Abstract
Purpose The purpose of this study was to compare complication rates following inpatient versus outpatient distal radius fracture ORIF and identify specific complications that occur at increased rates among inpatients.
Methods Using the 2005–2013 ACS-NSQIP, we collected patient demographics, comorbidities, surgical characteristics, and 30-day postoperative complications following isolated ORIF of distal radius fractures. A propensity score matched design using an 8-to-1 “greedy” matching algorithm in a 1:4 ratio of inpatients to outpatients was utilized. Rates of minor, major, and total complications were compared. A multinomial logistic regression model was then used to assess the odds of complications following inpatient surgery.
Results Total 4,016 patients were identified, 776 (19.3%) of whom underwent inpatient surgery and 3,240 (80.3%) underwent outpatient surgery. The propensity score matching algorithm yielded a cohort of 629 inpatients who were matched with 2,516 outpatients (1:4 ratio). After propensity score matching, inpatient treatment was associated with increased rates of major and total complications but not with minor complications. There was an increased odds of major complications and total complications following inpatient surgery compared with outpatient surgery. There was no difference in odds of minor complications between groups.
Conclusion Inpatient operative treatment of distal radius fractures is associated with significantly increased rates of major and total complications compared with operative treatment as an outpatient. Odds of a major complication are six times higher and odds of total complications are two and a half times higher following inpatient distal radius ORIF compared with outpatient. Quality improvement measures should be specifically targeted to patients undergoing distal radius fracture ORIF in the inpatient setting.
Keywords: complications, distal radius, inpatient, open reduction and internal fixation, outpatient
National health care costs, which comprised 17.2% of the U.S. gross domestic product (GDP) in 2012, continue to rise at an alarming rate, 1 causing some payers to advocate for a bundled-payment system. 2 Medicare has already begun bundling payments for selected orthopaedic diagnosis-related groups (DRGs) including major joint arthroplasty with the intention of expanding this system to include all orthopaedic subspecialties. 3 4 5 Under a bundled payment system, health care facilities receive a single index lump-sum payment for a particular DRG, which would be expected to cover all costs of care during a 90-day period beginning with the date of surgery. Importantly, facilities and surgeons would not receive additional reimbursement for treatment of patient complications and/or readmissions during this time period. As a result, rates of perioperative adverse events for facilities and individual surgeons will be monitored closely, 6 7 and successfully delivering high-quality care while maintaining low complication rates will be paramount. An effective strategy for improving quality of care and minimizing complications is to identify patients at high risk for developing adverse events following common orthopaedic procedures. Targeted interventions can then be developed aimed at decreasing complication rates in these high-risk patient populations.
Fractures of the distal radius are the most common injuries treated by orthopaedic surgeons, representing 17.5% of all fractures. 8 These injuries follow a bimodal distribution, occurring frequently in younger patients following high-energy mechanisms of injury and in older patients following lower-energy trauma. 9 While many distal radius fractures can be successfully treated nonoperatively, certain displaced and unstable fracture patterns often require surgical intervention. Risk factors for complications following open reduction and internal fixation (ORIF) of distal radius fractures were reported in a recent publication by Schick et al using the 2011 American College of Surgeons' National Surgical Quality Improvement Program (NSQIP) database. 10 Overall complication rates were generally low, but the authors reported a significantly higher rate of complications among patients who underwent distal radius ORIF in the inpatient setting compared with the outpatient setting. However, as the authors acknowledged, there were significant differences in patient demographics and medical comorbidities between inpatient and outpatient groups, and these differences were not evaluated with further statistical analysis. Additionally, the specific complications experienced by inpatient and outpatient groups were not reported.
Using the updated 2013 NSQIP database, the purpose of our study was to use a rigorous statistical model to compare complication rates following inpatient versus outpatient ORIF of a distal radius fracture. We also sought to identify specific complications that occur at increased rates among inpatients. The main hypothesis of this study was that the rate of complication after ORIF for distal radius fractures is higher among inpatients compared with outpatients.
