Abstract
Background:
Should the SYNTAX score be integrated in Interventional Cardiology? Should it really be considered as a vital decision-making tool in percutaneous coronary intervention (PCI)? To confirm the importance of this score, we aimed to systematically compare the postinterventional adverse cardiovascular outcomes which were observed in patients who were allotted a low versus a high SYNTAX score.
Methods:
Randomized controlled trials and observational studies which were published from January 2007 to January 2017 were identified from MEDLINE, EMBASE, and the Cochrane databases using the searched terms ‘SYNTAX score and percutaneous coronary intervention.’ Adverse cardiovascular outcomes were considered as the major endpoints. Risk ratios (RRs) with 95% confidence intervals (CIs) were used as the statistical parameters, and the main analysis was carried out by the RevMan 5.3 software.
Results:
Sixteen studies with a total number of 19,751 participants (8589 participants with a low versus 11,162 participants with a high SYNTAX score) were included. Current results showed mortality to be significantly higher with a higher SYNTAX score (RR 2.09, 95% CI 1.78–2.46, P = .00001). Cardiac death also significantly favored a low SYNTAX score (RR 2.08, 95% CI 1.66–2.61, P = .00001. Similarly, myocardial infarction, major adverse cardiac events, repeated revascularization, and stent thrombosis were significantly higher following a high SYNTAX score (RR 1.71, 95% CI 1.45–2.03, P = .00001; RR 2.03, 95% CI 1.81–2.26, P = .00001; RR 1.96, 95% CI 1.69–2.28, P = .00001; and RR 3.16, 95% CI 2.17–4.59, P = .00001, respectively). Even when patients with ST-segment elevation myocardial infarction were separately analyzed, a low SYNTAX score was still significantly associated with lower adverse outcomes.
Conclusions:
This analysis is a confirmatory piece of evidence to show that the application of the SYNTAX score in Interventional Cardiology is apparently relevant. The use of this scoring system to grade patients with coronary artery disease and to further guide for revascularization should be encouraged.
Keywords: coronary artery disease, interventional cardiology, percutaneous coronary intervention, SYNTAX score
1. Introduction
What is Interventional Cardiology? It might be defined as a branch of cardiology which focuses specifically on the treatment and management of structural heart diseases in catheter-based laboratories. The current status, new updates, and future directions related to Interventional cardiology have recently been published.[1–4] Interventional procedures are becoming increasingly common and they are now becoming the preferred modes of treatment among patients with specific cardiac disorders. Percutaneous coronary intervention (PCI), which is often associated with earlier hospital discharge,[5] is 1 among the most common interventional procedures which are carried out in PCI-capable centers. Management of acute coronary syndrome (ACS) including ST-segment elevation myocardial infarction (STEMI) and non-STEMI,[6] and also several types of nonsevere multivessel coronary artery diseases (MVCADs),[7] and unprotected left main coronary artery diseases (ULMCAD) is nowadays possible with PCI.[8] Even though PCI might be an acceptable choice in most of the patients, certain patients’ conditions and the extent of coronary lesions might restrict its use, thereby shifting its place to coronary artery bypass surgery (CABG).[9]
However, the question which has to be raised at this particular point concerns the identification of patients who might benefit from PCI. Recently, the Synergy Between PCI With Taxus and CABG (SYNTAX) score was developed.[10] It is a tool which takes into consideration the anatomical features of the coronary lesions as a guide to assess patients who will be eligible for PCI.[11]
Nevertheless, should the SYNTAX score be integrated in Interventional Cardiology? Should it really be considered as a vital decision-making tool in PCI? To confirm the importance of this score, we aimed to systematically compare the postinterventional adverse cardiovascular outcomes which were observed in patients who were allotted a low versus a high SYNTAX score.
2. Methods
2.1. Searched databases and strategies
Following the PRISMA guideline,[12] randomized controlled trials and observational studies published from January 2007 to January 2017 were identified through MEDLINE, EMBASE, and the Cochrane databases using the searched terms or keywords which were listed below:
-
1.
SYNTAX score
-
2.
SYNTAX score and percutaneous coronary intervention
-
3.
SYNTAX score and interventional cardiology
-
4.
SYNTAX score and coronary angioplasty
-
5.
SYNTAX score and PCI
-
6.
SYNTAX score and coronary artery disease (CAD)
-
7.
SYNTAX score and coronary stenting
It should be noted that the reference lists of suitable publications were also checked for relevant articles.
Our searched criteria were limited to English publications involving humans only.
2.2. Inclusion criteria
Studies were included if they met the following criteria:
-
1.
They were randomized trials or observational cohorts comparing PCI in patients who were allotted a low versus a high SYNTAX score.
-
2.
They reported adverse clinical outcomes as their major endpoints.
-
3.
They included any type of participants with CAD.
2.3. Exclusion criteria
Studies were excluded based on the following criteria:
-
1.
They were meta-analysis, case-control studies, or letters to editors.
-
2.
They compared only CABG in patients who were allotted a low versus a high SYNTAX score.
-
3.
They did not report adverse clinical outcomes as their major endpoints.
-
4.
They were duplicated studies or they were different studies which involved the same trial.
2.4. Types of participants, outcomes, and follow-ups
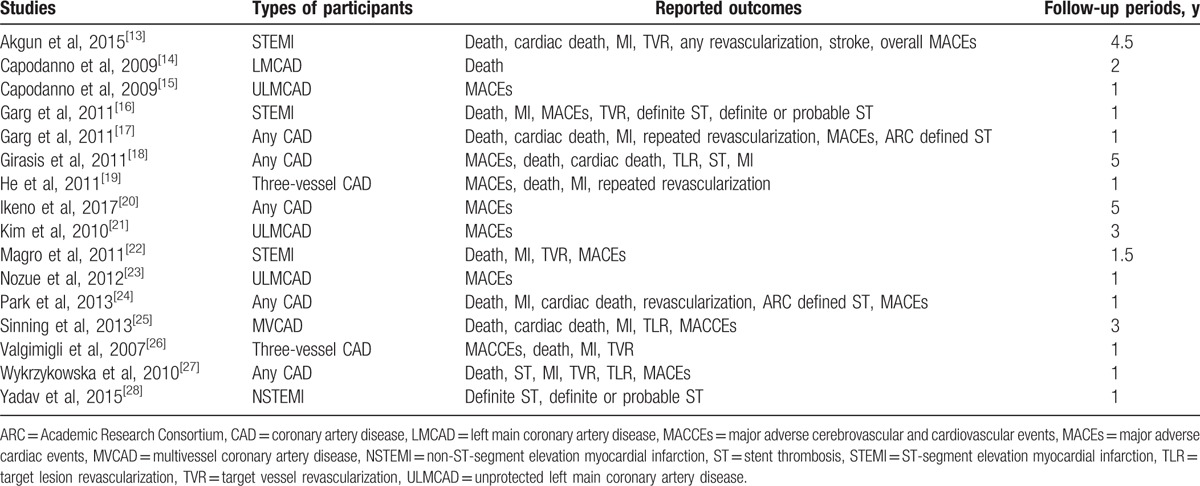
This research article included several types of patients with CAD who were revascularized by PCI. The different types of participants (Table 1) were patients with any type of CAD; ST-segment elevation MI (STEMI); non-ST-segment elevation MI (NSTEMI); left main CAD (LMCAD); MVCAD; and three-vessel CAD.
Table 1.
Type of participants, reported outcomes, and follow-ups.
The outcomes which were assessed included the following:
-
1.
All-cause mortality.
-
2.
Cardiac death.
-
3.
Myocardial infarction (MI).
-
4.
Major adverse cardiac events (MACEs), which were defined as the combination of death, MI, and revascularization. Major adverse cerebrovascular and cardiovascular events (MACCEs), which consisted of death, MI, stroke, and revascularization, were also included in the same category as MACEs and analyzed together.
-
5.
Repeated revascularization which consisted of target vessel revascularization (TVR) and/or target lesion revascularization (TLR).
-
6.
Stent thrombosis (ST), which was defined according to the Academic Research Consortium (ARC)[29] and which was composed of definite and probable ST.
The follow-up periods varied from study to study. Most of the studies had a follow-up period of 1 year, as shown in Table 1.
