87–0.90 |
| Expected need for clinical services | ||||
| Low (DxCG) | Reference Group | Reference Group | ||
| High (DxCG) | 1.35 | 1.33–1.37 | 1.14 | 1.12–1.16 |
| Primary care provider (PCP) | ||||
| Did not have regular PCP | Reference Group | Reference Group | ||
| Had a regular PCP | 2.68 | 2.61–2.76 | 1.41 | 1.36–1.45 |
| Neighborhood SES | ||||
| High | Reference Group | Reference Group | ||
| Low | 0.60 | 0.59–0.61 | 0.94 | 0.92–0.96 |
| Unknown | 0.42 | 0.40–0.45 | 0.78 | 0.73–0.84 |
| Insurance type | ||||
| Commercial | Reference Group | Reference Group | ||
| Medicaid | 0.46 | 0.42–0.49 | 0.91 | 0.83–1.01 |
| Medicare | 0.93 | 0.89–0.96 | 1.09 | 1.04–1.14 |
Logistic models of sociodemographic, clinical, and insurance characteristics associated with access to e-Health services. We defined subjects as having known e-Health access if they either had gone online to request an account or had used services through another subject's account (proxy use).
OR = odds ratio; CI = confidence interval; DxCG = comorbidity score; SES = socioeconomic status.
Given that differences in e-Health access affect use, we also examined use among subjects with known access. In these multivariate models of use given known access, subjects who were female, had a high expected need for clinical services, or had a regular PCP continued to be significantly more likely to use e-Health services. In contrast, subjects who were age 50 years or older or age 17 years or younger now were more likely to use services compared with the reference group of subjects age 30–49 years. Subjects with Medicare also were more likely to use services given known access. These associations were robust across multiple analytic approaches, e.g., using chronic disease indicators instead of the DxCG score or using different age categories.
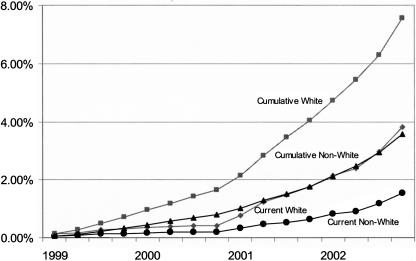
Disparities in Use across Races/Ethnicities
▶ depicts the unadjusted percentage of white and nonwhite subjects with e-Health use over the study period. The lower set of curves represents white and nonwhite users among all subjects in each quarter between 1999 and 2002. The top set of curves represents cumulative use during the study among white and nonwhite users. ▶ depicts the adjusted differences in use in 2002 across race/ethnicity categories. In the multivariate models of use among all subjects, all the nonwhite subjects were significantly less likely to use e-Health services compared with whites in 2002. Even after limiting the analyses to subjects with known e-Health access, the nonwhite subjects remained significantly less likely to use the services. These associations were robust across multiple analytic approaches, including recoding subjects with unknown race/ethnicity as white and using only white and nonwhite categories. Although use increased among all categories, the rate of use increased faster for whites compared with nonwhites, thus accounting for the increasing disparity in e-Health use across races/ethnicities. During the four-year study period, nonwhites were less likely to use e-Health services compared with whites (OR = 0.53, 95% CI = 0.45–0.62), and this gap widened during the four-year study period (OR = 0.96 per year, 95% CI = 0.93–1.00), after adjusting for covariates including SES.
Figure 3.
Current and cumulative users (1999–2002) by race/ethnicity. The definition of current users (calculated as a percentage) is the number of subjects who have used any e-Health service in each quarter divided by the total number of subjects in the quarter (lower curves of current users: whites [diamonds] and nonwhites [circles]). The definition of cumulative use (calculated as a percentage) is the number of subjects who have ever used e-Health services during the study divided by the total number of subjects in the quarter (upper curves of cumulative user: whites [squares] and nonwhites [triangles]).
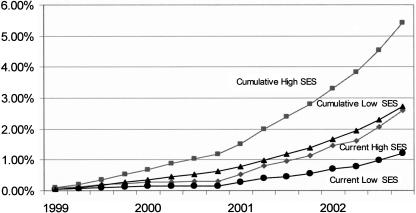
Disparities in Use by Socioeconomic Status
There also were differences in use by SES (▶). In the multivariate models, subjects living in low SES neighborhoods were significantly less likely to have used services (OR = 0.60, 95% CI = 0.59–0.61) in 2002. After limiting the analysis to subjects with known e-Health access, the low SES subjects still were less likely to have used services in 2002 but to a lesser degree (OR = 0.94, 95% CI = 0.92–0.96). Reclassifying subjects with unknown SES as high SES did not change any of the associations. ▶ depicts the unadjusted percentage of high and low SES subjects with e-Health use over the study period. The rates of use increased faster for high SES compared with low SES, resulting in an increasing relative disparity in e-Health use across SES. As in the analyses by race/ethnicity, during the four-year study period, low SES members were less likely to use e-Health services compared with high SES members (OR = 0.71, 95% CI = 0.61–0.84), and this gap widened over time (OR = 0.95 per year, 95% CI = 0.92–0.98), after adjusting for covariates including race/ethnicity.
