Abstract
Background:
The purpose of the present study was to determine if the duration of symptoms affects outcomes following the treatment of intervertebral lumbar disc herniation.
Methods:
An as-treated analysis was performed on patients enrolled in the Spine Patient Outcomes Research Trial (SPORT) for the treatment of intervertebral lumbar disc herniation. Randomized and observational cohorts were combined. A comparison was made between patients who had had symptoms for six months or less (n = 927) and those who had had symptoms for more than six months (n = 265). Primary and secondary outcomes were measured at baseline and at regular follow-up intervals up to four years. The treatment effect for each outcome measure was determined at each follow-up period for the duration of symptoms for both groups.
Results:
At all follow-up intervals, the primary outcome measures were significantly worse in patients who had had symptoms for more than six months prior to treatment, regardless of whether the treatment was operative or nonoperative. When the values at the time of the four-year follow-up were compared with the baseline values, patients in the operative treatment group who had had symptoms for six months or less had a greater increase in the bodily pain domain of the Short Form-36 (SF-36) (mean change, 48.3 compared with 41.9; p < 0.001), a greater increase in the physical function domain of the SF-36 (mean change, 47.7 compared with 41.2; p < 0.001), and a greater decrease in the Oswestry Disability Index score (mean change, –41.1 compared with –34.6; p < 0.001) as compared with those who had had symptoms for more than six months (with higher scores indicating less severe symptoms on the SF-36 and indicating more severe symptoms on the Oswestry Disability Index). When the values at the time of the four-year follow-up were compared with the baseline values, patients in the nonoperative treatment group who had had symptoms for six months or less had a greater increase in the bodily pain domain of the SF-36 (mean change, 31.8 compared with 21.4; p < 0.001), a greater increase in the physical function domain of the SF-36 (mean change, 29.5 compared with 22.6; p = 0.015), and a greater decrease in the Oswestry Disability Index score (mean change, −24.9 compared with −18.5; p = 0.006) as compared with those who had had symptoms for more than six months. Differences in treatment effect between the two groups related to the duration of symptoms were not significant.
Conclusions:
Increased symptom duration due to lumbar disc herniation is related to worse outcomes following both operative and nonoperative treatment. The relative increased benefit of surgery compared with nonoperative treatment was not dependent on the duration of the symptoms.
Level of Evidence:
Prognostic Level I. See Instructions for Authors for a complete description of levels of evidence.
Symptomatic herniation of the nucleus pulposus in the lumbar spine affects 1% to 2% of the general population at some time during their lives1,2. Symptomatic herniation of the nucleus pulposus is most prevalent in men during the fourth and fifth decades of life3. Although the presentation of symptoms is variable, many patients recall an acute event that precipitated low back pain associated with radicular unilateral or bilateral leg pain. Leg pain resolves in 70% of patients within six weeks after presentation4. Therefore, the treatment of herniation of the nucleus pulposus generally begins nonoperatively and includes education and counseling, nonsteroidal anti-inflammatory and narcotic medication, physical therapy, and epidural injections. According to most guidelines, surgery should be considered for patients with persistent pain beyond a reasonable course of nonoperative therapy5.
Randomized trials from the past thirty years have demonstrated the efficacy of the discectomy procedure for the treatment of herniation of the nucleus pulposus6. More recent studies, such as the Spine Patient Outcomes Research Trial (SPORT), have further demonstrated the benefit of operative over nonoperative treatment for herniation of the nucleus pulposus7-12. It is universally agreed that emergency surgery is rarely required. There is no consensus, however, regarding the timing of elective surgery for the treatment of lumbar disc herniation. Statements in the literature include waiting anywhere from “an appropriate amount of time” to twelve months after the onset of symptoms13-18. The purpose of the present study was to use the SPORT database to assess the effect of the duration of symptoms on outcomes following the treatment of lumbar disc herniation. We hypothesized that patients with a longer duration of pretreatment symptoms have less favorable clinical outcomes than those with a shorter duration of symptoms.
Materials and Methods
Study Design
SPORT was conducted at thirteen multidisciplinary spine practices in eleven states across the United States. The details of methods have been reported previously9,19-21.
Patients
The human subject committees at each center approved the standardized protocol. Patients over the age of eighteen years who had radicular pain for at least six weeks despite some form of nonoperative treatment, a positive nerve root tension sign and/or neurological deficit, and a confirmatory cross-sectional imaging study demonstrating intervertebral disc herniation at or caudad to L2, with the level and side corresponding with the symptoms, were included in the study. Patients with cauda equina syndrome, a progressive neurological deficit, malignant disease, scoliosis measuring >15°, previous back surgery, and/or other established contraindications to elective surgery were excluded.
