Abstract
Autologous cartilage grafting during open airway reconstruction is a complex skill instrumental to the success of the operation. Most trainees lack the adequate opportunity to develop proficiency in this skill. We hypothesized three-dimensional (3D) printing and computer-aided design can be used to create a high-fidelity simulator for developing skills carving costal cartilage grafts for airway reconstruction. The rapid manufacturing and low cost of the simulator allow deployment in locations lacking expert instructors or cadaveric dissection, such as medical missions and third world countries. In this blinded, prospective observational study resident trainees completed a physical simulator exercise using a 3D-printed costal cartilage grafting tool. Participant assessment was performed using a Likert-scale questionnaire and airway grafts were assessed by a blinded expert surgeon. A majority of participants found this to be a very relevant training tool and highly rated the level of realism of the simulation tool.
Keywords: 3D modeling, computer aided design, 3D printing, laryngotracheal reconstruction, surgical training, simulation, tool, anterior graft, posterior graft, costal cartilage, carving
Introduction
Hands-on experience is essential for acquiring and improving surgical skills of new procedures for surgeon trainees. While these skills have historically been acquired in live patients, anaesthetized animals, or human cadavers, surgical simulation is being increasingly recognized as an important tool in surgical training1–4.
Additive manufacturing, or three-dimensional (3D) printing, has potential to augment surgical simulation in Otolaryngology by facilitating production of high-fidelity models through computer-aided design (CAD) for hands-on simulation of complex anatomy or critical procedures1,4–5. When combined with thoughtful material choices, 3D printing can reproduce visuospatial and haptic characteristics of a surgical procedure1.
Airway reconstruction performed for airway stenosis, such as laryngotracheal reconstruction, is a technically demanding procedure where costal cartilage is carved to support and expand a reconstructed trachea. Currently, a surgeon in training has scarce opportunity to carve cartilage grafts in these procedures as this highly critical portion is not amenable to suboptimal outcome. We aimed to investigate the use of 3D printing for production of a lifelike simulation tool for surgical training of carving of costal cartilage grafts for airway reconstruction.
Methods
Following University of Michigan Health System (UMHS) institutional review board exemption, simulation training was conducted during the UMHS Otolaryngology-Head and Neck Surgery Dissection Course.
Production of Simulation Tool
A standardized 3D-printed representation of a harvested human costal cartilage graft was created via segmentation of a computed tomography (CT) scan of a normal 8-year-old pediatric rib via previously published methods6. A negative mold of the model was manufactured out of acrylonitrile butadiene styrene polymer using a fused-deposition modeling 3D printer and the simulation tool fabricated by filling the mold with 2:1 ratio of pure cornstarch and silicone (GE Silicone II White) (Figure 1A–B). The composition of the material has been previously validated by microtia surgeons6.
Figure 1. 3D-Printed Costal Cartilage Simulation for Carving of Airway Grafts.
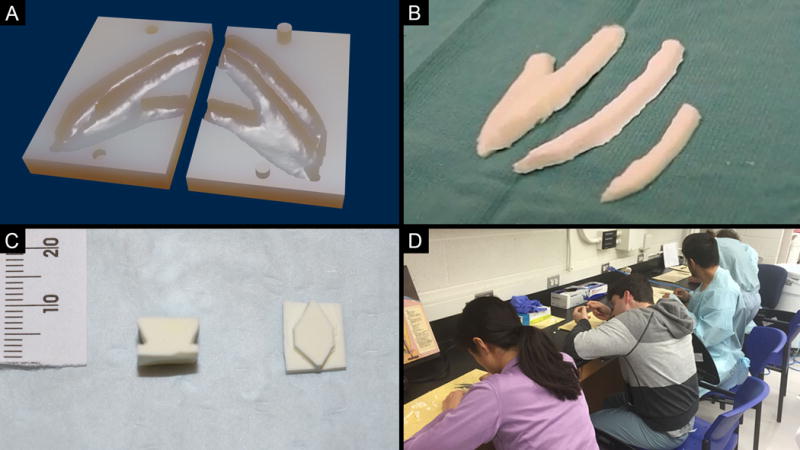
(A) Three-dimensional rendering of stereolithography (.STL) file for the costal cartilage 3D-printed mold. (B) Final costal cartilage simulation tool. (C) Examples of final carved posterior (left) and anterior (right) airway grafts. (D) Trainee participants performing the simulation exercise.
