Abstract
Setting: All health facilities providing routine immunisation services in Liberia.
Objective: To compare the number of routine facility-based and outreach immunisations and measles cases before, during and after the Ebola outbreak.
Design: A descriptive cross-sectional study.
Results: Immunisation coverage for fully immunised children before the Ebola outbreak was 73%. Immunisation coverage for all antigens declined by half compared to baseline during the outbreak. These findings were similar in facility-based and outreach immunisations. During the outbreak, the proportion of fully immunised children dropped by respectively 58%, 33% and 39% in the most, moderately and least Ebola-affected counties. Immunisation rate of recovery in the post-Ebola period was respectively 82%, 21% and 9% in the most, moderately and least affected counties compared to the Ebola-outbreak period. Outreach immunisation recovered slowly compared to facility-based immunisation. The mean number of measles cases reported per month was 12 pre-Ebola, 16 Ebola and 60 post-Ebola.
Conclusion: This study provides insights into the possible impact of an Ebola outbreak on countrywide immunisation. The outbreak weakened a struggling national immunisation programme, and post-outbreak recovery took significant time, which likely contributed to the measles epidemic. Recommendations for the improvement of immunisation services that could limit further preventable epidemics in Liberia and similar contexts at risk for Ebola are provided.
Keywords: vaccination, operational research, Africa, SORT IT, measles
Abstract
Contexte : Toutes les structures de santé offrant des services de vaccination de routine au Liberia.
Objectif : Comparer le nombre de vaccinations de routine dans des structures de santé et en stratégies avancées et le nombre de cas de rougeole avant, pendant et après l'épidémie d'Ebola.
Schéma : Étude descriptive transversale.
Résultats : La couverture vaccinale des enfants complètement immunisés avant l'épidémie d'Ebola était de 73%. La couverture vaccinale pour tous les antigènes a décliné de moitié pendant la flambée comparée à la période précédente. Ces résultats ont été similaires pour les vaccinations dans les structures de santé et les vaccinations périphériques. Pendant la flambée, la proportion d'enfants complètement immunisés a chuté de 58%, 33% et 39%, respectivement, dans les contés gravement, moyennement et faiblement affectés par Ebola. Le taux de vaccination de récupération dans la période post Ebola a été de 82%, 21% et 9%, respectivement, dans les comtés gravement, moyennement et faiblement affectés par Ebola comparés à la période de la flambée d'Ebola. Les vaccinations dans la communauté ont récupéré plus lentement que les vaccinations en structures de santé. Le nombre moyen mensuel de cas de rougeole rapporté a été de 12 avant Ebola, 16 Ebola et 60 après Ebola.
Conclusion : Cette étude permet de mieux comprendre l'impact possible d'une épidémie d'Ebola sur le programme de vaccination dans le pays. La flambée a affaibli un programme national de vaccination déjà en difficulté et après la flambée la récupération a pris du temps, ce qui a sans doute contribué à l'épidémie de rougeole. Des recommandations pour une amélioration des services de vaccination qui pourraient limiter les épidémies évitables à l'avenir au Liberia et dans des contextes similaires à risque d'Ebola sont proposées.
Abstract
Marco de referencia: Todos los establecimientos de salud que prestan servicios corrientes de vacunación en Liberia.
Objetivo: Comparar el número de vacunaciones corrientes institucionales y extrainstitucionales practicadas y de casos de sarampión antes de la epidemia de fiebre hemorrágica del Ébola, durante el brote y después del mismo.
Método: Fue este un estudio transversal descriptivo.
Resultados: La cobertura de los niños con un esquema completo de vacunación antes de la epidemia del Ébola era 73%. La cobertura con todos los antígenos disminuyó un 50% durante el brote epidémico en comparación con los datos preepidémicos. Esta proporción fue equivalente en la vacunación institucional y periférica. Durante el brote, la proporción de niños con un esquema completo de vacunación disminuyó según la intensidad alta, moderada o baja de la epidemia en un 58%, un 33% y un 39%, respectivamente. La tasa correspondiente de recuperación de la vacunación después del período epidémico fue de 82%, 21% y 9% con respecto al período epidémico. La vacunación periférica se recuperó más lentamente que la vacunación practicada en los establecimientos de salud. El promedio mensual de casos de sarampión notificados fue 12 antes del brote del Ébola, 16 durante la epidemia y 60 después de la misma.
