Abstract
Objective
The purpose of this pilot study was to (1) obtain preliminary data on changes in burden and quality of life in head and neck cancer caregivers during and shortly following patient radiotherapy, (2) assess the relationship between perceived social support and burden as well as perceived social support and quality of life in caregivers during radiotherapy, and (3) identify preferences for sources of support among caregivers during radiotherapy.
Methods
Caregivers completed burden and quality of life instruments at the start of patient radiotherapy (T1), 5 weeks into radiotherapy (T2), and 1 month post-radiotherapy (T3) and instruments for perceived social support and support preferences at T2 only.
Results
Caregivers showed a trend toward increased burden and worsened quality of life for the majority of subscales at T2 or T3 than at T1. Caregivers reported significantly lower esteem and significantly greater disruption at T2 than at T1 and significantly worse health at T3 than at T2. Higher perceived social support was typically associated with lower burden and higher quality of life at T2. Spouses/partners were the most commonly preferred source of support.
Discussion
These pilot findings suggest that caregivers experience psychosocial impairments during and shortly after patient radiotherapy, but more research using larger samples is warranted.
Keywords: Head and neck cancer, caregiving, radiotherapy, burden, quality of life
Introduction
About 3.5 million people provide informal care to cancer patients.1 Studies have overwhelmingly demonstrated poor quality of life (QOL) among cancer caregivers,2 but few studies have evaluated QOL and related psychosocial functioning among caregivers for people with head and neck cancer (HNC). Although HNC accounts for only ~3% of the cancer burden in the United States with an expected 61,760 diagnoses in 2015, the disease and its associated treatment can have overwhelming consequences for patients and their informal caregivers.3,4 For example, >75% of patients experience some form of swallowing difficulty (dysphagia) during or after treatment,5,6 which may result in complicated feeding (including nonoral feeding), coughing or choking upon swallowing, and difficulty breathing and speaking.4,7 Collectively, these symptoms significantly impede core aspects of daily life for HNC patients, necessitating significant responsibilities for informal caregivers and the need for better understanding caregivers’ psychosocial functioning.
Radiotherapy is time-consuming for HNC patients and their caregivers, and it is often supplemented with additional treatment or services such as chemotherapy, speech therapy, and nutrition counseling.8 Promoting caregiver wellbeing during this time may contribute to better outcomes for patients (e.g. physical and emotional functioning) and the health care system (e.g. lower discharge delays),9 but very little is known about caregiver QOL and their perceived burden during patient treatment for HNC. One pilot study10 suggested that HNC caregivers experience increased burden 3 weeks after the patient’s radiotherapy. Caregivers’ self-reported health also decreased at this time, but improved when patients finished radiation. Although informative, this study was limited by a small sample size and the use of non-cancer-specific caregiver burden and QOL instruments.10 Another study11 also followed HNC caregivers during patient radiotherapy; they found that although burden remained relatively stable, psychological distress increased and was highest at week 5. Although these studies suggest impaired psychosocial functioning in some domains for HNC caregivers during patient radiotherapy, their mixed findings regarding patterns of burden warrant further investigation. Additionally, others studies of psychosocial functioning among HNC caregivers were predominantly cross sectional and focused on the post-treatment period, providing little insight into the radiotherapy treatment period when toxicity accumulates and side effects increase.9,12,13
Similarly, we know little about HNC caregivers’ perceived social support during radiotherapy, including how it is related to caregivers’ burden and QOL, as well as who caregivers prefer to turn to for support. Research14,15 has shown that social support was related to schedule disruption, a perceived negative caregiving experience, and overall unmet supportive care needs in HNC caregivers. Whom caregivers prefer to turn to for support may have implications for the types of supportive care interventions developed. The Theory of the Social Care System16,17 posits that individuals seek support from biological family members and spouses first, and, when these are unavailable, that caregivers seek support from friends (including neighbors), but it is unclear if this is true for HNC caregivers. Many HNC caregivers recognize the importance of maintaining social contact, but 43% fail to do so.18 Further, one study reported that one-third of caregivers never call for help when experiencing excessive caregiving demands.18 A more recent study15 indicated that HNC caregivers perceived more support from family members than from health professionals. Thus, perceived social support and support-seeking behaviors may have implications for the HNC caregiving experience and development of supportive care interventions; however, more information is needed about these constructs during patient radiotherapy, when caregivers are managing patients’ intense treatment regimen and symptom burden.
