Abstract
Patients with interstitial lung disease (ILD) may have features of connective tissue disease (CTD), but lack findings diagnostic of a specific CTD. A recent European Respiratory Society/American Thoracic Society research statement proposed criteria for patients with interstitial pneumonia with autoimmune features (IPAF).
We applied IPAF criteria to patients with idiopathic interstitial pneumonia and undifferentiated CTD-ILD (UCTD). We then characterised the clinical, serological and morphological features of the IPAF cohort, compared outcomes to other ILD cohorts and validated individual IPAF domains using survival as an endpoint.
Of 422 patients, 144 met IPAF criteria. Mean age was 63.2 years with a slight female predominance. IPAF cohort survival was marginally better than patients with idiopathic pulmonary fibrosis, but worse than CTD-ILD. A non-usual interstitial pneumonia pattern was associated with improved survival, as was presence of the clinical domain. A modified IPAF cohort of those meeting the clinical domain and a radiographic or histological feature within the morphological domain displayed survival similar to those with CTD-ILD.
IPAF is common among patients with idiopathic interstitial pneumonia and UCTD. Specific IPAF features can identify subgroups with differential survival. Further research is needed to replicate these findings and determine whether patients meeting IPAF criteria benefit from immunosuppressive therapy.
Introduction
The interstitial lung diseases (ILDs) are a heterogeneous group of diffuse parenchymal lung disorders characterised by similar physiological and radiographic findings that may result in pulmonary fibrosis. The clinical course and therapeutic response vary substantially depending on ILD aetiology. Patients with connective tissue disease (CTD) associated ILD (CTD-ILD) are thought to have a more favourable clinical course when compared to those with idiopathic pulmonary fibrosis (IPF) [1, 2]. A significant subset of patients with ILD demonstrates clinical or serological features suggestive of a CTD, but fails to meet established CTD diagnostic criteria. These patients have been labelled undifferentiated CTD-associated ILD (UCTD-ILD), lung-dominant CTD and autoimmune-featured ILD by groups around the world using overlapping, but subtly different criteria [3–6].
Recognition that our understanding of this clinical entity might benefit from an improved classification system with uniform diagnostic criteria led to the formation of the European Respiratory Society (ERS)/American Thoracic Society (ATS) “Task Force on Undifferentiated Forms of Connective Tissue Disease-associated ILD.” This task force recently published a joint research statement proposing criteria for interstitial pneumonia with autoimmune features (IPAF)[7]. This new classification system incorporates not only clinical and serological manifestations of CTD, but also morphological features suggestive of a CTD encountered on high-resolution computed tomography (HRCT), surgical lung biopsy (SLB) and pulmonary function testing (PFTs).
In this study, we retrospectively apply IPAF criteria to patients with UCTD-ILD based on narrow criteria proposed by Corte et al. [3] and those with idiopathic interstitial pneumonia (IIP), including those previously diagnosed with IPF, biopsy-proven idiopathic non-specific interstitial pneumonia (NSIP), biopsy-proven cryptogenic organising pneumonia (COP) and unclassifiable IIP. We then characterised the clinical features of this IPAF cohort and compared outcomes to a cohort of patients with IPF and CTD-ILD. Finally, we attempted to validate individual IPAF criteria by identifying domains, and common features within domains, predictive of differential survival risk using longitudinal follow-up data.
Methods
Study design
This investigation was conducted at the University of Chicago (Chicago, IL, USA) and was approved by University’s Institutional Review Board (IRB protocol #14163-A). The University of Chicago ILD registry was used to identify patients followed in the ILD clinic from October 2006 to December 2014. Patients with IIP, including IPF, unclassifiable IIP, biopsy-proven idiopathic NSIP and biopsy-proven COP based on ERS/ATS criteria [8, 9] were identified. We also identified patients with a provisional diagnosis of UCTD-ILD based on previously proposed narrow criteria [3]. ILD diagnosis at our institution is performed in a rigorous, multidisciplinary fashion in conjunction with dedicated chest radiologists and thoracic pathologists. The electronic medical record was reviewed retrospectively to extract pertinent data. Vital status was determined using review of medical records, telephone communication and the social security death index. Follow-up time was censored on January 1, 2015. Patients were excluded if they had ILD from other causes, refused consent, or did not undergo the recommended tests needed for diagnosis, such as serology, HRCT or SLB.