Conclusión: Los resultados del presente estudio enriquecen la percepción de las repercusiones que puede provocar una epidemia de fiebre hemorrágica del Ébola en el sistema de vacunación a escala del país. El brote epidémico debilitó aun más el programa nacional de vacunación y su recuperación precisó un tiempo considerable; es probable que este factor haya contribuido al surgimiento de la epidemia de sarampión. Se aportan recomendaciones encaminadas a mejorar los servicios de vacunación, que pueden limitar mejor las epidemias prevenibles en Liberia y en otros entornos comparables donde existe un riesgo de aparición de la fiebre del Ébola.
During 2013–2014, West Africa experienced the largest Ebola virus disease (EVD) outbreak in history. The first cases of EVD in Liberia were reported in March 2014.1,2 The impact of the outbreak overwhelmed an already weak health care system;3 lapses in infection control at health care facilities led to the deaths of almost half (184/372) of the health care workers (HCWs) who were infected. This caused alarm among HCWs in facilities due to the risk of EVD, estimated at 30 times higher than in the general population,4 and many public and private health facilities were temporarily closed. A sense of apprehension was created among those who used health facilities, with significant concerns that they or their family members might contract EVD if they visited these facilities.5
Although improvements have been reported in the immunisation coverage for most antigens in Liberia, the performance of the national immunisation programme was suboptimal before the outbreak. The 2013 Demographic and Health Survey indicated 55% immunisation coverage for children aged 12–23 months,6 and there were repeated measles outbreaks in previous years. This dismal performance may have resulted from the country's intermittent turbulent political past as well as from the significant challenges of maintaining adequate vaccine supplies and managing the necessary cold chain requirements by the Ministry of Health (MoH).7
The Ebola outbreak likely compromised the immunisation programme further. The ‘no touch’ policy and restriction of invasive procedures, plus the suspension of routine immunisations in some counties during the outbreak, may have resulted in vaccination opportunities being missed.8–10 All planned national immunisation campaigns were suspended during the outbreak,10 and due to human resource constraints, HCWs were not in a position to extend immunisation through outreach services.10 Likewise, the community perceptions of an increased risk of contracting EVD in health facilities may have prevented care givers from seeking immunisation services for their children.5
The effects of the Ebola outbreak are particularly relevant to the immunisation programme, as children aged ⩽4 years are among those with the highest risk for mortality from EVD.11 This group is also at the highest risk of mortality from other preventable childhood infectious diseases, such as measles, pneumonia and meningitis.12 The World Health Organization (WHO) recommends that children receive the following vaccines before 1 year of age: bacille Calmette-Guérin (BCG), polio, pentavalent (diphtheria, pertussis, Haemophilus influenze, tetanus, hepatitis B), measles, yellow fever and pneumococcal.13 To attain herd immunity in a target population, immunisation coverage for most antigens should be at least 85%.13
The virulent nature of the disease, coupled with infection and deaths among health workers, led to a significant decrease in the use of and access to primary health care services, including the routine immunisation programme for children aged <1 year. The countrywide consequences of the Ebola outbreak on the immunisation programme in Liberia remain largely unknown. No peer-reviewed studies have specifically assessed the effects of the outbreak on child immunisation at national level in affected countries.
The present study aimed to examine the effects of the Ebola outbreak on national immunisation services, with specific objectives to estimate, at the national level, 1) the number of children aged <1 year who received the recommended vaccines; 2) the number of immunisations given at fixed facilities and outreach settings; and 3) the number of reported cases of measles and pertussis among children aged <5 years before, during and after the outbreak.
The insights from this study will contribute to bridging the knowledge gap on the effects of the outbreak on immunisation services and will guide both the post-Ebola recovery process and strategic planning for future outbreak responses in Liberia and elsewhere.