Study Interventions
Patients were enrolled into either a randomized cohort or an observational cohort. Those in the randomized cohort received computer-generated random treatment assignments. Those in the observational cohort chose their treatment with their physician. Patients in the operative treatment group underwent lumbar discectomy with use of a traditional open posterior approach. Patients in the nonoperative treatment group were managed with “minimum nonsurgical treatment,” defined as active physical therapy, education and/or counseling with home exercise instruction, and a nonsteroidal anti-inflammatory drug if tolerated. Additionally, patients in the nonoperative treatment group could receive any therapies above the minimum required protocol that were deemed appropriate by their physician. Given the extensive crossover in the randomized cohort and the similarity between baseline patient characteristics and outcomes when comparing the randomized and observational cohorts, both of the cohorts were combined for this study and an as-treated analysis was performed on the combined cohorts.
Study Measures
The data for the present study were obtained from patient questionnaires that were completed at baseline and at six weeks, three months, six months, one year, two years, and four years after enrollment or surgery. The primary outcome measures included the bodily pain and physical function domains of the Short Form-36 (SF-36)22 and the American Academy of Orthopaedic Surgeons MODEMS (Musculoskeletal Outcomes Data Evaluation and Management System) version of the Oswestry Disability Index (ODI)23. Secondary measures included patient self-reported improvement, work status, and satisfaction with current symptoms1. Symptom severity was measured with the Low Back Pain Bothersomeness Index, the Sciatica Bothersomeness Scale, and the Leg Pain Bothersomeness Scale10,24. The SF-36 scales and the ODI range from 0 to 100, the Sciatica Bothersomeness Scale ranges from 0 to 24, and the Low Back Pain Bothersomeness Index and the Leg Pain Bothersomeness Scale range from 0 to 6. Higher scores indicate more severe symptoms on the ODI, the Sciatica Bothersomeness Scale, and the Leg Pain Bothersomeness Scale, whereas higher scores indicate less severe symptoms on the SF-36.
Statistical Analysis
Differences in baseline characteristics were compared between patients who had had symptoms for six months or less and those who had had symptoms for more than six months. The primary analyses compared changes in the clinical outcome measures from baseline as a function of the duration of symptoms within each nonoperative or operative treatment arm. The duration of symptoms was based on the date of the onset of symptoms to the date of surgery for patients in the operative treatment arm and was based on the date of onset of symptoms to the date of enrollment in the study for those in the nonoperative treatment arm. The treatment effect of surgery was calculated as the change in outcome measure after operative treatment minus the change in outcome measure after nonoperative treatment25.
Significance was defined as a p value of <0.05 on the basis of a two-sided hypothesis test with no adjustment made for multiple comparisons. No adjustments were made because the analyses in the current study consisted of the longitudinal assessment of different dimensions of outcomes (that is, symptoms, function, and disability) over time. The analyses were not multiple independent comparisons from which we were looking for a single significant result, as would be implied by a Bonferroni or similar correction for multiple comparisons. The various time points were not independently assessed but were compared within the overall context of a longitudinal regression model across three complementary domains of outcome.
Source of Funding
Funds were received from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women's Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention. The Multidisciplinary Clinical Research Center in Musculoskeletal Diseases is funded by NIAMS (P60-AR048094). Funds were used for statistical analysis and manuscript publication.
Results
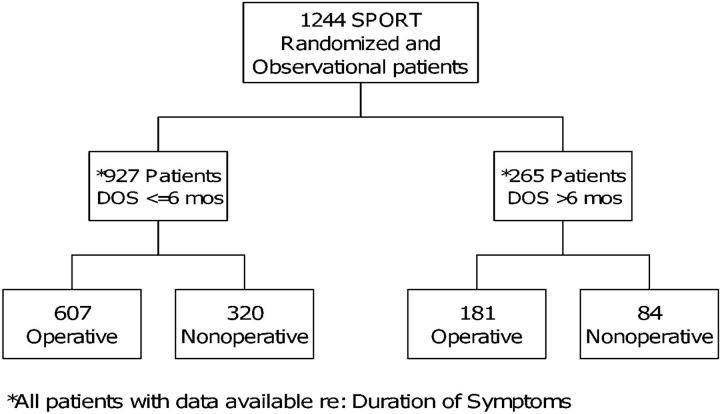
Of the 1244 patients who were enrolled in the SPORT study, 1192 patients had had data on the duration of symptoms; of these, 927 patients had had symptoms for six months or less, and 265 had had symptoms for more than six months (Fig. 1). The demographic and baseline characteristics are illustrated in a table in the Appendix. Significant baseline differences between the patients who had had symptoms for more than six months and those who had had symptoms for six months or less included a higher rate of depression (p = 0.005), a higher proportion of patients who perceived that the problem was getting worse (p = 0.002), and a greater proportion of patients who had a preference for surgical treatment (p = 0.04) among those who had had symptoms for more than six months. Otherwise, the demographic and baseline characteristics were similar. There was no difference between the two groups in terms of work status at baseline. In the operative treatment group, 57% of patients who had had symptoms for six months or less and 60% of those who had had symptoms for more than six months had worked at either a full or part-time job prior to surgery (p = 0.42). In the nonoperative treatment group, 66% of patients who had had symptoms for six months or less and 67% of those who had had symptoms for more than six months had worked either a full or part-time job prior to treatment (p = 0.11). There were no differences between the patients who had had symptoms for six months or less and those who had had symptoms for more than six months in terms of baseline primary outcome measures (that is, SF-36 bodily pain and physical function and Oswestry Disability Index).