The first ILD clinic visit was used to extract pertinent data, including: demographic information (age, race/ethnicity, sex); patient-reported medical/surgical history, including hypothyroidism, gastroesophageal reflux (GER), diabetes mellitus, coronary artery disease (CAD) and tobacco use; patient-reported medication use including thyroid replacement, proton pump inhibitor, histamine-2 blocker, systemic corticosteroids, azathioprine, mycophenolate mofetil, cyclophosphamide and tacrolimus therapy; physical examination findings that included body mass index, clubbing and crackles, laboratory studies that included antinuclear antibody (ANA) with immunofluorescence pattern, rheumatoid factors, cyclic citrullinated protein antibody, myositis-specific antibodies, anti-Ro/Anti-Sjögren’s-syndrome-related antigen A (SSA) antibody, anti-La/SSB antibody, anti-ribonucleoprotein (RNP) antibody, anti-Smith antibody and anti-Scl-70 antibody; and diagnostic studies including HRCT, SLB and PFTs, which included total lung capacity, forced vital capacity (FVC), and diffusion capacity of the lung for carbon monoxide (DLCO). Data from follow-up clinic visits were reviewed to ascertain the use of corticosteroid and immunosuppressive therapy and outcome data.
With regard to IPAF serological criteria, anti PM-Scl and anti-CADM (MDA-5) were not included in the routine ILD evaluation at our institution and could not be assessed. HRCTs and SLBs were re-reviewed blindly by two chest radiologists (S. Montner and J. Chung) and a pulmonary pathologist (A. Husain), who systematically applied IPAF criteria to available HRCTs and SLBs, respectively. NSIP pattern by HRCT was determined using previously suggested criteria [10]. In patients with usual interstitial pneumonia (UIP) on SLB, IPAF pathologic criteria could be met if such findings were concurrently present. When assessing multicompartment criteria within the morphologic domain, intrinsic airways disease was noted when forced expiratory volume in 1 s (FEV1)/FVC was <70, histopathologic bronchiolitis was present on SLB or when mosaic attenuation was seen on HRCT. Pulmonary vasculopathy was noted when FVC/DLCO ratio was >1.6 based on previously published data showing correlation between this metric and pulmonary vasculopathy [11, 12]. Because multicompartment criteria apply only when findings cannot otherwise be explained, intrinsic airways disease and pulmonary vasculopathy were only considered in nonsmokers, as these findings can be seen in concurrent chronic obstructive pulmonary disease.
Statistical analysis
Continuous variables are reported as means±SD and were compared using a two-tailed student’s t-test. Categorical variables were reported as counts and percentages and compared using the Chi-squared test or Fisher’s exact test, as appropriate. Survival was assessed using unadjusted log-rank testing along with univariate and multivariable Cox proportional-hazards regression. Survival curves are plotted using the Kaplan–Meier survival estimator. DLCO was imputed using lowest quartile mean (27.3%) in patients unable to perform this manoeuver. A possible UIP pattern on HRCT was recorded as UIP based on previous data showing a strong correlation between possible UIP on HRCT and histopathologic UIP [13]. SLB pattern was considered the final radiographic/histopathologic pattern when discordance occurred between the two diagnostic modalities. Survival time was defined as time from diagnostic test (SLB or HRCT) to death, transplant, loss to follow-up or end of study period. Survival time was censored on January 1, 2015 or at the time a patient underwent lung transplant or was lost to follow-up. All statistical analyses were performed using Stata (2015 Release 14; StataCorp, College Station, TX, USA).