METHODS
Study design
This was a descriptive cross-sectional study using routine programme data.
Study setting
General setting
Liberia is situated on the west coast of Africa, with a projected population of four million, 59% of whom live in urban areas; 17% of the population are children aged <5 years.14 Life expectancy is 61 years, and an estimated 54% live in poverty.15 Liberia is divided into 15 counties, subdivided into 91 health districts and managed by a decentralised health system. Primary health care, including routine paediatric care and immunisation services in public health facilities, are generally free of charge for all.16,17
The immunisation programme
In 2015, routine vaccines (BCG, oral polio, pentavalent, measles, yellow fever and pneumococcal) were provided free of charge in 522 health facilities. These services are provided by both public and private fixed facilities and community outreach. A trained vaccinator usually administers the vaccines. A registrar in charge of the health registers collects data from the vaccinators, compiles the reports and submits them in a consolidated health-reporting format to the officer in charge of the health facility. The final validated monthly reports are submitted to the district health officer. These reports are uploaded electronically at the county level into the District Health Information System, version 2 (DHIS-2, Oslo, Norway).
Study population
All children aged <1 year in Liberia who received routine immunisation and all children aged <5 years who suffered from measles or pertussis before (July–December 2013), during (July–December 2014) and after (July–December 2015) the Ebola outbreak were included in the study.
Data variables
The following variables were included: target population, month, year, number of immunisations for each antigen (BCG, oral polio 1, 2 and 3, pneumococcal 1, 2 and 3, pentavalent 1, 2 and 3, measles and yellow fever), type of setting (health facility or outreach), number of measles and pertussis cases among children aged < 5 years, and total number of children aged <5 years.
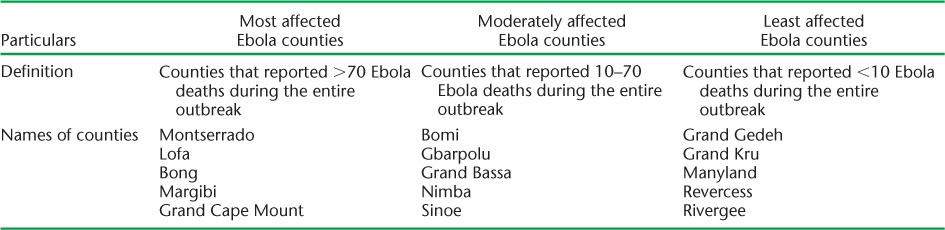
Analysis and statistics
All data were extracted from DHIS-2 using a standardised form. The data were analysed using EpiData Analysis software, version 2.2.2.182 (EpiData Association, Odense, Denmark). Depending on the number of deaths due to Ebola during the entire outbreak period, the counties were categorised as most (>70 deaths), moderately (10–70 deaths) and least (<10 deaths) affected by Ebola for analytical comparisons. The list of counties in each category is given in Table 1.
TABLE 1.
Categorisation of counties by level of Ebola infection, Liberia, 2013–2015
Ethics approval
Ethics approval was obtained from the University of Liberia-Pacific Institute for Research and Evaluation Institutional Review Board, Monrovia, Liberia, and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France. As de-identified aggregate routine programme data were used, informed consent from the participants was not required.
RESULTS
Of the total number of immunisation reports expected each month during the study period, the number of reports received varied from 83% of 496 in 2013, to 66% of 517 in 2014 and 78% of 522 in 2015.