Fig. 1.
Flowchart demonstrating the different study groups. SPORT = Spine Patient Outcomes Research Trial.
Clinical baseline characteristics are reported in Table I. Compared with patients who had had symptoms for more than six months, a higher percentage of patients who had had symptoms for six months or less had a positive straight leg raise test (8% difference; p = 0.028), neurological deficit (6% difference; p = 0.034), asymmetric depressed lower extremity deep tendon reflexes (8% difference; p = 0.013), and fewer protruding and greater extruded or sequestered types of herniation on magnetic resonance imaging (MRI) (p < 0.001). The details of operative treatment are indicated in Table II. The operative time was eight minutes greater for the patients who had had symptoms for more than six months (p = 0.008). There were other slight differences between the groups that did not reach significance.
TABLE I.
Clinical Baseline Characteristics of “As Treated” Randomized Controlled Trial and Observational Cohorts Combined
| Clinical Characteristic | Patients with Symptoms for ≤6 Months* (N = 927) | Patients with Symptoms for >6 Months* (N = 265) | P Value |
| Pain radiation | 903 (97%) | 259 (98%) | 0.94 |
| Positive straight leg raise test | |||
| Ipsilateral | 599 (65%) | 151 (57%) | 0.028† |
| Contralateral/bilateral | 139 (15%) | 49 (18%) | 0.2 |
| Neurological deficit | |||
| Any | 715 (77%) | 187 (71%) | 0.034† |
| Reflexes (asymmetrical depression) | 392 (42%) | 89 (34%) | 0.013† |
| Sensory (asymmetrical decrease) | 480 (52%) | 123 (46%) | 0.14 |
| Motor (asymmetrical weakness) | 398 (43%) | 103 (39%) | 0.27 |
| Herniation level | 0.13 | ||
| L2-L3/L3-L4 | 69 (7%) | 19 (7%) | |
| L4-L5 | 341 (37%) | 115 (43%) | |
| L5-S1 | 517 (56%) | 130 (49%) | |
| Herniation type | <0.001† | ||
| Protruding | 229 (25%) | 93 (35%) | |
| Extruded | 621 (67%) | 162 (61%) | |
| Sequestered | 77 (8%) | 9 (3%) | |
| Posterolateral herniation | 722 (78%) | 197 (74%) | 0.26 |
The values are given as the number of patients, with the percentage in parentheses.
Significant (p < 0.05).
TABLE II.
Operative Treatments, Complications, and Events of “As Treated” Randomized Controlled Trial and Observational Cohorts Combined*
| Patients with Symptoms for ≤6 Months (N = 616) | Patients with Symptoms for >6 Months (N = 182) | P Value | |
| Discectomy level (no. of patients) | |||
| L2-L3 | 12 (2%) | 2 (1%) | 0.68 |
| L3-L4 | 21 (3%) | 6 (3%) | 0.84 |
| L4-L5 | 238 (39%) | 74 (41%) | 0.54 |
| L5-S1 | 357 (58%) | 97 (53%) | 0.45 |
| Operative time† (min) | 74.8 ± 35.2 | 83.2 ± 43.4 | 0.008‡ |
| Blood loss† (mL) | 60.8 ± 85 | 76.9 ± 144.9 | 0.061 |
| Blood replacement (no. of patients) | |||
| Intraoperative replacement | 4 (1%) | 2 (1%) | 0.9 |
| Postoperative transfusion | 0 (0%) | 0 (0%) | — |
| Length of stay† (d) | 0.93 ± 0.9 | 1.1 ± 1 | 0.052 |
| Intraoperative complications (no. of patients) | |||
| Dural tear/spinal fluid leak | 18 (3%) | 6 (3%) | 0.99 |
| Nerve root injury | 1 (0%) | 1 (1%) | 0.94 |
| Other | 3 (0%) | 0 (0%) | 0.8 |
| None | 595 (97%) | 175 (96%) | 0.96 |
| Postoperative complications/events (no. of patients) | |||
| Wound hematoma | 4 (1%) | 0 (0%) | 0.62 |
| Wound infection | 15 (2%) | 3 (2%) | 0.73 |
| Other | 22 (4%) | 5 (3%) | 0.76 |
| None | 575 (94%) | 172 (95%) | 0.66 |
| Additional operations | |||
| 1-year rate | 37 (6%) | 9 (5%) | 0.58 |
| 2-year rate | 51 (8%) | 12 (7%) | 0.45 |
| 3-year rate | 55 (9%) | 15 (8%) | 0.75 |
| 4-year rate | 64 (10%) | 17 (9%) | 0.67 |
| Recurrent disc herniation | 37 (6%) | 12 (7%) | |
| Complication or other | 17 (3%) | 4 (2%) | |
| New condition | 8 (1%) | 1 (<1%) | |
The table includes complications for all patients in the study who had surgery, including ten patients who did not have enough follow-up data to be included in the project's data analysis set (represented by Figure 1).