2.5. Definitions
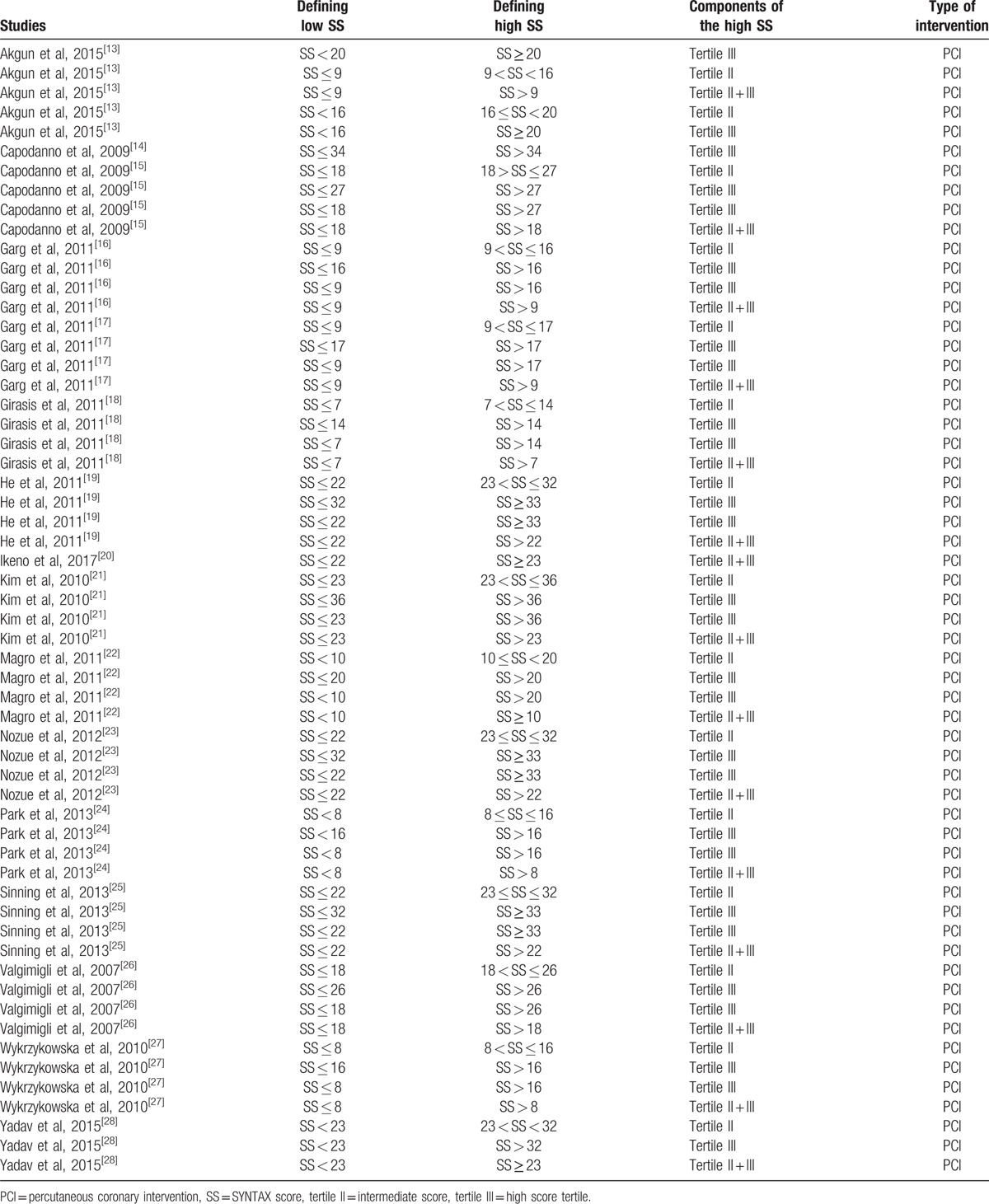
The SYNTAX score was classified into 3 different categories known as tertiles, as given below:
-
1.
Tertile I was defined as patients with the lowest SYNTAX score.
-
2.
Tertile II was defined as patients with an intermediate/mid SYNTAX score.
-
3.
Tertile III was defined as patients with the highest SYNTAX score.
This information has been represented in Table 2.
Table 2.
Definitions of low versus high SYNTAX score (the different tertiles).
2.6. Data extraction and quality assessment
Studies which were considered eligible for this analysis were first of all carefully assessed by 3 independent reviewers (P.K.B., Y.S., and A.B.) to ensure that they satisfied the eligibility criteria of this research article.
The following data were extracted by the same 3 reviewers:
-
1.
Names of the first author
-
2.
Year of publication
-
3.
Types of study which were reported
-
4.
Periods of participants’ enrollment
-
5.
Types of participants which were included
-
6.
Baseline characteristics of the participants (including the mean age, percentage of male participants, percentage of participants suffering from comorbidities such as hypertension, dyslipidemia, and diabetes mellitus)
-
7.
Total number of participants who were allotted a low SYNTAX score
-
8.
Total number of participants who were allotted a higher SYNTAX score
-
9.
The different tertiles (tertiles I, II, and III)
-
10.
The clinical outcomes and the number of events which were reported within the study and the control groups, respectively
-
11.
The follow-up periods
-
12.
The interventional procedures which were followed
-
13.
Details about the quality of the trials and observational studies
Quality assessment was carried out separately for the trials and the observational cohorts using the Cochrane Handbook[30] and the Newcastle Ottawa Scale (NOS),[31] respectively. The trials were assessed for the 6 components which were recommended by the Cochrane Collaborations, whereby scores were given in accordance to a low, unclear and high risk of bias, and the total score which was obtained by each trial was graded from A to E, whereby A implied a very low risk of bias, B and C implied low to moderate risk of bias, and E indicated a very high risk of bias.
For the observational studies, a star system assessment was carried out whereby stars were allotted based on certain components which were required during quality assessment. A maximum total number of 9 stars were possible which implied a very low risk of bias.
Any disagreement which followed whether during the data extraction process or the quality assessment was discussed among the reviewers. However, if a consensus could not be reached, a decision was finalized by the fourth reviewer (F.H.).
2.7. Statistical analysis
This is a meta-analysis of several studies, including different types of patients who underwent revascularization by PCI. Therefore, inconsistency across the studies was possible. To obtain a more consistent result, heterogeneity[32] across the studies was calculated/evaluated/assessed using the Q statistic test (P ≤ .05 was considered statistically significant) and the I2 statistic test (high percentage = higher heterogeneity [whereby a random-effects model was used if a value greater than 50% was obtained] and low percentage = lower heterogeneity [whereby a fixed-effects model was used if a value equal to or less than 50% was obtained]).
The analysis was carried out whereby risk ratios (RRs) with 95% confidence intervals (CIs) were calculated by the RevMan version 5.3 software.
Sensitivity analysis was also carried out by excluding each study one by one and observing any significant difference in subgroup analysis in comparison to the main results.
In addition, publication bias,[32] which was also possible across the studies, was visually estimated by assessing graphical plots through RevMan 5.3.
2.8. Ethical approval
Ethical or board review approval and patients’ consents were not required for meta-analyses.
3. Results
3.1. Searched outcomes
A careful search through the electronic databases which was carried out by those 3 reviewers resulted in a total number of 1147 articles as listed below:
-
1.
MEDLINE: 401 articles
-
2.
EMBASE: 423 articles
-
3.
Cochrane database: 234 articles
-
4.
Reference lists of relevant articles: 89 articles
The 3 reviewers carefully assessed the titles and abstracts. Based on this assessment, 1004 articles were eliminated since they were not considered relevant to the scope of this research.
In all, 143 full-text articles were assessed for eligibility. Further articles were eliminated due to the following reasons:
-
1.
They were meta-analysis, case-control studies, and letters to editors (n = 4).
-
2.
They only compared adverse outcomes in patients who were revascularized by PCI with a low SYNTAX score versus CABG with a high SYNTAX score (n = 12).
-
3.
They only compared CABG patients who were allotted a low versus a high SYNTAX score (n = 8).
-
4.
They were duplicated studies or they were different studies which were associated with similar trials (n = 103).
Finally, only 16 full-text articles[13–28] (6 randomized trials and 10 observational studies) were selected for this analysis as shown in Fig. 1.
Figure 1.
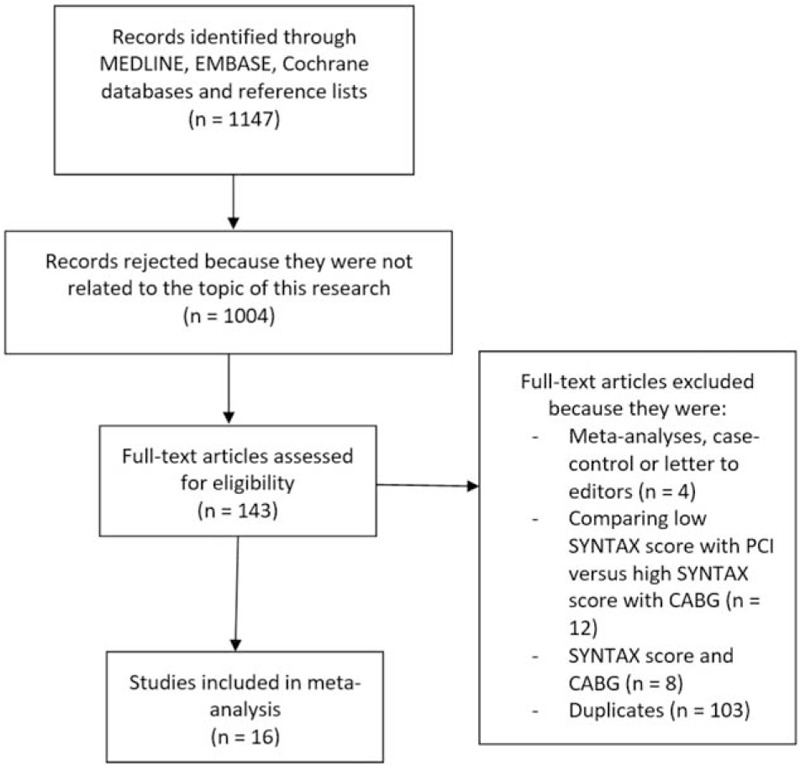
Flow diagram which represents the study selection.
