Abstract
Use of non-ionizing radiation (NIR) for diagnostic purposes allows non-invasive assessment of the structure and function of the human body and is widely employed in medical care. ICNIRP has published previous statements about the protection of patients during medical magnetic resonance imaging (MRI), but diagnostic methods using other forms of NIR have not been considered. This statement reviews the range of diagnostic NIR devices currently used in clinical settings; documents the relevant regulations and policies covering patients and health care workers; reviews the evidence around potential health risks to patients and health care workers exposed to diagnostic NIR; and identifies situations of high NIR exposure from diagnostic devices in which patients or health care workers might not be adequately protected by current regulations. Diagnostic technologies were classified by the types of NIR that they employ. The aim was to describe the techniques in terms of general device categories which may encompass more specific devices or techniques with similar scientific principles. Relevant legally-binding regulations for protection of patients and workers and organizations responsible for those regulations were summarized. Review of the epidemiological evidence concerning health risks associated with exposure to diagnostic NIR highlighted a lack of data on potential risks to the fetus exposed to MRI during the first trimester, and on long-term health risks in workers exposed to MRI. Most of the relevant epidemiological evidence that is currently available relates to MRI or ultrasound. Exposure limits are needed for exposures from diagnostic technologies using optical radiation within the body. There is a lack of data regarding risk of congenital malformations following exposure to ultrasound in utero in the first trimester and also about the possible health effects of interactions between ultrasound and contrast media.
Key words: diagnostic radiology; imaging; medical radiation; radiation, non-ionizing
INTRODUCTION
Diagnostic imaging with non-ionizing radiation (NIR) allows non-invasive assessment of the structure and function of the human body without the risks associated with imaging by ionizing radiation, and is widely employed in medical care. With advances in technology, increasingly sophisticated devices that exploit NIR are being introduced into clinical practice, and it is important to ensure that their use does not carry unwarranted risks to health.
ICNIRP has published previous statements in 2004 and 2009 about the protection of patients during medical magnetic resonance imaging (MRI), but not other forms of diagnostic NIR. Accordingly, ICNIRP here provides updated advice regarding a broad spectrum of diagnostic devices employing NIR, focusing on those that are currently used clinically.
The aims of this statement are to:
Review the range of diagnostic devices employing NIR that are currently used in clinical settings;
Document the regulations and policies governing the use of such devices for protection of patients and health care workers;
Describe potential risks to the health of patients (representing volunteers and comforters also) and health care workers (representing carers also) as a consequence of diagnostic use of NIR; and
Identify situations of potentially high NIR exposure to patients or health care workers from diagnostic devices, in which protection may not be adequate.
In regard to the last of these objectives, it is recognized that limits on exposure often incorporate reduction factors to allow for uncertainties in available scientific evidence, and that the magnitude of any such adjustment will depend on value judgements that are not simply a matter of science. Furthermore, diagnostic procedures can confer substantial benefits to health, such that, depending on the probability and severity of harm, a risk of adverse effects in patients may in some circumstances be acceptable. However, benefits must outweigh the risks in order to be ethical.
For these reasons, the statement does not form any judgement as to whether or not current regulatory limits are appropriate. Rather, it focuses on whether there is evidence that they fail to protect against demonstrable hazards and, if so, what risks could be expected. In addition, it identifies gaps in currently available evidence that might mask important, unrecognized risks, and that should be a priority for future research.
Consideration is limited to uses of NIR for diagnostic procedures in patients and does not extend to its application in diagnostic procedures conducted away from the patient (e.g., on tissue specimens in the laboratory), nor for use of NIR for therapeutic or cosmetic (the topic of a future ICNIRP Statement) purposes. NIR is taken to include static magnetic fields; time-varying electric, magnetic, and electromagnetic fields (EMF) with frequencies up to 300 GHz (wavelengths down to 1 mm in vacuum); optical radiation with wavelengths from 1 nm to 1 mm; and ultrasound with frequencies of 1 MHz to 40 MHz. Acoustic waves in the audible spectrum are considered only where they result from the use of NIR as defined above. Health effects which arise from the use of devices that employ NIR, but which are not a consequence of the NIR (e.g., claustrophobia from MRI scanners), are not addressed.
Even with these restrictions, the relevant scientific literature is large, and it was not judged practical or efficient to carry out a comprehensive systematic review of all pertinent primary research. Instead, the statement refers where possible to systematic reviews already published by ICNIRP or by other respected authorities (Stam and Bijwaard 2011; de Waard-Schalkx et al. 2015) with supplementary systematic searches of the literature to address any important gaps in their coverage (further details are given later).
DIAGNOSTIC TECHNOLOGIES BASED ON NIR
Diagnostic technologies have been classified by the NIR fields employed.
Electromagnetic fields
EMF with frequencies of 0 to 300 GHz are used in a range of diagnostic devices either directly on the patient to gather diagnostic information, or as a means of storing or transmitting data from monitoring of patients. The benefits of some of these devices are clear and they are used extensively (e.g., MRI) whereas the clinical value of others remains to be established (Table 1a).
Table 1a.
List of technologies applying NIR used for diagnostic purposes, static fields and up to 300 GHz (1 mm).
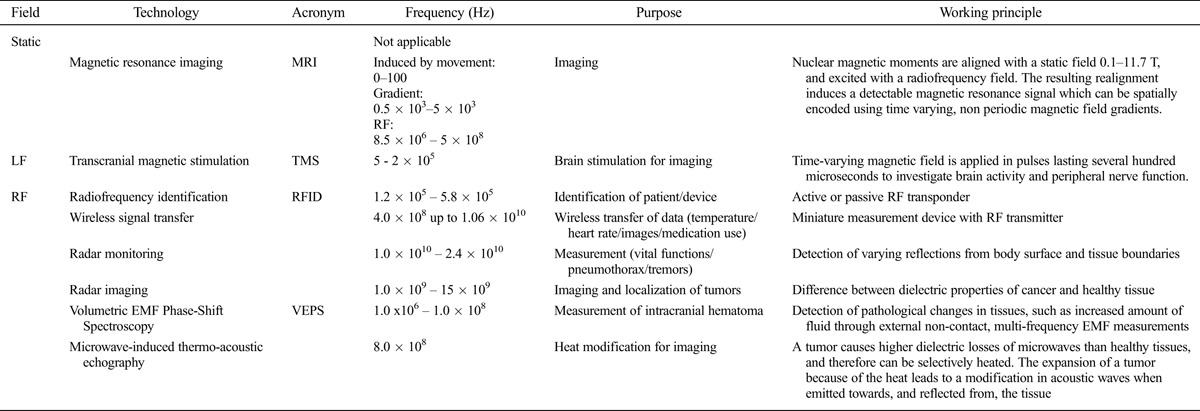
Magnetic resonance imaging (MRI)
MRI is a very widely employed method of clinical investigation which uses a static magnetic field, generally in the range 0.5 to 7 Tesla (T) in combination with time-varying non-periodic EMF (approximately in the range 100–1,000 Hz) and radio frequency EMF (in the range 20–300 MHz). MRI can generate images providing contrast to a wide range of different aspects of organ structure or function. With technological advances, including increases in the strengths of static magnetic fields up to and beyond 7 T, sub-millimetre resolution can now be achieved.
Transcranial magnetic stimulation (TMS)
Apart from its wide therapeutic use, electrical stimulation of brain cortex by magnetic induction is applied diagnostically to investigate brain activity. In addition, magnetic stimulation can be used to study peripheral nerve function. Typically, a time-varying magnetic field is applied in pulses lasting several hundred microseconds. The equivalent frequency based on pulse width and repetition rate can be in the lower kHz range.
RF identification (RFID)
RFID employs EM fields to remotely identify patients, and depending on the characteristic of the device, data such as temperature or blood glucose levels can be acquired and exchanged at distances up to a hundred meters (ICNIRP 2008). More recently, RFID has been further developed as an “implantable” technology. The frequencies employed in RFID range from hundreds of kHz up to 6 GHz.
Wireless signal transfer
As well as monitoring of temperature, wireless signal transfer applications include heart rate monitoring, and exchange of this information between patient and carer. Wireless signal transfer uses miniaturized measurement devices (e.g., temperature sensors) equipped with an RF transmitter to acquire and transmit data. The operational frequency is fixed from 400 MHz to 10 GHz.
Radar for vital functions
Radar using pulsed and ultra-wide band RF and MW signals is being evaluated as a tool for non-invasive monitoring of vital functions. Two of the diagnostic applications most advanced in development are monitoring of breathing for early detection of pneumothorax and monitoring for tremors. The frequencies employed range from nearly 10 GHz up to 24 GHz.
Radar imaging
Radar imaging or MW tomography is used mainly in the diagnosis of breast and skin cancers with some trials on stroke detection emerging (De Santis et al. 2012). The technique exploits the difference between dielectric properties of cancer and healthy tissue, to image and localize tumors even in 3D. The method employs an antenna array that transmits and receives. The frequency range spans 1 GHz to 15 GHz.
Electromagnetic (EM) movement tracking
EM movement tracking is used for diagnostic purposes, for example in analysing jaw movements during mastication. An antenna inserted at a relevant site in the patient transmits information about position.