The values are given as the mean and the standard deviation.
Significant (p < 0.05).
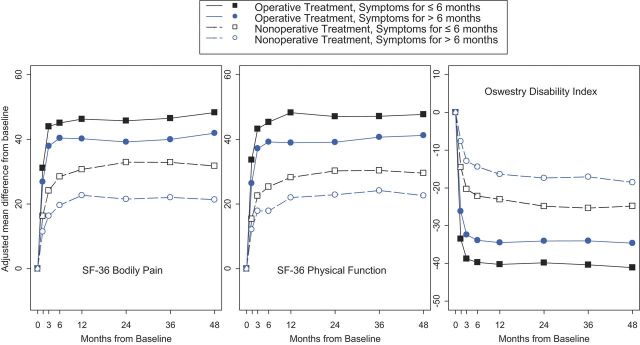
In the operative treatment group, patients who had had symptoms for six months or less had significantly improved primary outcome measures compared with those who had had symptoms for more than six months. When the measurements at each follow-up interval from one to four years were compared with the baseline values, patients who had had symptoms for six months or less had a greater increase in the bodily pain domain of the SF-36 (mean change at four years, 48.3 compared with 41.9; p < 0.001), a greater increase in the physical function domain of the SF-36 (mean change at four years, 47.7 compared with 41.2; p < 0.001), and a greater decrease in the ODI score (mean change at four years, −41.1 compared with −34.6; p < 0.001) in comparison with those who had had symptoms for more than six months (with higher scores indicating less severe symptoms on the SF-36 and indicating more severe symptoms on the Oswestry Disability Index) (Table III). In the operative treatment group, the majority of secondary outcome measures, including the Sciatica Bothersomeness Scale, satisfaction with symptoms, self-rated health status, and working status, demonstrated a significant benefit for patients who had had symptoms for six months or less (see Appendix). The Leg Pain Bothersomeness Scale and the Low Back Pain Bothersomeness Index showed a definite trend toward greater improvement in patients who had had symptoms for six months or less, but the difference did not reach significance at the time of the four-year follow-up (p = 0.051 and p = 0.084, respectively) (see Appendix).
TABLE III.
Change from Baseline in Primary Outcome Measures for Operatively and Nonoperatively Managed Patients, According to Duration of Symptoms, at One, Two, Three, and Four Years of Follow-up*
| Change from Baseline |
||||
| 1 Year | 2 Years | 3 Years | 4 Years | |
| Operative treatment group | ||||
| SF-36 bodily pain | ||||
| Patients with symptoms for ≤6 months | 46.3 ± 1.1 | 45.7 ± 1.1 | 46.5 ± 1.2 | 48.3 ± 1.2 |
| Patients with symptoms for >6 months | 40.2 ± 1.4 | 39.2 ± 1.4 | 40 ± 1.5 | 41.9 ± 1.5 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
| SF-36 physical function | ||||
| Patients with symptoms for ≤6 months | 48.3 ± 1.1 | 47.1 ± 1.1 | 47.1 ± 1.1 | 47.7 ± 1.1 |
| Patients with symptoms for >6 months | 39 ± 1.4 | 39.1 ± 1.3 | 40.7 ± 1.4 | 41.2 ± 1.4 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
| Oswestry Disability Index | ||||
| Patients with symptoms for ≤6 months | –40.3 ± 0.9 | –39.9 ± 0.9 | –40.4 ± 0.9 | –41.1 ± 0.9 |
| Patients with symptoms for >6 months | –34.5 ± 1.1 | –34.1 ± 1.1 | –34 ± 1.1 | –34.6 ± 1.2 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
| Nonoperative treatment group | ||||
| SF-36 bodily pain | ||||
| Patients with symptoms for ≤6 months | 30.7 ± 1.3 | 32.9 ± 1.3 | 32.9 ± 1.4 | 31.8 ± 1.4 |
| Patients with symptoms for >6 months | 22.7 ± 2.4 | 21.5 ± 2.5 | 22 ± 2.7 | 21.4 ± 2.8 |
| P value | 0.003 | <0.001 | <0.001 | <0.001 |
| SF-36 physical function | ||||
| Patients with symptoms for ≤6 months | 28.2 ± 1.2 | 30.3 ± 1.3 | 30.4 ± 1.3 | 29.5 ± 1.3 |
| Patients with symptoms for >6 months | 22 ± 2.3 | 22.8 ± 2.4 | 24.1 ± 2.6 | 22.6 ± 2.6 |
| P value | 0.013 | 0.005 | 0.025 | 0.015 |
| Oswestry Disability Index | ||||
| Patients with symptoms for ≤6 months | –23.1 ± 1 | –24.9 ± 1 | –25.4 ± 1.1 | –24.9 ± 1.1 |
| Patients with symptoms for >6 months | –16.4 ± 1.9 | –17.4 ± 2 | –17.1 ± 2.1 | –18.5 ± 2.1 |
| P value | 0.001 | <0.001 | <0.001 | 0.006 |
The values are given as the mean and the standard deviation.