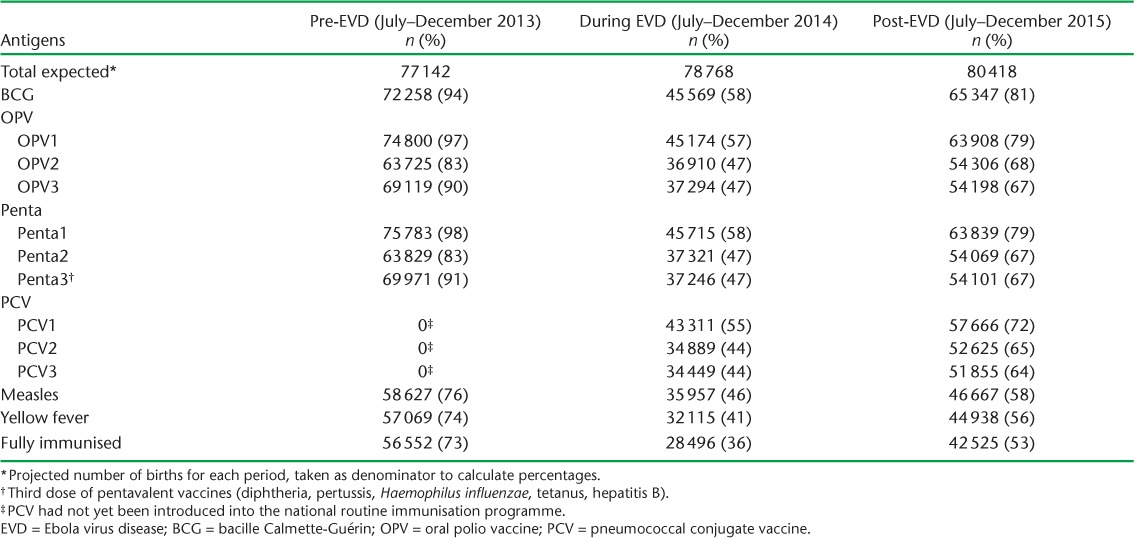
Overview of immunisation coverage
The total number of children immunised during the three study periods is shown in Table 2. There was a reduction in the number of children immunised for all antigens by almost 50% during the Ebola period. The proportion of children immunised for Penta3 before, during and after the Ebola outbreak was respectively 91%, 47% and 67%, while the proportion immunised for measles was respectively 76%, 46% and 58%. The proportion of children fully immunised was respectively 73%, 36% and 53%.
TABLE 2.
Antigen immunisation coverage in children aged <1 year before, during and after the EVD outbreak, Liberia, 2013–2015
Immunisation trends in children
Figure 1 shows the monthly trend of fully immunised children in the study period. The decline in mean monthly numbers of children fully immunised before and during the Ebola period was 4676 (50%). The trend increased after the Ebola period by 49% compared to during the Ebola period. The immunisation trends in facilities and through outreach services are shown in Figure 2. While both trends mirrored the trends of full immunisation, recovery was more robust in the case of facility-based immunisation.
FIGURE 1.
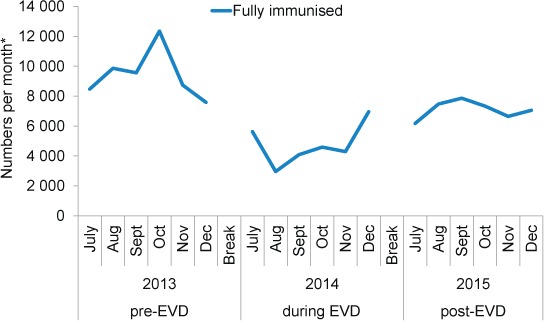
Number of children aged <1 year fully immunised before, during and after the Ebola outbreak, Liberia, 2013–2015. Pre-EVD = July–December 2013; during EVD = July–December 2014; post-EVD = July–December 2015. * Total number of children aged <1 year fully immunised each month in all counties. EVD = Ebola virus disease.
FIGURE 2.
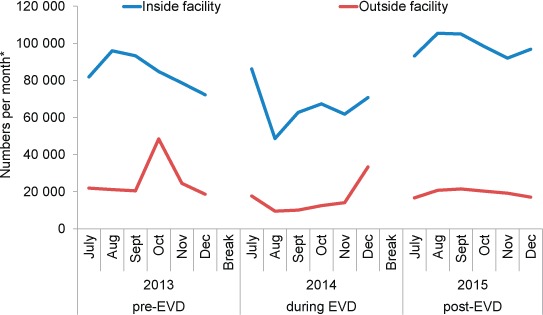
Total number of immunisations performed in facilities and outreach sessions before, during and after the Ebola outbreak, Liberia, 2013–2015. Pre-EVD = July–December 2013; during EVD = July–December 2014; post-EVD = July–December 2015. * Total number of immunisations administered together for all antigens per month. EVD = Ebola virus disease.