Current evidence regarding the psychosocial functioning of HNC caregivers is sparse, limited to only a few prospective evaluations and studies using measures nonspecific to cancer caregiving. Further, most studies have focused on caregivers of patients post-treatment, not during radiotherapy.9 The limited evidence suggests that HNC caregivers experience psychosocial impairments, but more studies are needed to understand these issues during patient radiotherapy to determine if and at what time supportive care interventions are needed for caregivers The purpose of this pilot study was to (1) obtain preliminary data on changes in burden and quality of life in head and neck cancer caregivers during and shortly after patient radiotherapy, (2) assess the relationship between perceived social support and burden as well as perceived social support and QOL among caregivers during radiotherapy, and (3) identify caregivers’ preferences for sources of support during patient radiotherapy. We hypothesized that burden and QOL would worsen during patient radiotherapy and would improve following radiotherapy. In addition, we hypothesized that higher perceived social support would be associated with lower burden and better QOL.
Methods
Participants
Caregivers of patients with HNC were recruited from an outpatient radiation clinic at an academic medical center over 8 months. Patients with HNC referred for radiotherapy were identified by the attending radiation oncologist and subsequently approached by a clinical researcher. Patients were asked to identify an informal caregiver. The study researcher obtained written informed consent from interested caregivers who were (1) providing informal (unpaid) care for a HNC patient with planned external beam radiotherapy with or without chemotherapy with a curative intent, and (2) between the ages of 21 and 90 years. Caregivers were excluded if they (1) had a current cancer diagnosis, and (2) were unable to communicate in English.
Procedure
Caregiver socio-demographics and comorbidities, and patient disease and treatment-related variables including treatment type (radiotherapy or combined chemoradiation), AJCC tumor stage, tumor location, and diagnosis type (new/recurrent) were recorded at the start of radiotherapy through an intake interview and medical chart review. Caregivers completed burden and QOL instruments at the beginning of radiotherapy (T1), 5 weeks into radiotherapy (T2), and 1 month post-radiotherapy (T3) and two social support instruments at T2. The study was approved by the local Institutional Review Board.
Measures
Caregiver burden
The Caregiver Reaction Assessment (CRA)19 was used to assess caregiver burden. This instrument evaluates positive and negative aspects of caregiving using 5 subscales: (esteem; lack of family support; and impact on finances, schedule, and health, respectively). The instrument has 24 items, uses a 5-point Likert scale (strongly disagree to strongly agree), and includes subscale scores only. Higher scores correspond to greater burden or esteem, depending on the subscale. The instrument has established construct validity and internal reliability and is recommended for assessing caregiver burden.20 Internal reliability for the subscales at T1 was excellent (Impact on finances α = 0.90), good (Impact on health α = 0.78; Impact on schedule α = 0.72), or acceptable (Lack of family support α = 0.69; Esteem α = 0.61).
Caregiver quality of life
The Caregiver Quality of Life Index-Cancer scale (CQOLC)21 was used to measure QOL (burden, disruptiveness, positive adaptation, and financial concerns). The instrument has 35 items and uses a 5-point Likert scale (not at all to very much), with higher scores indicating better QOL. The CQOLC was developed and tested in cancer caregivers, and has demonstrated construct validity, internal consistency, and test–retest reliability. It has been strongly recommended as a QOL assessment for cancer caregivers.20 Internal reliability at T1 was good (overall QOL α = 0.86; Burden α = 0.87; Disruptiveness α = 0.75; Finances α = 0.78) or acceptable (Positive adaptation α = 0.69).
