Abstract
Setting: Recognising the importance of infection prevention and control (IPC), a minimum standards tool (MST) was developed in Liberia to guide the safe (re-) opening and provision of care in health facilities.
Objectives: To analyse the implementation of specific IPC measures after the 2014 Ebola virus outbreak between June 2015 and May 2016, and to compare the relative improvements in IPC between the public and private sectors.
Design: A retrospective comparative cohort study.
Results: We evaluated 723 (94%) of the 769 health facilities in Liberia. Of these, 437 (60%) were public and 286 (40%) were private. There was an overall improvement in the MST scores from a median of 13 to 14 out of a maximum possible score of 16. While improvements were observed in all aspects of IPC in both public and private health facilities, IPC implementation was systematically higher in public facilities.
Conclusions: We demonstrate the feasibility of monitoring IPC implementation using the MST checklist in post-Ebola Liberia. Our study shows that improvements were made in key aspects of IPC after 1 year of evaluations and tailored recommendations. We also highlight the need to increase the focus on the private sector to achieve further improvements in IPC.
Keywords: IPC checklist, assessment tool, public, SORT IT, operational research
Abstract
Contexte : En reconnaissance de l'importance de la prévention et contrôle de l'infection (PCI), le Liberia a élaboré le « minimum standards tool » (MST) afin de guider en toute sécurité l'ouverture/réouverture des structures de santé et la prestation de soins.
Objectifs : Analyser la mise en œuvre des mesures spécifiques de PCI après la flambée épidémique d'Ebola en 2014, entre juin 2015 et mai 2016, et comparer les améliorations relatives de la PCI entre le secteur public et privé.
Schéma : Une étude rétrospective comparative de cohorte.
Résultats : Nous avons évalué 723 (94%) des 769 structures de santé au Liberia. Parmi elles, 437 (60%) étaient publiques et 286 (40%), privées. Il y a eu une amélioration générale des scores MST depuis une médiane de 13 à 14, avec un score maximal de 16. Des améliorations ont été observées dans tous les aspects de la PCI à la fois dans les structures de santé publiques et privées, mais la mise en œuvre de la PCI a été systematiquement plus élevée dans les structures publiques.
Conclusions: Nous avons démontré la faisabilité du suivi de la mise en œuvre de la PCI grâce à la check-list de la MST dans le Liberia d'après Ebola. Nous avons montré des améliorations dans des aspects clés de la PCI après une année d'évaluation et adapté les recommandations de la PCI. Nous mettons également en lumière le besoin d'accorder davantage d'attention au secteur privé, de manière à faire davantage de progrès dans la PCI.
Abstract
Marco de referencia: Al reconocer la importancia de las medidas de prevención y control de las infecciones (PCI), se elaboró en Liberia un instrumento de normas mínimas encaminado a orientar la apertura o reapertura y la prestación de servicios en los establecimientos de atención de salud de manera segura.
Objetivos: Analizar la ejecución de medidas específicas de PCI después de la epidemia del Ébola del 2014, entre junio del 2015 y mayo del 2016, y comparar los progresos relativos en la materia entre el sector público y el sector privado.
Método: Un estudio retrospectivo de cohortes comparativo.
Resultados: Se evaluaron 723 de los 769 establecimientos de salud de Liberia (94%). De estos, 437 pertenecían al sector público (60%) y 286 (40%) al sector privado. Se observó una mejoría global en las puntuaciones del instrumento de normas mínimas de una mediana de 13 a 14, sobre una puntuación máxima de 16. Hubo progresos en todos los aspectos de PCI en los establecimientos del sector público y privado, pero su aplicación fue sistemáticamente más alta en los centros del sector público.
Conclusiones: El presente estudio puso en evidencia la factibilidad de vigilar la ejecución de las medidas de PCI utilizando la lista de verificación del instrumento de normas mínimas, después de la epidemia del Ébola en Liberia. Los resultados revelaron progresos en aspectos primordiales, después de un año de evaluaciones y recomendaciones adaptadas en materia de PCI. Se destacó además la necesidad de aumentar la atención prestada al sector privado, con el fin de promover mayores progresos en este campo.