Figure 4.
Current and cumulative users (1999–2002) by socioeconomic status (SES). The definition of current users (calculated as a percentage) is the number of subjects who have used any e-Health service in each quarter divided by the total number of subjects in the quarter (lower curves of current users: high SES [diamonds] and low SES [circles]). The definition of cumulative use (calculated as a percentage) is the number of subjects who have ever used e-Health services during the study divided by the total number of subjects in the quarter (upper curves of cumulative users: high SES [squares] and low SES [triangles]).
Discussion
In this study of use of e-Health services over time in a well-defined population within an integrated system of care, our findings suggest that both access to and use of e-Health services are growing rapidly over time. Most persons, however, do not use e-Health services, even among those with known access. Not surprisingly, persons who are more likely to need health care tended to use the new electronic services more frequently compared with persons less likely to need health care. The findings also suggest that there is a significant and growing digital divide with respect to e-Health services across racial/ethnic and SES groups. These disparities persist even within an insured, integrated delivery system without any additional charges for e-Health services and despite general increases in the percentage of the population with access. To our surprise, these disparities were present in the population with established access to e-Health services.
It is important to note that e-Health services fundamentally are health care services delivered through new channels. Not everyone needs medical services, even among those who register for access, nor does everyone who needs services require them frequently. A recent study by Baker et al.12 found that most persons (78%) who reported prior use of the Internet for health information only used the Internet for health-related purposes sporadically. The low level of e-Health use suggests that much work is needed before these new services achieve their promise for improving quality and efficiency for the majority of Americans.13,14 Alternatively, the findings are reassuring given concerns that lower transaction costs associated with e-Health also could have led to a deluge of inappropriate patient use.
The apparent growing digital divide by race/ethnicity and by SES is concerning. Although the absolute numbers of nonwhite and low SES e-Health users is increasing over time, the numbers of white and high SES users was higher at baseline and is growing at a faster rate. In other words, this relative disparity not only persists as more persons start using e-Health services but actually widens over time. The findings reflect the growing body of literature suggesting a digital divide.12,15,16,17,18,19 In contrast to our findings, in a cross-sectional telephone interview study of Internet use for health information, Brodie et al.20 found that the divide in use by SES and by race/ethnicity disappeared once they adjusted for differences in Internet access. The discrepancy in findings could be a function of the differences in the types of service, definitions of use, or methods of data collection.
Further research is needed to confirm this growing divide as well as to assess the impact of this disparity in e-Health use on clinical outcomes. In addition, determining the root causes of these differences in use will be critical for informing policy decisions. In this study, we were able to investigate basic access to the online services as a potential cause. In future efforts, individual-level information on education, computer literacy, and income may help disentangle the effects of race/ethnicity and SES on e-Health use. Other potential explanations for disparities in use include differences in the quality or speed of the Internet connection (e.g., access at home vs. work, speed of the connection); the perceived value of the e-Health services, care delivery or other cultural preferences, or the level of trust and privacy concerns; or lags in the current location on similar adoption curves.
Our findings differ from other studies in several other important respects. First, we focused on use of actual e-Health services within an integrated system of care rather than on more nonspecific definitions such as use of the Internet for any health-related purpose or for seeking health information.12,15,21,22 In addition, we examined the proportion of use in the entire population rather than in a self-selected sample of subjects. Thus, it is not surprising that our estimates of use are lower than those of other published reports.12,13,16,23 As future studies examine the potential impacts of e-Health on quality, safety, and efficiency, focusing on e-Health services that are integrated with other forms of health care may be valuable. We also used a range of more stringent definitions of access, e.g., known access to services, which provide reasonable upper and lower boundaries of access. In addition, our study also examined use among households, which may provide an additional insight into “real-world” use, especially as more families engage in proxy use for children or elderly members. Finally, this study collected electronic data on actual e-Health service use rather than relying on self-reported data, which removes concerns about information bias that are common in other evaluations of patient behavior.
Some limitations of our study are that it did not capture individual measures of education, health beliefs, knowledge, trust in the health system, preferences for care, or awareness of the services. The use of neighborhood SES represents a reasonable proxy for individual SES; similarly, the known e-Health access represents a proxy of awareness. Other areas for further study include the usability of the e-Health services, the perceived need for specific services, and the value of e-Health services compared with alternatives (relative utility). Nevertheless, the findings persisted among patients with chronic diseases and high levels of expected need for clinical services; also, if present, the potential limitations would tend to bias toward a null result. The completeness and quality of the race/ethnicity data also could influence the study. The findings, however, were robust even after classifying all the subjects with missing data as white. In addition, the distribution of nonmissing race/ethnicity data resembles the distribution on survey and interview data from previous research studies. If there were a bias toward underreporting nonwhite race/ethnicity, this would tend to bias the results toward the null.
