Abstract
Purpose The aim of this study was to evaluate the mid- to long-term outcomes and complications in patients affected by rheumatic diseases treated with the Universal 2 (U2) total wrist arthroplasty (TWA).
Methods We reviewed, in a retrospective, noncontrolled cohort study, 22 patients affected by rheumatoid arthritis (RA), who underwent U2 total wrist replacement between March 2003 and January 2014 for the treatment of 23 rheumatoid wrists with the aim of obtaining the remission of pain and a range of motion (ROM) useful for daily activities, according to the patients' demands, as an alternative to total wrist arthrodesis. The cohort of patients included 20 females and 2 males, with a mean age of 54.9 years. Residual pain, preoperative ROM, postoperative ROM increases, grip strength, radiographic changes, long-term complications, and reasons for revision or failures were evaluated.
Results In this study, 22 patients were evaluated at a mean follow-up of 82.3 months (range: 2–12 years). All patients had good or complete pain relief, the mean visual analogue scale pain score was 0.82. The mean grip strength improved and postoperatively was 11 kg (Jamar). The mean total ROM of flexion–extension was 72.3 degrees; radial–ulnar deviation 24.9 degrees. The mean QuickDASH score of 49 and patient rate wrist/hand evaluation of 41.7 a revision surgical procedure in six cases (26%): in two cases, a carpal component revision procedure and in four cases, total implant failures requiring either conversion to a Swanson spacer or wrist joint fusion.
Conclusion TWA provides pain relief, preserves motion, and improves function in severe degenerative RA. Our results at a mid- to long-term follow-up with the U2 prosthesis were encouraging and represent, when indicated, a valid alternative to fusion which is less appealing for RA patients.
Level of Evidence Level of evidence is therapeutic IV.
Keywords: wrist joint, total wrist arthroplasty, rheumatoid arthritis, Universal 2
Wrist arthroplasty with silicone implants was first popularized by Swanson in the 1960s, and the early results of this procedure were promising. 1 Longer follow-up showed mechanical failure and severe inflammatory reactions caused by silicon. 2 3 4 The second-generation wrist arthroplasties, such as Meuli (1984) and Volz (1976) prostheses, included two metal components which articulated by means of a ball and socket. 5 6 In the 1980s and 1990s, a metal-on-plastic model with a hemispheric design was introduced (Biaxial–De Puy Orthopaedics Inc., Leeds, United Kingdom) to consider the wrist as a bicondylar joint. 7 Most of these implants were recalled due to instability, metacarpal fracture, loosening, and dislocation. The last generation of wrist arthroplasty, known as “anatomical,” represents an effort to prevent such complications via two features: carpal fixation (instead of metacarpal) and a new concept of kinematic through an intercarpal bone fusion, transforming the wrist into a “two-bone” joint. 8 9 Currently, there were three anatomical implants with these characteristics: Universal 2 (U2)/Freedom (Integra LifeSciences, Plainsboro, NJ), Re-Motion total wrist arthroplasty (TWA) (Small Bone Innovations Inc., Morrisville, PA), and Maestro Wrist Reconstructive System (Biomet, Warsaw, IN).
The most common indication for a TWA is rheumatoid arthritis (RA) with progressive pain and loss of function. 10 11 In RA, the involvement of the wrist has been described in several X-rays–based classifications: the Larsen et al's classification is the best known, 12 while the Flury et al's classification is an attempt to be more predictive for the treatment to consider the natural evolution of the disease. 13 Indications for wrist replacement have now been extended to all cases of pancarpal arthritis with total degenerative involvement of the carpus (radiocarpal [RC] and midcarpal [MC]) in Simmen's classification Types I and II (stable forms), and in case of bilateral involvement of the wrist and multiple affected joints. Moreover, it is mandatory to have a good clinical control of the activity of the disease (synovitis) via adequate medical therapy.
The purpose of this retrospective cohort study is to evaluate the outcomes of TWAs with U2 implants in patients affected by RA, focusing on the complications and the survival of the prostheses.
Materials and Methods
From March 2003 to January 2014, we performed 23 wrist replacements in 22 patients with a cementless implant (U2) and resection of the ulnar head. All patients were affected by pancarpal RA. The mean age was 54.9 years (range: 31–73 years). Twenty were women and 2 were men. Sixteen subjects underwent several surgical procedures as summarized in Table 1 . All surgeries were performed by the two senior authors (C.M. and P.S.)
Table 1. Presentation of the series.