The largest Ebola virus disease (EVD) outbreak to date in West Africa devastated the countries of Guinea, Liberia and Sierra Leone, with 28 616 cases and 11 310 deaths recorded as of 10 June 2016. In Liberia, there were more than 10 678 cases and 4810 deaths,1 including 372 cases among health-care workers (HCWs), resulting in 184 deaths.2 The impact and effect of EVD on health-care service delivery was significant, reflected by the steadily decreasing numbers of patients accessing health services in the early phase of the outbreak.3 The primary reasons for this decrease included the fear of contracting EVD from HCWs, the feeling of not being protected, and insecurity, prejudice and discrimination.4 At the beginning of the outbreak, HCWs did not have the ability to practise and maintain a safe working environment, and infection prevention and control (IPC) measures were limited; no IPC policies or guidelines existed and no routine evaluations of IPC were conducted in health facilities prior to the EVD outbreak.5–8 Due to the large number of deaths among health staff and the loss of community confidence in the health system, many health facilities closed completely during the outbreak.9
The EVD outbreak and the ensuing breakdown of the health system, the high burden of EVD among HCWs, the fact that health facilities acted as drivers of EVD transmission during the outbreak,10 and the closure of health facilities, all highlighted the importance and the necessity of IPC as the only measure capable of protecting patients, visitors, care givers, frontline HCWs and crucial health facilities in the face of a deadly outbreak.11 IPC knowledge and good practices consequently became a national priority in the affected countries, including Liberia.12
Studies have shown the powerful impact of using checklists as a tool for both IPC improvement as well as for monitoring and evaluating IPC practices, and particularly for reducing healthcare-associated infections (HAI).13,14 In view of this, the minimum standards tool (MST) checklist, assessing basic IPC elements, was developed in Liberia by a national IPC taskforce and introduced in February 2015 to determine whether clinics, health centres and hospitals could safely reopen and provide safe patient care.8,15 The MST checklist was originally designed to curtail disease transmission through direct and indirect contact and through droplet dispersal; airborne transmission was not explicitly targeted. However, despite the implementation of the MST checklist, the overall IPC situation for health facilities in post-EVD Liberia has not been systematically reported, and the various interventions put in place to improve IPC have not been evaluated. These initiatives may be of considerable relevance to other countries working on safeguarding health facilities in the case of outbreaks of both EVD and other infectious diseases.
We therefore conducted a study in Liberia's health facilities to describe the implementation of IPC measures shortly after the EVD outbreak, and to compare the level of IPC implementation after 1 year of tailored IPC interventions, including addressing infrastructural gaps, providing supportive supervision, mentorship, the provision of IPC supplies and specific training. As marked differences in IPC implementation have been documented in the literature between the public and private sectors, we also compared the changes made in the public and private facilities in Liberia.16–19
METHODS
Study design
This was a retrospective pre- and post-intervention study comparing IPC implementation before and after a set of tailored IPC interventions in private and public health facilities in Liberia.
General setting
Located in West Africa, Liberia is bordered by Guinea in the north, Sierra Leone in the west, Ivory Coast in the east and the Atlantic Ocean in the south. It has a total population of 4 million (2014), comprising 16 ethnic groups. There are 15 administrative subdivisions, known as counties, which are further divided into a total of 91 health districts. One third of the total population lives in Montserrado County, where Monrovia, the capital city, is located. Liberia experienced a protracted civil war from 1989 to 2003.
Liberia's health system
Liberia's Ministry of Health (MoH) provides the central policy for and oversight of the health sector on behalf of the government of Liberia. The National Health Policy and Plan (2011–2021) is predicated on the primary health care (PHC) approach, which decentralises resource management and health service delivery to the counties under the County Health Administration, with a focus on the community level. The national health system provides health services at three levels—primary, secondary and tertiary—with a referral system to ensure a continuum of care from the basic to higher levels, including in emergency situations. The Essential Package of Health Services (EPHS) introduced under the National Health Policy and Plan 2011–2021 stipulates the type of services to be delivered at each level of care.20 The primary health-care level is comprised of health clinics providing basic preventive and curative health services. The secondary level is comprised of health centres that provide primary care, with up to 40-bed capacity and referral services, and county referral hospitals that provide common surgical care and emergency/intensive care. The tertiary or central referral level provides specialist care.
There is a wide range of service delivery providers in Liberia, including government, faith-based, local and international non-governmental and private sector organisations. While the proportion of government expenditure on health care increased from 6.7% in 2000 to 13.2% in 2012, it is still less than the 15% target set in the Abuja Declaration.21,22 As of May 2016, there were 769 health facilities in the country, comprising 36 hospitals, 61 health centres and 672 clinics. The majority of these are public (84% vs. 16% private), excluding Montserrado County, where the majority of health facilities are private (81% vs. 19% public).