Materials and Methods
Data Extraction
This investigation was initiated following institutional review board approval. This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Access to the NSQIP dataset collected between 2005 and 2013 was granted by the American College of Surgeons. The dataset includes 462 hospitals across the United States and 34 hospitals in other countries including Saudi Arabia, Canada, Lebanon, the United Kingdom, and the United Arab Emirates. The 135 patient variables reported within the database include preoperative risk factors, intraoperative variables, and 30-day postoperative mortality and morbidity outcomes for patients undergoing major surgical procedures in both inpatient and outpatient settings. At each participating institution, two risk-assessment nurses trained as Surgical Clinical Reviewers (SCR) were appointed to collect data directly from patients' medical records. Inter-rater reliability disagreement of < 5% per site was considered acceptable. Audit reports of NSQIP data collection have identified disagreement rates of < 1.8%. 11
Patient Selection
All patients who underwent ORIF of a distal radius fracture during the study period were identified from the NSQIP dataset using Current Procedural Terminology (CPT) codes. Patients who had one of the following three procedures were eligible for inclusion in the study:
Open treatment of distal radial extra-articular fracture or epiphyseal separation (25607)
Open treatment of distal radial intra-articular fracture or epiphyseal separation, with internal fixation of two fragments (25608)
Open treatment of distal radial intra-articular fracture or epiphyseal separation, with internal fixation of three or more fragments (25609)
Patient demographics (including age, sex, and race) and preoperative comorbidities (including body mass index [BMI]), recent weight loss (> 10% in the last 6 months), insulin-dependent diabetes mellitus, smoking status, alcohol use, functional status, dyspnea, history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), hypertension requiring medication, history of esophageal varices, disseminated cancer, steroid use, bleeding disorders, hemodialysis, chemotherapy within 30 days of surgery, and radiotherapy within 90 days of surgery) were recorded. Operative characteristics including systemic inflammatory response syndrome (SIRS), sepsis, or septic shock at time of surgery, operative time, wound class, and American Society of Anesthesiologists (ASA) score were also recorded. Patients with incomplete data (including demographics, preoperative comorbidities, and/or operative characteristics) were excluded from the analysis.
Patients were categorized into inpatient and outpatient groups based on their admission status as entered in the NSQIP database. This designation is determined by each hospital's definition of inpatient and outpatient status, but generally outpatient status is utilized to describe patients who are brought to the hospital or facility for surgery from their present home or living situation on the day the procedure is performed and are discharged within 24 hours. 11
Outcome Measures
Perioperative complications within 30 days were categorized as either minor or major based on previously published literature using the NSQIP database. 12 13 14 15 16 17 Minor complications included wound dehiscence, superficial wound infection, pneumonia, and urinary tract infection. Major complications included deep wound infection, organ space infection, myocardial infarction, pulmonary embolism, deep venous thrombosis, cerebrovascular accident, postoperative neurologic deficit, sepsis, septic shock, coma, and death. A third outcome measure—total complications—was determined by identifying all patients who developed at least one minor and/or major complication.
Data Analysis
Baseline demographic characteristics were compared using chi-square tests for categorical variables and Wilcoxon-Mann-Whitney tests for continuous variables. Rates of minor, major, and total complications were calculated for the inpatient and outpatient groups. Complication rates between groups were compared using chi-square tests.
To control for differences between inpatient and outpatient groups, we utilized a propensity score matched study design. The propensity score model estimated for each patient the probability of undergoing outpatient surgery based on patient demographics (age, ASA physical status, BMI, sex, and smoking status), preoperative comorbidities (weight loss > 10% in the last 6 months, diabetes, dyspnea, use of steroids, bleeding disorders, dialysis, functional status, history of COPD, history of CHF, and disseminated cancer), and surgical procedure. Propensity scores were used to match inpatients and outpatients in a 1-to-4 ratio using an 8-to-1 “greedy” matching algorithm. This “greedy” matching algorithm obtains the best fit between patients in each cohort by first attempting to match patients' propensity scores to 8 decimal places. If not possible, propensity scores are matched to 7 decimal places and so on, down to 1 decimal place. Continuous variables were modeled using restricted cubic splines with 4 knots, and categorical variables were modeled using indicator/dummy variables.