Comparison of vaccinations by level of Ebola outbreak in counties
The vaccination coverage for Penta3 and measles antigens and the number of fully immunised children were compared by level of Ebola infection in the counties (Table 3A–C). The proportions of immunisation for Penta3, measles and fully immunised children dropped during the Ebola period (compared to pre-Ebola) across all counties, but the decrease was greatest in the most Ebola-affected counties, by respectively 54%, 49% and 58% (Table 3A).
TABLE 3.
Comparison of three key vaccinations before, during and after the EVD outbreak by type of counties affected by EVD, Liberia, 2013–2015
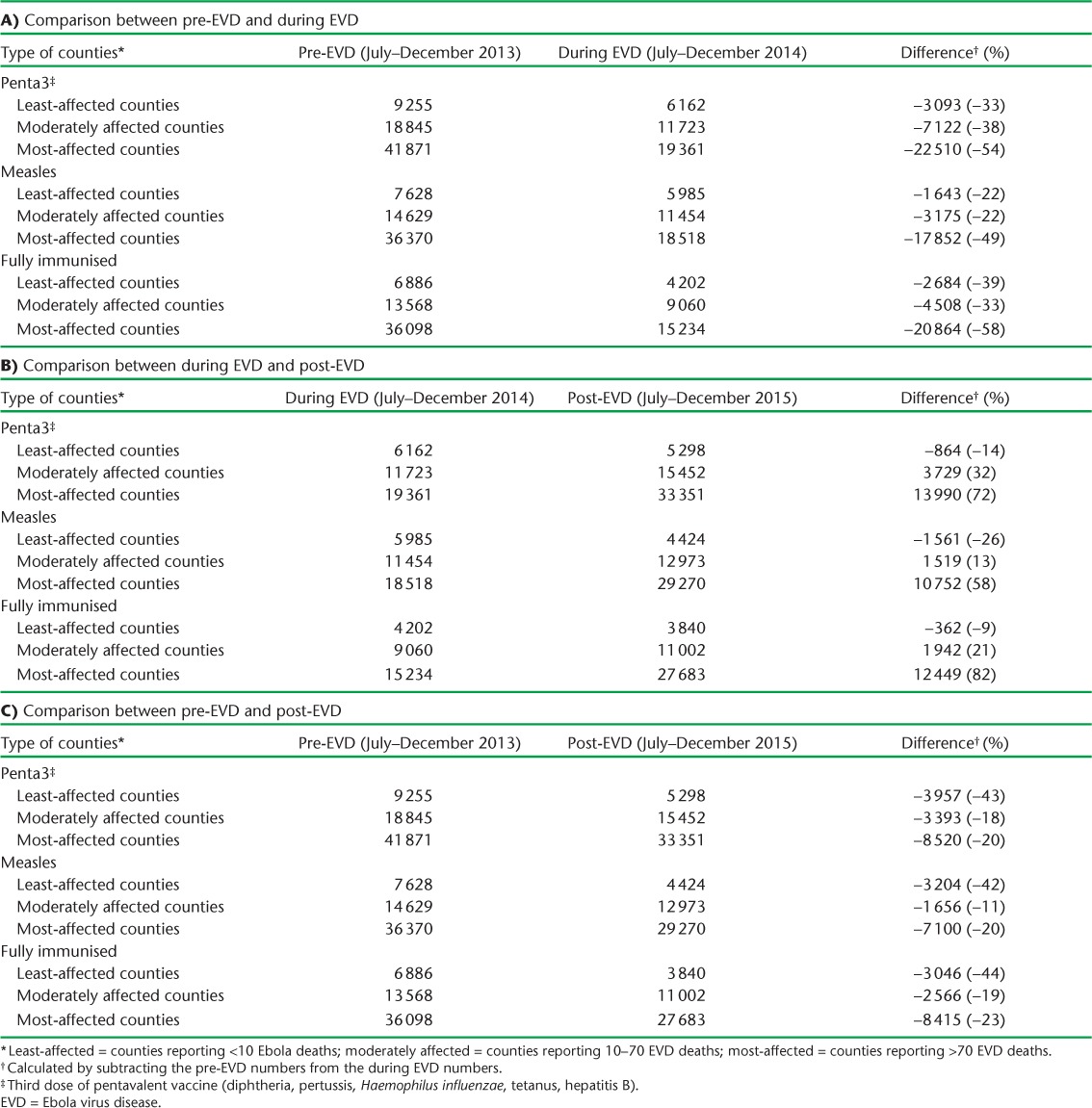
The proportions vaccinated with Penta3, measles and full immunisation showed variable increases in the post-Ebola period (compared to during Ebola) in the most and moderately affected counties. These proportions in the least-affected counties decreased instead by respectively 14%, 26% and 9% (Table 3B).