Results
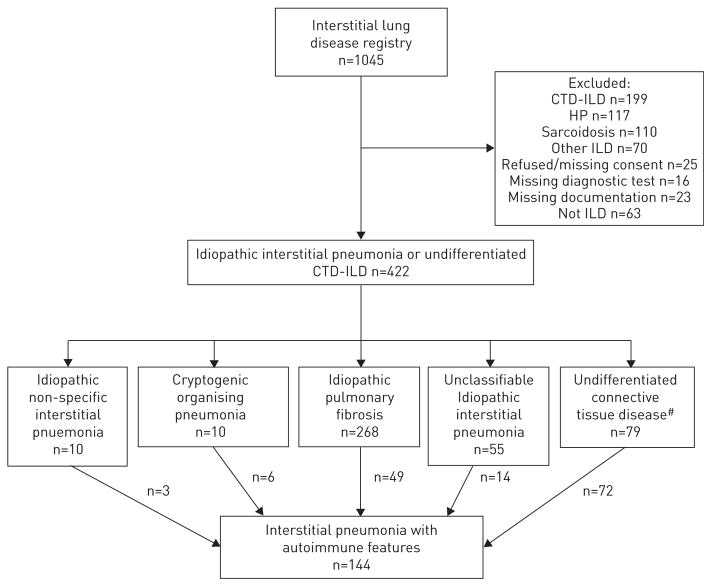
Of 1045 patients screened, 422 patients with IIP or UCTD-ILD were identified; 10 with biopsy-proven idiopathic NSIP, 10 with biopsy-proven COP, 268 with IPF, 55 with unclassifiable IIP, and 79 with UCTD-ILD (figure 1). Of those, three with NSIP, six with COP, 49 with IPF, 14 with unclassifiable IIP and 72 with UCTD-ILD met the IPAF criteria (n=144). Among those meeting IPAF criteria (table 1), the mean age was 63.2 years and 52.1% were females. Non-Hispanic white patients composed 71% of the cohort, followed by African American patients 17%, Hispanic patients 7% and Asian patients (5%). Common comorbid conditions included GER (52.8%), hypothyroidism (19.4%), diabetes mellitus (11.8%) and CAD (22.2%). The majority of the IPAF cohort had previous tobacco use (54.9%) and a significant minority was taking systemic corticosteroids (32.2%) at the time of evaluation. Nearly 90% of the cohort was found to have crackles on pulmonary auscultation. On HRCT, 54.6% of patients demonstrated a UIP pattern and of the 83 patients biopsied, 61 (73.5%) patients demonstrated a histological UIP pattern.
FIGURE 1.
Consort diagram. CTD: connective tissue disease; ILD: interstitial lung disease; HP: hypersensitivity pneumonitis; IIP: idiopathic interstitial pneumonia. #: based on narrow criteria as proposed by Corte et al. [3].
TABLE 1.
Interstitial pneumonia with autoimmune features cohort baseline demographic and clinical characteristics#
| Age | 63.2±11 |
| Sex female | 75 (52.1) |
| Race/ethnicity | |
| White | 102 (70.8) |
| African-American | 25 (17.4) |
| Hispanic | 10 (6.9) |
| Asian | 7 (4.9) |
| Gastroesophageal reflux | 76 (52.8) |
| Hypothyroidism | 28 (19.4) |
| Diabetes mellitus | 17 (11.8) |
| Coronary artery disease | 32 (22.2) |
| Ever smoker | 79 (54.9) |
| Systemic corticosteroid Use | 46 (32.2) |
| Gastroesophageal reflux therapy | 76 (53.2) |
| Body mass index | 30±6.6 |
| Crackles¶ | 125 (89.3) |
| Clubbing+ | 21 (18.9) |
| Usual interstitial pneumonia by high-resolution computed tomography§ | 77 (54.6) |
| Usual interstitial pneumonia by surgical lung biopsyƒ | 61 (73.5) |
| Forced vital capacity in 1 s % predicted | 61.9±18.3 |
| Diffusion capacity of the lung for carbon monoxide % predicted | 45.3±20.6 |
Data are presented as mean±SD or n (%).
N=144, unless otherwise stated;
N=140;
N=111;
N=141;
N=83.
Overall, 21 (14.6%) patients met IPAF criteria through a combination of clinical and serological domains, 12 (8.3%) by clinical and morphological domains, 73 (50.7%) by serological and morphological domains and 38 (26.4%) by all three domains (table 2). When stratifying IPAF domain combinations by initial diagnosis (table 2), substantial clustering of domain combinations was observed. Patients initially characterised as COP/NSIP and IPF met IPAF criteria through a combination of serologic and morphological domains in over 75% of cases. Those previously characterised as UCTD-ILD and unclassifiable IIP were more evenly distributed, though patients initially characterised as UCTD-ILD met IPAF criteria by fulfilling all three domains in nearly 50% of cases.
TABLE 2.
Interstitial pneumonia with autoimmune-features (IPAF) domains met by initial diagnosis
| Domains met | IPAF cohort | Initial diagnosis | |||
|---|---|---|---|---|---|
|
| |||||
| NSIP/COP | IPF | UCTD-ILD | Unclassifiable | ||
| Subjects | 144 | 9 | 49 | 72 | 14 |
| Clinical and serological | 21 (14.6) | 0 (0) | 3 (6.1) | 17 (23.6) | 1 (7.1) |
| Clinical and morphological | 12 (8.3) | 2 (22.2) | 0 (0) | 6 (8.3) | 4 (28.6) |
| Serological and morphological | 73 (50.7) | 7 (77.8) | 43 (87.8) | 16 (22.2) | 7 (50) |
| All three domains | 38 (26.4) | 0 (0) | 3 (6.1) | 33 (45.8) | 2 (14.3) |
Data are presented as n or n (%). NSIP: nonspecific interstitial pneumonia; COP: crytogenic organising pneumonia; IPF: idiopathic pulmonary fibrosis; UCTD: undifferentiated connective tissue disease; ILD: interstitial lung disease.