After propensity score matching, rates of minor, major, and total complications were again compared for the matched inpatient and outpatient groups using chi-square tests. A multinomial logistic regression model was then utilized to calculate the odds of minor and major postoperative complications within 30 days following inpatient surgery, using outpatient surgery as a control and adjusting for length of surgery using restricted cubic splines. A separate logistic regression model was then used to determine the odds of total complications (at least one minor and/or major complication) following inpatient versus outpatient ORIF, again adjusting for length of surgery. Statistical analysis was performed using Stata Statistical Software: Release 13 (StataCorp LP 2013, College Station, TX). Significance was set at p < 0.05.
Results
A total of 4,361 patients who underwent ORIF of a distal radius fracture were identified from the 2013 NSQIP database. As displayed in Fig. 1 , 345 (7.9%) patients were excluded due to incomplete demographic or comorbidity data. Of the remaining 4,016 patients, 776 (19.3%) underwent inpatient surgery and 3,240 (80.3%) underwent surgery as outpatients. Prior to propensity score matching, there were significant differences between groups in patient demographics, medical comorbidities, and operative characteristics ( Table 1 ). Rates of minor, major, and total complications between groups before matching are shown in Table 2 . Prior to matching, patients undergoing inpatient surgery had significantly increased rates of minor (1.3 vs. 0.5%, p = 0.009), major (1.9 vs. 0.2%, p < 0.001), and total complications (2.8 vs. 0.7%, p < 0.001).
Fig. 1.
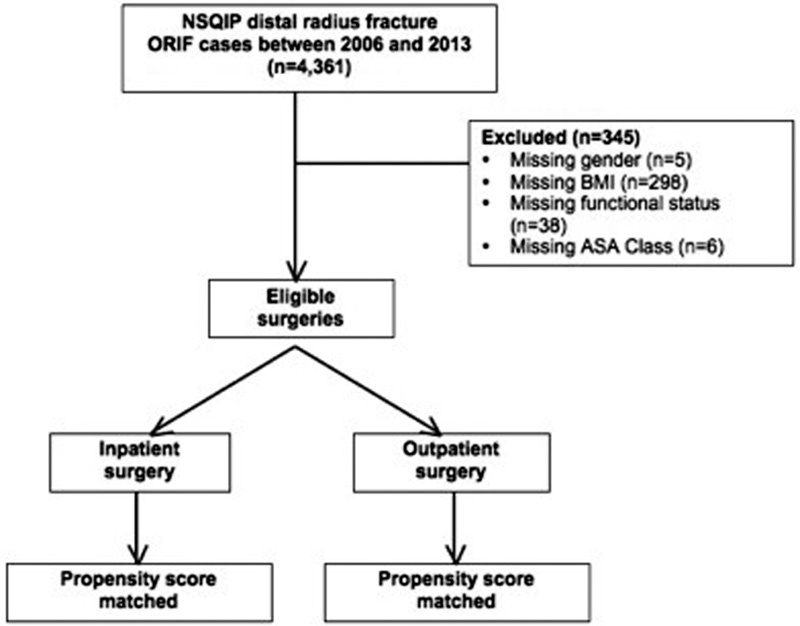
Flowchart showing application of inclusion/exclusion criteria. ASA, American Society of Anesthesiologists; BMI, body mass index; NSQIP, National Surgical Quality Improvement Program.
Table 1. Patient demographics, comorbidities, and operative characteristics among surgically treated distal radius fracture patients by inpatient/outpatient status, before and after propensity score matching.