In the nonoperative treatment group, patients who had had symptoms for six months or less also demonstrated improved primary outcome measures compared with those who had had symptoms for more than six months (Table III). When the measurements at each follow-up interval from one to four years were compared with the baseline values, patients who had had symptoms for six months or less had a greater increase in the bodily pain domain of the SF-36 (mean change at four years, 31.8 compared with 21.4; p < 0.001), a greater increase in the physical function domain of the SF-36 (mean change at four years, 29.5 compared with 22.6; p = 0.015), and a greater decrease in the ODI score (mean change at four years, –24.9 compared with –18.5; p = 0.006) in comparison with those who had had symptoms for more than six months (with higher scores indicating less severe symptoms on the SF-36 and indicating more severe symptoms on the Oswestry Disability Index) (Table III). The Sciatica Bothersomeness Scale, Leg Pain Bothersomeness Scale, Low Back Pain Bothersomeness Index, and working status demonstrated a consistent benefit for the patients who had had symptoms for six months or less (see Appendix).
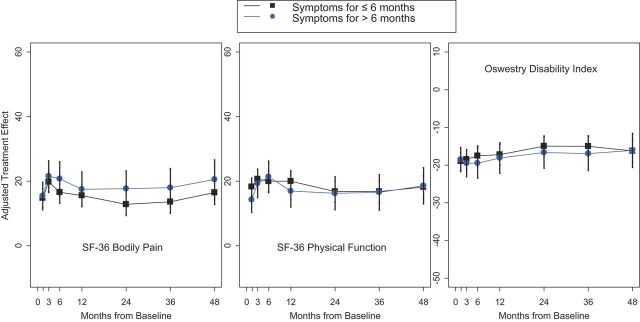
The patients in the operative treatment group had better outcomes than those in the nonoperative treatment group at every follow-up time point for all primary outcome measures (Fig. 2). The treatment effect, or the change from baseline following operative treatment minus the change from baseline following nonoperative treatment, was calculated separately at each time point for the patients who had had symptoms for six months or less and those who had had symptoms for more than six months to determine if the duration of symptoms influenced the relative effectiveness of operative intervention as compared with nonoperative intervention (Table IV) (see Appendix). The treatment effect for all primary and secondary outcome measures was similar in patients who had had symptoms for six months or less and those who had had symptoms for more than six months, indicating that operative treatment offers similar advantages over nonoperative treatment, regardless of the duration of symptoms (Fig. 3).
Fig. 2.
Line graph illustrating the change in primary outcome measures versus time for patients in the operative and nonoperative treatment groups who had had symptoms for six months or less or for more than six months.
TABLE IV.
Treatment Effect After Surgery for Primary Outcome Measures According to Duration of Symptoms
| Mean Treatment Effect (95% CI*) | ||||
| Outcome Scale | 1 Year | 2 Years | 3 Years | 4 Years |
| SF-36 bodily pain | ||||
| Patients with symptoms for ≤6 months | 15.6 (12.1 to 19) | 12.8 (9.3 to 16.3) | 13.6 (10 to 17.3) | 16.5 (12.8 to 20.3) |
| Patients with symptoms for >6 months | 17.5 (12.1 to 22.9) | 17.7 (12.2 to 23.2) | 18 (12.1 to 23.9) | 20.6 (14.5 to 26.6) |
| P value | 0.55 | 0.14 | 0.21 | 0.26 |
| SF-36 physical function | ||||
| Patients with symptoms for ≤6 months | 20 (16.8 to 23.3) | 16.8 (13.5 to 20.1) | 16.8 (13.4 to 20.2) | 18.2 (14.7 to 21.7) |
| Patients with symptoms for >6 months | 17 (12 to 22) | 16.3 (11.2 to 21.4) | 16.5 (11 to 22.1) | 18.6 (13 to 24.2) |
| P value | 0.31 | 0.86 | 0.94 | 0.91 |
| Oswestry Disability Index | ||||
| Patients with symptomsfor ≤6 months | −17.2 (−19.9 to −14.6) | −15 (−17.7 to −12.3) | −5 (−17.8 to −12.2) | −16.3 (−19.2 to −13.4) |
| Patients with symptoms for >6 months | −18.1 (−22.2 to −14) | −16.7 (−20.8 to −12.5) | −16.9 (−21.4 to −12.4) | −16.1 (−20.6 to −11.6) |
| P value | 0.72 | 0.5 | 0.46 | 0.96 |
CI = confidence interval.