3.2. General features of the studies
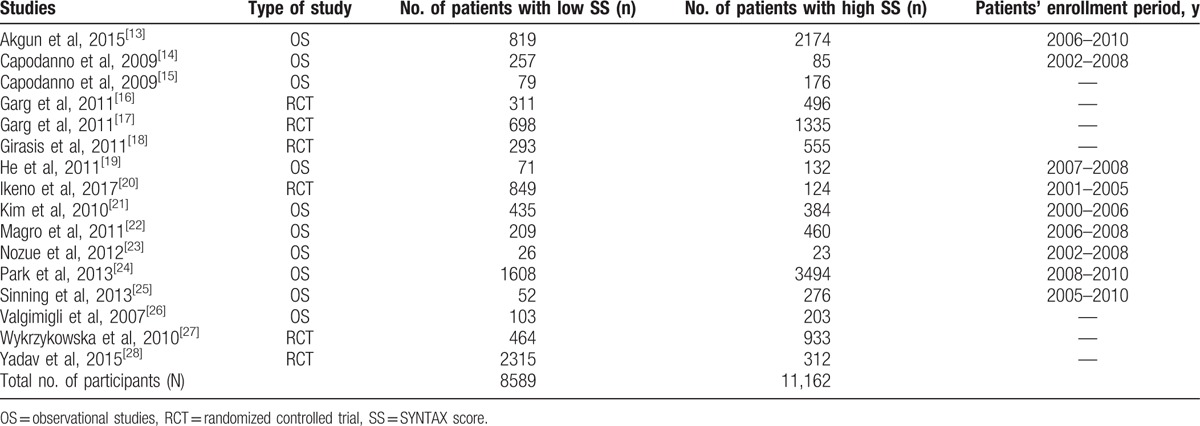
Six randomized trials and 10 observational cohorts with a total number of 19,751 participants (8589 participants with a low SYNTAX score versus 11,162 participants with a high SYNTAX score) were included in the main analysis. Patients’ enrollment periods varied from the years 2000 to 2010 as shown in Table 3.
Table 3.
General features of the studies which were included.
After the quality assessment, a grade B was allotted to the trials, whereas number of stars allotted to the observational studies varied from 6 to 8 stars.
3.3. Baseline features of the participants
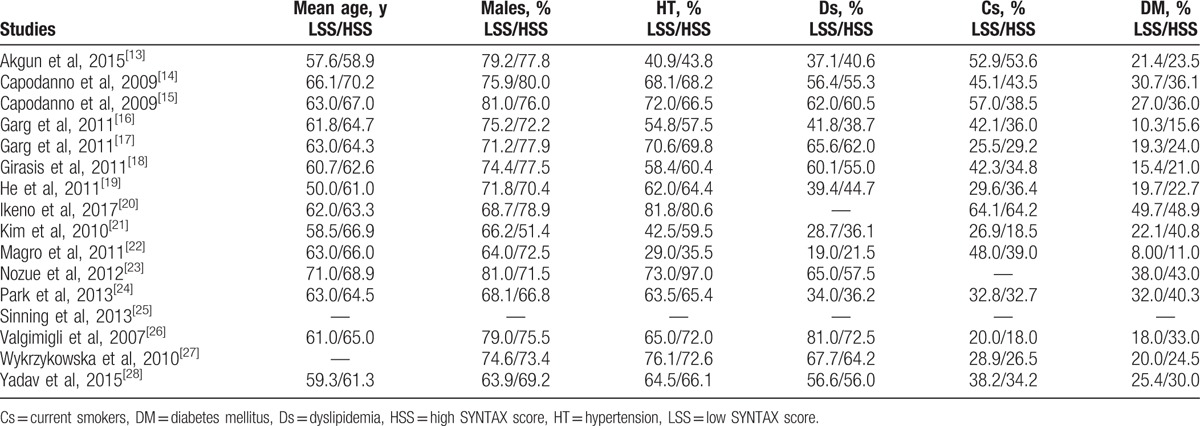
The baseline characteristics of the participants were summarized in Table 4. A mean age ranging from 50.0 to 71.0 years was noted among the participants. Most of the studies reported a majority of male compared with female participants as shown in Table 4. The percentage of participants with hypertension, dyslipidemia, current smoking, and those who suffered from type 2 diabetes mellitus were also listed in Table 4. According to the baseline features, almost no significant differences were observed among participants within the low SYNTAX and high SYNTAX groups, with the exception of a few studies.
Table 4.
Baseline features (for the participants with a low vs a higher SYNTAX score).
3.4. Main results of this analysis
The results were subdivided into different categories, as described in the following subsections.
3.4.1. Low SYNTAX score versus higher SYNTAX score (tertile II + III)
First of all, after PCI, adverse cardiovascular outcomes associated with a low SYNTAX score was compared with adverse outcomes associated with a higher SYNTAX score (tertile II + III).
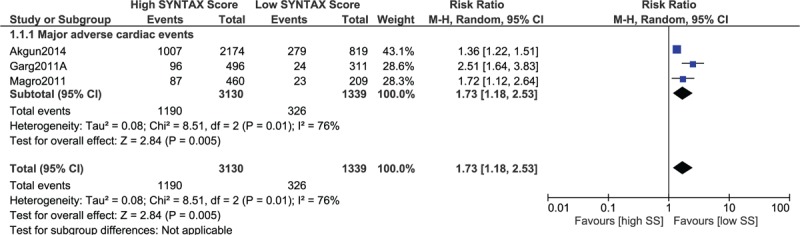
The current results showed mortality to be significantly higher with the higher SYNTAX score (RR 2.09, 95% CI 1.78–2.46, P = .00001, as shown in Fig. 2). Cardiac death also significantly favored a low SYNTAX score (RR 2.08, 95% CI 1.66–2.61, P = .00001). Similarly, MI, MACEs, repeated revascularization, and stent thrombosis were significantly higher with a high SYNTAX score (RR 1.71, 95% CI 1.45–2.03, P = .00001; RR 2.03, 95% CI 1.81–2.26, P = .00001; RR 1.96, 95% CI 1.69–2.28, P = .00001; and RR 3.16, 95% CI 2.17–4.59, P = .00001, respectively, as shown in Fig. 2).
Figure 2.
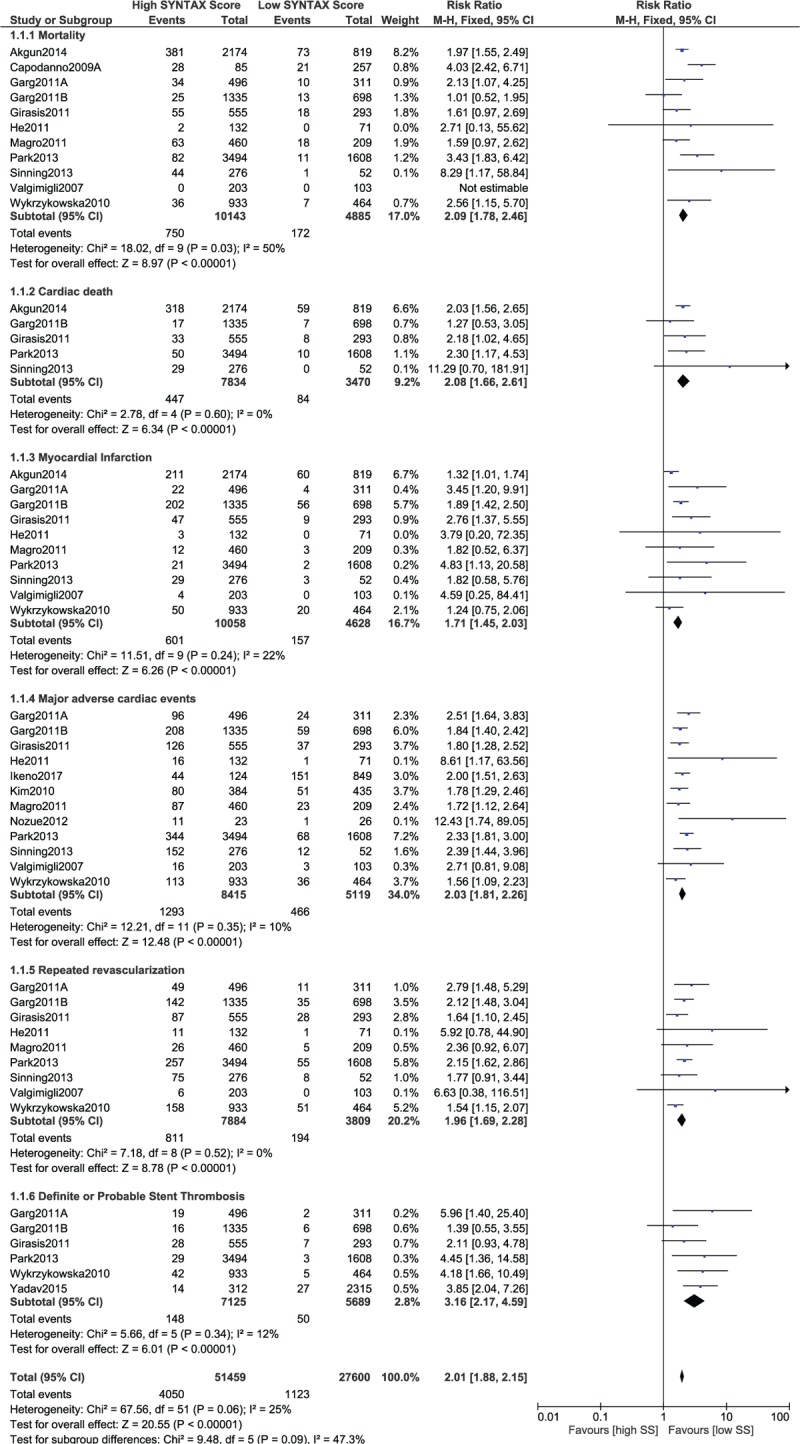
Postinterventional adverse cardiovascular outcomes which were observed between a low versus a higher (tertiles II and III) SYNTAX score.