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Inpatient | Outpatient | p Value | Inpatient | Outpatient | p Value | |
| ( n = 776) | ( n = 3,240) | ( n = 629) | ( n = 2,516) | |||
| Patient demographics | ||||||
| Age (y), median (IQR) | 63 (52–74) | 58 (56–67) | < 0.001 | 74 (62–83) | 74 (62–83) | 0.700 |
| ASA class, median (IQR) | 2 (2–3) | 2 (2–2) | < 0.001 | 2 (2–3) | 2 (2–3) | 0.978 |
| BMI, median (IQR) | 26.9 (23.5–31.6) | 26.6 (23.4–31.4) | 0.539 | 26.7 (23.5–31.5) | 26.8 (23.5–31.4) | 1.000 |
| Male, n (%) | 210 (27.1%) | 895 (27.6%) | 0.753 | 181 (28.8%) | 740 (29.4%) | 0.754 |
| Smoker, n (%) | 140 (18.0%) | 658 (20.3%) | 0.155 | 119 (18.9%) | 484 (19.2%) | 0.856 |
| Preoperative comorbidities | ||||||
| Weight loss > 10% in last 6 mo, n (%) | 1 (0.1%) | 5 (0.2%) | 0.869 | 1 (0.2%) | 2 (0.1%) | 0.564 |
| Diabetic, n (%) | 86 (11.1%) | 268 (8.3%) | 0.013 | 58 (9.2%) | 216 (8.6%) | 0.613 |
| Dyspnea, n (%) | 0.122 | 0.682 | ||||
| No | 738 (95.1%) | 3,130 (96.6%) | 605 (96.2%) | 2,435 (96.8%) | ||
| With moderate exertion | 36 (4.6%) | 102 (3.2%) | 23 (3.7%) | 79 (3.1%) | ||
| At rest | 2 (0.3%) | 8 (0.3%) | 1 (0.2%) | 4 (0.2%) | ||
| Use of steroids, n (%) | 28 (3.6%) | 55 (1.7%) | 0.001 | 15 (2.4%) | 45 (1.8%) | 0.328 |
| Bleeding disorder, n (%) | 49 (6.3%) | 59 (1.8%) | < 0.001 | 8 (1.3%) | 36 (1.4%) | 0.761 |
| On dialysis, n (%) | 4 (0.5%) | 4 (0.1%) | 0.028 | 1 (0.2%) | 1 (0.0%) | 0.289 |
| Functional status, n (%) | < 0.001 | 0.262 | ||||
| Independent | 705 (90.9%) | 3,184 (98.3%) | 623 (99.1%) | 2,502 (99.4%) | ||
| Partially dependent | 66 (8.5%) | 55 (1.7%) | 6 (1.0%) | 14 (0.6%) | ||
| Totally dependent | 5 (0.6%) | 1 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| History of COPD, n (%) | 54 (7.0%) | 96 (3.0%) | < 0.001 | 22 (3.5%) | 84 (3.3%) | 0.843 |
| History of CHF, n (%) | 2 (0.3%) | 2 (0.1%) | 0.120 | 0 (0.0%) | 1 (0.0%) | 0.617 |
| Disseminated cancer, n (%) | 5 (0.6%) | 4 (0.1%) | 0.006 | 1 (0.2%) | 1 (0.0%) | 0.289 |
| Operative characteristics | ||||||
| CPT code, n (%) | 0.007 | 0.688 | ||||
| 25607 | 280 (36.1%) | 1,170 (36.1%) | 217 (34.5%) | 887 (35.3%) | ||
| 25608 | 215 (27.7%) | 1,060 (32.7%) | 192 (30.5%) | 724 (28.8%) | ||
| 25609 | 281 (36.2%) | 1,010 (31.2%) | 220 (35.0%) | 905 (36.0%) | ||
| Length of surgery (min), median (IQR) | 74 (53–105) | 67 (51–89) | < 0.001 | 75 (52–106) | 67 (51–89) | < 0.001 |
| Propensity score, median (IQR) | 0.82 (0.74–0.85) | 0.84 (0.81–0.86) | < 0.001 | 0.83 (0.80–0.85) | 0.83 (0.80–0.85) | 0.834 |
Abbreviations: BMI, body mass index, CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CPT, Current Procedural Terminology; IQR, interquartile range.
Note: Significant findings indicated in bold.
Table 2. Rates of minor, major, and total complications among surgically treated distal radius fracture patients by inpatient/outpatient status, before and after propensity score matching.