A breakdown of features within each IPAF domain is shown in table 3. The most common clinical findings were Raynaud’s phenomenon (27.8%), inflammatory arthritis/morning stiffness lasting >60 min (17.4%) and mechanics hands (10.4%). An ANA ≥ 1:320 (or nucleolar or centromere pattern of any titre) was the most common serological finding (77.6%), followed by SSA (16.6%) and rheumatoid factor ≥x2 upper limit of normal (13%). Within the morphological domain, an NSIP pattern by HRCT was found in 31.9% of patients while histopathological NSIP and OP patterns were found in 22.9% and 16.9% of patients biopsied, respectively. Intrinsic airways disease was the most common multicompartment finding (22.2%), followed by pleural disease (12.5%) and pulmonary vasculopathy (18.8%).
TABLE 3.
Findings of interstitial pneumonia with autoimmune features by domain#
| Clinical domain | 71 (49.3) |
| Mechanics hands | 15 (10.4) |
| Distal digital tip ulceration | 3 (2.1) |
| Inflammatory arthritis/polyarticular morning joint stiffness ≥60 min | 25 (17.4) |
| Palmar telangiectasia | 0 (0) |
| Raynaud’s phenomenon | 40 (27.8) |
| Unexplained digital oedema | 5 (3.5) |
| Gottron’s sign | 7 (4.9) |
| Serological domain | 132 (91.7) |
| Antinuclear antibody¶ ≥1:320+ | 111 (77.6) |
| Rheumatoid factor§ ≥x2 upper limit normal | 18 (13) |
| Anti-cyclic citrullinated peptideƒ | 6 (4.7) |
| Anti-double stranded DNA## | 7 (7.2) |
| Anti-Ro Anti (SSA)¶¶ | 23 (16.6) |
| Anti-La Anti (SSB)¶¶ | 4 (2.9) |
| Anti-ribonucleoprotein | 7 (4.9) |
| Anti-Smith++ | 2 (1.5) |
| Anti-topoisomerase (Scl-70)§§ | 4 (3) |
| Anti-tRNA synthetase§§ | 1 (0.7) |
| Morphological domain | 123 (85.4) |
| High-resolution computed tomographyƒƒ | |
| Nonspecific interstitial pneumonia | 45 (31.9) |
| Organising pneumonia | 5 (3.5) |
| Nonspecific interstitial pneumonia with organising pneumonia overlap | 11 (7.8) |
| Histopathologic pattern### | |
| Nonspecific interstitial pneumonia | 19 (22.9) |
| Organising pneumonia | 14 (16.9) |
| Nonspecific interstitial pneumonia with organising pneumonia overlap | 3 (3.6) |
| Interstitial lymphoid aggregates with germinal centres | 11 (13.3) |
| Diffuse lymphoplasmacytic infiltration | 8 (9.6) |
| Multicompartment involvement¶¶¶ | |
| Pleural effusion or thickening (high-resolution computed tomography) or pleuritis (surgical lung biopsy) | 18 (12.5) |
| Pericardial effusion or thickening | 2 (1.4) |
| Intrinsic airways disease | 32 (22.2) |
| Pulmonary vasculopathy | 27 (18.8) |
Data are presented as n (%).
N=144, unless otherwise stated;
N=143;
or <1:320 with nucleolar or centromere pattern;
N=138;
N=127;
N=97;
N=139;
N=132;
N=135;
N=141;
N=83;
not otherwise explained.
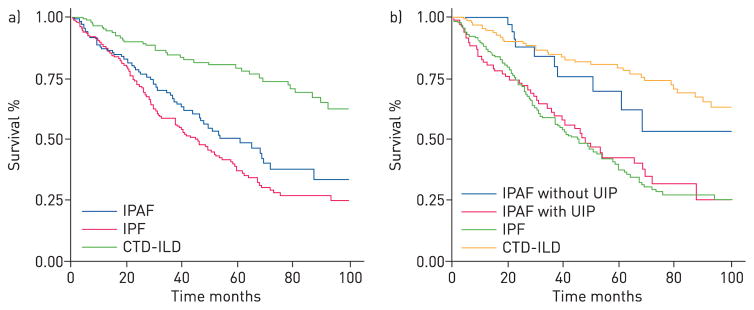
In outcome analysis, 57 (39.6%) of IPAF patients died during the follow-up period and 14 (10.8%) underwent lung transplantation. When comparing IPAF cohort survival to those with IPF and CTD-ILD (figure 2a), IPAF cohort survival was worse than CTD-ILD (p<0.001) and marginally better than IPF (p=0.07). After stratifying the IPAF cohort based on the presence of a UIP pattern by HRCT or SLB (figure 2b), those with a non-UIP pattern (n=46) demonstrated survival similar to those with CTD-ILD (p=0.45) and those with a UIP pattern (n=98) demonstrated survival similar to those with IPF (p=0.51).