Fig. 3.
A comparison of the treatment effects for each of the three primary outcome measures between patients who had had symptoms for six months or less and those who had had symptoms for more than six months. The p values comparing treatment effects between the groups were not significant.
A post hoc power analysis was performed to ensure that our study was sufficiently powered. We based the power analysis around one of the primary outcome variables in the operative treatment population, the SF-36 bodily pain subscale. In order to show a difference between patients who had had symptoms for six months or less and those who had had symptoms for more than six months prior to operative treatment, SF-36 bodily pain subscales in one group would have to exceed those in the other by at least the minimum clinically important difference. To maintain a conservative estimate of the power of the study, the minimum clinically important difference was selected on the basis of the study by Lauridsen et al.26, which demonstrated an increasing minimum clinically important difference with improved baseline scores up to a maximum value for the minimum clinically important difference of 5 on the SF-36 bodily pain subscale. On the basis of this minimum clinically important difference, the observed difference of 6.4 points between patients with symptoms for six months or less and those with symptoms for more than six months before operative treatment, and the observed standard deviation of approximately 1.5 points, the power of the study approaches 1. This is an expected result, both because of the large study size and because the difference between these groups in terms of the SF-36 bodily pain subscale exceeded the minimum clinically important difference.
Discussion
The authors of previous observational studies have identified worse outcomes in patients with a longer duration of pretreatment symptoms and have recommend earlier surgical intervention27-31. Nygaard et al. found worse self-reported outcomes in patients who had had leg pain for more than eight months in a prospective study of 132 consecutive patients27. Jansson et al., in a prospective follow-up study of 283 patients who underwent surgery for the treatment of lumbar disc herniation, showed that a duration of pain of more than six months was a risk factor for a worse health-related quality of life as determined with the EuroQol-5D measurement tool28. Ng and Sell, in a prospective cohort study of 113 consecutive patients with lumbar disc herniation, determined that patients who had had symptoms for more than twelve months had significantly worse outcomes in comparison with patients who had had symptoms for less than twelve months before operative treatment29. Jönsson investigated patient-related factors predicting the outcome after decompressive surgery in a study of 120 patients with lumbar disc herniation30. A duration of sciatica of more than six months and a long absence from work had significant negative influence on the two-year surgical outcome.
Recently, Peul et al.32 performed a large, multicenter randomized trial involving 283 patients with sciatica and lumbar disc herniation in which early surgery (that is, within two weeks) was compared with a six-month period of nonoperative treatment followed by surgery if needed after this period of nonoperative treatment. All patients had symptoms for six to twelve weeks prior to enrollment. Early surgery offered significant benefits over nonoperative treatment in the early follow-up period, with the maximum benefit achieved between eight to twelve weeks after enrollment. At one year and two years33,34 after randomization, however, there were no significant differences between the two groups in terms of the primary outcome measures. It should be noted that, during the first year of the study, 39% of the patients who had been randomized to six months of nonoperative treatment crossed over and underwent surgery at an average of 14.6 weeks after enrollment. It should also be noted that the authors chose to perform an intent-to-treat analysis of their data. In an intent-to-treat analysis, this substantial crossover may lead to an underestimation of the benefits of surgical treatment. According to the authors, patients who had unsuccessful nonoperative treatment and underwent late surgery had similar improvement at one and two years as compared with patients who were allocated to early surgery35. These findings suggest that there is no downside to attempting nonoperative treatment prior to performing surgery.
Similar to many of the previously published studies, the current study suggests that patients who have symptoms of a herniated lumbar disc for more than six months do not have clinical results that are as good as those for patients who have symptoms for six months or less prior to the initiation of any formal treatment program. In the operative treatment group, patients who had had symptoms for more than six months had significant improvements over baseline. However, the improvements were not as great as those achieved in the operatively managed patients who had had symptoms for six months or less. Similarly, in the nonoperative treatment group, patients who had had symptoms for more than six months had significant improvements over baseline, but the improvements were not as great as those seen in those who had had symptoms for six months or less. As indicated by the reported treatment effects, operative treatment provided a benefit over nonoperative treatment at all follow-up time intervals for all primary outcome measures. There was no significant difference in the calculated treatment effects between the two groups, suggesting that surgical treatment offers similar advantages over nonoperative treatment, regardless of the duration of symptoms. Although they may not have done as well as patients with a shorter duration of symptoms, those who had had symptoms for more than six months had a better outcome following surgery as compared with following nonoperative treatment. Similarly, consistent with the findings of Peul et al.32-34, no greater advantage is gained with operative over nonoperative treatment when performed for patients with shorter duration of symptoms. This information can be helpful when counseling patients on the options for the treatment of symptomatic lumbar disc herniation.