Caregiver perceived social support and support preferences
The Medical Outcomes Study (MOS) Social Support Survey22 was used to assess perceived availability of social support (emotional/informational, tangible, positive social interaction, and affectionate). This 19-item instrument uses a 5-point Likert scale (none of the time to all of the time), and higher scores represent greater perceived social support. This scale has been used in caregiver populations with demonstrated good internal reliability, test-retest reliability, and convergent and discriminant validity.22 Internal reliability for this instrument was excellent (α’s ≥ 0.93). Caregivers also completed a modified measure of support preferences.23 This questionnaire assesses respondents’ preferred sources of support (spouse/partner, other family, friend, neighbor, formal agency, no one/myself) for nine hypothetical situations in which they might require assistance (borrowing money, house or child care, filling out a form, and assistance with legal decisions); caregivers indicated their first and second choices for each situation.
Data analysis
Descriptive statistics (means, standard deviations, and standard errors) and graphic analyses were used to depict distribution, assumptions, and potential outliers for burden and QOL at all three time points. Burden, QOL, and perceived social support were treated as continuous variables. Repeated measures ANOVA or the equivalent nonparametric Friedman analysis (for skewed data) were used to assess differences in burden and QOL at T1, T2, and T2. Pairwise comparisons were selected to identify which time points were significantly different. All hypothesis testing was performed at a two-sided 0.05 level. Relationships between social support and burden as well as social support and QOL were evaluated using bivariate Pearson’s correlations or the equivalent nonparametric Spearman’s correlation. The most common first and second preferences for sources of support were identified by calculating percentages for each source of support. All analyses were performed using SPSS, version 21.0.
Results
Participants
Fifty-six caregivers were approached for study recruitment and 39 provided informed consent to participate. Five caregivers withdrew before completing their T1 assessment. Thirty-four caregivers completed T1 assessments, 32 completed T2 assessments, and 28 completed T3 assessments. Participant loss (approximately 28%) was due to caregivers feeling overwhelmed (n = 8), patient’s being medically unable to finish radiotherapy (n = 1), and patient death (n = 2) (Table 1).
Table 1.
Participant characteristics at study entry (n = 34).
| Age (years) Variable |
M = 57 n |
SD = 14.32 % |
|---|---|---|
| Relationship to patient | ||
| Spouse/partner | 25 | 74% |
| Gender | ||
| Female | 29 | 85% |
| Race | ||
| White | 30 | 88% |
| Other | 4 | 12% |
| Ethnicity | ||
| Not Hispanic/Latino | 32 | 94% |
| Education | ||
| < High School Degree | 1 | 3% |
| High School/GED | 10 | 29% |
| College/Tech. Degree | 17 | 50% |
| Graduate School | 6 | 18% |
| Income | ||
| ≤29,999 | 10 | 29% |
| 30,000–59,999 | 10 | 29% |
| ≥60,000 | 13 | 38% |
| Not reported | 1 | 3% |
| Employment | ||
| Not employed | 18 | 53% |
| Comorbidity | ||
| Yes | 13 | 38% |
| Treatment | ||
| Radiation only | 11 | 32% |
| Combined chemoradiation | 23 | 68% |
| Prior surgery | 13 | 38% |
| AJCC Stage | ||
| 0 | 2 | 6% |
| I | 3 | 9% |
| II | 2 | 6% |
| III | 6 | 18% |
| IV | 18 | 52% |
| Not staged | 3 | 9% |
| Recurrence | ||
| Yes | 3 | 9% |
AJCC: American Joint Committee on Cancer.