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Inpatient | Outpatient | p Value | Inpatient | Outpatient | p Value | |
| ( n = 776) | ( n = 3,240) | ( n = 629) | ( n = 2,516) | |||
| Minor complications, n (%) | ||||||
| Superficial wound infection | 1 (0.1%) | 9 (0.3%) | 0.455 | 1 (0.2%) | 8 (0.3%) | 0.504 |
| Pneumonia | 3 (0.4%) | 2 (0.1%) | 0.021 | 2 (0.3%) | 1 (0.0%) | 0.043 |
| Urinary tract infection | 7 (0.9%) | 4 (0.1%) | < 0.001 | 1 (0.2%) | 3 (0.1%) | 0.802 |
| Any minor complication | 10 (1.3%) | 15 (0.5%) | 0.009 | 4 (0.6%) | 12 (0.5%) | 0.616 |
| Major complications, n (%) | ||||||
| Deep wound infection | 1 (0.1%) | 1 (0.0%) | 0.272 | 1 (0.2%) | 0 (0.0%) | 0.045 |
| Organ space infection | 1 (0.1%) | 1 (0.0%) | 0.272 | 1 (0.2%) | 1 (0.0%) | 0.289 |
| Myocardial infarction | 1 (0.1%) | 0 (0.0%) | 0.041 | 0 (0.0%) | 0 (0.0%) | – |
| Stroke | 1 (0.1%) | 0 (0.0%) | 0.041 | 0 (0.0%) | 0 (0.0%) | – |
| Pulmonary embolism | 1 (0.1%) | 0 (0.0%) | 0.041 | 1 (0.2%) | 0 (0.0%) | 0.045 |
| Deep vein thrombosis | 1 (0.1%) | 1 (0.0%) | 0.272 | 1 (0.2%) | 1 (0.0%) | 0.289 |
| Sepsis | 3 (0.4%) | 0 (0.0%) | < 0.001 | 0 (0.0%) | 0 (0.0%) | – |
| Septic shock | 2 (0.3%) | 0 (0.0%) | 0.004 | 1 (0.2%) | 0 (0.0%) | 0.045 |
| Death within 30 d | 7 (0.9%) | 3 (0.1%) | < 0.001 | 3 (0.5%) | 2 (0.1%) | 0.025 |
| Any major complication | 15 (1.9%) | 6 (0.2%) | < 0.001 | 8 (1.3%) | 4 (0.2%) | < 0.001 |
| Total complications, n (%) | 22 (2.8%) | 21 (0.7%) | < 0.001 | 10 (1.6%) | 16 (0.6%) | 0.018 |
Note: Significant findings indicated in bold.
After the propensity score matching algorithm was performed, 629 patients undergoing inpatient surgery were matched with 2,516 patients undergoing outpatient surgery (1:4 ratio), and these 3,145 patients represented the final study cohort that was included in the multinomial analysis. Distributions of propensity scores before and after matching are displayed in Figs. 2 and 3 , respectively. After matching, there were no significant differences between groups in patient demographics, preoperative comorbidities, or operative characteristics with the exception of length of surgery ( Table 1 , after matching). As shown in Table 2 , after propensity score matching, inpatient treatment was associated with increased rates of major (1.3 vs. 0.2%, p < 0.001) and total complications (1.6 vs. 0.6%, p = 0.018) but not with minor complications (0.6 vs. 0.5%, p = 0.616). Individual complications that occurred at significantly higher rates among inpatients included pneumonia (0.3 vs. 0%, p = 0.043), deep wound infection (0.2 vs. 0%, p = 0.045), pulmonary embolism (0.2 vs. 0%, p = 0.045), septic shock, (0.2 vs. 0%, p = 0.045), and death within 30 days (0.5 vs. 0.1%, p = 0.025).
Fig. 2.
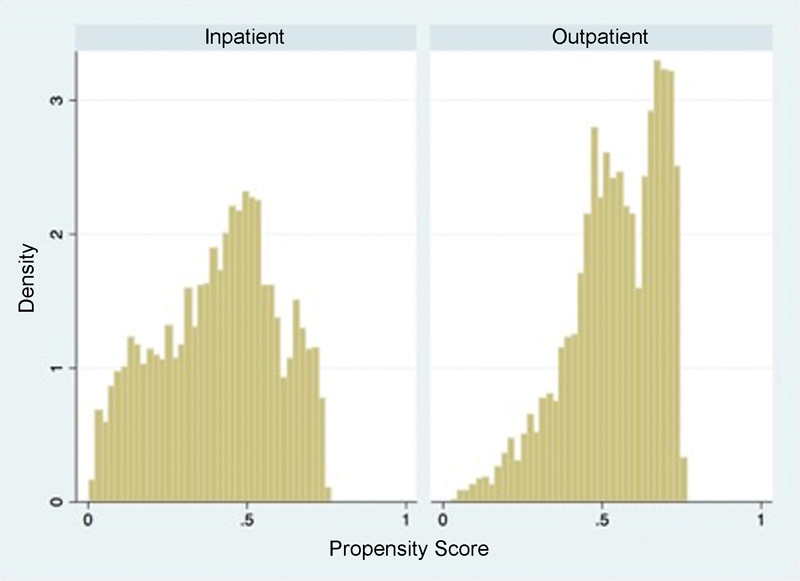
Distribution of propensity scores by inpatient/outpatient status before matching.