The level of Penta3 and measles vaccination coverage along with full immunisation in the post-Ebola period was still lower than baseline (pre-Ebola period) (Table 3C). Recovery was nevertheless better in the most and moderately Ebola affected counties than in the least-affected counties.
Trends in measles and pertussis
Figure 3 shows the trends in measles and pertussis cases among children aged <5 years. There was a marked rise in measles cases after the Ebola outbreak, with a monthly mean of 60 compared to 12 pre-Ebola and 16 during the Ebola outbreak.
FIGURE 3.
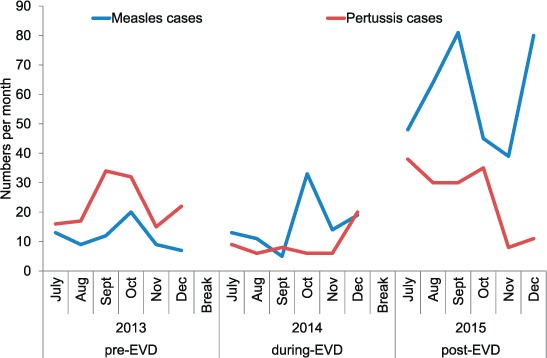
Trends in measles and pertussis cases before, during and after the EVD outbreak, Liberia, 2013–2015. Pre-EVD = July–December 2013; during EVD = July–December 2014; post-EVD = July–December 2015. EVD = Ebola virus disease.
DISCUSSION
This is the first study to date to look at the effects of the Ebola outbreak on a national immunisation programme in West Africa. There was a significant decrease in the monthly reports received during the Ebola outbreak. While baseline immunisation coverage was low before the Ebola outbreak, it declined further during the outbreak. The decreases were more marked in facility-based immunisation. Furthermore, the most Ebola-affected counties showed a greater decline during the outbreak than the least-affected counties. Recovery was also slow in outreach immunisations and in the least-affected counties. Finally, there was a sudden rise in reported measles cases in the post-Ebola period.
There was an overall reduction in the number of children immunised during the outbreak, which is consistent with the notion of reduced health services use secondary to community perceptions of an increased risk of contracting Ebola. The Liberian health workforce was severely affected during the outbreak, with many people dying due to Ebola and many more repurposed to deal with the epidemic.7 This, coupled with the ‘no touch’ policy in which health workers were ordered not to practise invasive procedures, might have contributed to the severe reduction in the number of vaccines provided, as most vaccines (except polio) require injection.8
Taken together, these factors most likely contributed to the decline in the number of children immunised nationally. It is understandable that the decline in facility-based immunisation was greater due to the closure of health facilities and limited health staffing.10 It is also predictable that the level of risk perception and the constraints in health resources varied between the least Ebola-affected counties and the most affected counties. The priority of Ebola control, coupled with constraints in logistical supplies, may also have played a role in the higher decline in immunisation coverage among counties most affected by Ebola.
The least Ebola-affected areas faced pre-existing challenges such as remoteness, geographic barriers and limited resources. The study region, in south-east Liberia, is usually cut off from the rest of the country during the rainy season (April–September), which coincided with the peak of the Ebola outbreak. As there were fewer Ebola cases in these areas, investment and capacity development initiatives were minimal during and after the outbreak; this might have made recovery more slow in the least affected areas.