Change in burden and quality of life
Descriptive statistics for the burden, QOL, and social support subscales are shown in Table 2. Caregivers showed a trend toward increased burden and worsened QOL for the majority of subscales at T2 or T3 than at T1. Caregivers showed a significant change in two of the burden subscales, including esteem (F(2, 26) = 3.82, p = 0.04, ) (Figure 1(a)) and impact on health= (F(2, 26) = 7.66, p = 0.002, ) (Figure 1(b)). Caregivers’ esteem was significantly worse at T2 versus T1 (p = 0.01, d = 0.47), and caregivers had a greater impact on their health at T3 than at T2 (p = 0.02, d = −0.15). Among the QOL subscales, there was a significant time effect in caregivers’ disruption (X2(2) = 7.58, p = 0.02) (Figure 1(c)). Caregivers reported significantly more disruption at T2 than at T1 (p = 0.02).
Table 2.
Descriptive statistics for caregiver burden, QOL, and social support.
| Scale | T1 M (SD) (n = 34) | Range | T2 M (SD) (n = 32) | Range | T3 M (SD) (n = 28) | Range |
|---|---|---|---|---|---|---|
| CRA | ||||||
| Esteem | 4.47 (0.42) | 3.57–5.00 | 4.23 (0.54) | 3.29–5.00 | 4.37 (0.48) | 3.29–5.00 |
| Family support | 1.98 (0.62) | 1.00–3.00 | 2.20 (0.90) | 1.00–4.80 | 2.14 (1.00) | 1.00–5.00 |
| Finances | 2.79 (1.13) | 1.00–5.00 | 2.70 (1.17) | 1.00–4.67 | 2.68 (1.27) | 1.00–5.00 |
| Schedule | 3.15 (0.83) | 1.60–4.80 | 3.26 (0.93) | 1.00–4.60 | 3.19 (0.91) | 1.20–5.00 |
| Health | 2.07 (0.81) | 1.00–4.00 | 2.23 (0.88) | 1.00–4.25 | 2.51 (0.93) | 1.00–4.75 |
| CQOLC | ||||||
| QOL total | 92.14 (18.43) | 44.69–124.00 | 92.94 (19.12) | 55.00–128.00 | 89.51 (24.42) | 44.00–128.00 |
| Burden | 23.21 (7.93) | 5.00–35.00 | 25.38 (7.51) | 12.00–40.00 | 24.54 (8.72) | 7.00–37.00 |
| Disruptiveness | 22.15 (4.45) | 13.00–28.00 | 20.72 (4.67) | 12.00–28.00 | 20.75 (6.00) | 5.00–28.00 |
| Positive adaptation | 17.47 (4.99) | 8.00–25.00 | 17.03 (5.43) | 2.00–26.00 | 16.82 (6.20) | 6.00–27.00 |
| Financial | 8.35 (3.06) | 1.00–12.00 | 8.63 (3.21) | 3.00–12.00 | 8.93 (3.40) | 0.00–12.00 |
| MOS SS | ||||||
| SS Total | – | – | 3.73 (1.04) | 1.37–5.00 | – | – |
| Affectionate | – | – | 4.07 (1.11) | 2.00–5.00 | – | – |
| Positive social | – | – | 3.75 (1.12) | 1.00–5.00 | – | – |
| Tangible | – | – | 3.52 (1.14) | 1.00–5.00 | – | – |
| Emotional/Informational | – | – | 3.70 (1.05) | 1.50–5.00 | – | – |
CRA: caregiver reaction assessment; CQOLC: caregiver quality of life index-cancer scale; QOL: quality of life; MOS SS: medical outcomes study social support; SS: social support.
Figure 1.