| Patients | Age at surgery | Side | Sex | Hobby or sport | Work or occupation | Diagnosis | Others procedures | First surgery | Secondary surgery | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | P.S. | 71 | L | F | Retired | RA | Right wrist arthrodesis | 2003 | 2012 | |
| 2 | R.M. | 42 | R | F | Office worker | RA | Right IV, V extensors repair | 2003 | ||
| 3 | M.L. | 58 | R | F | Housewife | RA | Extensor tendon synovectomy of left wrist | 2004 | ||
| 4 | G.M.F. | 47 | L | F | Cleaning lady | RA | Right RSL fusion, left MP Swanson arthroplasty | 2004 | 2011 | |
| 5 | L.R.G. | 39 | R | F | Teacher | R.A | Right TEA, left RSL, and tenodesis for swan neck deformity of thumb, trapeziectomy, and pyrocarbon interposition arthroplasty, MP fusion of thumb | 2004 | 2006 | |
| 6 | B.P. | 56 | R | F | Housewife | RA | 2006 | |||
| 7 | F.A. | 62 | R | F | Housewife | RA | Right MP Swanson arthroplasty, II MP pyrocarbon arthroplasty, and left RSL fusion | 2006 | 2009 | |
| 8 | C.A. | 68 | L | F | Retired | RA | Left III and IV PIP fusion, right TEA | 2006 | ||
| 9 | M.F. | 36 | R | F | Lawyer | RA | Extensor tendon synovectomy of left wrist, left Darrach | 2006 | ||
| 10 | B.F. | 50 | L | F | Janitor | RA | Right TEA, right RSL fusion, right MP Swanson arthroplasty, right I IP fusion, left MP fusion of the thumb | 2007 | ||
| 11 | G.A. | 42 | R | F | Secretary | RA | 2007 | |||
| 12 | S.W. | 59 | L | F | RA | 2007 | ||||
| 13 | R.A. | 66 | R | F | Piano player | RA | Right III–V extensor repair | 2007 | ||
| 14 | M.M. | 54 | R | F | Retired | RA | Right MP Swanson arthroplasty, III–V flexor tendons repair by graft | 2008 | 2013 | |
| 15 | G.C. | 49 | L | F | Scooter driver | Secretary | RA | 2008 | ||
| 16 | G.V. | 73 | R | M | Woodcarver | RA | Left RSL fusion, III–V extensor repair | 2009 | ||
| 17 | R.A. | 68 | L | F | Piano player | Retired | RA | Left MP fusion of the thumb | 2009 | |
| 18 | B.E. | 61 | L | F | Painting | Writer | RA | Right total wrist fusion, MP fusion of the thumb | 2009 | |
| 19 | M.F.N. | 31 | R | F | Salesperson | RA | Left total wrist fusion | 2009 | ||
| 20 | C.P. | 47 | R | M | Cyclist | Salesperson | RA | Left total wrist fusion, MP Swanson arthroplasty, II, III PIP fusion | 2010 | 2015 |
| 21 | S.D. | 72 | L | F | Retired | RA | Right total wrist fusion, right MP Swanson arthroplasty, right MP, IP fusion of the thumb, left TCS | 2011 | ||
| 22 | C.R. | 59 | R | F | Retired | RA | Right MP Swanson arthroplasty | 2012 | ||
| 23 | S.M. | 54 | L | F | Retired | RA | 2014 |
Abbreviations: CTS, carpal tunnel syndrome; IP, interphalangeal joint; MP, metacarpal-phalangeal joint; RA, rheumatoid arthritis; RSL, radioscapholunate fusions; TEA, total elbow arthroplasty; PIP, proximal interphalangeal joint.
The U2 is a semiconstrained prosthesis providing a double fixation for a distal component (a short central porous-coating stem in the capitate and two self-tapping titanium variable angle screws). Specifically, the implant consists of a polyethylene (ultra-high-molecular-weight polyethylene, UHMWPE) insert and a cobalt–chromium radial component inclined at the level of the joint plateau of 14 degrees. Other features are the ellipsoidal contact surface to increase stability, a convex distal component, and a concave radial component which enhances stability of the implant.
In our series, indications for wrist replacement were pancarpal arthritis with degenerative inflammatory involvement of RC and MC joints; grade 2 or 3 of Larsen or Types I to II of Simmen's classification; bilateral involvement of the wrist; adequate control of the disease; and motivated patients. Contraindications were severe deformity related to irreparable wrist tendon extensors rupture, inadequate skin coverage, infections; progressive unbalanced RA despite a medical therapy. Osteopenia and poor bone stock were considered relative contraindications.
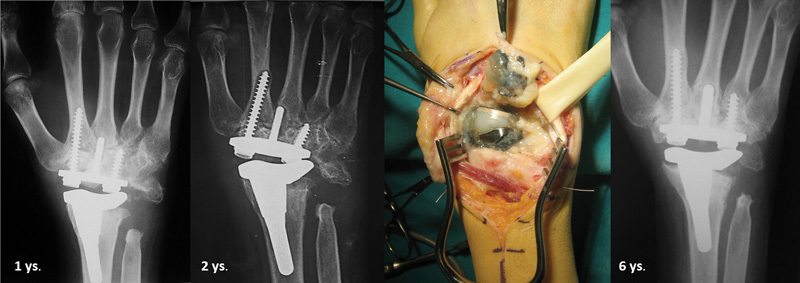
Surgical procedure has been described in the manufacturer's technical guide and literature. 14 15 In all cases, we performed a resection of the caput ulnae with Darrach procedure. Additional steps of the procedure in RA patients should: (1) prepare a “Z” retinacular flap based on the radial side from the VI compartment to run the balancing of the extensor carpi ulnaris (ECU) at the end of the procedure; (2) check for the correct rotational alignment of the radial stem; (3) align the carpal component in relation only to capitate and not considering the third metacarpus, often unaligned in rheumatoid patients ( Fig. 1 ); (4) carpal stem, radial, and ulnar screws have to be aligned in the center of respective bones and on the same level in the frontal plane; (5) perform a solid arthrodesis between carpal bones, using the removed proximal carpal rows as graft, to improve the local bone stock and a stronger integration of the carpal component; (6) test the stability of the trials implant with a shaking maneuver; (7) handling of soft tissue intraoperatively and accurate reconstruction, such as capsule, retinaculum, and ECU.
Fig. 1.