The health system in Liberia faced structural and resource vulnerabilities following the 14-year civil conflict; these were further aggravated by the Ebola outbreak.23
Infection prevention and control
During the peak of the Ebola outbreak, a national IPC taskforce was established to provide guidance to patients and HCWs on how to protect themselves during the EVD outbreak in the short term, and in the long term to create an IPC culture to prevent future outbreaks within the health-care facilities. Prior to the EVD outbreak, no IPC policies or guidelines existed in Liberia. In January 2015, the Liberian MoH requested the taskforce to develop a checklist of minimum standards to ensure that health-care facilities could operate and provide care in a safe environment. Officially named the Liberia Health System Minimum Standards for Safe Care Provision by Healthcare Facilities in the Context of Ebola, and referred to as the MST, it helped to coordinate IPC activities and implementing partners.8 The minimum standards address IPC core components, which include administrative control, staff training and health, IPC supply and equipment, triage and isolation capacity, IPC-specific human resources in each health facility and waste management.15 IPC teams, comprised of IPC focal persons from county health teams and county-based World Health Organization (WHO) IPC focal persons, visited health facilities using the MST to evaluate the implementation of the IPC standards; tailored interventions were subsequently implemented to address the gaps identified.24 Both public and private facilities received similar IPC evaluations and interventions.
The tailored interventions included supportive supervision to build a team approach towards problem solving. When assessing the facility using the MST, the IPC team identified gaps and provided support, such as specific training or development of an action plan to address specific gaps, to the on-site IPC officer. During this process, the on-site IPC officer became a mentor for her/his co-workers. Specific training covered topics such as sterilisation processes or surgical care.
Study population and period
Public and private health facilities, including hospitals, health centres and clinics, which were assessed for IPC implementation in June–July 2015 for the baseline and in February–May 2016 for the follow-up, were included in the study. A total of 3552 assessments were conducted using the MST over the study period, leading to an average of 4.6 assessments per facility.
Data variables, sources of data and data collection
Data were sourced from the assessment information collected by the Ebola IPC teams using the MST at county level for each facility. Baseline and 1-year follow-up data were collected respectively in June–July 2015 and April–May 2016. Data were collected on paper during the evaluation visits and entered into an Excel database (Microsoft Corp, Redmond, WA, USA). All records were cross-checked for validity.
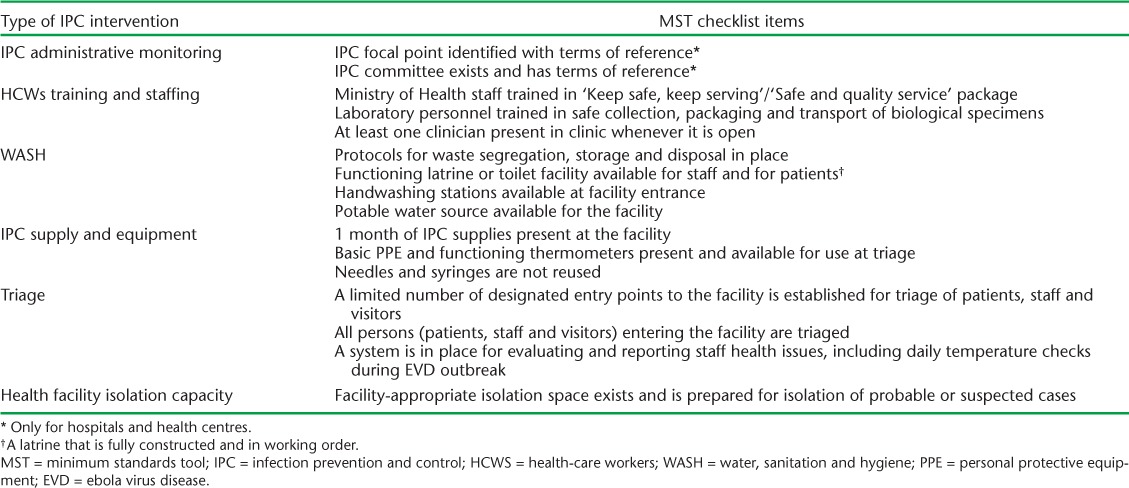
Output indicators were the overall MST scores for 16 key questions (yielding a score between 0 and 16) and the degree of implementation of six core aspects of IPC practice (Table). Implementation for each IPC aspect was classified as not implemented (no requirements met), partially implemented (at least one requirement met) or fully implemented (all requirements met).