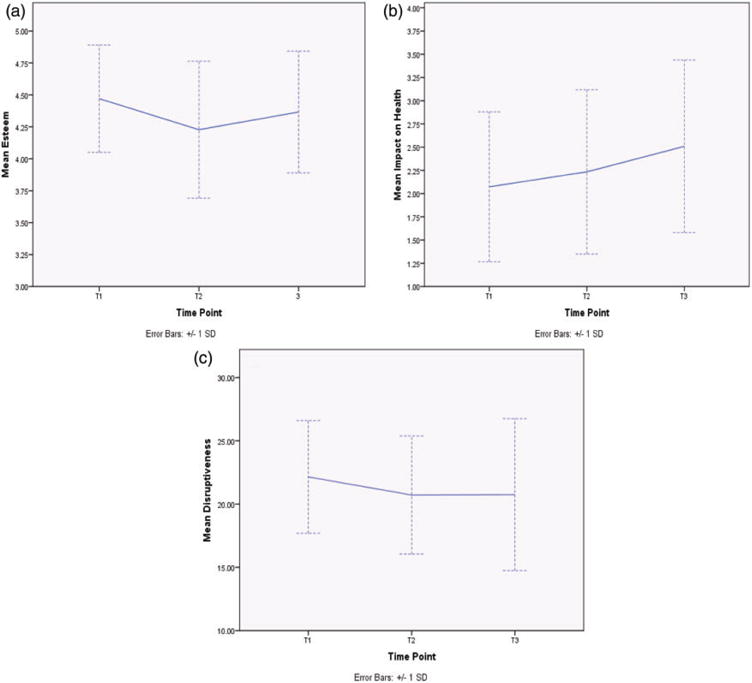
(a) Caregiver Esteem, as measured by the CRA, changed significantly over the treatment period (F(2, 26) = 3.82, p = 0.04, ). (b) Caregiver Impact on Health, as measured by the CRA, changed significantly over the treatment period (F(2, 26) = 7.66, p = 0.002, ). (c) Caregiver Disruptiveness, as measured by the CQOLC instrument, changed significantly over the treatment period (X2(2) = 7.58, p = 0.02).
Relationships between burden and QOL with social support
Correlational analyses (Table 3) demonstrated that greater perceived social support was typically associated with lower burden at T2. Similarly, higher perceived social support was associated with higher overall QOL (r(30) = 0.61, p < 0.001); many QOL and social support subscales mirrored this relationship.
Table 3.
Correlations for social support and burden (n = 32).
| Scales | Overall support | Affectionate support | Positive social support | Emotional/Informational support | Tangible support |
|---|---|---|---|---|---|
| CRA instrument | |||||
| Esteem | NS | rs = 0.35* | rs = 0.36* | NS | NS |
| Lack of family support | rs = −0.62*** | rs = 0.35* | rs = 0.36* | rs = −0.48** | rs = −0.60*** |
| Impact on finances | r = −0.41* | rs = −0.43* | rs = −0.46** | r = −0.38* | r = −0.41* |
| Impact on health | r = −0.48** | rs = −0.52** | rs = −0.53** | r = −0.44** | r = −0.46** |
| Impact on schedule | NS | NS | NS | NS | NS |
| CQOLC instrument | |||||
| Overall QOL | r = 0.61*** | rs = 60*** | rs = 0.53** | r = 0.53** | r = 0.55*** |
| Disruptiveness | r = 0.46** | rs = −0.43* | rs = 0.60*** | r = 0.43** | r = 0.55*** |
| Positive adaptation | r = 0.44** | rs = 0.60*** | rs = 0.53** | r = 0.44** | r = 0.40* |
| Financial | rs = 0.50** | rs = 0.50** | rs = 0.53** | rs = 0.48** | rs = 0.46** |
| Burden | NS | NS | NS | NS | NS |
CRA: caregiver reaction assessment; CQOLC: caregiver quality of life index-cancer scale; QOL: quality of life.
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
Preferences for sources of support
Caregivers’ first preference
Spouses and partners were most often identified as the first preference for each type of support. Caregivers preferred to ask their spouses/partners for help if they suddenly felt ill (73%), needed to borrow money (43%), needed help with house or child care (53%), were lonely and wanted to talk (77%), needed someone to listen (73%), wanted encouragement (67%), needed help filling out a form (47%), wanted medical advice (40%), and needed assistance with legal decisions (47%). However, caregivers’ second source of preferred support varied. “No one/myself” was the most common second preference selected for borrowing money (32%), house or child care (27%), completing a form (29%), and assistance with legal decisions (27%). Caregivers mostly commonly preferred relying on another family member if they suddenly felt ill (29%), wanted encouragement (38%), or medical advice (27%) and most commonly preferred a friend if they were lonely and wanted to talk (44%) or needed someone to listen (38%).