Volumetric EMF phase-shift spectroscopy (VEPS)
VEPS is being developed to detect and measure intracranial hematoma and oedema. The technology uses frequencies from a few MHz up to hundreds of MHz and can detect pathological changes in tissues, such as increased amount of fluid, through external non-contact, multi-frequency EM measurements. VEPS is relatively inexpensive and therefore could be amenable for use in economically disadvantaged parts of the world.
Microwave-induced thermo-acoustic echography
The main application of microwave-induced thermo-acoustic echography is breast cancer imaging. It uses a combination of microwaves to heat tumors and acoustic waves to sense microwave absorption. A tumor causes higher dielectric losses of microwaves than healthy tissues, and therefore can be selectively heated, optimally at around 800 MHz. The expansion of the tumor because of the heat leads to a modification in acoustic waves when emitted towards, and reflected from, the tissue.
Optical radiation
Diagnostic applications of optical radiation employ wavelengths ranging from short wavelength ultraviolet radiation through the visible spectrum to near infrared radiation (Table 1b).
Table 1b.
List of technologies applying NIR used for diagnostic purposes, optical radiation.
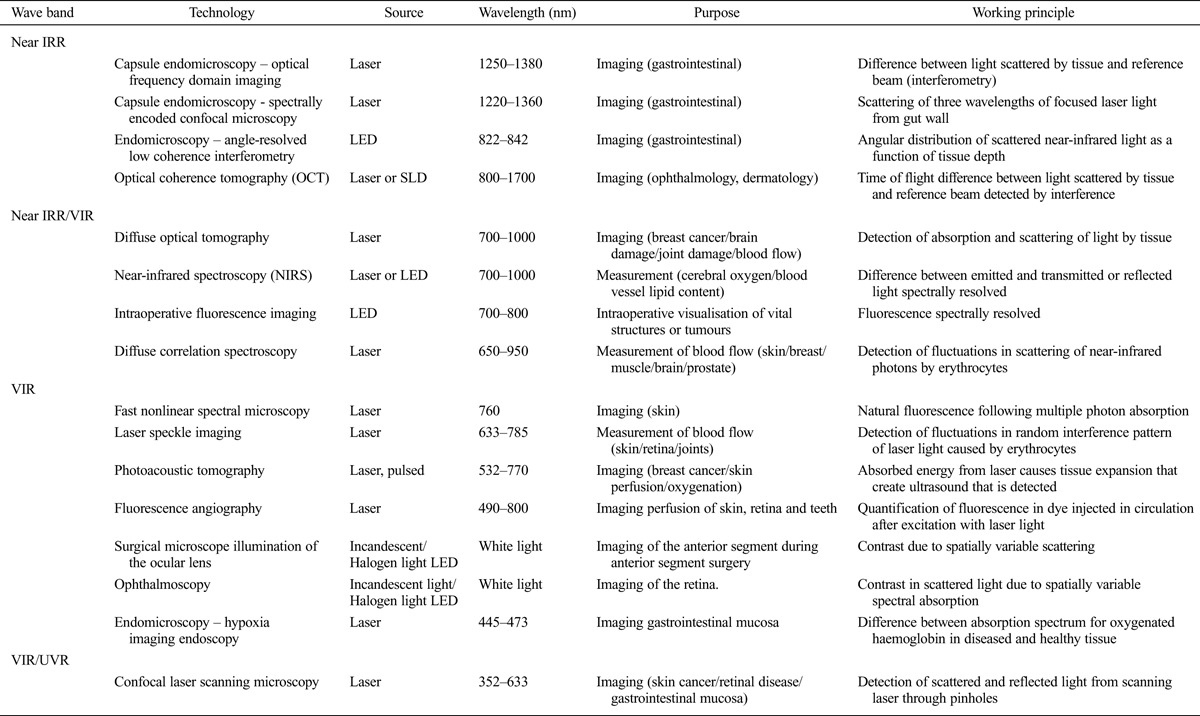
Near-infrared radiation applications
Near-infrared radiation (near IRR) is used as a light source for in vivo internal imaging of the upper gastrointestinal tract. The radiation is delivered through an optical fibre attached to swallowed graded-index lens optics which illuminate the mucosa and record the scatter of near IRR.
Another major clinical application of near IRR is optical coherence tomography. A short coherence super-luminescent light diode (SLD) is used as the source. The primary beam is split into a reference path, which is reflected by a mirror, and a measurement path which is backscattered by the tissues. High lateral resolution of the target tissue requires it to be as close to a point source as possible, and therefore involving high irradiance. The technology is used as a standard diagnostic procedure in ophthalmology and also in dermatology.
Near-infrared radiation-visible radiation (VIR) applications
Diffuse optical tomography uses near IRR and long wavelength visible radiation, typically from an array of diode lasers, as a primarybeam and the backscattered radiation is detected for different wavelengths. The scattering and absorption topography is calculated to create a detailed three-dimensional image of the tissue.
Near-infrared spectroscopy uses a laser or light emitting diode (LED) as the source and detects backscattered light, which is spectrally resolved to calculate cerebral and tissue oxygenation and estimate lipid content. Near-infrared diffuse correlation spectroscopy can be used to measure blood flow in brain, muscle and superficial tumors with a penetration depth of several centimeters. This technique quantifies the motion of red blood cells by measuring fluctuations in their scattering of near-infrared photons.
Intraoperative fluorescence imaging is used during surgical procedures, usually to distinguish tumor tissue from normal tissue. It employs LEDs as a source of near-infrared radiation or visible radiation, and image contrast is due to fluorescence. Irradiance should be below threshold for heating when in use.
Visible radiation applications
Fast non-linear spectral microscopy is used in dermatology in diagnosis of superficial skin cancers. A very short laser pulse induces multiple photon absorption with very high resolution, and secondary fluorescence is then detected. This requires a pulse time in the order of a picosecond, and with current detector technology, an irradiance that exceeds the ICNIRP exposure limit (ICNIRP 2013a).
Laser speckle imaging records fluctuations in random interference patterns of coherent light from a laser. It is used to quantify blood flow in superficial body tissues. Irradiances normally are below the ICNIRP exposure limit. In photoacoustic tomography, a short visible radiation pulse of high intensity is focused with high resolution. The energy that is absorbed causes a rapid increase in temperature and some of the energy is transformed into a mechanical pressure wave, an ultrasound pulse that is time-resolved and recorded for imaging. The magnitude of the ultrasound pulse from a defined depth depends on the optical properties of tissues in front of the focal point.
In fluorescence angiography, a fluorescent dye, fluorescein, is injected into a peripheral vein and the filling of the retinal vessels is observed over time by illumination with an excitation light and concurrent recording of fluorescence.
White light from an incandescent source, a halogen source or an LED lamp is used in ophthalmic surgical microscopes to induce light scattering and enable the structures of the patient’s anterior segment to be visualized. The illumination, particularly with short wavelength visible radiation, exceeds the ICNIRP photochemical exposure limit (ICNIRP 2013b) and is hazardous for the patient’s retina but the exposure is necessary for safe surgery. Thus exposure time is minimized as far as possible, with short wavelength visible radiation filtered out.
White light from the same sources used in ophthalmic surgical microscopes may be used also for illumination of the retina, the backscatter being observed by the examiner or recorded by a camera (fundus photography). Again the principle is to minimize irradiance and exposure time as far as possible (see below).
In endomicroscopy, light of different wavelengths from laser diodes is delivered via a fiber. The fibre tip is coupled into a miniature graded-index lens microscope that focuses the light on the mucosa of the upper gastrointestinal tract, and the backscattered light is imaged with the microscope and recorded as spectrally-resolved wavelength-dependent absorption images.
Visible radiation-ultraviolet radiation applications
In confocal laser scanning microscopy, the illumination is confocal with the focal point of the microscope. Typically, a laser emitting in the visible radiation waveband is used for illumination. The technique is used to image the mucosa of internal organs and for retinal and skin imaging.