The effects of the outbreak on the number of children vaccinated against measles and pertussis may have increased the pool of children susceptible to measles. In addition to the low level of immunisation coverage among children, the number susceptible to measles may have increased due to compromised immunity secondary to malnutrition, as an estimated 4200 children lost their primary care givers during the Ebola outbreak.18,19
This study has several policy implications. First, there is an acute need to focus on strengthening infection prevention control in a fragile health system to reduce the death toll in future outbreaks. This is especially important for an immunisation programme where invasive procedures, such as injections, are used. There is also an acute need for pre-emptive measures to put in place contingent logistical and resource arrangements before similar outbreaks. A recent study in Guinea showed that health programmes could be managed without significant limitations if contingent planning was in place.20 Lessons learnt elsewhere need to be implemented.
Second, while the faster recovery in the most highly Ebola-affected regions is encouraging, there seems to be some complacency in those areas less affected by Ebola. These areas need special attention to scale up immunisation services and prevent a yet greater death toll due to vaccine-preventable diseases. This is of especial concern in the wake of the measles outbreak immediately following the Ebola period.
Third, according to the WHO, immunisation coverage for the majority of antigens should be at least 85% to maximise herd immunity.13 The measures necessary to strengthen the generally low level of immunisation coverage (as evidenced by the poor coverage before the Ebola outbreak), to enhance immunity within the population, include a shift of focus from facility-based immunisation to outreach immunisation, scaling up advocacy, communication and social mobilisation to enhance awareness in the community, measures to enhance parents/guardians' satisfaction and the allocation of more resources and better logistics.
The study has several strengths. It included all health facilities, both public and private, throughout the country. As they were generated from the MoH information system, the study data are representative of the data used to make national decisions and reported to the WHO. Furthermore, the study adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines on the conduct and reporting of observational studies.21
The study also had some limitations. The data lacked disaggregated information on immunisation by sex and socio-economic background. As we used monthly aggregated data, linked, interdependent characteristics could not be reported. Furthermore, routine programme data may have some inherent reporting errors. However, it is more likely that the total number of diseases preventable by vaccines was actually under-reported during and following the Ebola outbreak, making our findings even more notable.
In conclusion, this study provides insight into the effects of an Ebola outbreak on countrywide immunisation services. We found that the Ebola outbreak weakened a struggling national immunisation programme and that post-outbreak recovery took significant time, which, taken together, likely resulted in an increase in the number of measles cases reported.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR Geneva, Switzerland). The training model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union; Paris, France) and Médecins Sans Frontières (MSF; Paris, France). The specific SORT IT programme that resulted in this publication was jointly developed and implemented by the WHO/TDR, the Liberia Ministry of Health (Monrovia), WHO Liberia (Monrovia, Liberia) and the Centre for Operational Research, The Union. Mentorship and the coordination/facilitation of the SORT IT workshops were provided through the Centre for Operational Research, The Union; The Union SouthEast Asia Office, New Delhi, India; the Ministry of Health, Government of Karnataka, Bangalore, India; the Operational Research Unit (LUXOR), MSF, Brussels Operational Centre (AMPATH), Luxembourg; Academic Model Providing Access to Healthcare, Eldoret, Kenya; the Baroda Medical College, Vadodara, India; the Institute of Medicine, University of Chester, Chester, UK; The Lighthouse Trust, Lilongwe, Malawi; and Aklilu Lemma Institute of Pathobiology, Addis Ababa, Ethiopia.