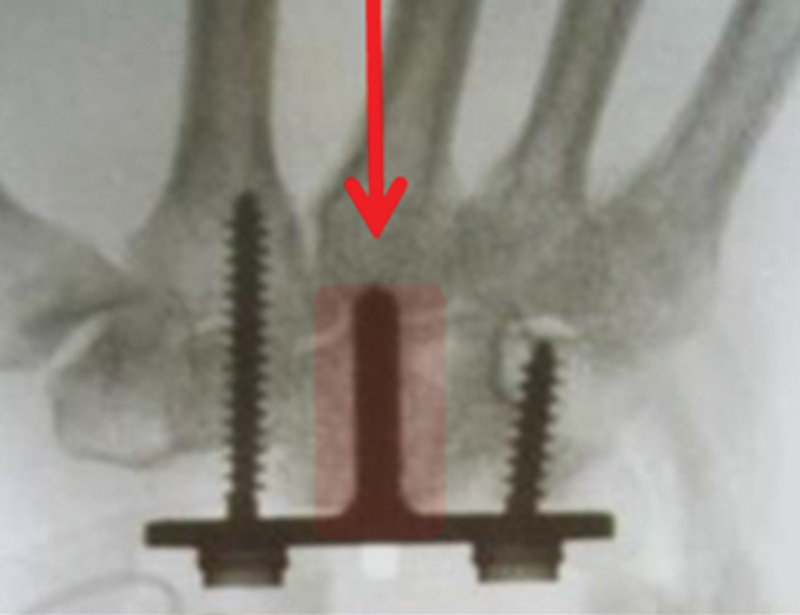
The evolution pattern of the rheumatoid arthritis disease with progressive deviation of metacarpals altering the carpal–metacarpal (capitate—third metacarpal) joint's axis, it is representing a critical point for surgical procedure.
A Kaplan–Meier's survival analysis was performed to calculate the survival curve of the implants; the end point chosen was the time of primary wrist replacement until revision. A revision was defined as an exchange of the whole or parts of the prosthesis or removal of the prosthesis.
Rehabilitative Protocol
After surgery, a bulky dressing was maintained for 2 weeks. After the removal of sutures and bulky dressing substitution with a custom-made plastic splint in a neutral position of the wrist with free fingers, all patients were allowed to temporarily remove the splint to perform active mobilization in flexion–extension and ulnar and radial deviation and gentle stretching exercises, in absence of pain, and assisted by hand therapists. During the sessions, the therapist also performed a gentle passive mobilization preceded by pompage according to Bienfait and scar treatment. 16 All these treatments, followed by cryotherapy, were considered important at this stage to reduce the edema and to maintain the mobility of the fingers. Furthermore, patients had to wear a splint during the night for 4 weeks. After the first X-ray control, 1 month postsurgery, paraffin therapy, isometric contractions of the muscles of the fingers and wrist, and electrotherapy in cases of limited range of motion (ROM) have been prescribed to increase strength. Eight weeks after surgery, the splint was removed, allowing the patients to return within 12 weeks to their daily activities, avoiding weights over 3 kg permanently.
Clinical Evaluation
Symptoms reported by patients before surgery were pain (assessed by a visual analogue scale [VAS] score); reduced active ROM; impairment in daily activities; and deformity and swelling of the wrist. Postoperatively, QuickDASH and patient rate wrist/hand evaluation (PRWHE) scores were analyzed; VAS, ROM, and testing for standard grip strength evaluation compared with the contralateral side (Jamar Hydraulic Hand Dynamometer) were recorded, but these outcomes were limited by the complex underlying disease involving multiple joints.
Whether the patient would repeat this type of surgery was also recorded, and in patients with a contralateral arthrodesis, which of the two was the preferred surgery.
Radiographic Assessment
Preoperative standard X-rays of the wrist were performed. In selected cases, 13 cases out of 23, in which there was doubt whether it would be possible to do a partial arthrodesis or a TWA, a computed tomography scan was also performed to evaluate the degree of bone loss of the radiocarpal and mid-carpal joints.
At the time of final follow-up, all patients were assessed with standard X-rays to evaluate the intercarpal fusion and to detect any radial stress shielding, radiolucent lines, resorption around the stems, migration, and subsidence. X-rays were then performed at 3, 6, and 12 months, and each subsequent year.
Several patterns were described as follows:
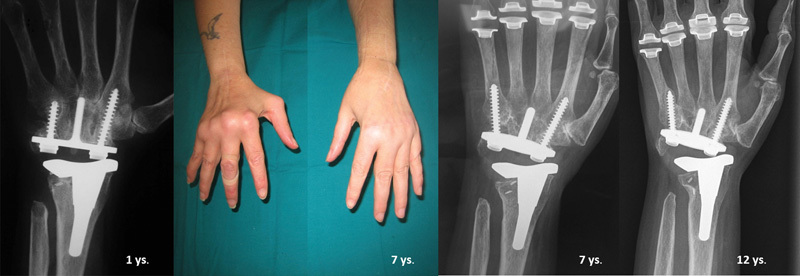
No radiologic changes, stable clinical outcome ( Fig. 2 )
Radiologic changes, stable clinical outcome: (1) radiologic changes (stress shielding, osteolysis, bony resorption, sclerosis, radiolucency) unmodified on subsequent X-rays with stable implant ( Fig. 3 ) and (2) progression of tilting, subsidence, and/or loosening. Implant migration or radiological loosening not related to symptoms but with probable worsening of the clinical setting in the future ( Fig. 4 ). 17 18
Progression of implant tilting, subsidence, and/or loosening with recurrence of synovitis, ongoing RA disease, and symptoms, requiring revision surgery.