It should be noted that while carrying out this analysis, data which were obtained from observational studies were combined with data which were obtained from randomized controlled trials. Therefore, another analysis was separately carried out involving only data which were obtained from randomized trials to observe any change in the results. However, similar to the previous results, this separate analysis also showed that significantly higher mortality, cardiac death, MI, MACEs, repeated revascularization, and stent thrombosis were observed with a high SYNTAX score (RR 1.69, 95% CI 1.23–2.32, P = .001; RR 1.75, 95% CI 0.99–3.10, P = .05; RR 1.89, 95% CI 1.51–2.37, P = .00001; RR 1.88, 95% CI 1.63–2.18, P = .00001; RR 1.83, 95% CI 1.51–2.21, P = .00001; and RR 2.99, 95% CI 2.02–4.43, P = .00001, respectively, as shown in Fig. 3).
Figure 3.
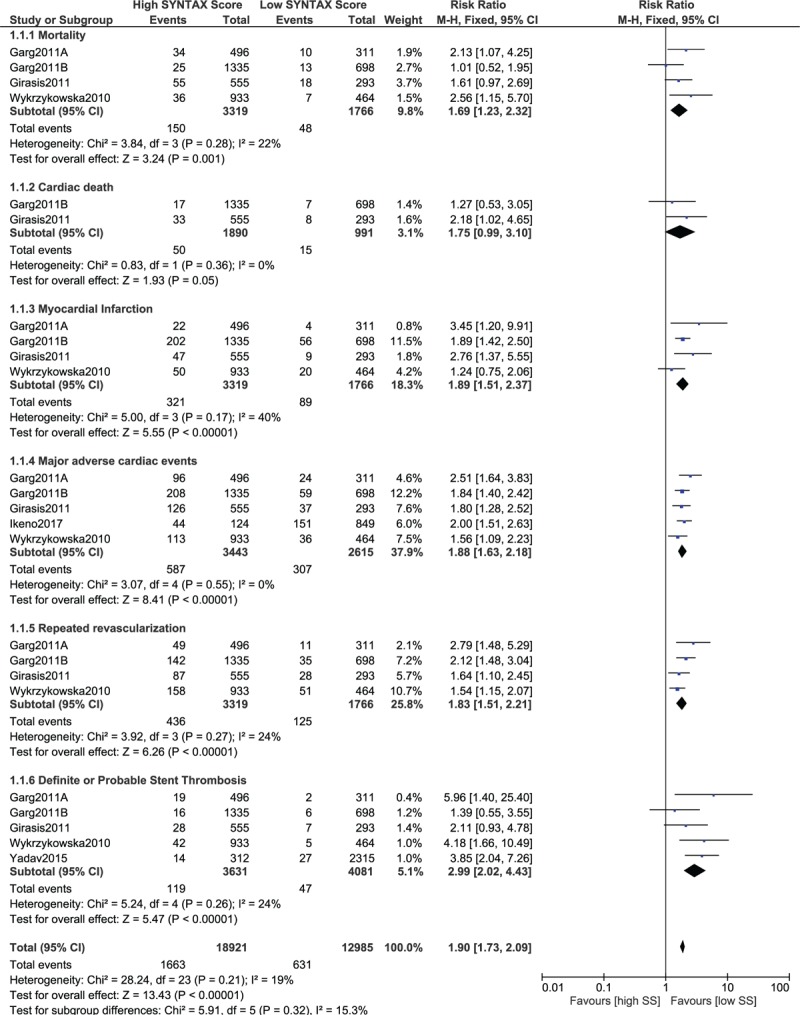
Postinterventional adverse cardiovascular outcomes which were observed between a low versus a higher (tertiles II and III) SYNTAX score using data which were obtained only from randomized controlled trials.
3.4.2. Low SYNTAX score versus higher SYNTAX score (tertile II + III) with specific limits/ranges of score
The score range was completely omitted in the above-shown analysis. A low SYNTAX score with any range was compared with the corresponding higher score. However, the analysis was further divided into several subsets with different score limits.
When the adverse outcomes were compared in patients who were allotted a low SYNTAX score of ≤10 versus a higher score, significantly higher mortality, MI, MACEs, repeated revascularization, and stent thrombosis were still associated with the higher score (RR 1.78, 95% CI 1.50–2.12, P = .00001; RR 1.96, 95% CI 1.57–2.43, P = .00001; RR 1.98, 95% CI 1.73–2.26, P = .00001; RR 1.94, 95% CI 1.66–2.27, P = .00001; and RR 3.01, 95% CI 1.94–4.67, P = .00001, respectively, as shown in Fig. 4).
Figure 4.
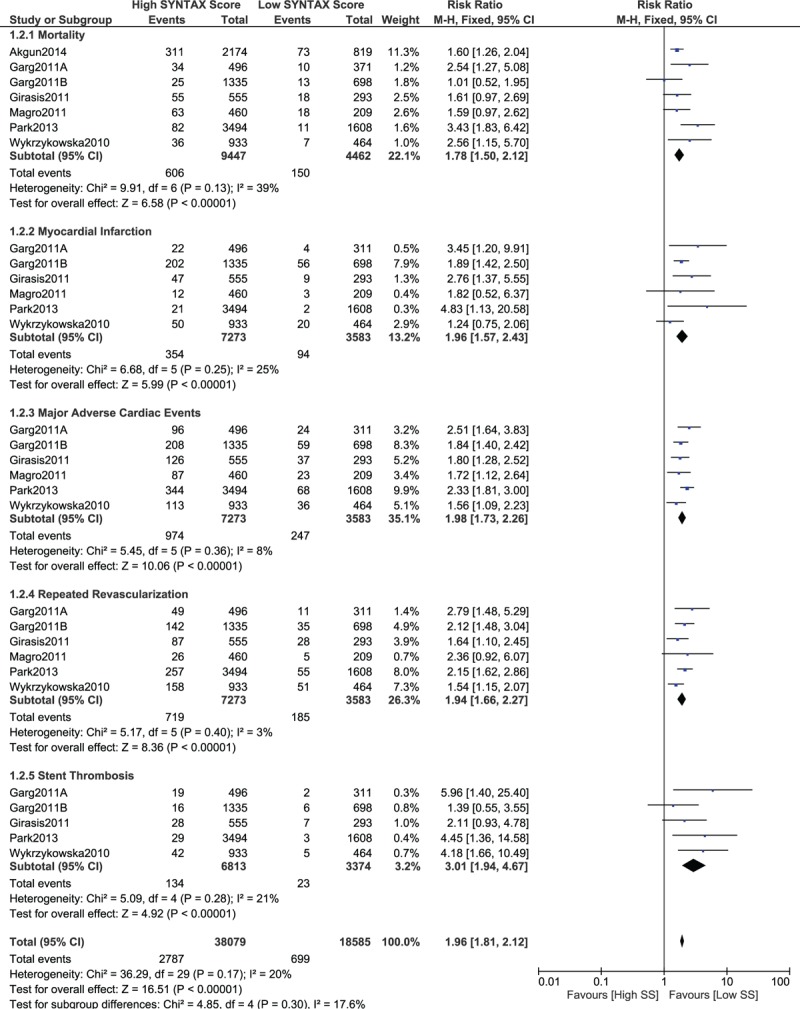
Postinterventional adverse cardiovascular outcomes which were observed between a low (SS ≤ 10) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
When a lower SYNTAX score 10 > SYNTAX score ≤ 20 was considered as the lower score range, mortality, MI and MACEs still significantly favored the lower score (RR 2.12, 95% CI 1.85–2.42, P = .00001; RR 1.68, 95% CI 1.46–1.93, P = .00001; and RR 2.02, 95% CI 1.82–2.23, P = .00001, respectively, as shown in Fig. 5). In addition, repeated revascularization and stent thrombosis were also significantly in favor of a lower SYNTAX score (RR 2.03, 95% CI 1.57–2.64, P = .00001 and RR 2.56, 95% CI 1.46–4.48, P = .001, respectively, as shown in Fig. 6).