FIGURE 2.
Kaplan–Meier survival curves of interstitial pneumonia with autoimmune features (IPAF), idiopathic pulmonary fibrosis (IPF) and connective tissue disease (CTD)-interstitial lung disease (ILD) cohorts. Overall a) IPAF cohort survival was significantly worse than the CTD-ILD cohort (p<0.001) and marginally better than the IPF cohort (p=0.07). After stratification of the IPAF cohort by the presence of a usual interstitial pneumonia pattern on high-resolution computed tomography and/or surgical lung biopsy b) IPAF patients without usual interstitial pneumonia (UIP) demonstrated survival similar to those with CTD-ILD (p=0.45), while those with UIP demonstrate survival similar to those with IPF (p=0.51).
In univariate Cox regression (table 4), predictors of increased mortality risk among those meeting IPAF criteria included each year of increased age from the mean (hazard ratio (HR) 1.06, 95% CI 1.03–1.08; p<0.001), prevalent hypothyroidism (HR 1.97, 95% CI 1.05–3.67; p=0.03) and a UIP pattern on HRCT and/or SLB (HR 2.4, 95% CI 1.21–4.76; p=0.01). Each percentage increase in DLCO from the mean was associated with decreased mortality risk (HR 0.97, 95% CI 0.96–0.99; p<0.001). Sex, smoking history, GER therapy, chronic systemic corticosteroid therapy, immunosuppressive therapy and FVC were not significant predictors of survival in univariate analysis. Only age and DLCO remained significant predictors of differential mortality risk after multivariable adjustment.
TABLE 4.
Variables predicting survival in patients with interstitial pneumonia with autoimmune features
| Characteristic | Unadjusted#
|
Adjusted#
|
||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Age | 1.06 (1.03–1.08) | <0.001 | 1.05 (1.02–1.08) | 0.001 |
| Male sex | 1.54 (0.91–2.60) | 0.11 | 1.65 (0.92–2.97) | 0.09 |
| Hypothyroidism | 1.97 (1.05–3.67) | 0.03 | 1.08 (0.52–2.22) | 0.84 |
| Ever smoker | 0.92 (0.54–1.54) | 0.74 | 1.11 (0.60–2.05) | 0.74 |
| GER therapy | 1.12 (0.66–1.88) | 0.67 | 1.38 (0.79–2.43) | 0.26 |
| Chronic systemic corticosteroid therapy | 0.82 (0.49–1.38) | 0.46 | 1.39 (0.73–2.63) | 0.32 |
| Immunosuppressive therapy¶ | 0.74 (0.47–1.17) | 0.2 | 0.7 (0.35–1.4) | 0.31 |
| UIP pattern+ | 2.4 (1.21–4.76) | 0.01 | 1.72 (0.83–3.56) | 0.14 |
| FVC % predicted | 0.99 (0.98–1.01) | 0.22 | 1 (0.97–1.02) | 0.76 |
| DLCO % predicted | 0.97 (0.96–0.99) | <0.001 | 0.97 (0.95–0.99) | 0.01 |
| Clinical domain | 0.56 (0.32–0.96) | 0.03 | ||
| Raynaud’s phenomenon | 0.57 (0.29–1.10) | 0.09 | ||
| Serologic domain | 1.89 (0.59–6.06) | 0.28 | ||
| ANA seropositivity | 0.91 (0.51–1.62) | 0.75 | ||
| Morphological domain | 1.31 (0.56–3.06) | 0.53 | ||
| HRCT features | 0.58 (0.34–1.0) | 0.05 | ||
| SLB features | 0.36 (0.11–1.18) | 0.09 | ||
| Multicompartment features | 2.01 (1.19–3.38) | 0.009 | ||
HR: hazard ratio; GER: gastroesophageal reflux; UIP: usual interstitial pneumonia; FVC: forced vital capacity; DLCO: diffusion capacity of the lung for carbon monoxide; ANA: antinuclear antibody; HRCT: high-resolution computed tomography; SLB: surgical lung biopsy.