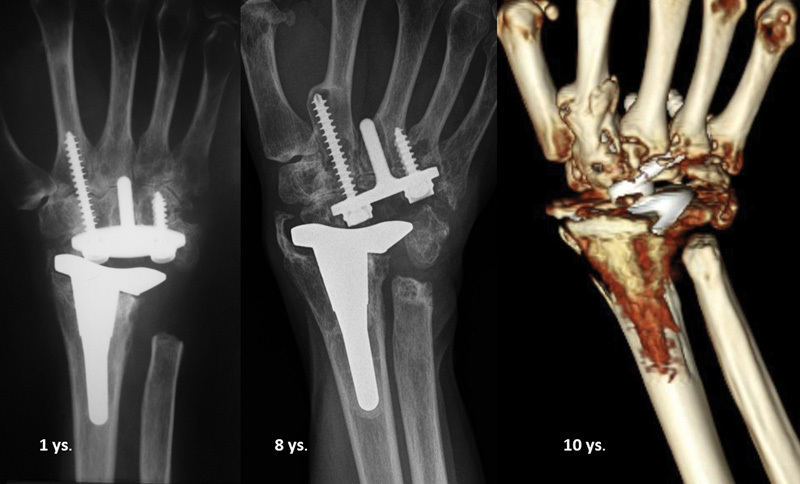
Fig. 2.

Type A radiological pattern: stable over the time.
Fig. 3.

Type B.1: X-ray changes may be observed on sequential X-rays within the first 2 years after surgery; unmodified on the following radiological control at 7 and 9 years after surgery as implants settle in a stable position (case 13).
Fig. 4.
Type B.2: progressive radiological loosening not related to a symptomatic condition (painless, functional range of motion) but with probable worsening of the clinical setting in the future.
Results
The mean follow-up was 82.3 months (range: 24–148 months). In all patients, we observed a significant reduction in pain; the mean VAS score preoperative was 9 and postoperative decreased to 0.82. All patients reported that they would repeat the surgery. Grip strength and manual agility increased in all cases; mean grip strength improved and postoperatively was 11 kg (Jamar Hydraulic Hand Dynamometer). The mean total postoperative flexion–extension ROM of 72.3 degrees (from 38 to 110 degrees) and ROM of radial–ulnar deviation of 24.9 degrees (from 0 to 42 degrees) were noted ( Fig. 5 ).
Fig. 5.
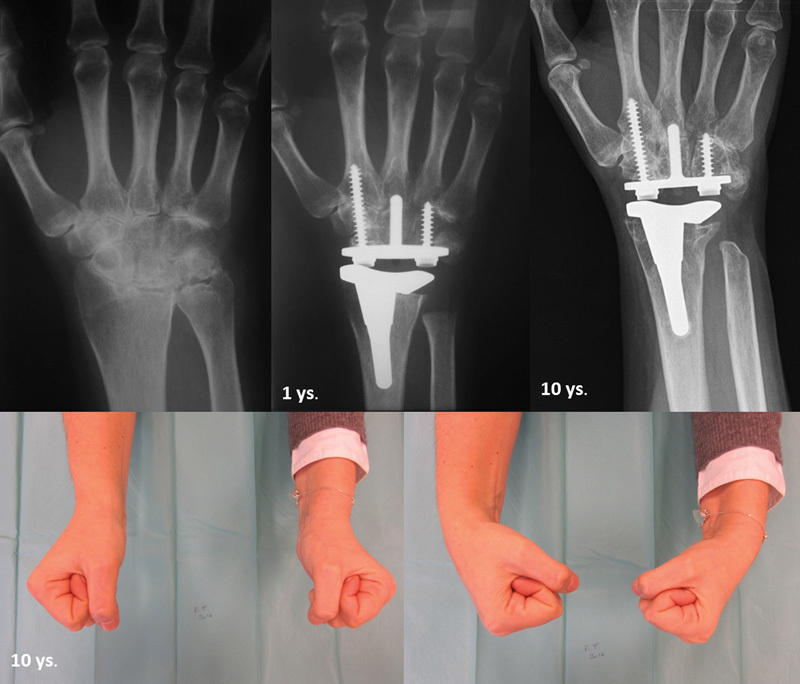
Radiological and clinical results 10 years after surgery with no pain and functional range of motion (case 9).
Postoperative self-assessment showed a value of QuickDASH 49 and PRWHE 41.7 in activities of daily living ( Table 2 ). All patients returned to their manual tasks and work with satisfaction after 3 months. In two cases, with adequate splinting, they could also participate in selected sports (skiing, cycling).