Figure 5.
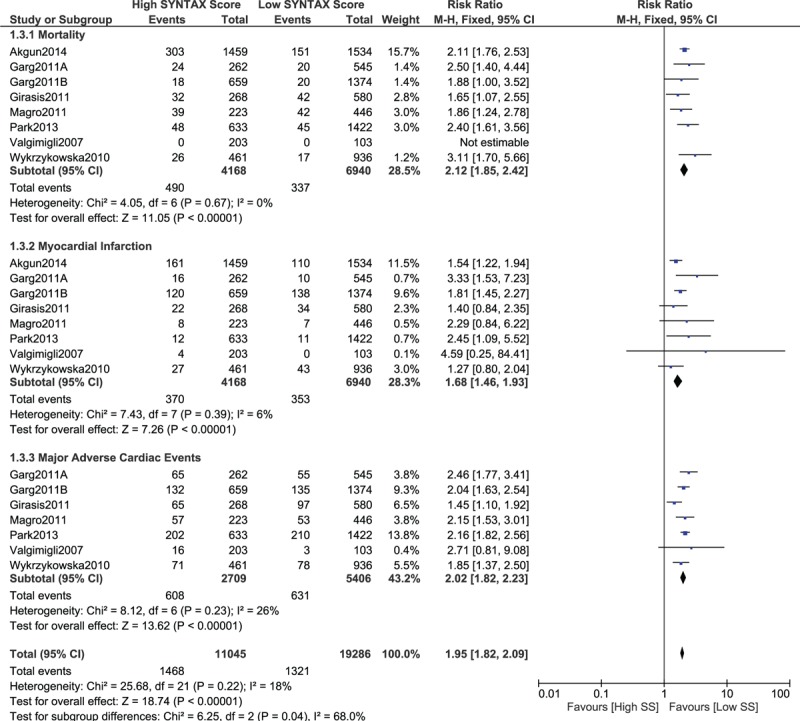
Postinterventional adverse cardiovascular outcomes which were observed between a low (10 > SS ≤ 20) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
Figure 6.
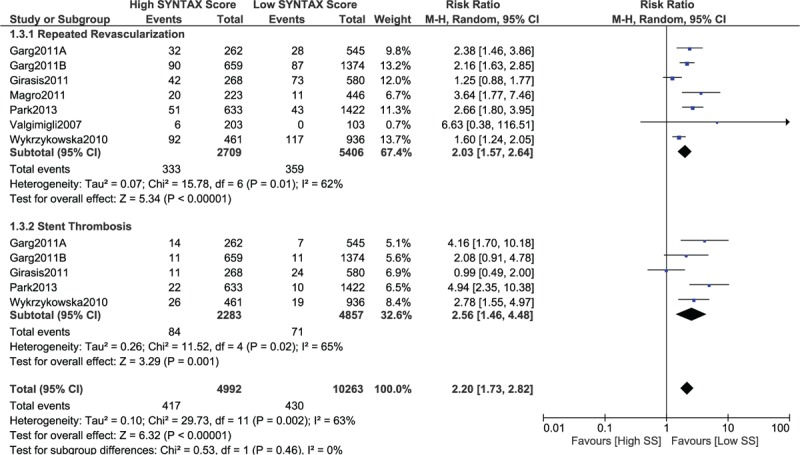
Postinterventional adverse cardiovascular outcomes which were observed between a low (10 > SS ≤ 20) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
When a score range 20 > SYNTAX score < 30 was considered for a low SYNTAX score, mortality, MI, MACEs, and repeated revascularization were still significantly higher (RR 6.74, 95% CI 1.28–35.33, P = .02; RR 2.63, 95% CI 1.42–4.85, P = .002; RR 2.18, 95% CI 1.80–2.65, P = .00001; and RR 2.50, 95% CI 1.39–4.49, P = .002, respectively, as shown in Fig. 7).
Figure 7.
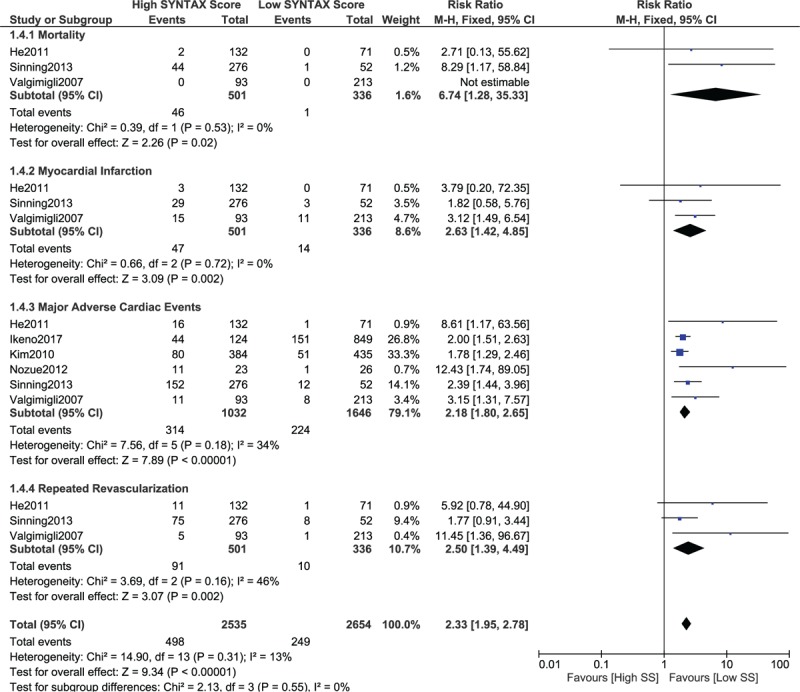
Postinterventional adverse cardiovascular outcomes which were observed between a low (20 > SS < 30) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
When a score range 30 > SYNTAX score < 40 was considered in the lower SYNTAX range, mortality and MI were still significantly higher with a high SYNTAX score (RR 3.34, 95% CI 2.26–4.93, P = .00001 and RR 2.03, 95% CI 1.06–3.89, P = .03, respectively; Fig. 8). In addition, MACEs were also significantly higher with a high SYNTAX score (RR 1.72, 95% CI 1.07–2.77, P = .02; Fig. 9).
Figure 8.
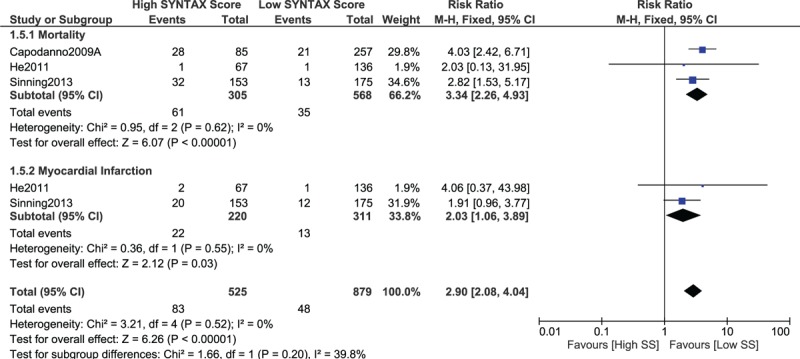
Postinterventional adverse cardiovascular outcomes which were observed between a low (30 > SS < 40) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
Figure 9.
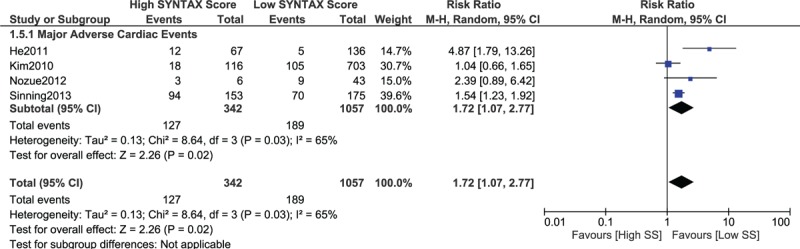
Postinterventional adverse cardiovascular outcomes which were observed between a low (30 > SS < 40) versus a higher (tertiles II and III) SYNTAX score. SS = SYNTAX score.
3.4.3. Low versus intermediate SYNTAX score (tertile I vs tertile II)
When a low SYNTAX score was compared with an intermediate SYNTAX score, mortality, MI, MACEs, repeated revascularization, and stent thrombosis were still significantly lower with a lower SYNTAX score (RR 1.36, 95% CI 1.10–1.67, P = .004; RR 1.40, 95% CI 1.15–1.71, P = .0009; RR 1.52, 95% CI 1.34–1.72, P = .00001; RR 1.57, 95% CI 1.32–1.86, P = .00001; and RR 2.12, 95% CI 1.30–3.47, P = .003, respectively, as shown in Fig. 10).