Recruitment and Randomization
All Otolaryngology resident trainees including interns and rotating medical students were invited to participate. Participants were divided per postgraduate year (PGY) and randomized by PGY level into two groups: 1) pre-simulation instructions provided by a single live demonstration by the senior author or 2) single viewing of short instructional video (Video S1–S2). Participants completed the simulator in groups of 5 that were heterogeneous by PGY level and instructional method.
Simulation and Assessment
All participants completed two sequential simulations of carving an anterior and posterior graft for airway reconstruction (Figure 1C–D). After completion, all participants completed a previously-validated 10-item Likert scale survey which had been modified to query about the simulator characteristics (Figure S1A)7.
The final graft carvings were evaluated using a Likert scale assessing accuracy and appropriateness for clinical use by a blinded expert airway reconstructive surgeon (Figure S1B).
Data Analysis
Data was analyzed with SPSS Statistics (SPSS Inc.) software. Independent sample student’s t-test compared the mean between groups. Paired sample student’s t-test was used to compare the means of the variables. ANOVA analysis was used to compare the training level to factors related to the carvings. We defined statistical significance as 5% (α = 0.05).
Results
There were 18 participants (four medical students, two PGY-1, three PGY-2, four PGY-3, two PGY-4, and three PGY-5 trainees) with nine participants randomized per simulation group. 66.7% of trainees had not participated in an airway reconstruction procedure, with the greatest number of exposures by a participant being six operations. Observation of or experience in graft carving prior to the training session did not impact speed or quality of carving (p>0.05).
78% of the participants rated this as a very relevant training tool. Of the residents that had experience in airway reconstruction procedures, 56% reported that the simulation was highly realistic. Of the learners who did not rate the simulator highly, concerns expressed included material heterogeneity and unfamiliarity of the tactile feel of normal pediatric costal cartilage.
Participants’ self-assessments of confidence and efficiency increased with subsequent repetition of the simulation exercise (Figure 2). Both variables were associated with the time to carve both anterior and both posterior grafts (p<0.05 for all analyses), but neither were significantly associated with expert assessments of either attempt of either graft type. Training level did not influence the time it took to carve the grafts. There was no difference in the expert rating between the video demonstration or live demonstration groups for either graft type.
Figure 2.
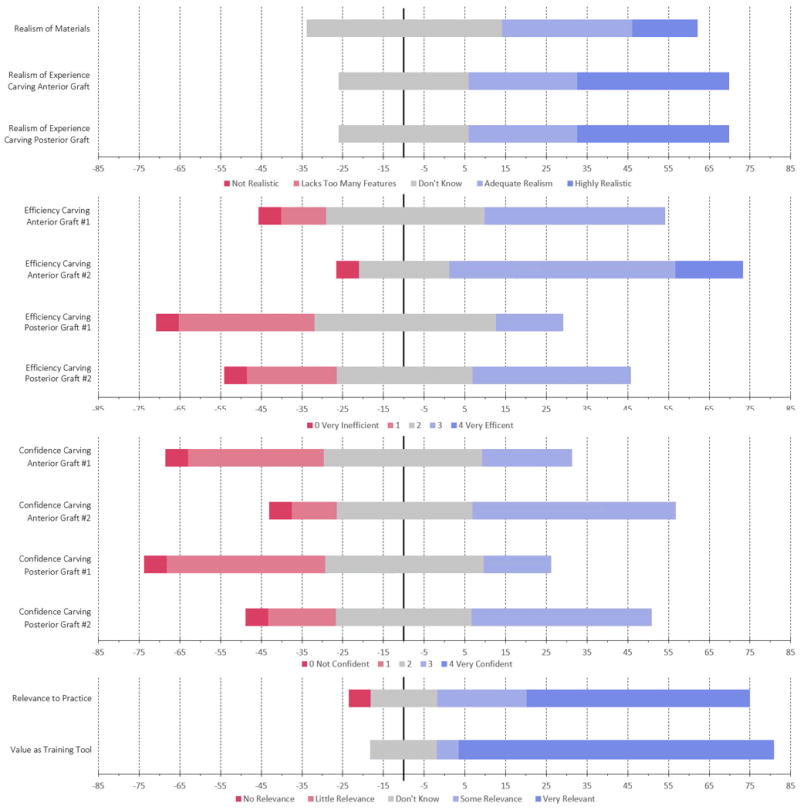
Participant Likert Scale Self-Assessment Results.