Table 2. Results.
| Patients | Preoperative VAS | Postoperative VAS | ROM (flexion/extension) | ROM (radial/ulnar deviation) | Jamar (kg) | QuickDASH | PRWHE | |
|---|---|---|---|---|---|---|---|---|
| 2 | R.M. | 10 | 0 | 50 | 20 | 10 | 36.3 | 38.5 |
| 3 | M.L. | 9 | 0 | 69 | 25 | 7.5 | 43.1 | 26.5 |
| 6 | B.P. | 9 | 1 | 74 | 42 | 2.5 | 63.6 | 64.5 |
| 8 | C.A. | 9 | 0 | 38 | 15 | 1 | 84.0 | 78 |
| 9 | M.F. | 10 | 0 | 115 | 25 | 21 | 29.5 | 24 |
| 10 | B.F. | 8 | 1 | 100 | 40 | 30 | 22.7 | 23.5 |
| 11 | G.A. | 7 | 0 | 70 | 35 | 0 | 27.2 | 23.5 |
| 12 | S.W. | 10 | 0 | 110 | 35 | 13 | 43.1 | 19 |
| 13 | R.A. | 8 | 3 | 65 | 15 | 8.5 | 79.5 | 62 |
| 15 | G.C. | 9 | 3 | 65 | 30 | 10 | 47.7 | 25 |
| 16 | G.V. | 9 | 0 | 95 | 30 | 22 | 20.4 | 12.5 |
| 17 | R.A. | 9 | 2 | 70 | 35 | 9 | 70.4 | 57 |
| 18 | B.E. | 8 | 0 | 55 | 30 | 10 | 63.6 | 44.5 |
| 19 | M.F.N. | 10 | 3 | 80 | 35 | 13.5 | 65.9 | 70.5 |
| 21 | S.D. | 10 | 1 | 73 | 0 | 0.5 | 59.0 | 56 |
| 22 | C.R. | 9 | 0 | 50 | 2 | 2.5 | 59.0 | 47 |
| 23 | S.M. | 9 | 0 | 50 | 10 | 8 | 18.1 | 38.5 |
Abbreviations: ROM, range of motion; VAS, visual analogue scale; PRWHE, patient rate wrist/hand evaluation.
We recorded several complications; one marginal skin necrosis of the wound in the perioperative period, healed by advanced wound care, in six cases (26%) was necessary revision surgery.
Radiological Evaluation
We recorded no radiographic changes over time in nine cases (Type A), and signs of remodeling in eight cases (Type B) due to stress shielding in the radial styloid (case 3), osteolysis around screws and the central stem (cases 15 and 23), and bony resorption around the radial baseplate (case 19) ( Fig. 6 ). Two cases, cases 13 and 15, showed a partial migration of the implant; three cases, cases 6, 10, and 11, showed signs of subsidence and loosening. Among these eight patients, five are Type B.1 (cases 3, 13, 15, 19, and 23) and three are B.2 (cases 6, 10, and 11). All of these cases were not yet revised and asymptomatic.
Fig. 6.
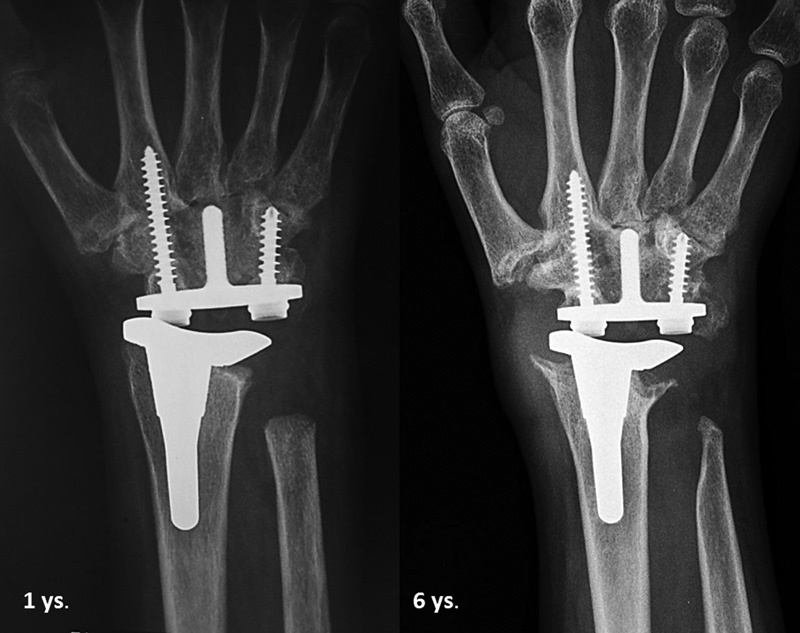
Radiological evaluation at 6-year follow-up showed signs of change in bone density around the radial baseplate (case 19).
Revision—Failures (Aseptic Loosening)
Of the 23 implants, 6 (Type C) (26%) were revised. A second surgery was mandatory in case of swelling, pain, deformity, progressive reduction of ROM, and unstable joint with impairment of the function associated with radiographic loosening or with a malalignment of the implant. In all cases of secondary surgery, we also performed histological examination of the periprosthetic tissues to determine the presence of metal particles or any polyethylene debris. Two cases (4 and 6) were revised in the carpal component: one for improper fusion of the carpal bones and one for a massive reactivation of rheumatic disease no longer responsive to drugs ( Figs. 7 and 8 ). Total failure of the implant which required conversion surgery was performed in four cases (1, 7, 14, and 20) out of six (17%) ( Fig. 9 ). Procedures and implant revisions are summarized in Table 3 .
Fig. 7.
Case 5 (L.R.G.) showed a periprosthetic osteolysis at the radial screw, an improper fusion of the carpal bones and clinically characterized by pain without reduction of the range of motion at 2 years after surgery. In this case, a revision has been performed a revision with replacement of the polyethylene implant and the distal anchoring screws, as well as a fusion between the bones of the carpus and between carpal–metacarpal joints; the prosthesis is implanted to date, and clinically silent.
Fig. 8.