TABLE.
MST checklist items extracted individually for the evaluation of specific aspects of IPC implementation in Liberia, June 2015–May 2016
Sample size and statistical analysis
The data entered into Excel were exported and analysed using EpiData Analysis (v. 2.2.2.183, EpiData Association, Odense, Denmark). Comparisons of the overall IPC implementation (MST scores) before and after the interventions, disaggregated by facility ownership, were performed using the Wilcoxon signed-rank test. The proportions of facilities with no, partial or full implementation for specific components of the MST checklist before and after the intervention, again disaggregated by facility ownership, were compared using the χ2 test, with levels of significance set at 5%.
Ethics approval
Permission for the study was sought from the MoH, Monrovia, Liberia. Ethics approval was obtained from the Liberia National Ethics Committee (Monrovia) and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (Paris, France).
RESULTS
We evaluated 723 (94%) of a total of 769 facilities in Liberia. Of these, 437 (60%) were public and 286 (40%) were private. The distribution per county is shown in Figure 1. Hospitals represented 37 (5%) of the evaluated facilities, health centres 63 (9%) and clinics 623 (86%).
FIGURE 1.
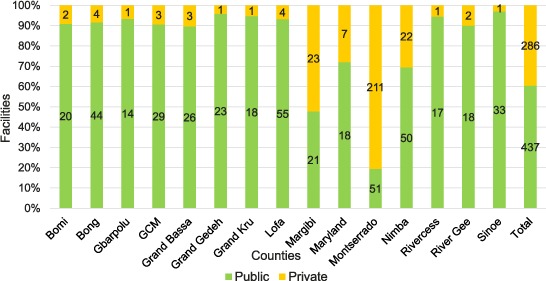
Proportion of public and private facilities evaluated per county, Liberia, May 2016.
Overall, there was an improvement in the median MST scores from a baseline of 13 (interquartile range [IQR] 10–14) to 14 (IQR 12–15) in the follow-up period (Figure 2). While statistically significant improvements were observed in both public and private facilities between baseline and follow-up, MST scores for public facilities were systematically higher than for private facilities.
FIGURE 2.
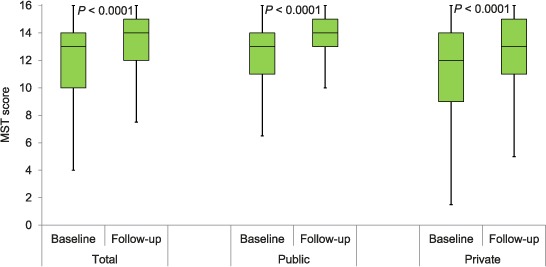
Baseline and follow-up MST score in 723 health facilities (437 public and 286 private), Liberia, June 2015–May 2016. MST = minimum standards tool.
The changes in the implementation of IPC measures for the six key components of the MST for public and private facilities are shown in Figure 3 (A–F). Similar to the overall MST scores, improvement (a shift to better implementation) was observed for all components; the magnitude of the improvements was systematically greater in the public sector. The MST components that rely on infrastructure, i.e., water, sanitation and isolation capacity, tended to score lower than those linked to procedural issues, including administrative monitoring, guaranteeing adequate IPC supplies and implementation of appropriate triage procedures. IPC implementation linked to staffing and staff training, while showing improvement at 1 year follow-up, also continued to fall short of complete implementation (64% in the public and 51% in the private sector).
FIGURE 3.