Fig. 3.
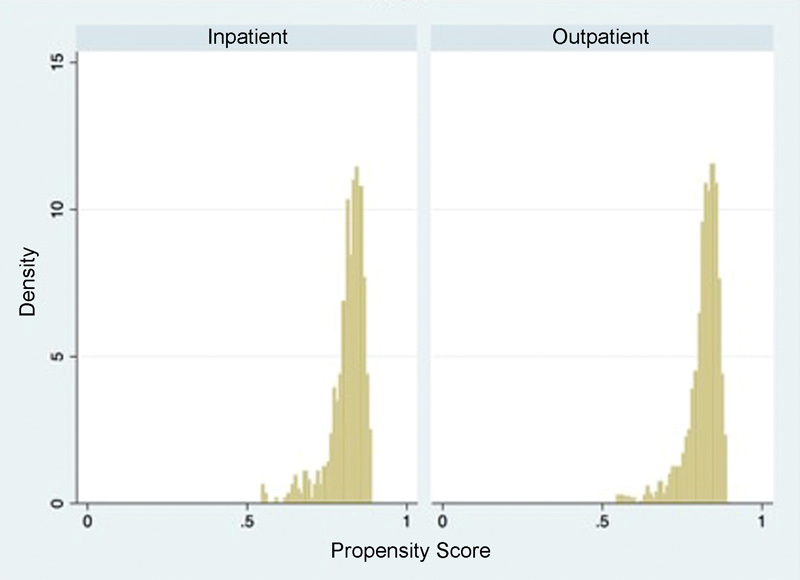
Distribution of propensity scores by inpatient/outpatient status after matching.
After adjusting for length of surgery, multinomial logistic regression analysis demonstrated no difference in odds of a minor complication between inpatient and outpatient groups (adjusted odds ratio [OR] 1.30, 95% CI 0.42–4.05, p = 0.649). However, patients who underwent inpatient surgery had significantly increased odds of major complications (adjusted OR 6.48, 95% CI 1.81–23.19, p = 0.004) and total complications (adjusted OR 2.45, 95% CI 1.10–5.42, p = 0.028) compared with those undergoing outpatient surgery ( Table 3 ).
Table 3. Adjusted a ORs (95% CI) for minor, major, and total complications by inpatient/outpatient status .
| Minor complications | Major complications | Total complications | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Inpatient surgery | 1.30 (0.42–4.05) | 0.649 | 6.48 (1.81–23.19) | 0.004 | 2.45 (1.10–5.42) | 0.028 |
| Outpatient surgery | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
Abbreviations: CI, confidence interval; OR, odds ratio.
Based on multinomial regression analysis of propensity-matched inpatient/outpatient groups, after adjusting for length of surgery.
Note: Significant findings indicated in bold.
Discussion
We utilized the 2013 ACS-NSQIP database to compare complication rates following inpatient versus outpatient ORIF of a distal radius fracture. Using a rigorous statistical model, we demonstrate that inpatient distal radius fracture ORIF is associated with significantly increased odds of major complications and total complications compared with outpatient surgery. Furthermore, our results validate and expand upon the findings of a recent study of distal radius fracture ORIF using the 2011 NSQIP database.
In their recent publication, Schick et al identified risk factors for complications following operative fixation of distal radius fractures. 10 A higher total complication rate following inpatient distal radius fracture ORIF compared with outpatient surgery (10 vs. 1.3%) was reported as a secondary outcome. Interestingly, the authors performed a post hoc univariate analysis between the inpatient and outpatient groups and found significant differences in mean age, incidence of COPD and bleeding disorders, ASA physical status classification, and length of surgery. In their discussion, the authors posited that the increased complication rate seen among inpatients was attributable to the higher incidence of medical comorbidities in this group. However, this hypothesis was not investigated further and the conclusion was therefore not supported statistically.