Discussion
This pilot study evaluated burden, QOL, and perceived social support and support preferences among caregivers of patients with HNC during the course of patient radiotherapy. As expected, burden typically worsened once the patient was 5 weeks into radiotherapy (T2) and improved following radiotherapy (T3); however, many of the burden subscales (lack of family support, impact on finances, and impact on schedule) did not significantly change across time points. Caregivers’ esteem was significantly lower at T2 than at T1 and caregivers reported a significantly greater impact on their health at T3 than at T2. Caregivers reported the highest burden for the impact on schedule subscale at all time points. Collectively, these results suggest that HNC caregivers felt considerably less esteem associated with their caregiving role during radiotherapy, and perceived a significantly greater negative impact on their health one month following radiotherapy. Our QOL findings showed significantly more disruption at T2 than at T1. Other QOL subscales (burden, positive adaptation, financial) and overall QOL did not change significantly across the three time points.
Caregivers’ decreased esteem near the conclusion of treatment may have been associated with reduced functional ability in patients and increased care demands. For example, dysphagia is common among HNC patients undergoing treatment, and dysphagia is associated with caregiver distress24 and poorer caregiver QOL.25 While caregivers may initially value their care role, these feelings may attenuate as patients deteriorate and caregivers struggle to support them. Similarly, the increased negative impact on caregivers’ health shortly following treatment may be a consequence of the cumulative stress and burden associated with caregiving. Likewise, a greater impact on health shortly following treatment may reflect caregivers’ neglect of their own personal health care needs.
High schedule burden may reflect the time commitment associated with the patient’s treatment. HNC patients typically have a myriad of medical appointments and are often accompanied by the caregiver. Following treatment, patients and caregivers may undergo a long-term rehabilitation process, and caregivers may continue to experience daily disruptions at this time.4 Similar to the reported high schedule burden, our QOL findings showed that caregivers reported significant disruption in their daily schedules at T2.
These findings are consistent with prior burden and QOL findings reported for cancer caregivers. Our caregiver burden scores at treatment initiation are similar to those reported by Chen et al.14 who assessed caregivers of oral cancer patients soon after surgery. However, caregivers in our study reported much higher esteem than did caregivers in Chen et al.’s report.14 Compared to caregivers in another study focused advanced cancer caregivers (mostly prostate and breast), caregivers in our study reported more burden but better esteem.26
As expected, higher perceived social support was typically associated with lower burden and higher QOL 5 weeks into patient radiotherapy. Caregivers reported that a spouse/partner was the preferred source of support, but the second most preferred source of support varied widely. Many caregivers preferred to be self-sufficient rather than to seek help from others for four of the nine types of support. This is concerning, since most caregivers in this study were providing support to a spouse/partner as the patient.
Our findings of caregivers’ preferences for sources of support in part support the Theory of the Social Care System.16,17 We found that in the absence of a spouse or partner, caregivers prefer to be self-sufficient for some of their support needs. Similarly, in an earlier study, 33% of HNC caregivers never called for help when faced with excessive caregiving demands.18 However, caregivers in that study were more likely to receive support from friends. In our study, caregivers preferred to seek support from a spouse or partner. This discrepancy may stem from the fact that only 20% of caregivers in the earlier study were spouses to the patient, versus 74% in our study.
Strengths
This pilot study has several notable strengths. It was the first to evaluate burden and QOL prospectively at the start of, toward the conclusion of, and one-month after radiotherapy in HNC caregivers. Previous studies focused predominantly on caregivers of patients who were farther out from treatment, when patient care demands and caregivers’ day-to-day activities likely differ from those during the radiotherapy treatment period. We also identified caregivers’ preferences for sources of different types of support during patient radiotherapy, which is important when considering supportive interventions targeted for HNC caregivers during this time period.