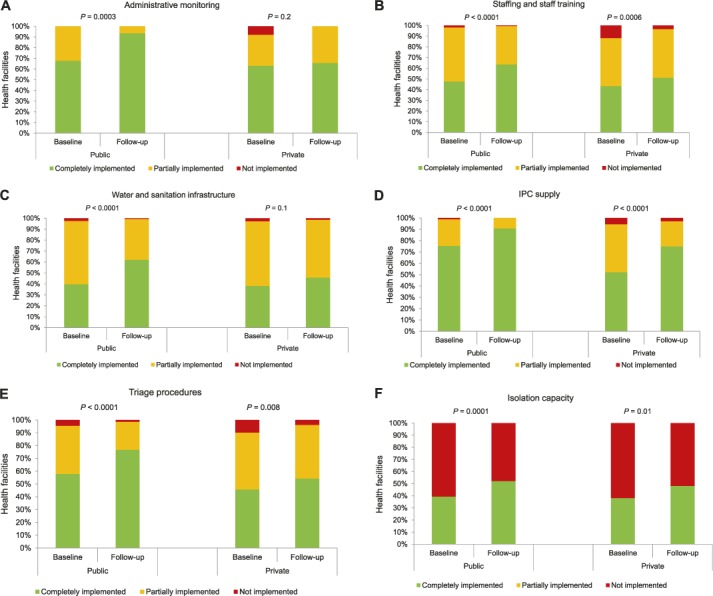
Implementation of IPC measures as assessed by the MST at baseline and after follow-up, Liberia, June 2015–May 2016. Not implemented is defined as no requirements met; partially implemented is defined as at least one requirement met; completely implemented is defined as all requirements met. A) Administrative monitoring. B) Staffing and training. C) Water and sanitation infrastructure. D) IPC supply. E) Triage procedures. F) Isolation capacity. IPC = infection prevention and control; MST = minimum standards tool.
DISCUSSION
This is the first study to document the use of the MST score as an assessment tool for health facility IPC implementation. It also represents one of the first overviews of the IPC situation in health facilities in West Africa following the 2014 EVD outbreak. We show that wide national coverage of facilities could be achieved using the MST tool over a short timeframe, even in the immediate post-EVD context, and that significant improvements in the implementation of IPC measures were observed over the course of 1 year of IPC interventions. As in other IPC studies, the improvements were greater in magnitude in the public vs. the private sector.17–19
A key strength of this study is that it assessed almost all of the health facilities in Liberia, and the findings are thus representative of the situation countrywide. Only facilities that were inaccessible and new facilities that were added after the baseline assessments were excluded. This may, however, have led to a slight overestimation of the IPC situation, as poorly accessible facilities may be more likely to suffer challenges to IPC implementation, particularly in terms of supply and staffing. The conduct and reporting of the study adhered to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines and sound ethics principles.25,26 One limitation of the study is that in the baseline assessments some IPC officers did not receive adequate orientation on how to use the MST checklist, as staff turnover was high and the amount of time available for training was limited in the immediate aftermath of the EVD outbreak. This may have introduced some heterogeneity into the answers based on the understanding of the question by the assessor. As the MST checklist mainly focuses on quantitative IPC indicators (structural aspects) that are easier to assess in an objective manner, however, we do not anticipate that the lack of training had a significant impact on the study findings.
The administrative monitoring of IPC, i.e., the existence of an IPC focal point and an IPC committee with clear terms of reference, restricted to health centres and hospitals only, saw a marked improvement over the year in the public sector, although only limited improvement was seen in private facilities, even though the same interventions were provided in both sectors. This may have been a consequence of the obligation for the public sector to follow directives from the MoH to have IPC committees and identify focal persons following the EVD outbreak. Such directives could not be enforced in the private sector. Similarly, staffing and training improved significantly in the public sector, and less so in the private sector; this may have been a consequence of the over-representation of the public sector compared to the private sector in training in Safe Quality Services (SQS).
The study has several implications. First, we have demonstrated that it is possible to achieve nearly national coverage of health facilities with a simple IPC tool—the MST checklist—and that this tool, paired with the requisite human resources, can register improvements in the IPC situation in the different facilities. The focus on structural issues allows the tool to be implemented with only limited training for assessors over a short period of time, suggesting that it is particularly appropriate for emergency or immediate post-emergency settings, where staff are overburdened and time is of the essence. However, as procedural/behavioural issues play a major role in the overall IPC situation of a health facility, and such issues are poorly addressed by the MST checklist, other assessment tools may be required in the longer term. Liberia is currently in the early process of developing and piloting a new assessment tool focusing on IPC procedures.