N=143;
azathioprine n=41, mycophenolate mofetil n=19, tacrolimus n=4, and cyclophosphamide n=2;
based on HRCT or SLB, with SLB serving as final diagnosis when discordant.
To validate individual IPAF criteria using survival as an endpoint, domains and common features within domains were tested for survival association using univariate Cox regression (table 4). Presence of the clinical domain was associated with significantly decreased mortality risk (HR 0.56, 95% CI 0.32–0.96; p=0.03), while presence of the serological and morphological domains were associated with a nonsignificant increase in mortality risk. Presence of the most common feature within the clinical (Raynaud’s phenomenon) and serological (ANA sero-positivity) domains was not predictive of differential survival risk. When assessing features within the morphological domain, a marginally decreased mortality risk was observed with the presence of HRCT (HR 0.58, 95% CI 0.34–1.0; p=0.05) and SLB (HR 0.36, 95% CI 0.11–1.18; p=0.09) features, while a significantly increased mortality risk was observed with the presence of multicompartment features (HR 2.01, 95% CI 1.19–3.38; p=0.009).
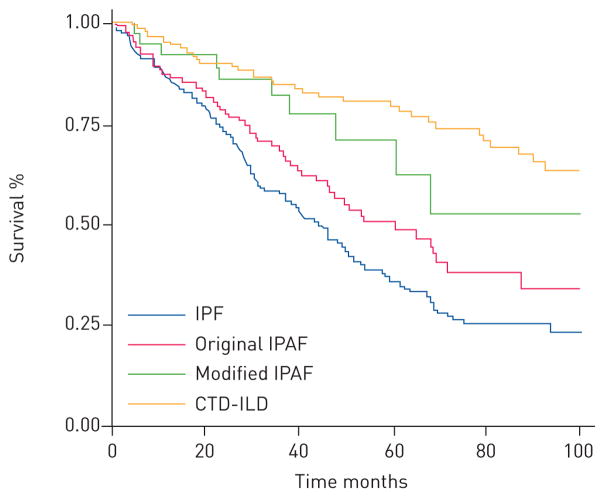
Based on these results, we constructed a new IPAF cohort (n=40) composed of individuals meeting the clinical domain and a HRCT or SLB feature within the morphological domain. Survival of this modified IPAF cohort was plotted against CTD-ILD and IPF cohorts, along with the original IPAF cohort (figure 3). Survival of the modified IPAF cohort was similar to that of CTD-ILD (p=0.26), marginally better than the original IPAF cohort (p=0.09) and significantly better than the IPF cohort (p=0.005).
FIGURE 3.
Kaplan–Meier survival curves of modified interstitial pneumonia with autoimmune features (IPAF), original IPAF, idiopathic pulmonary fibrosis (IPF) and connective tissue disease (CTD)-interstitial lung disease (ILD) cohorts. Modified IPAF cohort survival was similar to the CTD-ILD cohort (p=0.26), marginally better than the original IPAF cohort (p=0.09) and significantly better than the IPF cohort (p=0.005).
Discussion
In this study, we identified patients meeting IPAF criteria among a cohort of individuals previously diagnosed with an IIP or UCTD-ILD. Of these individuals, approximately one-third met IPAF criteria, including nearly 20% of patients with IPF, 25% of patients with unclassifiable IIP and the overwhelming majority of those previously characterised as UCTD-ILD. Our findings parallel those of Corte et al. [3], Ferri et al. [14], and Assayag et al. [15], all of whom showed that features of CTD are common among patients with IIP.
Patients meeting IPAF criteria tended to be older and have a higher percentage of ever smokers than those previously characterised as UCTD-ILD [4], likely related to the high percentage of patients (~30%) with IPF who met IPAF criteria. This may account for the higher proportion of UIP compared to NSIP in our cohort compared to the UCTD-ILD described by Kinder et al. [4] and Kim et al. [16] GER was also prevalent in our IPAF cohort, similar to that observed in study subjects with UCTD-ILD and autoimmune-featured (AIF) ILD, raising the question of whether this may contribute to disease pathogenesis [3, 5].
While the overall survival did not significantly differ between patients with IPAF and IPF, there was a suggestion of improved survival in the IPAF cohort. Despite this, survival was markedly worse than that observed in a CTD-ILD cohort. This appears to be driven in part by the underlying radiographic and/or histological pattern, as those meeting IPAF criteria with a UIP pattern displayed survival similar to an IPF cohort and those with a non-UIP pattern displayed survival similar to CTD-ILD cohort. This parallels the findings of Strand et al. [17] who showed similar survival between UCTD-UIP and IPF cohorts and a previous study at our centre in a UIP-predominant AIF-ILD cohort [5]. The significantly improved survival among IPAF patients with a non-UIP pattern is similar to that observed by Kim et al. [16] and Omote et al. [6], in subjects with UCTD-ILD and lung-dominant CTD, respectively. As such, one may expect IPAF cohorts with a larger percentage of patients with NSIP to demonstrate a more favourable survival patterns than observed in our cohort.