The present study had limitations. Differences in baseline data between the group of patients who had had symptoms for six months or less and the group of patients who had had symptoms for more than six months may have affected the results. These differences included the type of disc herniation, the presence of neurological deficit, the operative time, the percentage of patients who reported depression, the percentage of patients who perceived that the problem was getting worse, and the percentage of patients who had a preference for surgical treatment. Several of these variables have been shown in previous studies to have an effect on the outcome of lumbar discectomy36-44. Although the SPORT investigation was not powered specifically to detect differences between subgroups on the basis of the duration of symptoms, we did detect significant differences between the patients who had symptoms for six months or less and those who had had symptoms for more than six months. However, it is possible that there may be additional clinically relevant differences between the subgroups in terms of baseline characteristics or outcomes that we were not able to detect. Future investigations might address the role of potential confounding variables, such as patient expectations, the perception of symptomatic improvement, and depression/mental status, in determining patient outcomes.
Appendix
Tables showing the baseline characteristics of the cohorts, the change from baseline in terms of secondary outcome measures for the operatively and nonoperatively managed patients, and the treatment effect of surgery in terms of secondary outcome measures are available with the online version of this article as a data supplement at jbjs.org
Investigation performed at the Rothman Institute, Thomas Jefferson University Hospital, Philadelphia, Pennsylvania, and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, one or more of the authors has had another relationship, or has engaged in another activity, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Deyo RATsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987;12:264-8. [DOI] [PubMed] [Google Scholar]
- 2.Rhee JMSchaufele MAbdu WA. Radiculopathy and the herniated lumbar disc. Controversies regarding pathophysiology and management. J Bone Joint Surg Am. 2006;88:2070-80. [DOI] [PubMed] [Google Scholar]
- 3.Boden SDDavis DODina TSPatronas NJWiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403-8. [PubMed] [Google Scholar]
- 4.Vroomen PCde Krom MCKnottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002;52:119-23. [PMC free article] [PubMed] [Google Scholar]
- 5.Koes BWvan Tulder MWPeul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334:1313-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber H. The natural history of disc herniation and the influence of intervention. Spine (Phila Pa 1976). 1994;19:2233-8. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein JNTosteson TDLurie JDTosteson ANHanscom BSkinner JSAbdu WAHilibrand ASBoden SDDeyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinstein JNLurie JDTosteson TDSkinner JSHanscom BTosteson ANHerkowitz HFischgrund JCammisa FPAlbert TDeyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinstein JNLurie JDTosteson TDTosteson ANBlood EAAbdu WAHerkowitz HHilibrand AAlbert TFischgrund J. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2008;33:2789-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atlas SJDeyo RAKeller RBChapin AMPatrick DLLong JMSinger DE. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976). 1996;21:1777-86. [DOI] [PubMed] [Google Scholar]
- 11.Tosteson ANLurie JDTosteson TDSkinner JSHerkowitz HAlbert TBoden SDBridwell KLongley MAndersson GBBlood EAGrove MRWeinstein JN; SPORT Investigators. Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med. 2008;149:845-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tosteson ANSkinner JSTosteson TDLurie JDAndersson GBBerven SGrove MRHanscom BBlood EAWeinstein JN. The cost effectiveness of surgical versus nonoperative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2008;33:2108-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rothoerl RDWoertgen CBrawanski A. When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev. 2002;25:162-5. [DOI] [PubMed] [Google Scholar]
- 14.Hurme MAlaranta H. Factors predicting the result of surgery for lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 1987;12:933-8. [DOI] [PubMed] [Google Scholar]
- 15.Jönsson BStrömqvist B. Neurologic signs in lumbar disc herniation. Preoperative affliction and postoperative recovery in 150 cases. Acta Orthop Scand. 1996;67:466-9. [DOI] [PubMed] [Google Scholar]
- 16.Postacchini F. Results of surgery compared with conservative management for lumbar disc herniations. Spine (Phila Pa 1976). 1996;21:1383-7. [DOI] [PubMed] [Google Scholar]
- 17.Fisher CNoonan VBishop PBoyd MFairholm DWing PDvorak M. Outcome evaluation of the operative management of lumbar disc herniation causing sciatica. J Neurosurg. 2004;100(4 Suppl Spine):317-24. [DOI] [PubMed] [Google Scholar]