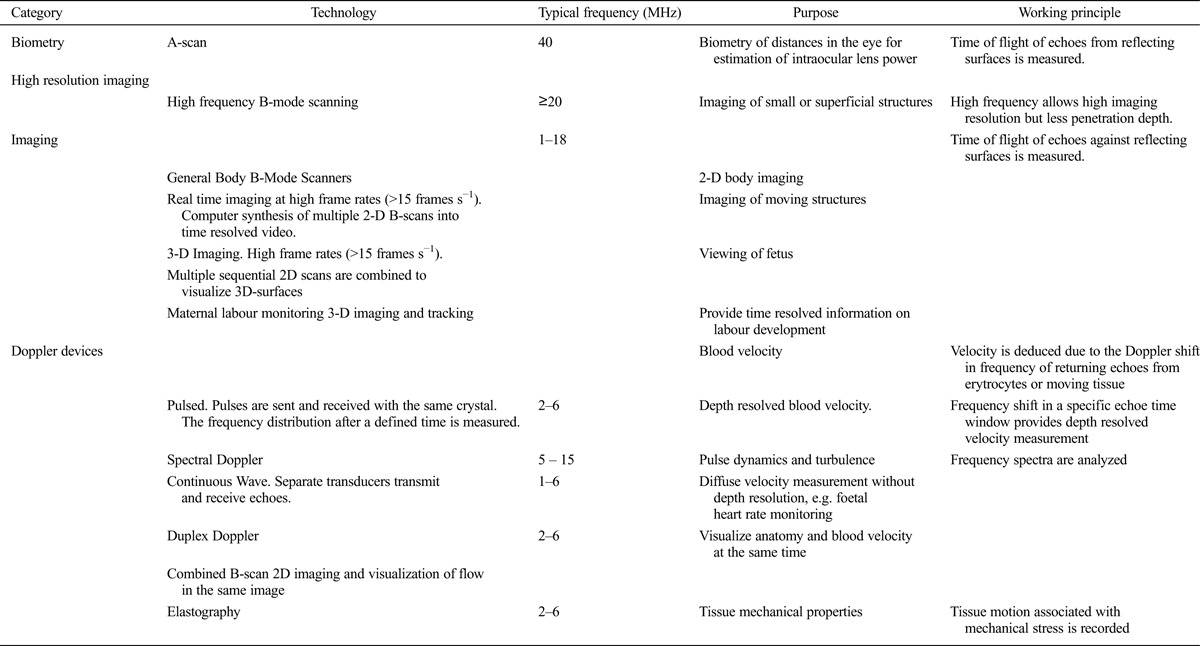
Ultrasound
Ultrasound is a form of oscillating mechanical energy with frequency higher than 20 kHz, a cut-point which is above the audible frequency range for most people. Diagnostic ultrasound devices operate at between 1 MHz and 40 MHz.
Diagnostic ultrasound has advanced remarkably in the past 50 years. It can provide exquisite visualization of internal anatomy and is used extensively in clinical practice. Currently, pregnant women in most countries are examined with ultrasound at least once.
Diagnostic ultrasound machines operate with different modes. In the A mode the intensities of echoes from various depths are resolved in one dimension. In B-mode the ultrasound beam is scanned in two dimensions thus providing 2D information. In C-mode, several adjacent B-scans are stacked together to provide 3D information. In M mode, the B-scan or the C-scan is resolved over time thus showing motion in the tissue examined. In the Doppler mode the scan is used to assess the velocity of blood flow or a moving internal structure, which is determined by measuring the Doppler shift of frequency in returning echoes. A summary of ultrasound techniques is given in Table 1c.
Table 1c.
List of technologies applying NIR used for diagnostic purposes, ultrasound.
INTERNATIONAL AND NATIONAL REGULATORY STRUCTURES
Several independent organizations have published guidelines on the avoidance of harm from exposures to NIR generated by diagnostic devices (Table 2). These guidelines may be used by governmental bodies that issue legally-binding regulations on exposures to NIR.
Table 2.
Examples of organisations issuing legally binding regulation and guidelines for human protection against hazardous health effects of NIR.
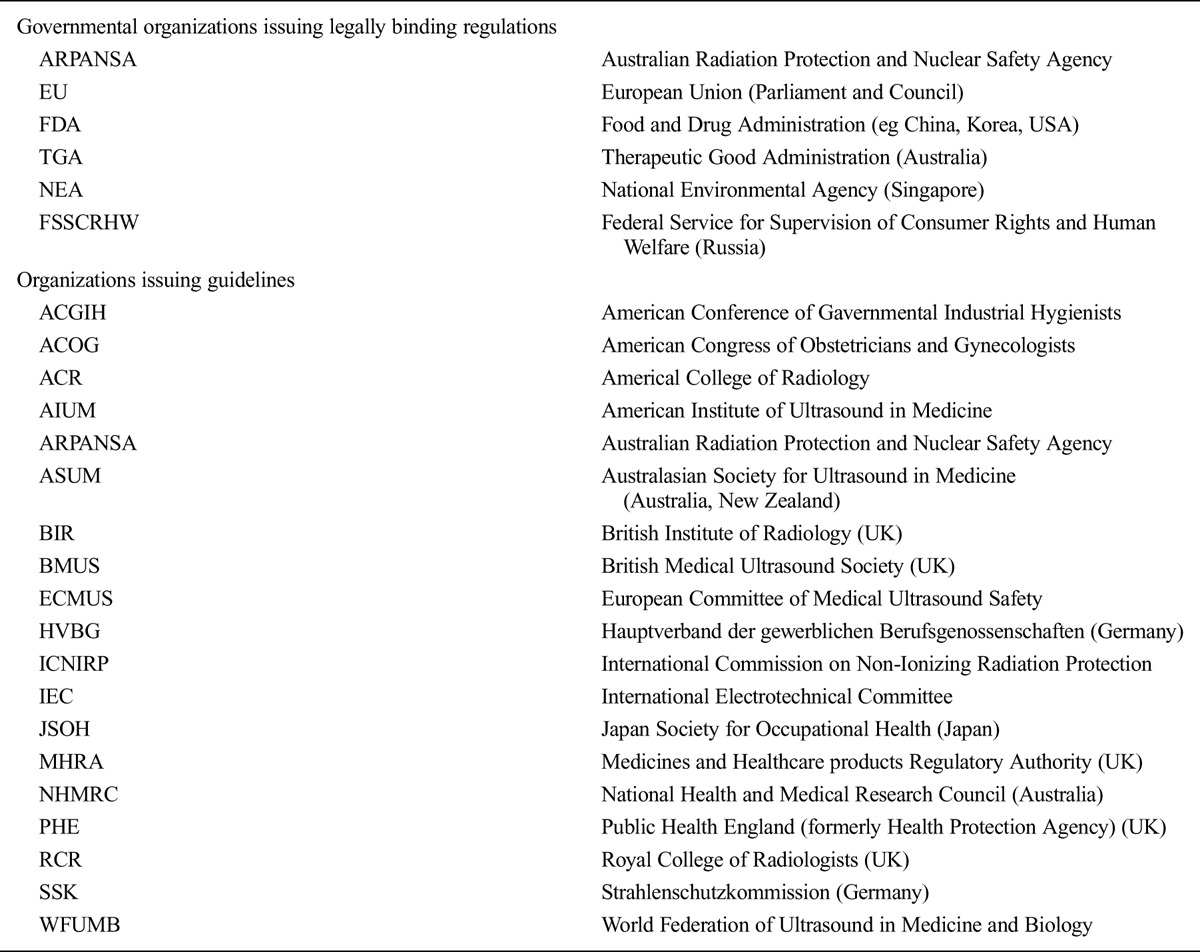
Regulation of medical devices is intended to ensure effective medical devices of good quality that are safe for the intended purpose. The essential requirements concern the protection of the users and the environment. In most countries that regulate medical devices, a national regulatory authority (NRA) sets regulatory controls in pre-market, on the market and post-market phases of the medical device. The safe use of medical devices in health care settings is usually not the responsibility of the NRA.
In European Union (EU) countries, EU Directives regulating exposures from NIR devices are implemented by transposition into national laws or regulations. Separate directives cover devices, patients and workers (Tables 3a–c; 4a–c). It is notable that in the recent EU Directive (2013/35/EU) limiting the exposure of workers to electromagnetic fields, exposures from MRI used in the healthcare sector could exceed the exposure limit values, provided other conditions were satisfied. On the other hand, EU member states are free to apply stricter limits for workers than those in the EMF directive and some (e.g., Poland) have already done so.
Table 3a.
Examples of legally binding regulations associated with diagnostic devices based on NIR for protection of patients, static fields and time varying electromagnetic fields less than 0.3 THz.