Other limitations include the relatively small number of e-Health services available in this IDS, and, conversely, the number of alternatives to e-Health services available in the IDS, such as through telephone call centers. Based on the patterns of use after the introduction of the drug refill service and real-time appointment scheduling, the addition of new e-Health services with high relative utility could drive increases in use considerably. These data also do not address subject preferences for the availability of the e-Health services or the perceived or real value of the services to patients who are using them. Finally, whether the disparities in e-Health use result in differences in access or clinical outcomes deserves additional study.
In short, access to and use of e-Health services are growing rapidly over time. Despite this growth, the number of users is only a small percentage of potential users, and even fewer are using services on a regular basis. There also appear to be increasing and significant disparities in e-Health use between persons of white and nonwhite race/ethnicity and between persons of low and high SES. These disparities were present even among persons with known access to these services. Given the potential of e-Health services to improve the quality and efficiency of health care delivery, more research is needed to understand why rates of use are low, particularly among some SES and racial/ethnic groups. In addition, as e-Health services improve and mature, information is needed on whether these disparities in use persist and on the impact of these trends on patient health, safety, and resource use.
This research was performed by the Kaiser Foundation Research Institute through the support of the Agency for Healthcare Research and Quality (AHRQ) under Contract 290-00-0015, Task Order No. 8. The authors of this article are solely responsible for its contents. No statements or views in this article should be construed as official positions of AHRQ, the U.S. Department of Health and Human Services, Department of Veterans Affairs, or the Federal government.
References
- 1.Institute of Medicine. The Computer-based Patient Record: An Essential Technology for Health Care. Washington, DC: National Academy Press, 1997. [PubMed]
- 2.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001. [PubMed]
- 3.Goldsmith J. The Internet and managed care: a new wave of innovation. Health Affairs. 2000;19:42–56. [DOI] [PubMed] [Google Scholar]
- 4.Robinson TN, Patrick K, Eng TR, Gustafson D. An evidence-based approach to interactive health communication: a challenge to medicine in the information age. Science Panel on Interactive Communication and Health. JAMA. 1998;280:1264–9. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson T. Digital doctoring—opportunities and challenges in electronic patient-physician communication. JAMA. 1998;280:1361–2. [DOI] [PubMed] [Google Scholar]
- 6.Mandl KD, Kohane IS, Brandt AM. Electronic patient–physician communication: problems and promise. Ann Intern Med. 1998;129:495–500. [DOI] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? JAMA. 2003;290:259–64. [DOI] [PubMed] [Google Scholar]
- 8.Eng TR, Maxfield A, Patrick K, Deering MJ, Ratzan SC, Gustafson DH. Access to health information and support: a public highway or a private road? JAMA. 1998;280:1371–5. [DOI] [PubMed] [Google Scholar]
- 9.Ash AS, Ellis RP, Pope GC, et al. Using diagnoses to describe populations and predict costs. Health Care Financ Rev. 2000;1:7–28. [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao Y, Randall PE, Ash AS, et al. Measuring population health risks using inpatient diagnoses and outpatient pharmacy data. Health Serv Res. 2001;36:180–93. [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker L, Wagner TH, Singer S, Bundorf MK. Use of the Internet and e-mail for health care information: results from a national survey [erratum appears in JAMA. 2003;290:334]. JAMA. 2003;289:2400–6. [DOI] [PubMed] [Google Scholar]
- 13.Pew Internet & American Life Project. Wired for Health: How Californians Compare to the Rest of the Nation: A Case Study Sponsored by the California HealthCare Foundation. Washington, DC: The California HealthCare Foundation, 2003.
- 14.Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care. Am J Manag Care. 2002;8:, 4277–33. [PubMed]
- 15.Mandl KD, Feit S, Pena BM, Kohane IS. Growth and determinants of access in patient e-mail and Internet use. Arch Pediatr Adolesc Med. 2000;154:508–11. [DOI] [PubMed] [Google Scholar]
- 16.Murray E, Lo B, Pollack L, et al. The impact of health information on the Internet on the physician–patient relationship. Arch Intern Med. 2003;163:17–27. [DOI] [PubMed] [Google Scholar]
- 17.Fogel J, Albert SM, Schnabel F, Ditkoff BA, Neugut AI. Use of the Internet by women with breast cancer. J Med Internet Res. 2002;4:E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dickerson S, Reinhart AM, Feeley TH, et al. Patient Internet use for health information at three urban primary care clinics. J Am Med Inform Assoc. 2004;11:499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz SJ, Moyer CA, Cox DT, Stern DT. Effect of a triage-based E-mail system on clinic resource use and patient and physician satisfaction in primary care. A randomized controlled trial. J Gen Intern Med. 2003;18:736–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Affairs. 2000;19:255–65. [DOI] [PubMed] [Google Scholar]
- 21.Pew Internet & American Life Project. The Ever-shifting Internet Population: A New Look at Internet Access and the Digital Divide. Washington, DC: The California HealthCare Foundation, 2003.
- 22.Novak TP, Hoffman DL. Bridging the Digital Divide: The Impact of Race on Computer Access and Internet Use. 1998.
- 23.U.S. Department of Commerce. Falling Through the Net II: New Data on the Digital Divide. Washington, DC: U.S. Department of Commerce, 1998.