Figure 10.
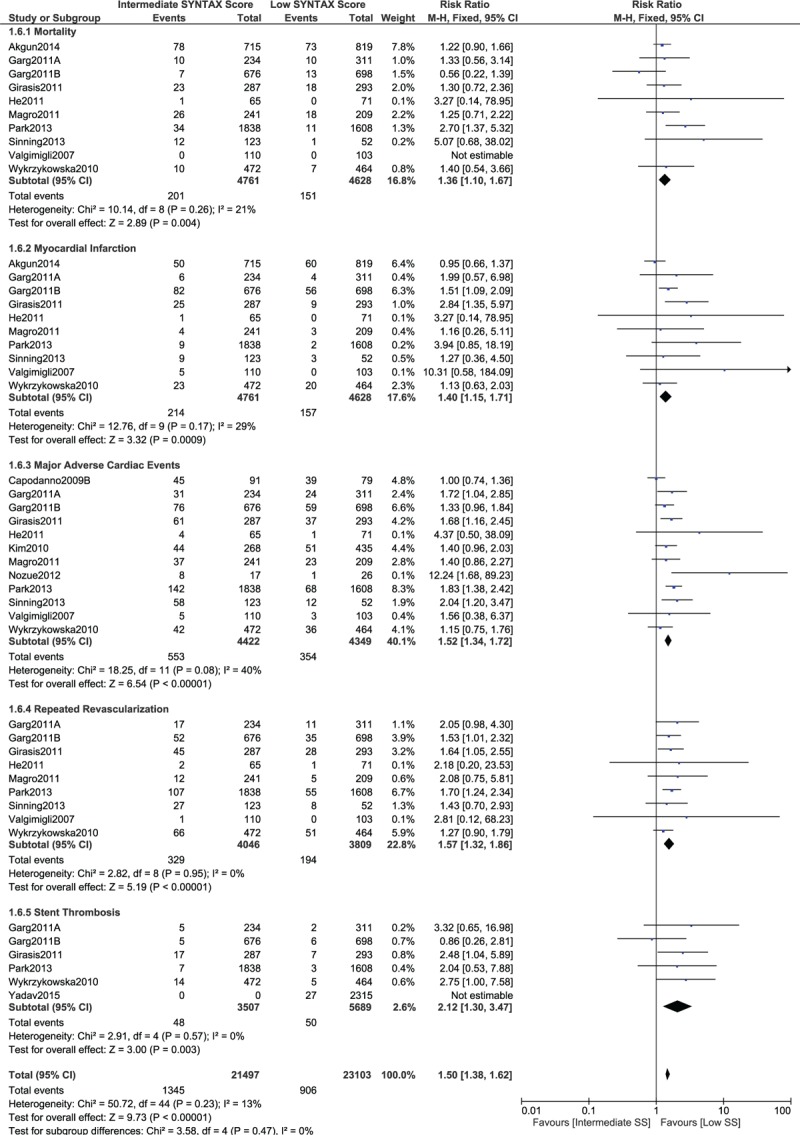
Postinterventional adverse cardiovascular outcomes which were observed between a low versus an intermediate (tertile II) SYNTAX score.
3.4.4. Low versus high SYNTAX score (tertile I vs tertile III)
When a low SYNTAX score was compared with a high SYNTAX score, mortality, cardiac death, MI, MACEs, repeated revascularization, and stent thrombosis significantly favored a lower score (RR 2.86, 95% CI 2.42–3.39, P = .00001; RR 2.91, 95% CI 2.29–3.70, P = .00001; RR 2.18, 95% CI 1.82–2.61, P = .00001; RR 2.34, 95% CI 2.09–2.61, P = .00001; RR 2.37, 95% CI 2.02–2.78, P = .00001; and RR 4.09, 95% CI 2.67–6.27, P = .00001, respectively, as shown in Fig. 11).
Figure 11.
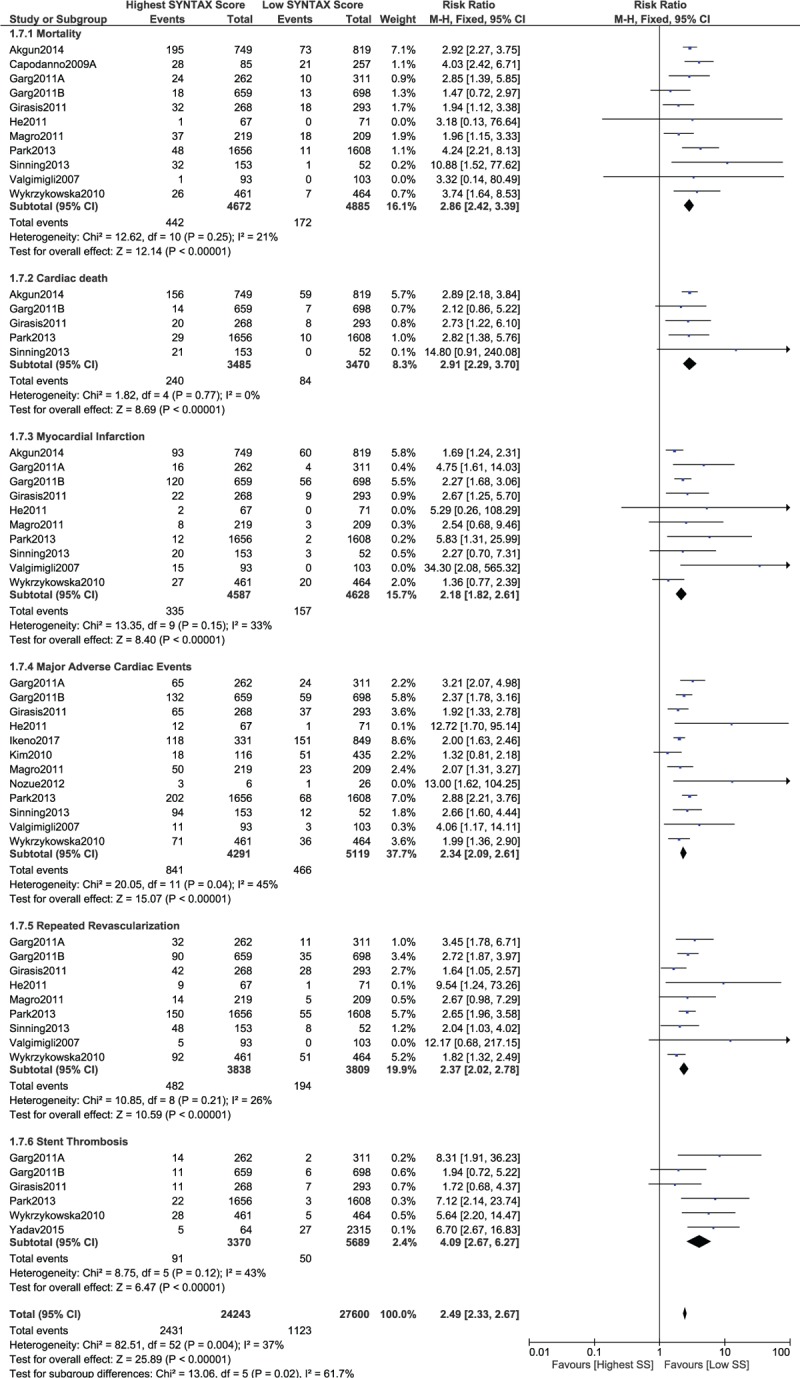
Postinterventional adverse cardiovascular outcomes which were observed between a low versus a high (tertile III) SYNTAX score.
3.4.5. Low versus higher SYNTAX score (tertile II + III) in a subset of patients with STEMI
A separate analysis was carried out involving only patients with STEMI. The results were still in favor of a low SYNTAX score, whereby mortality and MI were significantly lower in STEMI patients with a low SYNTAX score (RR 1.92, 95% CI 1.56–2.35, P = .00001 and RR 1.45, 95% CI 1.12–1.88, P = .005, respectively; Fig. 12). In addition, MACEs also significantly favored a low SYNTAX score in these patients with STEMI (RR 1.73, 95% CI 1.18–2.53, P = .005; Fig. 13).
Figure 12.
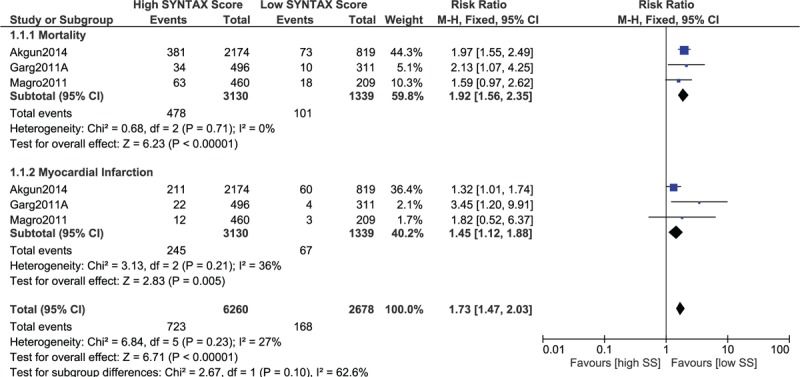
Postinterventional adverse cardiovascular outcomes which were observed between a low versus a higher (tertile II + III) SYNTAX score in patients with STEMI. STEMI = ST-segment elevation myocardial infarction.