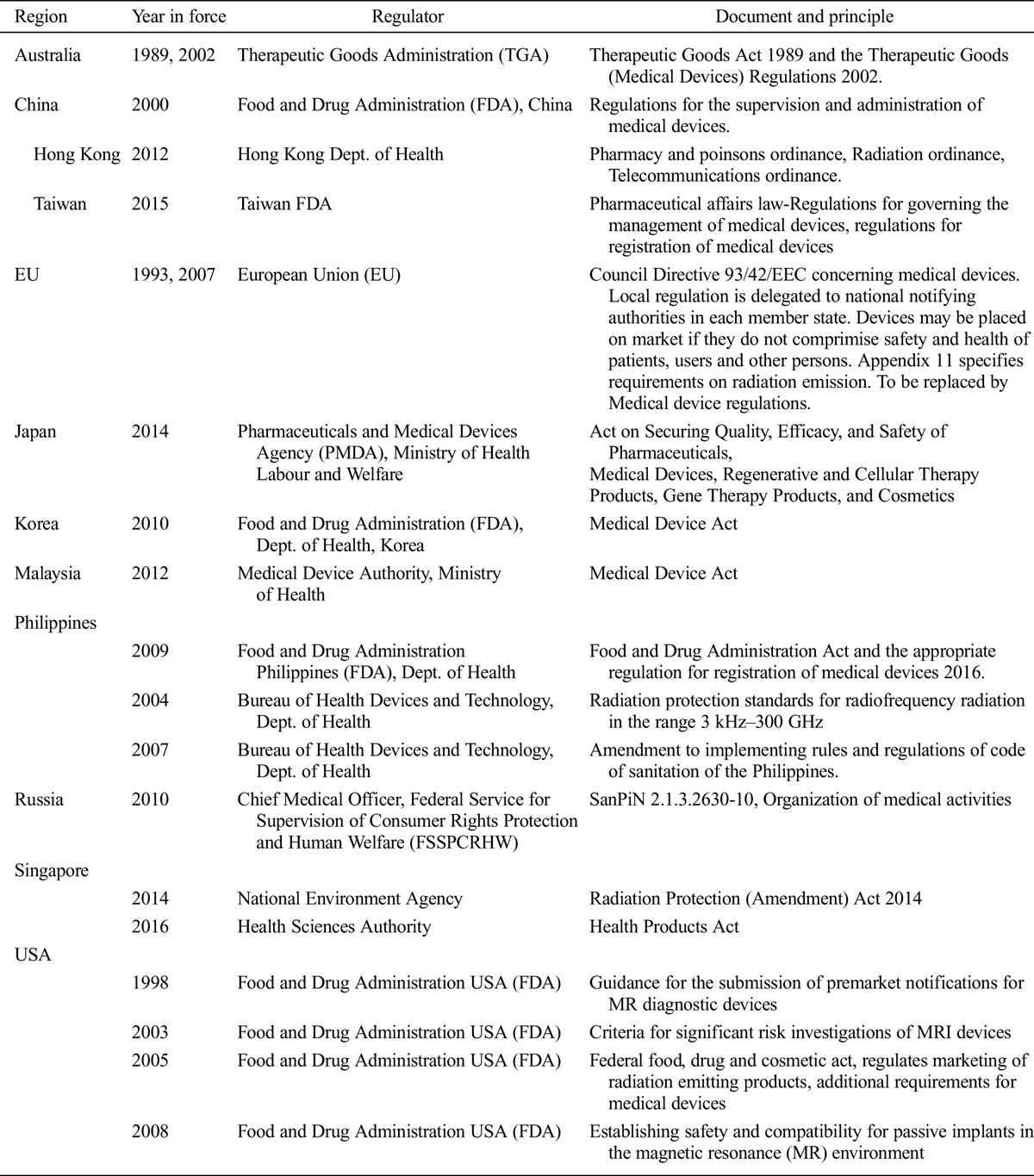
Table 3c.
Examples to show range of legally binding regulations associated with diagnostic devices based on NIR for protection of patients, ultrasound.
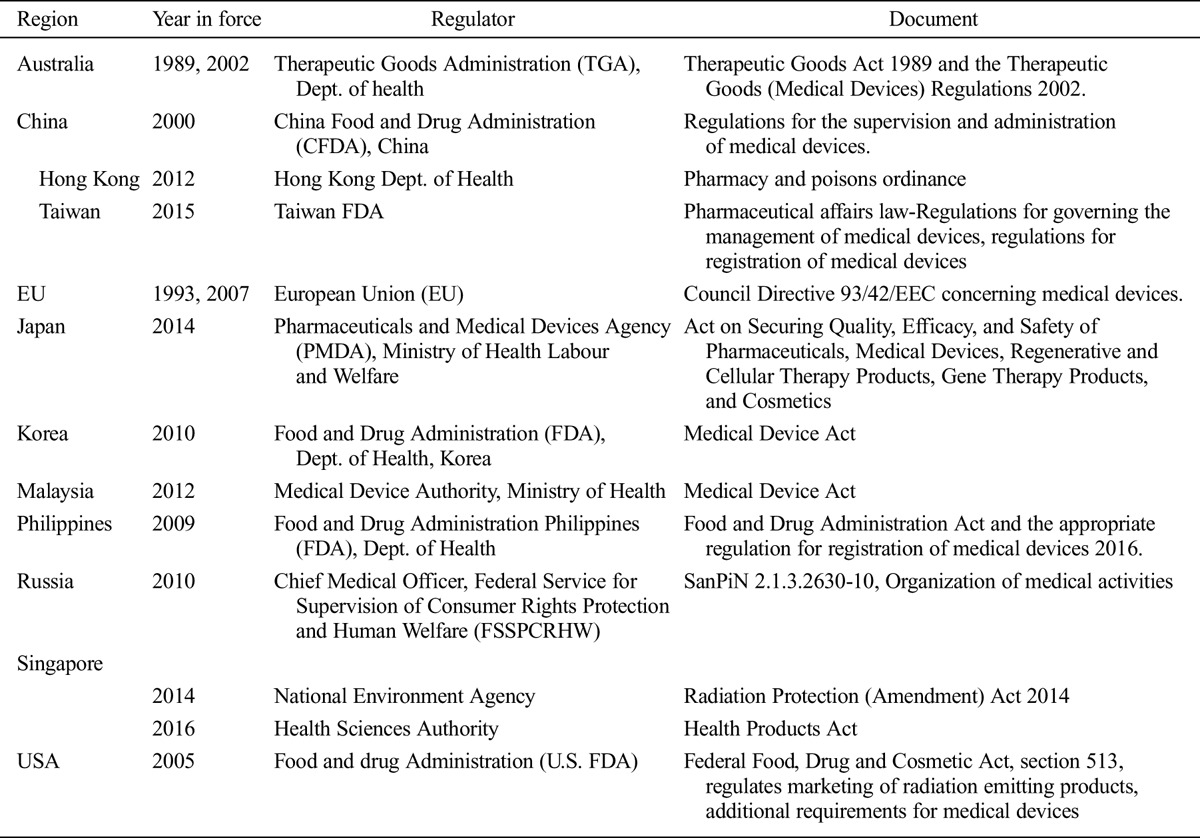
Table 4a.
Examples of legally binding regulations associated with diagnostic devices based on NIR for protection of workers, static and time varying electromagnetic fields less than 0.3 THz.
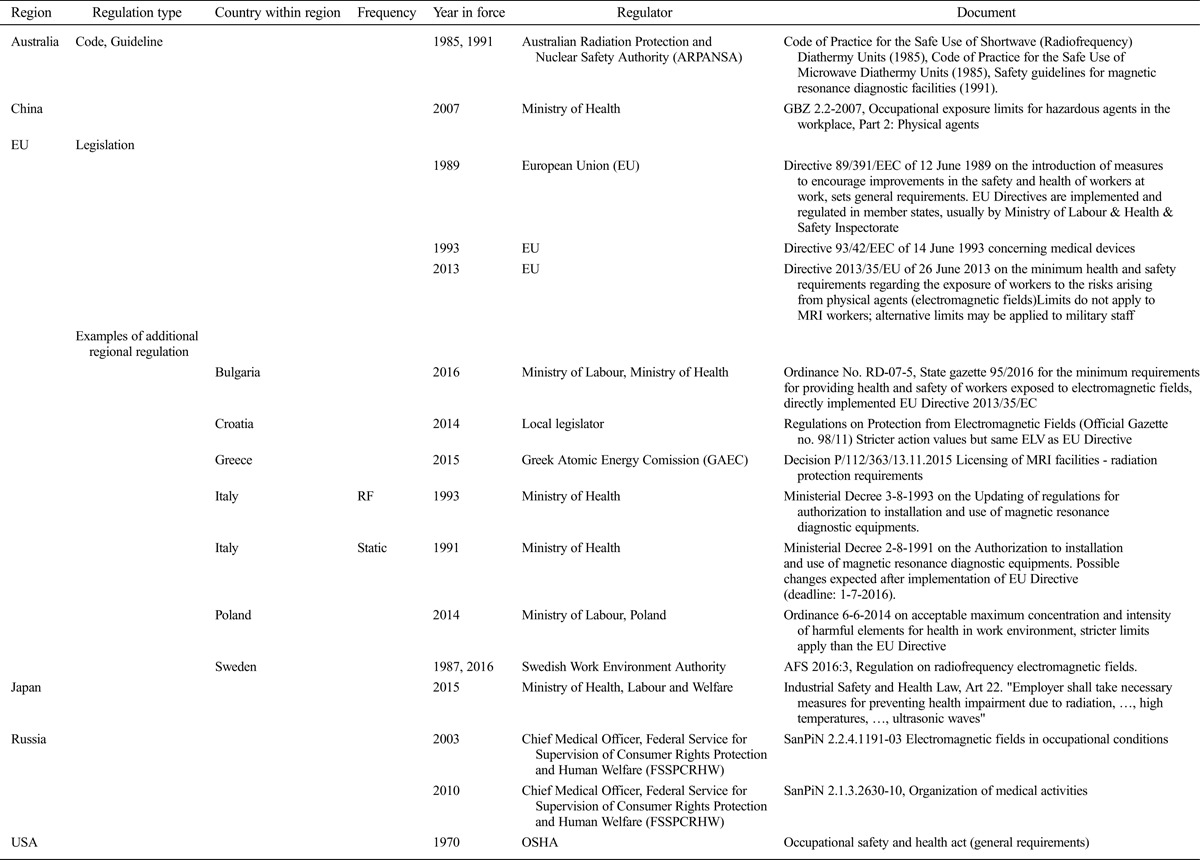
Table 4c.
Examples of legally binding regulation associated with diagnostic devices based on NIR for protection of workers, ultrasound.