Limitations and future research
This study was conducted at a single institution and was limited by a small sample size. Consequently, additional factors that may affect caregiver burden and QOL were not identified or controlled. For example, patient’s disease and treatment characteristics, caregiver’s personal characteristics (e.g. coping mechanisms, availability of supportive resources), and indicators of care intensity (e.g. hours of daily care), may have contributed to resilience or impaired psychosocial functioning during treatment.27,28 Given the pilot nature of this study, we did not apply a Bonferroni correction to the multiple analyses, which increased the chances of testwise error. However, this pilot study was intended to be exploratory and to provide preliminary data on psychosocial functioning at time points previously neglected. We focused on psychosocial functioning in caregivers during and shortly following radiotherapy, although caregiving likely began before and extended long after the period measured. Consequently, this study did not capture true baseline or long-term survivorship burden and QOL outside of the radiotherapy treatment period among HNC caregivers. Perceived social support and support preferences were assessed at one time point, which did not allow for examination of associations among support, burden, and QOL or assessment of support preferences at multiple time points. Finally, caregivers in this study were predominantly highly educated and Caucasian and may have had different experiences than would have members of racial/ethnic minority groups or those with less education. Future studies with larger samples are needed to explore factors associated with burden and QOL among a diverse group of HNC caregivers during and shortly following radiotherapy. Further, future studies should explore perceived social support and support preferences across treatment to identify potential changes over time.
Conclusion and clinical implications
Our findings suggest that HNC caregivers may benefit from psychosocial services during and shortly following patient radiotherapy. Specifically, multimodality interventions that target caregivers’ esteem as well as managing schedule burden, daily disruptions, and their own health needs, should be considered. Additionally, interventions should focus on ways to improve HNC caregivers’ ability to identify sources of support, and know when and how to seek support from others. A critical consideration will be integrating any intervention into caregivers’ schedules, when they have substantial schedule burden and daily disruption.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Paul M., Laura L., and Amy L. Deutsch Endowment in Life Care Planning Award and the Behavioral Science and Community Health Dissertation Award at the University of Florida. Chandylen Nightingale’s work on this manuscript was in part supported by a Cancer Control Traineeship, National Cancer Institute/National Institute of Health (NCI/NIH; R25CA122061).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.National Alliance for Caregiving and AARP. Caregiving in the US. 2009 [Google Scholar]
- 2.Northouse L, Williams AL, Given B, et al. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30:1227–1234. doi: 10.1200/JCO.2011.39.5798. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society. Cancer facts & figures. 2016 [Google Scholar]
- 4.Eades M, Chasen M, Bhargava R. Rehabilitation: Long-term physical and functional changes following treatment. Semin Oncol Nurs. 2009;25:222–230. doi: 10.1016/j.soncn.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Carnaby-Mann G, Crary M, Amdur R. “Pharyngocise”: Randomized controlled trial of preventative exercises to maintain muscle structure and swallowing function during head-and-neck chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83 doi: 10.1016/j.ijrobp.2011.06.1954. [DOI] [PubMed] [Google Scholar]
- 6.Murphy BA, Gilbert J. Dysphagia in head and neck cancer patients treated with radiation: Assessment, sequelae, and rehabilitation. Semin Radiat Oncol. 2009;19:35–42. doi: 10.1016/j.semradonc.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Penner JL. Psychosocial care of patients with head and neck cancer. Semin Oncol Nurs. 2009;25:231–241. doi: 10.1016/j.soncn.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Ward E, van As-Brooks C. Head and neck cancer: Treatment, rehabilitation, and outcomes. 2nd. San Diego, CA: Plural Publishing, Inc; 2014. [Google Scholar]