The programme was funded by the Department for International Development (London, UK) and WHO/TDR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with the WHO's open-access publication policy for all work funded by the WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution Intergovernmental organizations license (http://creativecommons.org/licenses/by/3.0/igo/legalcode) which permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
References
- 1. World Health Organization. . World Health Organization response to the Ebola (EVD) outbreak. Geneva, Switzerland: WHO, 2014. www.afro.who.int/index.php? Accessed March 2017. [Google Scholar]
- 2. World Health Organization. . Ebola data and statistics. Geneva, Switzerland: WHO, 2016. http://apps.who.int/gho/data/view.ebola-sitrep.ebola-country-LBR-new-conf-prob-districs-20160120-graphs?lang=en Accessed March 2017. [Google Scholar]
- 3. Varpilah S T, Safer M, Frenkel E, Baba D, Massaquoi M, Barrow G.. Rebuilding human resources for health: a case study from Liberia. Hum Resour Health 2011; 9: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. . Health worker Ebola infections in Guinea, Liberia and Sierra Leone: a preliminary report. WHO/EVD/SDS/REPORT/2015.1 Geneva, Switzerland: WHO, 2015. http://www.who.int/csr/resources/publications/ebola/health-worker-infections/en/ Accessed March 2017. [Google Scholar]
- 5. Matanock A, Arwady M A, Ayscue P, . et al. Ebola virus disease cases among health care workers not working in Ebola treatment units—Liberia, June–August, 2014. MMWR Morb Mortal Wkly Rep 2014; 63: 1077– 1081. [PMC free article] [PubMed] [Google Scholar]
- 6. Liberia Institute of Statistics and Geo-Information Services. . Liberia Demographic and Health Survey 2013. Monrovia, Liberia: Liberia Institute of Statistics and Geo-Information Services, 2014. [Google Scholar]
- 7. Ministry of Health Liberia. . Liberia effective vaccines management (EVM) assessment report, 2015. Monrovia, Liberia: MoH, 2015. [Google Scholar]
- 8. Centers for Disease Control and Prevention. . Recommendations for managing and preventing cases of malaria in areas with Ebola. Ebola hemorrhagic fever. Atlanta, GA, USA: CDC, 2015. http://www.cdc.gov/vhf/ebola/outbreaks/malaria-cases.html Accessed March 2017. [Google Scholar]
- 9. Ministry of Health, Liberia. . Infection prevention control (IPC) guidelines for vaccinators. Monrovia, Liberia: MoH, 2014. [Google Scholar]
- 10. Ministry of Health, Liberia. . Liberia expanded program on immunization (EPI) post Ebola recovery plan. Monrovia, Liberia: MoH, 2015. [Google Scholar]
- 11. Agua-Agum J, Ariyarajah A, Blake I M, . et al. Ebola virus disease among children in West Africa. N Engl J Med 2015; 372: 1274– 1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. . Children: reducing mortality. Fact Sheet No. 178 Geneva, Switzerland: WHO, 2013. [Google Scholar]
- 13. World Health Organization. . Vaccination greatly reduces disease, disability, death and inequity worldwide. Geneva, Switzerland: WHO, 2017. http://www.who.int/bulletin/volumes/86/2/07-040089/en/. Accessed March 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liberia Institute of Statistics and Geo-Information Services. . Liberia Households Income and Expenditure Survey 2014 Statistical Abstract. Monrovia, Liberia: LISGIS, 2016. [Google Scholar]
- 15. United Nations Development Programme. . Human Development Report 2014. New York, NY, USA: UNDP, 2014. http://hdr.undp.org. [Google Scholar]
- 16. Ministry of Health, Liberia. . National Health Policy and Plan 2011–2021. Monrovia, Liberia: MoH, 2011. [Google Scholar]
- 17. Ministry of Health, Liberia. . Country Situational Analysis Report, 2011. Monrovia, Liberia: MoH, 2011. [Google Scholar]
- 18. Evans D K, Popova A.. West African Ebola crisis and orphans. Lancet 2015; 385: 945– 946. [DOI] [PubMed] [Google Scholar]
- 19. Rice A L, Sacco L, Hyder A, Black R E.. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull World Health Organ 2000; 78: 1207– 1221. [PMC free article] [PubMed] [Google Scholar]
- 20. Ortuno-Gutierrez N, Zachariah R, Woldeyohannes D, . et al. Upholding tuberculosis services during the 2014 Ebola storm: an encouraging experience from Conakry, Guinea. PLOS ONE 2016; 11: e0157296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Von Elm E, Altman D G, Egger M, . et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453– 1457. [DOI] [PubMed] [Google Scholar]