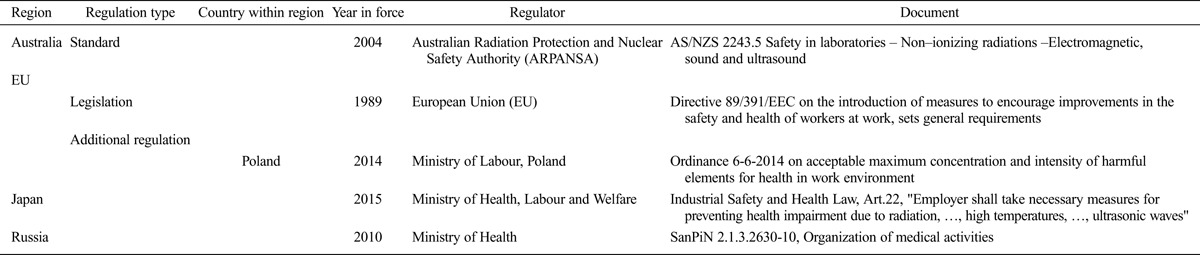
Table 3b.
Examples of legally binding regulations associated with diagnostic devices based on NIR for protection of patients, optical radiation (1 nm-1 mm).
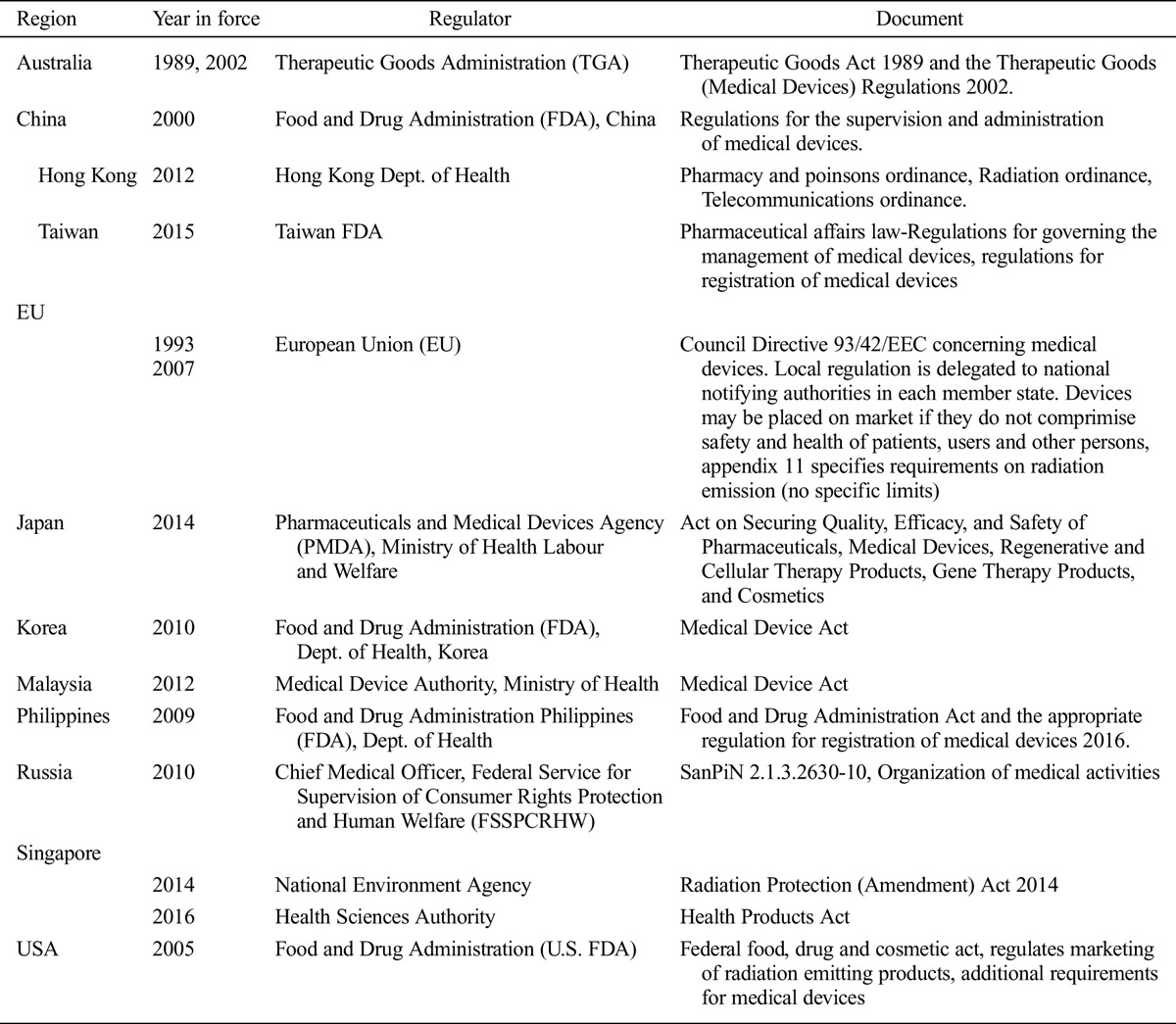
Table 4b.
Examples of legally binding regulation associated with diagnostic devices based on NIR for protection of workers, optical radiation (100 nm–1 mm).
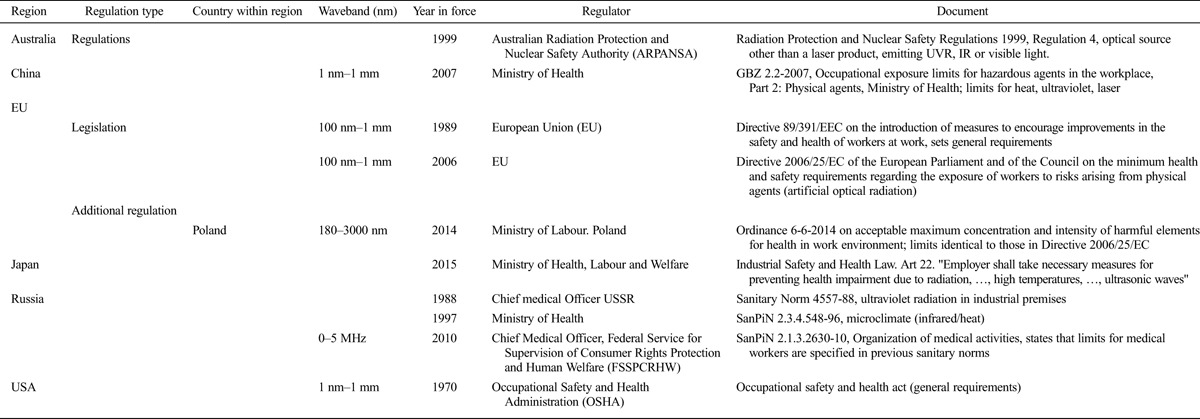
In the Russian Federation, medical devices and activities must comply with a federal sanitary regulation which lists fixed emission limits for NIR. In addition, there are federal regulations for workers with occupational exposure limits for EMF, infrared, and ultraviolet radiation. The occupational EMF limits are stricter than ICNIRP occupational reference levels and depend on the duration of exposure.
In many Asian countries, a law is passed by the country’s legislative body creating an NRA that then issues the regulations. Examples of NRAs that regulate medical devices (mainly through registration of such devices) are the Food and Drug Administration of the Philippines, the Malaysia Medical Device Authority, the Thai Food and Drug Administration, the China Food and Drug Administration, the Hong Kong Medical Device Control Office, the Ministry of Food and Drug Safety of Korea, and the Vietnam Department of Medical Equipment and Health Works. In Singapore, the National Environment Agency regulates use of devices while the Health Sciences Authority regulates production, import, export, sale, and distribution of medical devices. In the Philippines, the Food and Drug Administration regulates not just the production, import, export, sale, and distribution of medical and radiation devices but also their use, when applicable. In November 2014, the Association of Southeast Asian Nations (ASEAN) signed the ASEAN Medical Device Directive (AMDD), which establishes a harmonized regulatory model for medical device regulation for its member states. The regulation will come into force upon ratification.
The U.S. Food and Drug Administration implements its federal Food, Drugs, and Cosmetics Act by issuing regulations which become part of the U.S. Code of Federal Regulations. Individual states of the U.S. may have further regulations for the use of NIR medical devices. Arizona, which is an example of a state with regulations on the use of NIR devices, requires the registration of non-ionizing radiation facilities. At the same time, a non-governmental organization, the American College of Radiology (ACR), operates a scheme for accreditation of MRI facilities (and offers this service internationally). Similarly, the American Institute of Ultrasound in Medicine accredits clinical facilities using ultrasound. Although accreditation is voluntary, it is required for reimbursement by many private health insurance companies.
In many countries, there is no legislation/regulation governing the use of NIR in diagnostic devices. Instead, practitioners refer to guidelines issued by national or international or professional associations. These guidelines may or may not be followed.
Legislation/Regulation for protection of patients
Legally-binding regulations associated with diagnostic devices based on NIR intended for protection of patients are listed in Table 3a–c.