Case 4 (G.M.F.) after 7 years from surgery, the patient developed a massive reactivation of rheumatic disease no longer responsive to drugs, which determined a progressive failure of the carpal component with proximal migration of the screws and broke the carpal stem accompanied by pain, swelling, and functional impairment; intraoperative an extended metallosis was found but the polyethylene was in good condition with no coarse signs of wear. The carpal component was replaced and now the prosthesis shows no mobilization and is clinically silent.
Fig. 9.
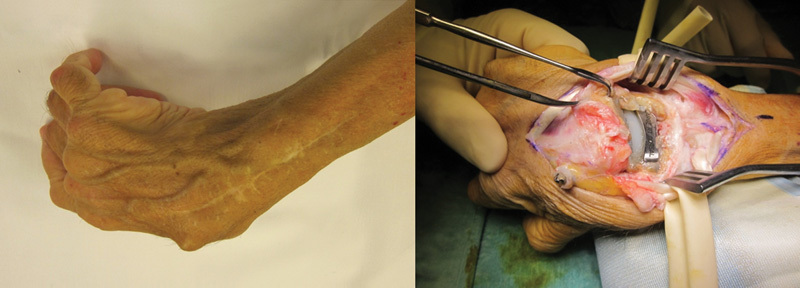
Case 20 was characterized intraoperative by loss of joint congruity and leakage of the radial screw from two midcarpal.
Table 3. Second surgery.
| Case | Patients | Implant mode of failure | Second surgery | ||
|---|---|---|---|---|---|
| Revision surgery | Conversion surgery | Intraoperative view | |||
| 1 | P.S. | Aseptic loosening (ongoing disease) | Swanson silicone spacer | Breakage of carpal implant, metallosis, and polydebris | |
| 4 | G.M.F. | Aseptic loosening (ongoing disease) | Revision surgery (polyethylene, carpal plate, and screws) | Breakage of carpal implant, metallosis | |
| 5 | L.R.G. | Failure of fusion (ongoing disease) | Revision surgery (polyethylene, two MC screws) | Metallosis | |
| 7 | F.A. | Imbalance | Swanson silicone spacer | ||
| 14 | M.M. | Malalignment (ongoing disease) | Swanson silicone spacer | Leakage of the radial screw from two MC, metallosis | |
| 20 | C.P. | Malalignment (ongoing disease) | Total wrist fusion | Leakage of the radial screw from two MC, metallosis | |
Abbreviation: MC, midcarpal.
The implant survival curve was estimated using the Kaplan–Meier's method; follow-up regarding implant survival was measured as the time of primary wrist replacement until revision surgery for any reason (survival criterion). Regarding U2 implants in RA patients of our cohort, they show a smooth and progressive curve over time with a steady failure rate. The U2 survivorship would be of 64% at 12 years ( Fig. 10 ).
Fig. 10.
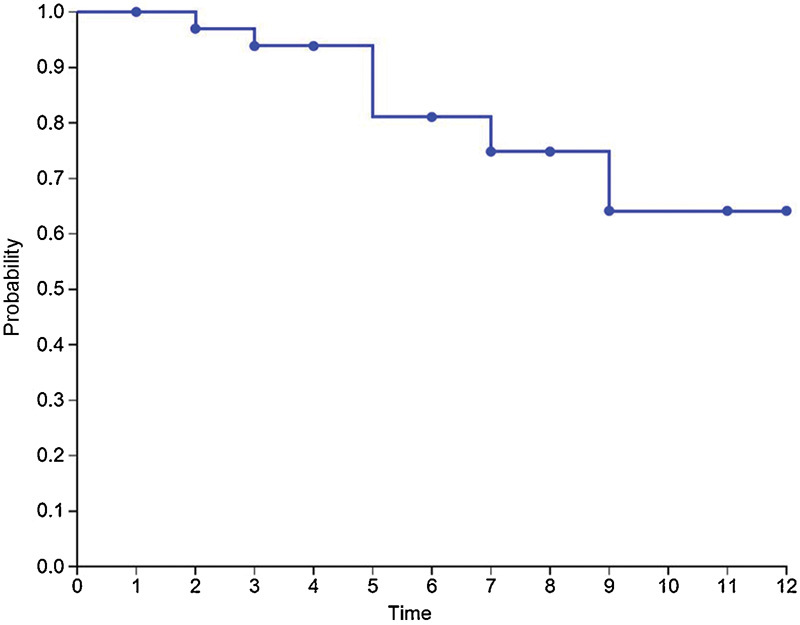
The Kaplan–Meier's survival analysis estimated a survival of implants at 12 years (64%).
Discussion
We reviewed 23 TWA, who underwent to U2 total wrist replacement, in rheumatoid patients. In our series, at mean follow-up of 82.3 months (2–12 years), the survival rate was 74%, and six TWA were reoperated. The Kaplan–Meier's survival analysis estimated a survival of all implants at 12 years (64%). In our series of RA patients, the pathogenetic mechanisms that led to revision of the implant were mainly related to a progressive evolution of the disease, despite modern drugs, and failure of carpal bones arthrodesis that compromise the stability of the prosthesis and its regular function (normal wrist kinematics) with a secondary mechanical wear of polyethylene.
The parameters assessed in our last follow-up in 2016 are as follow: functional scores improved and were maintained over the mid- to long term; however, QUICK DASH and PRWHE scores were unreliable in rheumatoid patients compared with a posttraumatic subjects because the rheumatoid patient experiences disease involvement not only in the wrist but also in fingers and the proximal districts, such as elbow and shoulder, and daily activities are affected by the general condition of the patient. 19 The cooperation of the patient in the postoperative rehabilitation program directed by the hand therapist was a determinant for the quality of the final results.