Discussion
Surgical simulation has previously been demonstrated to be effective for acquisition of certain surgical skills in trainees8–9. We hypothesized that simulating carving of cartilage grafts for airway reconstruction may assist with skill attainment. Of importance, whereas 11% of residents had prior exposure with carving airway reconstruction grafts before the teaching session, within an hour, all participants received the experience of carving four grafts themselves. It is of interest to consider how that may affect future exposures and engagement in the actual operative setting.
Our results demonstrate the simulation was rated highly by participants who felt it was relevant and of value to their practice as residents. Despite this, several participants commented that the material was inconsistent at times, noting that some constructs were softer and fractured more easily. We are currently refining the formula, though suspect curing time to be essential.
No differentiation could be made between participants of different PGY level or by number of attempts. This may be due to the heterogeneity of the participant groups, difficulty of the simulation task, lack of prior exposure by participants and limited corrective instruction provided during or between attempts. Increased number of attempts in the simulation may be necessary before baseline performance expectations or gains in skill can be quantified2,10. No differentiation could be made between educational modality (video versus live demonstration), which may be attributed to inadequate exposures to the instructional materials and limitations of the educational environment.
The material cost per simulation model was $0.60, and the mold for the model was manufactured using a consumer 3D printer costing approximately $1,000. As such, this simulator is low-cost and rapidly deployable in a variety of situations, including where training resources are limited. The simulator can also be customized based on individual patient imaging, allowing for patient-specific and scenario-specific simulation.
Our pilot study is limited by small sample size, which may restrict the ability to generalize findings across a broader population of Otolaryngology trainees. Additionally, while competency carving grafts is an important skill for airway reconstruction it does not convey competency to perform the entire operation. The use of Likert questionnaires introduces potential for acquiescence bias, which may overrate the favorability of the simulator. Further investigation, including increased repetitions through the simulator, are necessary to assess the true effect of the simulator on surgical skill in carving airway grafts.
This pilot study demonstrates the use of CAD and 3D printing to create a rapidly producible and deployable, low-cost physical simulator for cartilage graft carving in airway reconstruction. The cost and ability for this simulation training to be done in any setting is particularly advantageous. When considering international or remote surgical training, leveraging low-cost, standardized tools such as this simulator may be an effective use of resources to assist in training surgeons worldwide.
Supplementary Material
Figure S1. Likert Scale Simulation Assessments. (A) Simulation participant self-assessment form. (B) Expert airway reconstructive surgeon graft assessment form. (Adapted from Journal of Pediatric Surgery, Volume 48, Issue 6, KA Barsness, DM Rooney, LM Davis, Collaboration in simulation: The development and initial validation of a novel thoracoscopic neonatal simulator, 1232–1238, Copyright (2013), with permission from Elsevier.)
Video S1 Instructional Video for Anterior Cartilage Graft Carving: Video shown to all participants in Group 1 in preparation for the surgical simulation of anterior graft carving.
Video S2 Instructional Video for Posterior Cartilage Graft Carving: Video shown to all participants in Group 1 in preparation for the surgical simulation of posterior graft carving.