Figure 13.
Postinterventional major adverse cardiac events which were observed between a low versus a higher (tertile II + III) SYNTAX score in patients with STEMI. STEMI = ST-segment elevation myocardial infarction.
3.5. Publication bias
Sensitivity analysis did not show any deviation from these main results. Moreover, based on a visual evaluation of the funnel plots, there has been very little evidence for the existence of publication bias across all the eligible studies which were involved in assessing the relevant cardiovascular outcomes (Figs. 14 and 15).
Figure 14.
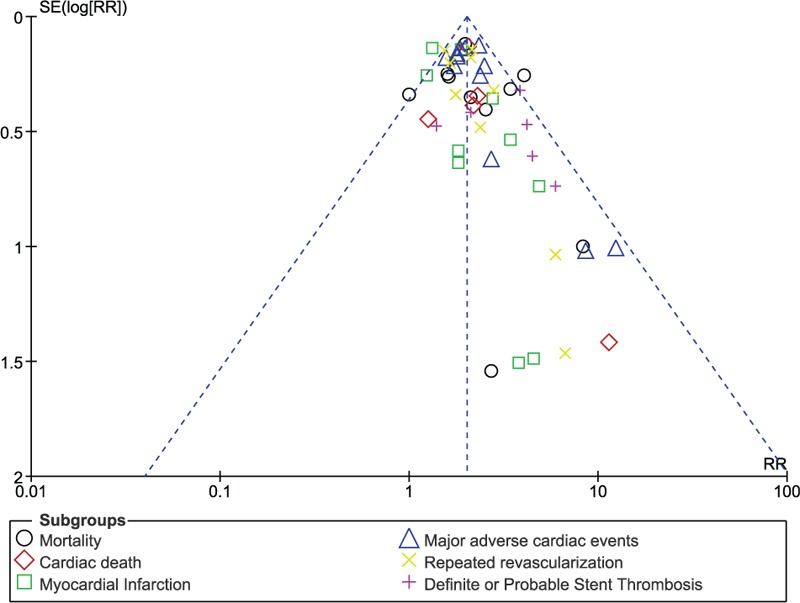
Funnel plot (A) representing publication bias.
Figure 15.
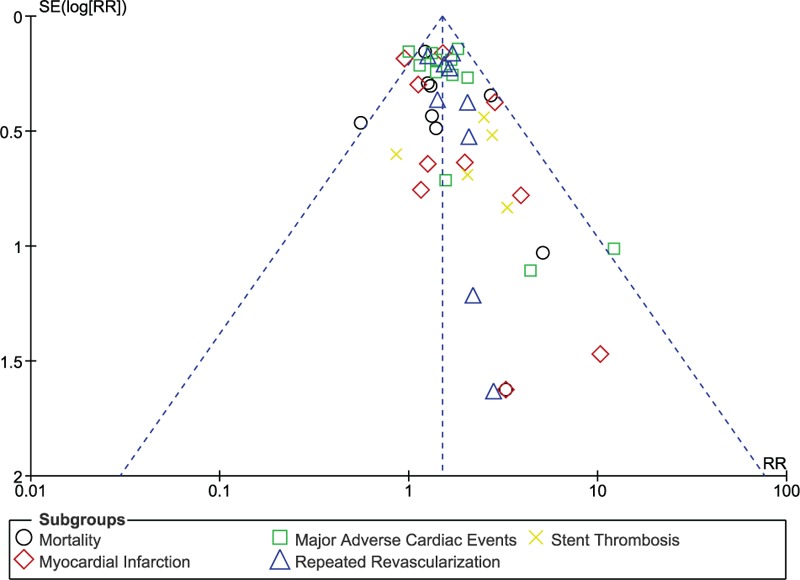
Funnel plot (B) representing publication bias.
4. Discussion
Even if the SYNTAX score is not among the newest angiographic tools which have been used in clinical practice, it was the most common one to be used to stratify patients who would benefit from either PCI or CABG until recently, newer scientific reports showed its application in Interventional cardiology, whereby it could potentially stratify those patients who would most probably benefit from PCI alone.
In this analysis, we demonstrated the potential benefits of the SYNTAX score and its potential application in Interventional cardiology. These current results showed that when a low SYNTAX score was compared with an intermediate or higher SYNTAX score, significantly lower adverse cardiovascular outcomes were associated with the lower score. A consistent result was obtained among all the subgroups. This analysis included patients with STEMI, NSTEMI, ULMCAD, and MVCAD. However, even when patients with STEMI were separately analyzed, a low SYNTAX score was still significantly associated with lower adverse outcomes.
A subanalysis of the shinshu prospective multicenter study of elderly patients with coronary artery disease undergoing percutaneous coronary intervention registry also supported the results of this current analysis showing that a lower SYNTAX score predicted a lower incidence of MACEs.[33] The authors also stated that the SYNTAX score should be considered an important parameter to improve risk stratification in similar patients. Even if the study satisfied most of the eligibility criteria for this analysis, it was not included among the eligible studies because the patients also suffered from heart failure.
The gene polymorphism, platelet reactivity, and the syntax score study,[34] which was a prospective, multicentered cohort including 1053 patients with NSTEMI who underwent coronary revascularization by PCI, and who were treated with clopidogrel after this invasive procedure, showed higher platelet reactivity to be independently associated with an increased risk of MACEs only in patients with a high SYNTAX score. This association was not visible in patients with lower SYNTAX scores.
In addition, a recently published meta-analysis also showed a positive aspect of the SYNTAX score in predicting all-cause mortality in patients who were treated by PCI, indicating its importance in Interventional cardiology.[35] However, in this same analysis, the authors stated that the SYNTAX score often overestimated the risk of MACEs. However, in this current analysis, MACEs, which are among the vital clinical endpoints in Interventional cardiology,[36] were not overestimated.
Nevertheless, it should be noted that this current analysis has almost all the features that are required to be considered a well-carried out meta-analysis in terms of the total number of studies and participants, low bias risks across the studies, low levels of heterogeneity in almost all the subgroups, and well-presented robust results. Therefore, the SYNTAX score should be expected to at least be integrated in Interventional cardiology, despite emerging newer clinical tools,[37–39] which should but might take longer to find a place in Interventional cardiology.
4.1. Novelty
New features in this analysis include the following:
-
1.
A new idea in Interventional cardiology.
-
2.
An important potential tool has been studied.
-
3.
This meta-analysis might be among the first analyses demonstrating the use of this new tool in Interventional cardiology.
-
4.
A large number of participants who underwent revascularization by PCI were included.
-
5.
Low SYNTAX score was compared with higher (tertiles II and III) SYNTAX score.
-
6.
Low SYNTAX score was compared with intermediate (tertile II) SYNTAX score.
-
7.
Low SYNTAX score was compared with high (tertile III) SYNTAX score.
-
8.
Different range limits of SYNTAX score were also compared.
-
9.
Randomized trials were also separately analyzed.
-
10.
Several adverse cardiovascular outcomes were analyzed.
-
11.
Patients who suffered from STEMI were also separately analyzed to show a result specifically for this particular subgroup of patients.
4.2. Limitations
The limitations of this study were as follows:
-
1.
Different studies reported different follow-up periods which might have influenced the result. However, most of the studies reported a follow-up period of 1 year only.
-
2.
Several types of patients with CAD were analyzed together. However, when patients with STEMI were separately analyzed, the same results were obtained.
-
3.
Data obtained from observational studies and randomized trials were combined and analyzed. However, even when randomized trials were separately analyzed, a similar result was obtained, partly solving this limitation.
-
4.
The range limit of the scores was not exactly the same; small variations might have been responsible for the moderate level of heterogeneity observed in certain subgroups.
5. Conclusions
This analysis is a confirmatory piece of evidence to show that the application of the SYNTAX score in Interventional cardiology is apparently relevant. A low SYNTAX score was associated with significantly better cardiovascular outcomes in comparison with a higher SYNTAX score. Therefore, the SYNTAX score is an angiographic tool which might possibly be of some importance and should be applied in clinical practice.
Footnotes
Abbreviations: CABG = coronary artery bypass surgery, CAD = coronary artery disease, MACEs = major adverse cardiac events, PCI = percutaneous coronary intervention, RR = risk ratios, STEMI = ST-segment elevation myocardial infarction.
Authors’ contributions: P.K.B., Y.S., A.B., and F.H. were responsible for the conception and design, acquisition of data, analysis and interpretation of data, drafting the initial manuscript, and revising it critically for important intellectual content. P.K.B. wrote the final manuscript. All authors read and approved the final manuscript.
Funding: This research was supported by National Natural Science Foundation of China (No. 81560046), Scientific Project of Guangxi Higher Education (No. KY2015ZD028), and the Youth Science Foundation of Guangxi Medical University (No. GXMUYSF201308).