- 9.Longacre ML, Ridge JA, Burtness BA, et al. Psychological functioning of caregivers for head and neck cancer patients. Oral Oncol. 2012;48:18–25. doi: 10.1016/j.oraloncology.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nightingale CL, Lagorio L, Carnaby G. A prospective pilot study of psychosocial functioning in head and neck cancer patient-caregiver dyads. J Psychosocial Oncol. 2014;32:477–492. doi: 10.1080/07347332.2014.936649. [DOI] [PubMed] [Google Scholar]
- 11.Badr H, Gupta V, Sikora A, et al. Psychological distress in patients and caregivers over the course of radiotherapy for head and neck cancer. Oral Oncol. 2014;50:1005–1011. doi: 10.1016/j.oraloncology.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Givens DJ, Karnell LH, Gupta AK, et al. Adverse events associated with concurrent chemoradiation therapy in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2009;135:1209–1217. doi: 10.1001/archoto.2009.174. [DOI] [PubMed] [Google Scholar]
- 13.Logan RM. Advances in understanding of toxicities of treatment for head and neck cancer. Oral Oncol. 2009;45:844–848. doi: 10.1016/j.oraloncology.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Chen SC, Tsai MC, Liu CL, et al. Support needs of patients with oral cancer and burden to their family caregivers. Cancer Nurs. 2009;32:473–481. doi: 10.1097/NCC.0b013e3181b14e94. [DOI] [PubMed] [Google Scholar]
- 15.Chen SC, Lai YH, Liao CT, et al. Unmet supportive care needs and characteristics of family caregivers of patients with oral cancer after surgery. Psychooncology. 2014;23:569–577. doi: 10.1002/pon.3458. [DOI] [PubMed] [Google Scholar]
- 16.Cantor M. Neighbors and friends: An overlooked resource in the informal support system. Res Aging. 1979;1:434–463. [Google Scholar]
- 17.Cantor MH. Family and community: Changing roles in an aging society. Gerontologist. 1991;31:337–346. doi: 10.1093/geront/31.3.337. [DOI] [PubMed] [Google Scholar]
- 18.Baghi M, Wagenblast J, Hambek M, et al. Demands on caring relatives of head and neck cancer patients. Laryngoscope. 2007;117:712–716. doi: 10.1097/mlg.0b013e318031d0b4. [DOI] [PubMed] [Google Scholar]
- 19.Given CW, Given B, Stommel M, et al. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 20.Deeken JF, Taylor KL, Mangan P, et al. Care for the caregivers: A review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Sympt Manage. 2003;26:922–953. doi: 10.1016/s0885-3924(03)00327-0. [DOI] [PubMed] [Google Scholar]
- 21.Weitzner MA, Jacobsen PB, Wagner H, Jr, et al. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: Development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res. 1999;8:55–63. doi: 10.1023/a:1026407010614. [DOI] [PubMed] [Google Scholar]
- 22.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 23.Cantor M, Brennan M. Growing older in New York in the 1990’s: A study of changing lifestyles, quality of life, and quality of care. New York, NY: Center for Policy on Aging on the New York Community Trust; 1993. [Google Scholar]
- 24.Verdonck-de Leeuw IM, Eerenstein SE, Van der Linden MH, et al. Distress in spouses and patients after treatment for head and neck cancer. Laryngoscope. 2007;117:238–241. doi: 10.1097/01.mlg.0000250169.10241.58. [DOI] [PubMed] [Google Scholar]
- 25.Patterson JM, Rapley T, Carding PN, et al. Head and neck cancer and dysphagia; caring for carers. Psychooncology. 2013;22:1815–1820. doi: 10.1002/pon.3226. [DOI] [PubMed] [Google Scholar]
- 26.Utne I, Miaskowski C, Paul SM, et al. Association between hope and burden reported by family caregivers of patients with advanced cancer. Support Care Cancer. 2013;21:2527–2535. doi: 10.1007/s00520-013-1824-5. [DOI] [PubMed] [Google Scholar]
- 27.Pearlin LI, Mullan JT, Semple SJ, et al. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 28.Sherwood PR, Given BA, Donovan H, et al. Guiding research in family care: A new approach to oncology caregiving. Psychooncology. 2008;17:986–996. doi: 10.1002/pon.1314. [DOI] [PubMed] [Google Scholar]