- 18.Vucetic NAstrand PGüntner PSvensson O. Diagnosis and prognosis in lumbar disc herniation. Clin Orthop Relat Res. 1999;361:116-22. [DOI] [PubMed] [Google Scholar]
- 19.Weinstein JNLurie JDTosteson TDZhao WBlood EATosteson ANBirkmeyer NHerkowitz HLongley MLenke LEmery SHu SS. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lurie JDFaucett SCHanscom BTosteson TDBall PAAbdu WAFrymoyer JWWeinstein JN. Lumbar discectomy outcomes vary by herniation level in the Spine Patient Outcomes Research Trial. J Bone Joint Surg Am. 2008;90:1811-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Birkmeyer NJWeinstein JNTosteson ANTosteson TDSkinner JSLurie JDDeyo RWennberg JE. Design of the Spine Patient outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2002;27:1361-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ware JE JrSherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83. [PubMed] [Google Scholar]
- 23.Daltroy LHCats-Baril WLKatz JNFossel AHLiang MH. The North American spine society lumbar spine outcome assessment instrument: reliability and validity tests. Spine (Phila Pa 1976). 1996;21:741-9. [DOI] [PubMed] [Google Scholar]
- 24.Patrick DLDeyo RAAtlas SJSinger DEChapin AKeller RB. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976). 1995;20:1899-909. [DOI] [PubMed] [Google Scholar]
- 25.Pearson AMBlood EAFrymoyer JWHerkowitz HAbdu WAWoodward RLongley MEmery SELurie JDTosteson TDWeinstein JN. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine (Phila Pa 1976). 2008;33:428-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lauridsen HHHartvigsen JManniche CKorsholm LGrunnet-Nilsson N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord. 2006;7:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nygaard OPKloster RSolberg T. Duration of leg pain as a predictor of outcome after surgery for lumbar disc herniation: a prospective cohort study with 1-year follow up. J Neurosurg. 2000;92(2 Suppl):131-4. [DOI] [PubMed] [Google Scholar]
- 28.Jansson KANémeth GGranath FJönsson BBlomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg Br. 2005;87:959-64. [DOI] [PubMed] [Google Scholar]
- 29.Ng LCSell P. Predictive value of the duration of sciatica for lumbar discectomy. A prospective cohort study. J Bone Joint Surg Br. 2004;86:546-9. [PubMed] [Google Scholar]
- 30.Jönsson B. Patient-related factors predicting the outcome of decompressive surgery. Acta Orthop Scand Suppl. 1993;251:69-70. [DOI] [PubMed] [Google Scholar]
- 31.Folman YShabat SCatz AGepstein R. Late results of surgery for herniated lumbar disk as related to duration of preoperative symptoms and type of herniation. Surg Neurol. 2008;70:398-402. [DOI] [PubMed] [Google Scholar]
- 32.Peul WCvan Houwelingen HCvan den Hout WBBrand REekhof JATans JTThomeer RTKoes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245-56. [DOI] [PubMed] [Google Scholar]
- 33.Peul WCvan den Hout WBBrand RThomeer RTKoes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008;336:1355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peul WCArts MPBrand RKoes BW. Timing of surgery for sciatica: subgroup analysis alongside a randomized trial. Eur Spine J. 2009;18:538-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peul WCBrand RThomeer RTKoes BW. Improving prediction of “inevitable” surgery during non-surgical treatment of sciatica. Pain. 2008;138:571-6. [DOI] [PubMed] [Google Scholar]
- 36.Carragee EJKim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976). 1997;22:1650-60. [DOI] [PubMed] [Google Scholar]
- 37.Carragee EJHan MYSuen PWKim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85:102-8. [PubMed] [Google Scholar]
- 38.Dewing CBProvencher MTRiffenburgh RHKerr SManos RE. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine (Phila Pa 1976). 2008;33:33-8. [DOI] [PubMed] [Google Scholar]
- 39.Hurme MAlaranta H. Factors predicting the result of surgery for lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 1987;12:933-8. [DOI] [PubMed] [Google Scholar]
- 40.Herron LDTurner J. Patient selection for lumbar laminectomy and discectomy with a revised objective rating system. Clin Orthop Relat Res. 1985;199:145-52. [PubMed] [Google Scholar]
- 41.Dvorak JGauchat MHValach L. The outcome of surgery for lumbar disc herniation. I. A 4-17 years’ follow-up with emphasis on somatic aspects. Spine (Phila Pa 1976). 1988;13:1418-22. [DOI] [PubMed] [Google Scholar]
- 42.Spengler DMOuellette EABattié MZeh J. Elective discectomy for herniation of a lumbar disc. Additional experience with an objective method. J Bone Joint Surg Am. 1990;72:230-7. [PubMed] [Google Scholar]
- 43.Junge ADvorak JAhrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine (Phila Pa 1976). 1995;20:460-8. [DOI] [PubMed] [Google Scholar]
- 44.Kjellby-Wendt GStyf JRCarlsson SG. The predictive value of psychometric analysis in patients treated by extirpation of lumbar intervertebral disc herniation. J Spinal Disord. 1999;12:375-9. [PubMed] [Google Scholar]