Legislation/Regulation for protection of health workers
Legally binding regulations associated with diagnostic devices based on NIR intended for protection of workers are listed in Table 4a–c.
EPIDEMIOLOGICAL EVIDENCE FOR HEALTH RISKS ASSOCIATED WITH EXPOSURE TO DIAGNOSTIC NIR DEVICES
Most of the relevant epidemiological evidence that is currently available relates to MRI or ultrasound.
MRI
Research on possible adverse effects from diagnostic use of MRI was identified by a non-systematic review of the literature for relevant epidemiological studies and clinical reports and by hand-searching references of key reports.
Overall, MRI has been used clinically for about three decades with apparently few serious side effects aside from well-documented acute injuries resulting from effects on implanted electronic devices or acceleration of ferromagnetic materials towards the scanner by the magnetic field, or from RF-induced burns due to poor positioning of the patient in the scanner.
Previous reviews of the health effects of fields of MRI equipment do not suggest long-term adverse health effects (HPA 2008a; ICNIRP 2009a). This is particularly the case for static fields (WHO 2006; HPA 2008b; ICNIRP 2009b), for which there is no substantiated evidence for any health effect that could inform the design of an epidemiological study. However, the effect of RF power deposition in tissues should be investigated.
Patients: Acute perceptual and cognitive effects
Acute perceptual and cognitive effects are well recognized effects that have been reported by subjects undergoing diagnostic MRI. They occur particularly when high static magnetic fields are employed (Rauschenberg et al. 2014), but symptoms have sometimes been reported in relation to field strengths as low as 1.5 T (Heilmaier et al. 2011). The largest study available was a multicentre trial that used 7 T and 9.4 T MRI systems and collected data through 3,457 completed questionnaires (Rauschenberg et al. 2014). The study aimed to separate sensory side effects during movement on the patient table from those experienced while lying still at the isocenter. Most participants (82%) rated the examination at least as tolerable; 8% felt discomfort; and only 1% of the image acquisitions had to be terminated prematurely. No adverse events occurred in any examination. Only 1% of the subjects were unwilling to undergo further ultra-high field MRI examinations. Long duration of examination was the most frequent cause of discomfort, followed by acoustic noise and lying still. All magnetic-field-related sensations were more pronounced when moving the patient table compared to resting at the isocenter position (19%/2% of the subjects felt unpleasant vertigo during the moving/stationary state). Vertigo was the most frequently reported sensory side effect overall, and was more pronounced at 9.4 T than at 7 T, although its prevalence varied substantially between the different trial sites. Several mechanisms have been proposed to explain this vertigo including differences in magnetic susceptibility between the vestibular organs and surrounding fluid, induced currents acting on hair cells (Glover et al. 2007) or the Lorentz force inside the lateral semi-circular canal (Roberts et al. 2011).
Patients: Developmental effects of prenatal MRI
A large prospective observational study examining the effects of prenatal exposure to 1.5-T MRI on developmental outcome (Bouyssi-Kobar et al. 2015), as assessed by a norm-referenced, psychometrically sound functional assessment scale, found no association with adverse functional outcomes or hearing impairment.
Medium- to long-term ill-effects of undergoing diagnostic MRI are believed to be few, though there is a dearth of epidemiological studies to evaluate this. This may reflect the difficulty of designing patient-studies that are not substantially confounded. Firstly, both the medical indication for the scan and the range of associated investigations and treatments may have their own health consequences. Secondly, MRI is often associated with the administration of contrast agents which themselves can have clear short- and medium-term effects (e.g. accumulation of gadolinium from contrast agents in the body). Using a control group who have had a CT scan, for example, is not feasible since CT carries its own, established health risks. A future opportunity to obtain unbiased data about possible health effects of diagnostic MRI arises from its use in large population-based longitudinal studies. For example, the UK Biobank project is planning to phenotype 100,000 apparently healthy subjects in the next few years using MRI, although their exposure will be limited. There are also other groups (such as workers and consumers involved in neuro-marketing) who volunteer for MR scans and receive regular, high exposure over several years. While these voluntary exposures vary considerably and may be confounded by other exposures such as to ionizing radiation, such groups may be a useful resource for epidemiological research in the future. While molecular changes have been demonstrated following in vitro experimental exposures to magnetic fields (with and without contrast agents) (Fiechter et al. 2013; Lancellotti et al. 2015; Vijayalaxmi et al. 2015), such findings have not been reflected in the limited evidence that is available on health outcomes.
Health workers: Acute perceptual and cognitive effects
It has long been known that people working in the vicinity of MRI scanners can experience transient vertigo (as well as a metallic taste in their mouths). These effects occur not only with movement in the field, but also when people are stationary, and they become pronounced when staff work inside or close to the end of the bore (where the field can be particularly high for shielded magnets). Underlying mechanisms that have been proposed include hydrodynamic effects in the vestibular system (Schenck 2005; Glover et al. 2007), and a direct magnetic susceptibility effect on the sensory hair cells (Glover et al. 2007), but currently the accepted mechanism is a Lorentz force on the dark current within the vestibular system (Roberts et al. 2011).
A study among 361 healthcare and research staff working with MRI scanners in the Netherlands (Schaap et al. 2014) assessed the incidence and association of transient perceptual symptoms with static magnetic field exposure based on diaries reporting work activities and symptoms during work shifts inside and/or outside an MRI facility. Participants included both MRI staff and radiographers who never worked with MRI. Symptoms (mainly vertigo and metallic taste) were reported during 16–39% of the MRI work shifts, and there were significant positive associations with increasing scanner strength, ranging from 2-fold increases at 1.5 T to 4‐fold increases at 7.0 T. A meta-analysis of 5 studies published during 1992–2007 found the only neuropsychological effect relating to static magnetic field exposure to be visual impairment. Further research into this possibility is needed.
Health workers: Pregnancy outcomes
One study compared self-reported pregnancy outcomes of female MRI workers from the 1990s (Kanal et al. 1993) (when fields were lower than today but extended further to non-MRI workers) adjusted for age, smoking, and alcohol use. No increase in risk of spontaneous abortions, delayed conception, early delivery, low birth weight, or male sex of offspring was seen compared to when they were employed elsewhere before working with MRI.
Optical radiation
A current literature search did not reveal any studies indicating adverse effects associated with the use of optical radiation in diagnostic procedures. Surveillance programs for workers using laser applications had not revealed any unexpected health hazards by the early 1990s, and since then have been abandoned in most countries.
Ultrasound
Research on possible adverse effects from diagnostic use of ultrasound was identified from a previous systematic review (HPA 2010), and through a systematic search of the Embase and Ovid Medline databases, looking for relevant epidemiological studies and clinical case reports. Information was found concerning potential acute effects, longer term obstetric and developmental outcomes following use of ultrasound during pregnancy, and risk of childhood cancer after prenatal exposure to ultrasound.
Acute effects
Possible acute effects that have been investigated include stimulation of foetal movements during the later stages of pregnancy (Fatemi et al. 2001); altered electroencephalographic (EEG) activity in neonates during and after ultrasound examination (Kohorn et al. 1967); erythrocyte fragility in women exposed to continuous ultrasound monitoring during labor (Bause et al. 1983); and structural changes in the brain (assessed by MRI) following insonation through the temporal bone (Schlachetzki et al. 2002). Adverse outcomes reported to follow ultrasound imaging of the liver (Piscaglia et al. 2006) and heart (van der Wouw et al. 2000) may have been a toxic effect of contrast agents (such as microbubbles with high echogenicity used to enhance the sonogram), and cannot be attributed to ultrasound exposure per se with certainty. They could also reflect an interaction between ultrasound and contrast agents. Study findings to date do not point clearly to any acute adverse effects of human exposure to diagnostic ultrasound, but further research on possible interactions with contrast agents would be useful.
Pregnancy and birth outcomes
B-scans are used for dating conception, identifying multiple pregnancies, fetal abnormalities, and placental location. Later in pregnancy, Doppler studies, usually employing continuous wave sources, may be used to study blood flow in the umbilical artery as a guide to fetal well-being, while low intensity Doppler ultrasound is often used to monitor fetal heart rate (cardiotocography). The progressive adoption of these techniques over the last 50 years has been so extensive that in many countries, almost all pregnancies now entail some exposure to ultrasound. Thus most research on humans has compared higher with lower exposures rather than exposure with no exposure.
A substantial number of observational studies have assessed outcomes of pregnancy in relation to exposure to diagnostic ultrasound, but in some investigations, associations may have been confounded by the clinical indications for ultrasound examination. Such confounding could occur if diagnostic ultrasound were used more frequently in patients already at higher risk of adverse outcomes. However, results of more than 25 randomized controlled trials of ultrasound scans at different stages of pregnancy, or of Doppler studies of the umbilical artery, do not suggest any adverse effects of ultrasound examination on miscarriage rate, gestational age at delivery, or perinatal mortality (Bucher and Schmidt 1993; McKenna et al. 2003; Skråstad et al. 2013). Similarly, the balance of evidence does not indicate any adverse effect of prenatal ultrasound on anthropometric measures at birth or neonatal morbidity (Alfirevic and Neilson 1995; McKenna et al. 2003; Skråstad et al. 2013), though evidence about specific congenital malformations is limited (Hellman et al. 1970; Mukubo 1986; Tikkanen and Heinonen 1992). In theory, congenital malformations might be an adverse outcome, especially from high intensity exposures in the first trimester, since they may be induced by heating. However, it is unlikely that increases in temperature from diagnostic ultrasound as currently used would be sufficient to cause congenital abnormalities.