Predictors of mortality in the IPAF cohort included age and DLCO, suggesting that the sex, age, physiology (GAP) scoring system, validated in other forms of ILD, may also be an effective tool for prognostication in those meeting criteria for IPAF [18, 19]. We also showed hyperthyroidism to be associated with mortality in this IPAF cohort, similar to a previous study of patients with IPF at our centre [20], but this association was not maintained after multivariable adjustment. Similarly, a UIP pattern was associated with increased mortality risk in univariate analysis, but not after multivariable adjustment.
Finally, because we observed substantial clustering of IPAF domain combinations after stratification by initial diagnosis, we questioned whether IPAF criteria identified a homogenous phenotype. As no gold standard exists against which to validate IPAF criteria, we attempted to do so by identifying individual IPAF domains, and common features within domains, predictive of differential phenotypes using survival as an endpoint. We found that while presence of the clinical domain was a predictor of favourable outcome, presence of a multicompartment feature within the morphological domain was a strong predictor of poor outcome, perhaps as this allowed several patients with IPF to be classified as IPAF. When considering only those meeting the clinical domain and a HRCT or SLB feature within the morphological domain, also predictors of favourable outcome, we identified a phenotype with survival much closer to that of CTD-ILD. Interestingly, 17 (42.5%) out of 40 patients in this modified IPAF cohort had a UIP pattern by HRCT or SLB, indicating that some meeting IPAF criteria may have a favourable prognosis despite the presence of UIP.
There are a number of limitations to our investigation. First, this study was conducted retrospectively, limiting it to identification of association, rather than causation. However, data is obtained prospectively in all patients at our institution regardless of referring diagnosis. Second, treatment data was limited for patients in this investigation. We were, therefore, unable to robustly explore immunosuppressive response and were limited to categorically testing chronic immunosuppressive exposure at any point during the follow-up period. Next, our study population was drawn from a single tertiary referral centre with expertise in IPF. As such, patients with IPF may have been overrepresented, potentially biasing our results by enrichment of the IPAF cohort with patients known to have a poorer prognosis relative to other IIPs. The single-centre HRCT and SLB interpretation has the potential to introduce institutional bias as well. Last, formal histopathological re-review utilising IPAF criteria was not possible for some patients, as SLB slides sent from outside institutions were returned and not available for re-review. However, the initial histopathological review was performed by an experienced pulmonary pathologist with expertise in ILD.
Conclusion
This study is an important first step in evaluating the new IPAF classification criteria and is, to our knowledge, the first attempt at systematic validation of these criteria. This work identifies IPAF subgroups that demonstrate differential survival and suggests predictors of mortality that may inform future studies and prognostication models. It remains to be seen whether application of these IPAF criteria can identify patients who may benefit from immunosuppressive therapy, as is the case with CTD-ILD [21–24]. Further, as our cohort is UIP-predominant, we recognise that other cohorts with NSIP-predominant IPAF may have a more favourable natural history. Prospective investigation in larger, multicentre cohorts and through randomised clinical trials will be important in determining efficacy of therapy and outcomes for patients with IPAF.
Acknowledgments
Support statement: This study was funded by the US Department of Health and Human Services National Institutes of Health, grant number: T32 HL007605. Funding information for this article has been deposited with FundRef.