Second, the finding that facilities in the private sector showed more limited improvements in the IPC situation than their counterparts in the public sector highlights the need to adapt IPC interventions to the health facility. Private facilities may have different priorities and resources available for IPC, and the government may have less ability to enforce specific directives and guidelines in the private sector. Systematic inclusion of the private sector is recommended, for example, in initiatives such as SQS training. Suboptimal IPC interventions could have grave consequences, including, but not only, for HAI, which have been shown to play an important role in the West Africa Ebola outbreak, with many adverse consequences.5,9 Further research is needed, including qualitative and cost studies, to better understand the determinants of poor IPC implementation in the private sector. Research could also include a thorough analysis of the incidence of HAI and/or the occurrence of infections among HCWs, in relation to the implementation of different IPC measures.
Third, the improvements seen in the IPC situation as a result of the implementation of the MST tool are encouraging, illustrating that changes can be effected over a relatively short period of time. The specific actions taken in Liberia, which may have relevance for other countries facing similar IPC challenges, include recruitment and training of national IPC officers, development of a national IPC programme and guidelines and the systematic integration of the private sector in MoH programmes, training and assessments. Another initiative that may be beneficial in the future is the development of certification and accreditation processes that are applicable to all facilities, regardless of type or ownership. It should be noted, however, that IPC measures relying on infrastructural adaptation, such as ensuring appropriate water and sanitation infrastructures and providing isolation capacity, have been shown to be much more challenging to achieve, and a specific focus on the infrastructural rehabilitation of facilities to meet IPC requirements may be necessary. Likewise, appropriate staffing and staff training remain a challenge, and there is an urgent need for a more cohesive curriculum around IPC for HCWs of all cadres.
In conclusion, this study confirms the feasibility of monitoring IPC implementation in a low-income country in a post-emergency context by implementing an MST checklist. Improvements were demonstrated in key aspects of IPC after 1 year of evaluation and tailored IPC recommendations. The study also highlights the need for increased focus on the private sector to achieve further improvements in implemented IPC interventions.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). The training model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Médecins Sans Frontières (MSF, Geneva, Switzerland). The specific SORT IT programme that resulted in this publication was jointly developed and implemented by the WHO/TDR, the Liberia Ministry of Health and Social Welfare (Monrovia), the WHO Country Office for Liberia (Monrovia) and the Centre for Operational Research, The Union. Mentorship and the coordination/facilitation of the SORT IT workshops were provided through the Centre for Operational Research, The Union; The Union South-East Asia Regional Office (New Delhi, India); the Ministry of Health, Government of Karnataka (Bengaluru, India); the Operational Research Unit (LUXOR), MSF, Brussels Operational Centre (Luxembourg); AMPATH (Eldoret, Kenya); Baroda Medical College, (Vadodara, India); Institute of Medicine, University of Chester (Chester, UK); Lighthouse Trust (Lilongwe, Malawi); and Aklilu Lemma Institute of Pathobiology, Addis Ababa University (Addis Ababa, Ethiopia).
The authors thank the numerous colleagues who made significant contributions during the Liberian IPC response. While they did not specifically contribute to this article, the authors acknowledge colleagues from Liberia's Ministry of Health (Monrovia), partner and WHO IPC colleagues who developed the minimum standards tool (MST) checklist and undertook the MST assessments referenced in this article.
The programme was funded by the Department for International Development (London, UK) and the WHO/TDR. An important portion of the IPC work reported in this paper was funded by the United States Office for Disaster Assistance (United States Agency for International Development, Washington, DC, USA). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with WHO's open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO license (http://creativecommons.org/licenses/by/3.0/igo/legalcode) that permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
References
- 1. World Health Organization. . Ebola situation report. 20 January 2016. Geneva, Switzerland: WHO, 2016. http://apps.who.int/ebola/current-situation/ebola-situation-report-20-january-2016 Accessed February 2017. [Google Scholar]
- 2. Ministry of Health. . Investment plan for building a resilient health system, Liberia 2015–2021. Monrovia, Liberia: MoH, 2015. [Google Scholar]