Developmental outcomes
Research using various designs, including case-control and cohort studies and randomized controlled trials, has explored the relationship of diagnostic ultrasound in pregnancy to a wide range of developmental outcomes in childhood—namely, growth, vision, hearing and speech, reading and intellectual performance, handedness and mental health (Salvesen et al. 1992a and b, 1993a and b; Kieler et al. 1997, 1998a and b, 2001, 2002, 2005). Among these, the only possible association to emerge has been with non-right-handedness (Salvesen et al. 1993b) (a possible marker for adverse impacts on neurological development). However, the findings on this have not been entirely consistent, and it cannot be regarded as an established effect.
Childhood cancer
Case-control studies of the risk of childhood cancer collectively suggest that prenatal exposure to ultrasound does not increase the risk of any of the most common types of childhood cancer (Shu et al. 1994, 2002; Sorahan et al. 1995). Although the results of some studies may have been biased by selective participation (e.g. controls being unrepresentatively affluent or better educated) or by mothers’ inaccurate recall of exposure, it seems unlikely that this would have obscured important associations. Moreover, studies that ascertained exposures only from medical records (Naumburg et al., 2000; Stålberg et al. 2008) did not suggest higher risks.
Risks to patients
The balance of evidence now available does not point to any serious adverse effects in patients from exposure to diagnostic ultrasound as used in normal clinical practice, in the absence of ultrasound contrast agents.
Risks to workers
No studies were found that directly examined potential health risks in health care workers using diagnostic ultrasound. However, given the apparent absence of harm in patients, and the low exposure of operators (perhaps most likely to occur if they informally test the ultrasound probe on their arm before applying it to the patient), no risk would be expected from current exposures.
Uncertainties
Among the uncertainties in the current evidence base, highest priorities for further research are the risks of congenital malformations following exposure to ultrasound in utero (particularly in the first trimester), and the potential for adverse effects from interactions between ultrasound and contrast media, on which relatively little information is available.
POTENTIAL HEALTH RISKS NOT COVERED BY LEGISLATION/REGULATION AND IMPORTANT AREAS OF UNCERTAINTY
Static magnetic field and radiofrequency EMF
Apart from MRI, specific guidelines or regulations to limit exposure and/or quantify dose in patients or health workers are few. For example, while there are occupational studies (Karlström et al. 2006) and safety guidelines (Rossi et al. 2009) concerning TMS, these mostly concern therapeutic applications. Evaluation of health effects or safety risks for many NIR diagnostic methods is therefore difficult and deserves further research.
Potential effects on the patient
MRI is associated with several adverse effects in patients, including a potential for uncomfortable exposure to acoustic noise, heating, and sensory disturbances (in particular vertigo). However, all of these effects are reversible and can be prevented or ameliorated. There is insufficient evidence on which to draw firm conclusions about long-term health effects, although there is little theoretical reason to expect any permanent damage if scanners are operated in line with existing regulations. A priority for further research is to investigate any potential harmful effects from exposure to the fetus during pregnancy, particularly during the first trimester.
Potential effects on health workers
In normal clinical practice, staff working with MRI scanners may experience transient vertigo and related sensory disturbances which might carry a risk of personal injury. Again, there is insufficient evidence from which to draw solid conclusions about long-term risks to health, although theoretical considerations suggest that a hazard is unlikely. More information on any long-term effects in well-defined MRI worker cohorts would be useful.
Optical radiation
No reports were found of adverse short- or long-term health effects, either in patients or in health care workers, from diagnostic technologies using optical radiation that complied with current guidelines.
Potential risks to the patient
Regulations for avoidance of skin and eye damage from diagnostic exposure are based on tissue-specific estimates of thresholds across the optical spectrum for short-term onset (within a week), and cover exposure times from femtoseconds to hrs. Accidental ocular exposure is potentially hazardous and data on thresholds for effects from exposures to repetitive short pulses are limited. However, the reduction factor that is applied in current regulations and guidelines for safe exposure should be sufficiently conservative to protect against injury.
As there is little or no systematic information on threshold doses for harm from exposures to optical radiation within the body, no specific regulations have been developed. However, exposure limits for such exposures would be useful.
Potential risks in health workers
Regulations place controls on the geometry of spaces where diagnostic technologies using optical radiation are used. Moreover, special warning lights must be mounted outside such spaces, where exposures could exceed regulatory limits. Both of these requirements are intended to avoid any exposure without use of protective equipment.
Optical radiation can efficiently be blocked by safety goggles. Appropriate use of safety goggles in a space where diagnostic technologies using optical radiation are used is required by regulations and eliminates any risk for health workers being exposed to harmful doses.
Ultrasound
The balance of evidence now available does not point to any harmful effects, either in patients or health care workers, from exposure to diagnostic ultrasound as used in normal clinical practice, in the absence of contrast agents.
It would, however, be useful to carry out further research on the risks of congenital malformations following exposure to ultrasound in utero (particularly in the first trimester), and the potential for adverse effects from interactions between ultrasound and contrast media.
Acknowledgment
ICNIRP is grateful for the contributions and comments by Emilie van Deventer (WHO, Team Leader, Radiation Programme), Josée Hansen (WHO, Senior Advisor, Department of Essential Medicines and Health Products) and Adriana Velazquez Berumen (WHO, Senior Advisor and Focal Point on Medical Devices).
ICNIRP gratefully acknowledges also the general support received from the International Radiation Protection Association (IRPA), the German Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety (BMUB), and the European Union Programme for Employment and Social Innovation "EaSI" (2014–2020). For further information please consult: http://ec.europa.eu/social/easi. The information contained in this publication does not necessarily reflect the official position of the European Commission or any other donors. All information concerning the support received by ICNIRP is available at http://www.icnirp.org/en/about-icnirp/support-icnirp/index.html.
Footnotes
The authors declare no conflicts of interest.
(Manuscript accepted 18 December 2016)
Contributor Information
Collaborators: International Commission on Non-Ionizing Radiation Protection (ICNIRP)
REFERENCES
- Alfirevic Z, Neilson JP. Doppler ultrasonography in high-risk pregnancies: systematic review with meta-analysis. Am J Obstet Gynecol 172:1379–1387; 1995. [DOI] [PubMed] [Google Scholar]
- Bause GS, Niebyl JR, Sanders RC. Doppler ultrasound and maternal erythrocyte fragility. Obstet Gynecol 62:7–10; 1983. [PubMed] [Google Scholar]
- Bouyssi-Kobar M, du Plessis AJ, Robertson RL, Limperopoulos C. Fetal magnetic resonance imaging: exposure times and functional outcomes at preschool age. Pediatr Radiol 45:1823–1830; 2015. [DOI] [PubMed] [Google Scholar]
- Bucher HC, Schmidt JG. Does routine ultrasound scanning improve outcome in pregnancy? Meta-analysis of various outcome measures. BMJ 307:13–17; 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Santis V, Sill JM, Bourqui J, Fear EC. Safety assessment of ultra-wideband antennas for microwave breast imaging. Bioelectromagnetics 33:215–225; 2012. [DOI] [PubMed] [Google Scholar]
- de Waard-Schalkx I, Stam R, van der Schaaf M, Bijwaard H. Recent developments in medical techniques involving ionising or non-ionising radiation: update 2014. Bilthoven: National Institute for Public Health and the Environment; 2015. [Google Scholar]
- Fatemi M, Ogburn PL, Greenleaf JF. Fetal stimulation by pulsed diagnostic ultrasound. J Ultrasound Med 20:883–889; 2001. [DOI] [PubMed] [Google Scholar]