Our study was specifically designed to investigate complication rates between inpatient and outpatient distal radius fracture ORIF, using a propensity score matched design to control for demographics, comorbidities, and operative characteristics. As seen in Table 1 , this propensity score matching algorithm was effective in generating inpatient and outpatient cohorts with no significant differences in patient demographics, preoperative comorbidities, or operative characteristics except for length of surgery. The success of this algorithm is demonstrated graphically in Figs. 2 and 3 , which depict the distribution of propensity scores both before and after matching. Our multinomial logistic regression analysis was then performed on these matched cohorts after controlling for length of surgery. As such, our conclusions—that inpatient distal radius fracture ORIF is associated with increased odds of major and total complications compared with outpatient surgery—are supported by a statistically rigorous study design and methodology. 18
In addition to validating the findings of Schick et al with a statistically rigorous model, our study also sheds light on the particular complications that affect inpatients preferentially. Although there were no significant differences in odds of aggregate minor complications between groups, patients who underwent inpatient ORIF of a distal radius fracture were more likely to develop pneumonia than those who had outpatient surgery (0.3 vs. 0.0%, p = 0.043). Inpatients also had significantly higher rates of several major complications, including deep wound infection, pulmonary embolism, septic shock, and mortality within 30 days ( Table 2 ). The increased deep wound infection rate among inpatients likely reflects the impact of soft tissue swelling on wound healing potential. Inpatient ORIF in the early postinjury period may place patients at risk for wound complications when surgery is performed through an unfavorable soft tissue envelope. Surgeons must carefully assess the readiness of the soft tissues prior to proceeding with definitive fracture fixation. Increased rates of pulmonary embolism, septic shock, and 30-day mortality among inpatients may indicate the influence of other associated injuries on these specific outcomes. Distal radius fracture fixation should not proceed in the inpatient setting until patients are physiologically stable.
Our study does have some limitations, and foremost is that this study was conducted retrospectively. However, the NSQIP database is comprehensive in its scope and contains prospectively collected data, which largely mitigates this limitation. Large multicenter studies using high-quality, prospectively collected databases such as NSQIP allow surgeons to answer relevant clinical questions while avoiding the significant expense and logistical challenges associated with prospective trials. 12 13 14 15 16 17 Furthermore, we utilized the most updated NSQIP data available, which uses a standardized protocol for reporting complications and has been shown to have inter-rater disagreement rates of < 1.8%. 11 Another limitation of our study is that the NSQIP database does not record complications that occur > 30 days after surgery. However, the fact that we identified significant differences in complication rates between groups within the first 30 days underscores the significance of these findings.
Other limitations include the fact that the NSQIP database does not include functional outcomes or other outcomes specific to ORIF of the distal radius, such as grip strength, wrist range of motion, or fracture union. The addition of functional outcomes scores to large, multicenter databases, particularly for orthopaedic diagnoses or procedures, would greatly improve the utility of these databases to answer clinically relevant questions with greater statistical power. In addition, although our propensity score matched cohorts had no statistically significant differences in patient demographics or preoperative comorbidities, patients who underwent inpatient surgery may have had more complex distal radius fractures or other associated injuries that necessitated inpatient hospitalization. In these situations, even though inpatient surgery is associated with increased complication rates, it may be completely appropriate to perform distal radius ORIF in the inpatient setting to facilitate patient care and expedite recovery.
In conclusion, using the 2013 NSQIP database, we demonstrate that inpatient operative treatment of distal radius fractures is associated with significantly increased odds of major complications (OR 6.48) and total complications (OR 2.45) compared with operative treatment as an outpatient. To decrease complications such as pneumonia, deep wound infection, and pulmonary embolism following ORIF of distal radius fractures, interventions should be specifically targeted to patients undergoing surgery in the inpatient setting. The main hypothesis of this study was verified; higher rates of major complications and total complications exist among the inpatient population as compared with the outpatient population.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest Author William T. Obremskey has done expert testimony in legal matters. The institution of one or more authors (William T. Obremskey) has received a grant from the Department of Defense. The remaining authors certify that they have no commercial associations that might pose a conflict of interest in connection with the submitted article.