- 3. Arwady M A, Bawo L, Hunter J C, . et al. Evolution of Ebola virus disease from exotic infection to global health priority, Liberia, mid-2014. Emerg Infect Dis 2015; 21: 578– 584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sagoe-Moses C, Pearson R D, Perry J, Jagger J.. Risks to health care workers in developing countries. N Engl J Med 2001; 345: 538– 541. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. . Health worker Ebola infections in Guinea, Liberia and Sierra Leone. Preliminary report. WHO/EVD/SDS/REPORT/2015.1 Geneva, Switzerland: WHO, 2015. http://www.who.int/csr/resources/publications/ebola/health-worker-infections/en/ Accessed February 2017. [Google Scholar]
- 6. Nyarko Y, Goldfrank L, Ogedegbe G, Soghoian S, de-Graft Aikins A, NYU-UG-KBTH Ghana Ebola Working Group. . Preparing for Ebola Virus Disease in West African countries not yet affected: perspectives from Ghanaian health professionals. Global Health 2015; 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smego R A, Sarwari A R, Siddiqui A R.. Crimean-Congo hemorrhagic fever: prevention and control limitations in a resource-poor country. Clin Infect Dis 2004; 38: 1731– 1735. [DOI] [PubMed] [Google Scholar]
- 8. Cooper C, Fisher D, Gupta N, Macauley R, Pessoa-Silva C L.. Infection prevention and control of the Ebola outbreak in Liberia, 2014–2015: key challenges and successes. BMC Med 2016; 14: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hageman J C. Infection prevention and control for Ebola in health care settings—West Africa and United States. MMWR 2016; 65 Suppl: 4– 11. [DOI] [PubMed] [Google Scholar]
- 10. Merler S, Ajelli M, Fumanelli L.. Spatiotemporal spread of the 2014 outbreak of Ebola virus disease in Liberia and the effectiveness of non-pharmaceutical interventions: a computational modelling analysis. Lancet Infect Dis 2015; 15: 204– 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Matanock A, Arwady M A, Ayscue P, . et al. Ebola virus disease cases among health care workers not working in Ebola treatment units—Liberia, June–August, 2014. MMWR Morb Mortal Wkly Rep 2014; 63: 1077– 1081. [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. . Liberia: survivors help train health workers for Ebola care. Geneva, Switzerland: WHO, 2014. [Google Scholar]
- 13. Pronovost P J, Goeschel C A, Colantuoni E, . et al. Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ 2010; 340: c309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Morton A, Cook D, Mengersen K, Waterhouse M.. Limiting risk of hospital adverse events: avoiding train wrecks is more important than counting and reporting them. J Hosp Infect 2010; 76: 283– 286. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization. . Core components of infection prevention and control programmes in health care. Geneva, Switzerland: WHO, 2011. [Google Scholar]
- 16. Aslesh O P, Ubaid N P, Nagaraja S B, . et al. Compliance with infection control practices in sputum microscopy centres: a study from Kerala, India. Public Health Action 2015; 5: 255– 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Amoran O, Onwube O.. Infection control and practice of standard precautions among healthcare workers in northern Nigeria. J Glob Infect Dis 2013; 5: 156– 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Oli A N, Okoli K C, Ujam N T, Adje D U, Ezeobi I.. Health professionals' knowledge about relative prevalence of hospital-acquired infections in Delta State of Nigeria. Pan Afr Med J 2016: 24: 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Barden-O'Fallon J, Barry M A, Brodish P, Hazerjian J.. Rapid assessment of Ebola-related implications for reproductive, maternal, newborn and child health service delivery and utilization in Guinea. PLOS Curr 2015; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ministry of Health. . National Health and Social Welfare Policy and Plan 2011–2021. Monrovia, Liberia: MoH, 2011. [Google Scholar]
- 21. World Health Organization. . The Abuja declaration: ten years on. Geneva, Switzerland: WHO, 2011. [Google Scholar]
- 22. World Health Organization. . World health statistics 2015. Geneva, Switzerland: WHO, 2015. [Google Scholar]
- 23. Ministry of Health. . Investment plan for building a resilient health system in Liberia (2015 to 2021) in response to the Ebola virus disease outbreak. Monrovia, Liberia: MoH, 2015. [Google Scholar]
- 24. World Health Organization. . Interim infection prevention and control guidance for care of patients with suspected or confirmed filovirus haemorrhagic fever in health-care settings, with focus on Ebola. WHO/HIS/SDS/2014.4Rev.1 Geneva, Switzerland: WHO, 2014. [Google Scholar]
- 25. von Elm E, Altman D G, Egger M, . et al. The Strengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med 2007; 45: 247– 251. [DOI] [PubMed] [Google Scholar]
- 26. Edginton M, Enarson D, Zachariah R, . et al. Why ethics is indispensable for good-quality operational research. Public Health Action 2012; 2: 21– 22. [DOI] [PMC free article] [PubMed] [Google Scholar]