The main potential advantage of TWA over total wrist fusion is the preservation of movement. In our series, 10 patients had contralateral arthrodesis, including 5 total wrist fusion and 5 radioscapholunate fusions, and all preferred the side with TWA as reported by several authors; recent studies of patients who have performed wrist arthrodesis show that they have difficulty performing everyday activities, such as writing, brushing hair, and sitting. 17 19 20 21 22
In RA patients, the surgeon has to face several challenges due to muscle imbalance, reduction of bone stock, messy and subverted anatomy of the rheumatoid wrist, ligamentous laxity, potential worsening of disease, and a potential instability of the joint at risk for prostheses components misalignment. With the current generation of implants, such as U2, it is critical for the RA wrist balancing muscles to achieve stability and alignment of the prosthetic components. Muscle imbalance, included between 16 and 32% of RA population, is due to the inability of the patient to voluntarily hold the wrist in a neutral position (dorsiflexion 10–15 degrees, slight ulnar deviation). 19 20 21 22 23 This imbalance may be evident both in flexion–extension and radioulnar deviation and can be exacerbated by the involvement in the process of tendons degeneration, made inefficient by fibrotic substitution processes or by their own failure. The most common related condition is a radial displacement of the rotation center that has led to development in the design of the prosthesis, but on the contrary requires adequate knowledge by surgeons of force vectors determinants in rheumatoid deformities where the stronger deformation element is the flexor carpi ulnaris tendon. Therefore, we cannot count solely on the intrinsic stability of the prosthesis, and it is always necessary to accurately handle soft tissues and fix the causes of imbalance. The success of the U2 implant in terms of fixation is well established, and once initial stability is achieved, this usually leads to long-term biological fixation.
Only short- to mid-term follow-up results for U2 wrist arthroplasty have been reported in a small series of patients. Ferreres et al 17 in 2011 reviewed 21 TWA U2, 14 patients with RA and 2 with Kienböck's disease, 1 had degenerative arthrosis, and 1 had chondrocalcinosis. After a mean follow-up of 5.5 years, two patients were found with osteolysis around screws and distal components with subsidence on the ulnar side of the carpus. Morapudi et al 24 in 2012 reported 21 TWA using the U2, 19 RA and 2 posttraumatic. After a mean follow-up of 3.1, only two patients underwent to a second surgical procedure. The study revealed no radiological evidence of loosening. Cooney et al 25 in 2012 published a comparative retrospective study on 30 Biaxial, and 16 U2 and Re-Motion TWA. Ten were posttraumatic arthritis and 36 had RA. After a 6-year follow-up, nine implant failures were noted for distal component implant loosening and wrist instability; only one in the U2 series. Sagerfors et al 26 in 2012 in a prospective cohort study evaluated 219 TWA, 185 RA and 34 osteoarthrosis, with a follow-up of 7 years with four types of prosthesis: Biax, Re-Motion, U2 (with 8-year follow-up and 12 RA patients), and Maestro. Nineteen TWA underwent revision, 16 for radiographic loosening combined with pain and 3 for deep infection. Loosening 5 years postoperatively was present in 36% of the U2 implants. Chevrollier et al 27 in 2016 reported in a retrospective study with 17 TWA, U2 and Re-Motion, with a follow-up of 5.2 years. Three were converted to arthrodesis and observed implant loosening in eight patients. The author confirms the discordance observed between patients' subjective satisfaction and mediocre clinical and radiological results over the medium term. Yeoh and Tourret 11 in 2015 published a systematic review of the past 5 years in the literature, and found U2 the best for survival rate compared with others prostheses, but the analysis was based only on Morapudi and Ferreres series. The authors noted a reduction of risk of dislocation in U2 compared with the previous model.
There were limitations in the present study. It was a retrospective cohort study. We also had lack of preoperative data in a relatively small numbers of the cases that were included. Lack of homogeneity age at surgery and follow-up was also noted.
The characteristics of implants currently used allow us to no longer consider wrist replacement a salvage procedure, but rather a primary indication of reconstructive surgery for RA patients, with reliable results intended to last; U2 implants have definitely entered in our armamentarium. Careful patient selection is essential. Naturally, this surgery has some limitations, which are attributable to a small group of indications for pathology and degree of evolution of the disease, and the need for considerable technical pre- and intraoperative experience, as well as other limitations related to mechanical failures due to the technical characteristics of the implant.
Footnotes
Conflict of Interest None.