Acknowledgments
We would like to thank the Rontal family for their support of resident training and funding of the head & neck dissection course and Dr. Deborah Rooney in the University of Michigan Clinical Simulation Center for providing the initial simulation assessment forms.
Funding: R.J.M. is supported by NIH grant T32 DC005356-12.
Footnotes
Presentation: Abstract has not been previously presented at a national meeting.
Competing interests: Author D.A.Z. has filed a patent application related to the simulation device. The authors declare no other competing financial interests.
References
- 1.Rose AS, Kimbell JS, Webster CE, Harrysson OL, Formeister EJ, Buchman CA. Multi-material 3D Models for Temporal Bone Surgical Simulation. Ann Otol Rinol Laryngol. 2015;124(7):528–536. doi: 10.1177/0003489415570937. [DOI] [PubMed] [Google Scholar]
- 2.Wijewickrema S, Piromchai P, Zhou Y, et al. Developing Effective Automated Feedback for Temporal Bone Surgery Simulation. Otolaryngol Head Neck Surg. 2015;152(6):1082–1088. doi: 10.1177/0194599815570880. [DOI] [PubMed] [Google Scholar]
- 3.Ventola CL. Medical Applications for 3D Printing: Current and Projected Uses. PT. 2014;30(10):704–711. [PMC free article] [PubMed] [Google Scholar]
- 4.Scawn RL, Foster A, Lee BW, Kikkawa DO, Korn BS. Customised 3D Printing: An Innovative Training Tool for the Next Generation of Orbital Surgeons. Orbit. 2015;34(4):216–219. doi: 10.3109/01676830.2015.1049367. [DOI] [PubMed] [Google Scholar]
- 5.AlAli AB, Griffen MF, Butler PE. Three-Dimensional Printing Surgical Applications. Eplasty. 2015;15:e37. [PMC free article] [PubMed] [Google Scholar]
- 6.Berens AM, Newman S, Bhrany AD, Murakami C, Sie KC, Zopf DA. Computer-Aided Design and 3D Printing to Produce a Costal Cartilage Model for Simulation of Auricular Reconstruction. Otolaryngol Head Neck Surg. 2016;155(2):356–9. doi: 10.1177/0194599816639586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barsness KA, Rooney DM, Davis LM. Collaboration in simulation: the development and initial validation of a novel thoracoscopic neonatal simulator. J Pediatr Surg. 2013 Jun;48(6):1232–8. doi: 10.1016/j.jpedsurg.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 8.Costello JP, Olivieri LJ, Su L, et al. Incorporating Three-Dimensional Printing into a Simulation-Based Congenital Heart Disease and Critical Care Training Curriculum for Resident Physicians. Congenit Heart Dis. 2015;10(2):185–90. doi: 10.1111/chd.12238. [DOI] [PubMed] [Google Scholar]
- 9.Cook DA, Hatala R, Brydges R, et al. Technology-Enhnaced Simulation for Health Professions Education: A Systematic Review and Meta-Analysis. JAMA. 2011;306(9):978–88. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 10.Firmin F, Marchac A. A Novel Algorithm for Autologous Ear Reconstruction. Semin Plast Surg. 2011;25(4):257–264. doi: 10.1055/s-0031-1288917. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Likert Scale Simulation Assessments. (A) Simulation participant self-assessment form. (B) Expert airway reconstructive surgeon graft assessment form. (Adapted from Journal of Pediatric Surgery, Volume 48, Issue 6, KA Barsness, DM Rooney, LM Davis, Collaboration in simulation: The development and initial validation of a novel thoracoscopic neonatal simulator, 1232–1238, Copyright (2013), with permission from Elsevier.)
Video S1 Instructional Video for Anterior Cartilage Graft Carving: Video shown to all participants in Group 1 in preparation for the surgical simulation of anterior graft carving.
Video S2 Instructional Video for Posterior Cartilage Graft Carving: Video shown to all participants in Group 1 in preparation for the surgical simulation of posterior graft carving.