The authors declare no competing interests.
References
- [1].Lüscher TF. Update on interventional cardiology: outcome according to stent type and implantation technique. Eur Heart J 2016;37:3359–61. [DOI] [PubMed] [Google Scholar]
- [2].Jiménez-Quevedo P, Serrador A, Pérez de Prado A, et al. Spanish Cardiac Catheterization and Coronary Intervention Registry. 25th Official Report of the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology (1990-2015). Rev Esp Cardiol (Engl Ed) 2016;69:1180–9. [DOI] [PubMed] [Google Scholar]
- [3].Mehta RM, Agarwal M, Ifedili I, et al. Procedural variations in performing primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. Curr Probl Cardiol 2017;42:46–60. [DOI] [PubMed] [Google Scholar]
- [4].Faxon DP, Williams DO. Interventional cardiology: current status and future directions in coronary disease and valvular heart disease. Circulation 2016;133:2697–711. [DOI] [PubMed] [Google Scholar]
- [5].Bundhun PK, Soogund MZ, Huang WQ. Same day discharge versus overnight stay in the hospital following percutaneous coronary intervention in patients with stable coronary artery disease: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2017;12:e0169807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wang L, Zhou Y, Qian C, et al. Clinical characteristics and improvement of the guideline-based management of acute myocardial infarction in China: a national retrospective analysis. Oncotarget 2017;doi: 10.18632/oncotarget.14890 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bates ER, Tamis-Holland JE, Bittl JA, et al. PCI strategies in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. J Am Coll Cardiol 2016;68:1066–81. [DOI] [PubMed] [Google Scholar]
- [8].Hyun DY, Jeong MH, Sim DS, et al. Two-year clinical outcomes in stable angina and acute coronary syndrome after percutaneous coronary intervention of left main coronary artery disease. Korean J Intern Med 2016;31:1084–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Upadhaya S, Baniya R, Madala S, et al. Drug-eluting stent placement versus coronary artery bypass surgery for unprotected left main coronary artery disease: a meta-analysis of randomized controlled trials. J Card Surg 2017;32:70–9. [DOI] [PubMed] [Google Scholar]
- [10].Franzone A, Taniwaki M, Rigamonti F, et al. Angiographic complexity of coronary artery disease according to SYNTAX score and clinical outcomes after revascularisation with newer-generation drug-eluting stents: a substudy of the BIOSCIENCE trial. EuroIntervention 2016;12:e595–604. [DOI] [PubMed] [Google Scholar]
- [11].Amsterdam EA, Wenger NK, Brindis RG, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. Am Assoc Clin Chem 2014;64:e139–228. [Google Scholar]
- [12].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Akgun T, Oduncu V, Bitigen A, et al. Baseline SYNTAX score and long-term outcome in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Clin Appl Thromb Hemost 2015;21:712–9. [DOI] [PubMed] [Google Scholar]
- [14].Capodanno D, Capranzano P, Di Salvo ME, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc Interv 2009;2:731–8. [DOI] [PubMed] [Google Scholar]
- [15].Capodanno D, Di Salvo ME, Cincotta G, et al. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv 2009;2:302–8. [DOI] [PubMed] [Google Scholar]
- [16].Garg S, Sarno G, Serruys PW, et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a substudy of the STRATEGY (Single High-Dose Bolus Tirofiban and Sirolimus-Eluting Stent Versus Abciximab and Bare-Metal Stent in Acute Myocardial Infarction) and MULTISTRATEGY (Multicenter Evaluation of Single High-Dose Bolus Tirofiban Versus Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in AcuteMyocardial Infarction Study) trials. JACC Cardiovasc Interv 2011;4:66–75. [DOI] [PubMed] [Google Scholar]
- [17].Garg S, Serruys PW, Silber S, et al. The prognostic utility of the SYNTAX score on 1-year outcomes after revascularization with zotarolimus- and everolimus-eluting stents: a substudy of the RESOLUTE All Comers Trial. JACC Cardiovasc Interv 2011;4:432–41. [DOI] [PubMed] [Google Scholar]
- [18].Girasis C, Garg S, Räber L, et al. SYNTAX score and clinical SYNTAX score as predictors of very long-term clinical outcomes in patients undergoing percutaneous coronary interventions: a substudy of SIRolimus-eluting stent compared with pacliTAXel-eluting stent for coronary revascularization (SIRTAX) trial. Eur Heart J 2011;32:3115–27. [DOI] [PubMed] [Google Scholar]
- [19].He JQ, Gao YC, Yu XP, et al. Syntax score predicts clinical outcome in patients with three-vessel coronary artery disease undergoing percutaneous coronary intervention. Chin Med J (Engl) 2011;124:704–9. [PubMed] [Google Scholar]
- [20].Ikeno F, Brooks MM, Nakagawa K, et al. SYNTAX score and long-term outcomes: the BARI-2D trial. J Am Coll Cardiol 2017;69:395–403. [DOI] [PubMed] [Google Scholar]
- [21].Kim YH, Park DW, Kim WJ, et al. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) score for prediction of outcomes after unprotected left main coronary revascularization. JACC Cardiovasc Interv 2010;3:612–23. [DOI] [PubMed] [Google Scholar]
- [22].Magro M, Nauta S, Simsek C, et al. Value of the SYNTAX score in patients treated by primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: the MI SYNTAX score study. Am Heart J 2011;161:771–81. [DOI] [PubMed] [Google Scholar]
- [23].Nozue T, Kamijima R, Iwaki T, et al. Impact of SYNTAX score on 1-year clinical outcomes in patients undergoing percutaneous coronary intervention for unprotected left main coronary artery. Am J Cardiovasc Dis 2012;2:216–22. [PMC free article] [PubMed] [Google Scholar]
- [24].Park KW, Kang J, Kang SH, et al. Usefulness of the SYNTAX and clinical SYNTAX scores in predicting clinical outcome after unrestricted use of sirolimus- and everolimus-eluting stents. Circ J 2013;77:2912–21. [DOI] [PubMed] [Google Scholar]
- [25].Sinning JM, Asdonk T, Erlhöfer C, et al. Combination of angiographic and clinical characteristics for the prediction of clinical outcomes in elderly patients undergoing multivessel PCI. Clin Res Cardiol 2013;102:865–73. [DOI] [PubMed] [Google Scholar]
- [26].Valgimigli M, Serruys PW, Tsuchida K, et al. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol 2007;99:1072–81. [DOI] [PubMed] [Google Scholar]
- [27].Wykrzykowska JJ, Garg S, Girasis C, et al. Value of the SYNTAX score for risk assessment in the all-comers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus ERodable Stent coating) trial. J Am Coll Cardiol 2010;56:272–7. [DOI] [PubMed] [Google Scholar]
- [28].Yadav M, Généreux P, Palmerini T, et al. SYNTAX score and the risk of stent thrombosis after percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndromes: an ACUITY trial substudy. Catheter Cardiovasc Interv 2015;85:1–0. [DOI] [PubMed] [Google Scholar]
- [29].Cutlip DE, Nakazawa G, Krucoff MW, et al. Autopsy validation study of the Academic Research Consortium stent thrombosis definition. JACC Cardiovasc Interv 2011;4:554–9. [DOI] [PubMed] [Google Scholar]
- [30].Wiley, Higgins JP, et al. Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions 2008;187–241. [Google Scholar]
- [31].Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed October 19, 2009. [Google Scholar]
- [32].Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 2001;323:101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Minamisawa M, Miura T, Motoki H, et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with prior heart failure undergoing percutaneous coronary intervention: sub-analysis of the SHINANO registry. Heart Vessels 2017;32:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Palmerini T, Calabrò P, Piscione F, et al. Impact of gene polymorphisms, platelet reactivity, and the SYNTAX score on 1-year clinical outcomes in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: the GEPRESS study. JACC Cardiovasc Interv 2014;7:1117–27. [DOI] [PubMed] [Google Scholar]
- [35].Chen J, Tang B, Lin Y, et al. Validation of the ability of SYNTAX and clinical SYNTAX scores to predict adverse cardiovascular events after stent implantation: a systematic review and meta-analysis. Angiology 2016;67:820–8. [DOI] [PubMed] [Google Scholar]
- [36].Waliszewski M, Rittger H. Surrogate and clinical endpoints in interventional cardiology: are statistics the brakes? Ther Adv Cardiovasc Dis 2016;10:314–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chen SL, Chen JP, Mintz G, et al. Comparison between the NERS (New Risk Stratification) score and the SYNTAX (Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) score in outcome prediction for unprotected left main stenting. JACC Cardiovasc Interv 2010;3:632–41. [DOI] [PubMed] [Google Scholar]
- [38].Salvatore A, Boukhris M, Giubilato S, et al. Usefulness of SYNTAX score II in complex percutaneous coronary interventions in the setting of acute coronary syndrome. J Saudi Heart Assoc 2016;28:63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Madeira S, Raposo L, Brito J, et al. Potential utility of the SYNTAX score 2 in patients undergoing left main angioplasty. Arq Bras Cardiol 2016;106:270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