Funding
None.
References
- 1.National health expenditures highlightsCenters for Medicare & Medicaid Services; 2012.http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html. Accessed on May, 16 2014
- 2.Bundled payment: AHA research synthesis reportAmerican Hospital Association Committee on Research;2010http://www.aha.org/research/cor/content/BundledPayment.pdf. Accessed on May, 16 2014
- 3.Sood N, Huckfeldt P J, Escarce J J, Grabowski D C, Newhouse J P. Medicare's bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood) 2011;30(09):1708–1717. doi: 10.1377/hlthaff.2010.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fact sheets: bundled payments for care improvement initiative fact sheet. Centers for Medicare & Medicaid Services 2014http://www.cms.gov/Newsroom?mediaReleaseDatabase/Fact-Sheets/2014-Fact-sheets-items/2014-01-30-2.html. Accessed May, 16 2014
- 5.Froimson M I, Rana A, White R E, Jret al. Bundled payments for care improvement initiative: the next evolution of payment formulations: AAHKS Bundled Payment Task Force J Arthroplasty 201328(8, Suppl):157–165. [DOI] [PubMed] [Google Scholar]
- 6.Altman S H. The lessons of Medicare's prospective payment system show that the bundled payment program faces challenges. Health Aff (Millwood) 2012;31(09):1923–1930. doi: 10.1377/hlthaff.2012.0323. [DOI] [PubMed] [Google Scholar]
- 7.Steele J R, Reilly J D. Bundled payments: bundled risk or bundled reward? J Am Coll Radiol. 2010;7(01):43–49. doi: 10.1016/j.jacr.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Court-Brown C M, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(08):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 9.Alffram P A, Bauer G C. Epidemiology of fractures of the forearm. A biomechanical investigation of bone strength. J Bone Joint Surg Am. 1962;44-A:105–114. [PubMed] [Google Scholar]
- 10.Schick C W, Koehler D M, Martin C T et al. Risk factors for 30-day postoperative complications and mortality following open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2014;39(12):2373–23800. doi: 10.1016/j.jhsa.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 11.American College of Surgeons National Surgical Quality Improvement ProgramUser Guide for the Participant Use Data File; 2011.http://acsnsqip.org/main/programspecs/program_data_collection.jsp. Accessed October 4, 2013
- 12.Belmont P J, Jr, Davey S, Orr J D, Ochoa L M, Bader J O, Schoenfeld A J. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(03):370–378. doi: 10.1016/j.jamcollsurg.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Martin C T, Pugely A J, Gao Y, Wolf B R.Risk factors for thirty-day morbidity and mortality following knee arthroscopy: a review of 12,271 patients from the national surgical quality improvement program database J Bone Joint Surg Am 20139514e98(1–10): [DOI] [PubMed] [Google Scholar]
- 14.Pugely A J, Martin C T, Gao Y, Mendoza-Lattes S, Callaghan J J. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95(03):193–199. doi: 10.2106/JBJS.K.01682. [DOI] [PubMed] [Google Scholar]
- 15.Radcliff T A, Henderson W G, Stoner T J, Khuri S F, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(01):34–42. doi: 10.2106/JBJS.G.00065. [DOI] [PubMed] [Google Scholar]
- 16.Schoenfeld A J, Ochoa L M, Bader J O, Belmont P J., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93(17):1577–1582. doi: 10.2106/JBJS.J.01048. [DOI] [PubMed] [Google Scholar]
- 17.Suleiman L I, Ortega G, Ong'uti S K et al. Does BMI affect perioperative complications following total knee and hip arthroplasty? J Surg Res. 2012;174(01):7–11. doi: 10.1016/j.jss.2011.05.057. [DOI] [PubMed] [Google Scholar]
- 18.Linden A, Samuels S J. Using balance statistics to determine the optimal number of controls in matching studies. J Eval Clin Pract. 2013;19(05):968–975. doi: 10.1111/jep.12072. [DOI] [PubMed] [Google Scholar]