Footnotes
Conflict of interests: Disclosures can be found alongside the online version of this article at erj.ersjournals.com
References
- 1.de Lauretis A, Veeraraghavan S, Renzoni E. Review series: Aspects of interstitial lung disease: connective tissue disease-associated interstitial lung disease: how does it differ from IPF? How should the clinical approach differ? Chron Respir Dis. 2011;8:53–82. doi: 10.1177/1479972310393758. [DOI] [PubMed] [Google Scholar]
- 2.Fischer A, West SG, Swigris JJ, et al. Connective tissue disease-associated interstitial lung disease: a call for clarification. Chest. 2010;138:251–256. doi: 10.1378/chest.10-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corte TJ, Copley SJ, Desai SR, et al. Significance of connective tissue disease features in idiopathic interstitial pneumonia. Eur Respir J. 2012;39:661–668. doi: 10.1183/09031936.00174910. [DOI] [PubMed] [Google Scholar]
- 4.Kinder BW, Collard HR, Koth L, Jr, et al. Idiopathic nonspecific interstitial pneumonia: lung manifestation of undifferentiated connective tissue disease? Am J Respir Crit Care Med. 2007;176:691–697. doi: 10.1164/rccm.200702-220OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vij R, Noth I, Strek ME. Autoimmune-featured interstitial lung disease: a distinct entity. Chest. 2011;140:1292–1299. doi: 10.1378/chest.10-2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Omote N, Taniguchi H, Kondoh Y, et al. Lung-dominant connective tissue disease: clinical, radiologic and histologic features. Chest. 2015;148:1438–1446. doi: 10.1378/chest.14-3174. [DOI] [PubMed] [Google Scholar]
- 7.Fischer A, Antoniou KM, Brown KK, et al. An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J. 2015;46:976–987. doi: 10.1183/13993003.00150-2015. [DOI] [PubMed] [Google Scholar]
- 8.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch DA. Nonspecific interstitial pneumonia: evolving concepts. Radiology. 2001;221:583–584. doi: 10.1148/radiol.2213011510. [DOI] [PubMed] [Google Scholar]
- 11.Steen VD, Lucas M, Fertig N, et al. Pulmonary arterial hypertension and severe pulmonary fibrosis in systemic sclerosis patients with a nucleolar antibody. J Rheumatol. 2007;34:2230–2235. [PubMed] [Google Scholar]
- 12.Solomon JJ, Olson AL, Fischer A, et al. Scleroderma lung disease. Eur Respir Rev. 2013;22:6–19. doi: 10.1183/09059180.00005512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raghu G, Lynch D, Godwin JD, et al. Diagnosis of idiopathic pulmonary fibrosis with high-resolution CT in patients with little or no radiological evidence of honeycombing: secondary analysis of a randomised, controlled trial. Lancet Respir Med. 2014;2:277–284. doi: 10.1016/S2213-2600(14)70011-6. [DOI] [PubMed] [Google Scholar]
- 14.Ferri C, Manfredi A, Sebastiani M, et al. Interstitial pneumonia with autoimmune features and undifferentiated connective tissue disease: Our interdisciplinary rheumatology-pneumology experience, and review of the literature. Autoimmun Rev. 2016;15:61–70. doi: 10.1016/j.autrev.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Assayag D, Kim EJ, Elicker BM, et al. Survival in interstitial pneumonia with features of autoimmune disease: a comparison of proposed criteria. Respir Med. 2015;109:1326–1331. doi: 10.1016/j.rmed.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Kim HC, Ji W, Kim MY, et al. Interstitial pneumonia related to undifferentiated connective tissue disease: pathologic pattern and prognosis. Chest. 2015;147:165–172. doi: 10.1378/chest.14-0272. [DOI] [PubMed] [Google Scholar]
- 17.Strand MJ, Sprunger D, Cosgrove GP, et al. Pulmonary function and survival in idiopathic vs secondary usual interstitial pneumonia. Chest. 2014;146:775–785. doi: 10.1378/chest.13-2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156:684–691. doi: 10.7326/0003-4819-156-10-201205150-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ryerson CJ, Vittinghoff E, Ley B, et al. Predicting survival across chronic interstitial lung disease: the ILD-GAP model. Chest. 2014;145:723–728. doi: 10.1378/chest.13-1474. [DOI] [PubMed] [Google Scholar]
- 20.Oldham JM, Kumar D, Lee C, et al. Thyroid disease is prevalent and predicts survival in patients with idiopathic pulmonary fibrosis. Chest. 2015;148:692–700. doi: 10.1378/chest.14-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tashkin DP, Elashoff R, Clements PJ, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl j Med. 2006;354:2655–2666. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 22.Kim EJ, Collard HR, King TE., Jr Rheumatoid arthritis-associated interstitial lung disease: the relevance of histopathologic and radiographic pattern. Chest. 2009;136:1397–1405. doi: 10.1378/chest.09-0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mileti LM, Strek ME, Niewold TB, et al. Clinical characteristics of patients with anti-Jo-1 antibodies: a single center experience. J Clin Rheumatol. 2009;15:254–255. doi: 10.1097/RHU.0b013e3181b0e910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parambil JG, Myers JL, Lindell RM, et al. Interstitial lung disease in primary Sjogren syndrome. Chest. 2006;130:1489–1495. doi: 10.1378/chest.130.5.1489. [DOI] [PubMed] [Google Scholar]