- Fiechter M, Stehli J, Fuchs TA, Dougoud S, Gaemperli O, Kaufmann PA. Impact of cardiac magnetic resonance imaging on human lymphocyte DNA integrity. Eur Heart J 34:2340–2345; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover PM, Cavin I, Qian W, Bowtell R, Gowland PA. Magnetic-field-induced vertigo: a theoretical and experimental investigation. Bioelectromagnetics 28:349–361; 2007. [DOI] [PubMed] [Google Scholar]
- Health Protection Agency. Protection of patients and volunteers undergoing MRI procedures: advice from the Health Protection Agency. Didcot, U.K.: Health Protection Agency; 2008a. [Google Scholar]
- Health Protection Agency. Static magnetic fields: report of the independent Advisory Group on Non-Ionising Radiation. Didcot, U.K.: Health Protection Agency; 2008b. [Google Scholar]
- Health Protection Agency. Health effects of exposure to ultrasound and infrasound: report of the independent Advisory Group on Non-Ionising Radiation. Didcot, U.K.: Health Protection Agency; 2010. [Google Scholar]
- Heilmaier C, Theysohn JM, Maderwald S, Kraff O, Ladd ME, Ladd SC. A large-scale study on subjective perception of discomfort during 7 and 1.5 T MRI examinations. Bioelectromagnetics 32:610–619; 2011. [DOI] [PubMed] [Google Scholar]
- Hellman LM, Duffus GM, Donald I, Sunden B. Safety of diagnostic ultrasound in obstetrics. Lancet 1:1133–1135; 1970. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. ICNIRP statement on EMF-emitting new technologies. Health Phys 94:376–392; 2008. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. Amendment to the ICNIRP Statement on Medical Magnetic Resonance (MR) Procedures: protection of patients. Health Phys 97:259–261; 2009a. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. Guidelines on limits of exposure to static magnetic fields. Health Phys 96:504–514; 2009b. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. ICNIRP guidelines on limits of exposure to laser radiation of wavelengths between 180 and 1000 μm. Health Phys 105:271–295; 2013a. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. ICNIRP Guidelines on limits of exposure to incoherent visible and infrared radiation. Health Phys 105:74-91; 2013b. [DOI] [PubMed] [Google Scholar]
- Kanal E, Gillen J, Evans JA, Savitz DA, Shellock FG. Survey of reproductive health among female MR workers. Radiol 187:395–399; 1993. [DOI] [PubMed] [Google Scholar]
- Karlström EF, Lundström R, Stensson O, Hansson Mild K. Therapeutic staff exposure to magnetic field pulses during TMS/rTMS treatments. Bioelectromagnetics 27:156–158; 2006. [DOI] [PubMed] [Google Scholar]
- Kieler H, Haglund B, Waldenström U, Axelsson O. Routine ultrasound screening in pregnancy and the children’s subsequent growth, vision and hearing. Br J Obstet Gynaecol 104:1267–1272; 1997. [DOI] [PubMed] [Google Scholar]
- Kieler H, Ahlsten G, Haglund B, Salvesen K, Axelsson O. Routine ultrasound screening in pregnancy and the children’s subsequent neurologic development. Obstet Gynecol 91:750–756; 1998a. [DOI] [PubMed] [Google Scholar]
- Kieler H, Axelsson O, Haglund B, Nilsson S, Salvesen KÅ. Routine ultrasound screening in pregnancy and the children’s subsequent handedness. Early Hum Dev 50:233–245; 1998b. [DOI] [PubMed] [Google Scholar]
- Kieler H, Cnattingius S, Haglund B, Palmgren J, Axelsson O. Sinistrality–a side-effect of prenatal sonography: a comparative study of young men. Epidemiol 12:618–623; 2001. [DOI] [PubMed] [Google Scholar]
- Kieler H, Cnattingius S, Palmgren J, Haglund B, Axelsson O. First trimester ultrasound scans and left-handedness. Epidemiol 13:370; 2002. [DOI] [PubMed] [Google Scholar]
- Kieler H, Haglund B, Cnattingius S, Palmgren J, Axelsson O. Does prenatal sonography affect intellectual performance? Epidemiol 16:304–310; 2005. [DOI] [PubMed] [Google Scholar]
- Kohorn EI, Pritchard JW, Hobbins JC. The safety of clinical ultrasound examination. Obstet Gynaecol 29:272–274; 1967. [PubMed] [Google Scholar]
- Lancellotti P, Nchimi A, Delierneux C, Hego A, Gosset C, Gothot A, Jean-Flory Tshibanda L, Oury C. Biological effects of cardiac magnetic resonance on human blood cells. Circ Cardiovasc Imaging 8:e003697; 2015. [DOI] [PubMed] [Google Scholar]
- McKenna D, Tharmaratnam S, Mahsud S, Bailie C, Harper A, Dornan J. A randomized trial using ultrasound to identify the high-risk fetus in a low-risk population. Obstet Gynecol 101:626–632; 2003. [DOI] [PubMed] [Google Scholar]
- Mukubo M. Epidemiological study: safety of diagnostic ultrasound during pregnancy on fetus and child development. Ultrasound Med Biol 12:691–693; 1986. [Google Scholar]
- Naumburg E, Bellocco R, Cnattingius S, Hall P, Ekbom A. Prenatal ultrasound examinations and risk of childhood leukaemia: case-control study. BMJ 320:282–283; 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piscaglia F, Bolondi L. Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 32:1369–1375; 2006. [DOI] [PubMed] [Google Scholar]
- Rauschenberg J, Nagel AM, Ladd SC, Theysohn JM, Ladd ME, Moller HE, Trampel R, Turner R, Pohmann R, Scheffler K, Brechmann A, Stadler J, Felder J, Shah NJ, Semmler W. Multicenter study of subjective acceptance during magnetic resonance imaging at 7 and 9.4 T. Invest Radiol 49:249–259; 2014. [DOI] [PubMed] [Google Scholar]
- Roberts DC, Marcelli V, Gillen JS, Carey JP, Della Santina CC, Zee DS. MRI magnetic field stimulates rotational sensors of the brain. Current Biol 21:1635–1640; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi S, Hallett M, Rossini PM, Pascual-Leone A. Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvesen KÅ, Vatten LJ, Jacobsen G, Eik-Nes SH, Økland O, Molne K, Bakketeig LS. Routine ultrasonography in utero and subsequent vision and hearing at primary school age. Ultrasound Obstet. Gynecol 2:243–247; 1992a. [DOI] [PubMed] [Google Scholar]
- Salvesen KÅ, Bakketeig LS, Eik-Nes SH, Undheim JO, Økland O. Routine ultrasonography in utero and school performance at age 8-9 years. Lancet 339:85–89; 1992b. [DOI] [PubMed] [Google Scholar]
- Salvesen KÅ, Jacobsen G, Vatten LJ, Eik-Nes SH, Bakketeig LS. Routine ultrasonography in utero and subsequent growth during childhood. Ultrasound Obstet Gynecol 3:6–10; 1993a. [DOI] [PubMed] [Google Scholar]
- Salvesen KÅ, Vatten LJ, Eik-Nes SH, Hugdahl K, Bakketeig LS. Routine ultrasonography in utero and subsequent handedness and neurological development. BMJ 307:159–164; 1993b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaap K, Christopher-de Vries Y, Mason CK, de Vocht F, Portengen L, Kromhout H. Occupational exposure of healthcare and research staff to static magnetic stray fields from 1.5-7 Tesla MRI scanners is associated with reporting of transient symptoms. Occup Environ Med 71:423–429; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenck JF. Physical interactions of static magnetic fields with living tissues. Prog Biophys Mol Biol 87:185–204; 2005. [DOI] [PubMed] [Google Scholar]
- Schlachetzki F, Hölscher T, Koch HJ, Draganski B, May A, Schuierer G, Bogdahn U. Observation on the integrity of the blood-brain barrier after microbubble destruction by diagnostic transcranial color-coded sonography. J Ultrasound Med 21:419–429; 2002. [DOI] [PubMed] [Google Scholar]
- Shu X-O, Jin F, Linet MS, Zheng W, Clemens J, Mills J, Gao Y-T. Diagnostic x-ray and ultrasound exposure and risk of childhood cancer. Br J Cancer 70:531–536; 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu XO, Potter JD, Linet MS, Severson RK, Han D, Kersey JH, Neglia JP, Trigg ME, Robison LL. Diagnostic x-rays and ultrasound exposure and risk of childhood acute lymphoblastic leukemia by immunophenotype. Cancer Epidemiol Biomarkers Prev 11:177–185; 2002. [PubMed] [Google Scholar]
- Skråstad RB, Eik-Nes SH, Sviggum O, Johansen OJ, Salvesen KÅ, Romundstad PR, Blass HG. A randomized controlled trial of third-trimester routine ultrasound in a non-selected population. Acta Obstet Gynecol Scand 92:1353–1360; 2013. [DOI] [PubMed] [Google Scholar]
- Sorahan T, Lancashire R, Stewart A, Peck I. Pregnancy ultrasound and childhood cancer: A second report from the Oxford Survey of Childhood Cancers. Br J Obstet Gynaecol 102:831–832; 1995. [DOI] [PubMed] [Google Scholar]
- Stålberg K, Haglund B, Axelsson O, Cnattingius S, Pfeifer S, Kieler H. Prenatal ultrasound and the risk of childhood brain tumour and its subtypes. Br J Cancer 98:1285–1287; 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stam R, Bijwaard H. Recent developments in medical techniques involving ionising or non-ionising radiation. Bilthoven: National Institute for Public Health and the Environment; 2011. [Google Scholar]
- Tikkanen J, Heinonen OP. Congenital heart disease in the offspring and maternal habits and home exposures during pregnancy. Teratol 46:447–454; 1992. [DOI] [PubMed] [Google Scholar]
- van der Wouw PA, Brauns AC, Bailey SE, Powers JE, Wilde AAA. Premature ventricular contractions during triggered imaging with ultrasound contrast. J Am Soc Echocardiogr 13:288–294; 2000. [DOI] [PubMed] [Google Scholar]
- Vijayalaxmi, Fatahi M, Speck O. Magnetic resonance imaging (MRI): a review of genetic damage investigations. Mutat Res 764:51–63; 2015. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Static fields. Environmental Health Criteria 232. Geneva: World Health Organization; 2006. [Google Scholar]