References
- 1.Swanson A B. Flexible implant arthroplasty for arthritic disabilities of the radiocarpal joint. A silicone rubber intramedullary stemmed flexible hinge implant for the wrist joint. Orthop Clin North Am. 1973;4(02):383–394. [PubMed] [Google Scholar]
- 2.Brase D W, Millender L H. Failure of silicone rubber wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am. 1986;11(02):175–183. doi: 10.1016/s0363-5023(86)80047-8. [DOI] [PubMed] [Google Scholar]
- 3.Jolly S L, Ferlic D C, Clayton M L, Dennis D A, Stringer E A. Swanson silicone arthroplasty of the wrist in rheumatoid arthritis: a long-term follow-up. J Hand Surg Am. 1992;17(01):142–149. doi: 10.1016/0363-5023(92)90130-h. [DOI] [PubMed] [Google Scholar]
- 4.Stanley J K, Tolat A R. Long-term results of Swanson silastic arthroplasty in the rheumatoid wrist. J Hand Surg Am. 1993;18B:381–388. doi: 10.1016/0266-7681(93)90069-r. [DOI] [PubMed] [Google Scholar]
- 5.Meuli H C. Meuli total wrist arthroplasty. Clin Orthop Relat Res. 1984;(187):107–111. [PubMed] [Google Scholar]
- 6.Volz R G. The development of a total wrist arthroplasty. Clin Orthop Relat Res. 1976;(116):209–214. [PubMed] [Google Scholar]
- 7.Cobb T K, Beckenbaugh R D. Biaxial total-wrist arthroplasty. J Hand Surg Am. 1996;21(06):1011–1021. doi: 10.1016/S0363-5023(96)80309-1. [DOI] [PubMed] [Google Scholar]
- 8.Menon J. Universal total wrist implant: experience with a carpal component fixed with three screws. J Arthroplasty. 1998;13(05):515–523. doi: 10.1016/s0883-5403(98)90050-x. [DOI] [PubMed] [Google Scholar]
- 9.Pfanner S, Ceruso M. Roma: Verduci; 2007. Artrite reumatoide: artrodesi, protesi articolari; pp. 1199–1224. [Google Scholar]
- 10.Divelbiss B J, Sollerman C, Adams B D. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am. 2002;27(02):195–204. doi: 10.1053/jhsu.2002.31728. [DOI] [PubMed] [Google Scholar]
- 11.Yeoh D, Tourret L. Total wrist arthroplasty: a systematic review of the evidence from the last 5 years. J Hand Surg Eur Vol. 2015;40(05):458–468. doi: 10.1177/1753193414539796. [DOI] [PubMed] [Google Scholar]
- 12.Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977;18(04):481–491. doi: 10.1177/028418517701800415. [DOI] [PubMed] [Google Scholar]
- 13.Flury M P, Herren D B, Simmen B R. Rheumatoid arthritis of the wrist. Classification related to the natural course. Clin Orthop Relat Res. 1999;(366):72–77. [PubMed] [Google Scholar]
- 14.Menon J. Universal Total Wrist Implant: experience with a carpal component fixed with three screws. J Arthroplasty. 1998;13(05):515–523. doi: 10.1016/s0883-5403(98)90050-x. [DOI] [PubMed] [Google Scholar]
- 15.Adams B D. Total wrist arthroplasty. Tech Hand Up Extrem Surg. 2004;8(03):130–137. doi: 10.1097/01.bth.0000131199.39073.2a. [DOI] [PubMed] [Google Scholar]
- 16.Bienfait M. Roma: Marrapese; 1995. La fascia. Anatomia, topografia, fisiologia, patologia. Il “Pompage”. Trattamento della fascia. [Google Scholar]
- 17.Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty: midterm follow-up study. J Hand Surg Am. 2011;36(06):967–973. doi: 10.1016/j.jhsa.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 18.Sagerfors M, Gupta A, Brus O, Pettersson K. Total wrist arthroplasty: a single-center study of 219 cases with 5-year follow-up. J Hand Surg Am. 2015;40(12):2380–2387. doi: 10.1016/j.jhsa.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Murphy D M, Khoury J G, Imbriglia J E, Adams B D. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg Am. 2003;28(04):570–576. doi: 10.1016/s0363-5023(03)00182-5. [DOI] [PubMed] [Google Scholar]
- 20.Vicar A J, Burton R I. Surgical management of the rheumatoid wrist--fusion or arthroplasty. J Hand Surg Am. 1986;11(06):790–797. doi: 10.1016/s0363-5023(86)80224-6. [DOI] [PubMed] [Google Scholar]
- 21.Takwale V J, Nuttall D, Trail I A, Stanley J K. Biaxial total wrist replacement in patients with rheumatoid arthritis. Clinical review, survivorship and radiological analysis. J Bone Joint Surg Br. 2002;84(05):692–699. doi: 10.1302/0301-620x.84b5.12276. [DOI] [PubMed] [Google Scholar]
- 22.Nydick J A, Greenberg S M, Stone J D, Williams B, Polikandriotis J A, Hess A V. Clinical outcomes of total wrist arthroplasty. J Hand Surg Am. 2012;37(08):1580–1584. doi: 10.1016/j.jhsa.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Adams B D. Complications of wrist arthroplasty. Hand Clin. 2010;26(02):213–220. doi: 10.1016/j.hcl.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Morapudi S P, Marlow W J, Withers D, Ralte P, Gabr A, Waseem M. Total wrist arthroplasty using the Universal 2 prosthesis. J Orthop Surg (Hong Kong) 2012;20(03):365–368. doi: 10.1177/230949901202000321. [DOI] [PubMed] [Google Scholar]
- 25.Cooney W, Manuel J, Froelich J, Rizzo M. Total wrist replacement: a retrospective comparative study. J Wrist Surg. 2012;1(02):165–172. doi: 10.1055/s-0032-1326728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sagerfors M, Gupta A, Brus O, Rizzo M, Pettersson K. Patient related functional outcome after total wrist arthroplasty: a single center study of 206 cases. Hand Surg. 2015;20(01):81–87. doi: 10.1142/S0218810415500112. [DOI] [PubMed] [Google Scholar]
- 27.Chevrollier J, Strugarek-Lecoanet C, Dap F, Dautel G. Results of a unicentric series of 15 wrist prosthesis implantations at a 5.2. year follow-up. Acta Orthop Belg. 2016;82(01):31–42. [PubMed] [Google Scholar]


