Abstract
Background
Several patients with new onset brain tumors present to the Emergency Department (ED) complaining for new symptoms. Although information exists on symptom prevalence in the entire population of patients with brain tumors, little is known about the clinical presentation in ED. This retrospective study was planned to investigate clinical presentation and epidemiology of brain tumors firstly diagnosed in a large urban ED throughout a 10-year period.
Methods
All medical records of patients aged ≥18 years, discharged from our ED with a diagnosis of brain tumor were retrieved from the electronic hospital database during a 10-year period (2006 to 2015). The records were reassessed for selecting only brain tumors firstly diagnosed in the ED. The symptoms at presentation were divided in six categories: (I) headache; (II) seizures; (III) focal signs; (IV) altered mental status; (V) nausea/vomiting/dizziness; (VI) trauma. For all cases, the hospital record was retrieved, to obtain histologic classification of tumors. Patients with inflammatory neoformations were excluded from the study.
Results
Overall, 205 patients with firstly diagnosed brain tumor were identified among 870,135 ED visits (i.e., <1%). Glial tumors were the most frequent (50% of the entire sample). No significant differences were found between mean age of patients in the different histologically based groups (meningiomas 66±14; glioblastomas 65±16 years; metastases 66±13 years; other miscellaneous 66±19 years). Focal signs accounted for more than 50% of all presentation signs/symptoms.
Conclusions
First presentation of brain tumor in the ED is not a rare occurrence, so that the emergency physicians should be aware of this possibility.
Keywords: Brain tumor, glial tumor, astrocytoma, meningioma, Emergency Department (ED)
Introduction
Although primary and metastatic brain tumors are a significant cause of morbidity and mortality, precise information on brain tumors’ epidemiology is poor, since the registration is not mandatory in many countries worldwide. Moreover, brain tumor recording is often limited to malignant tumors, thus excluding non-malignant or borderline ones (1). In both American and European studies, the incidence rate of brain tumors ranges from 17.6/105 to 22.0/105 (2,3). For example, approximately 18,500 new cases of primary malignant brain tumors are diagnosed each year in the United States, and they are associated with high rates of mortality (i.e., approximately 3% of 5-year survival) (4). In the United States patients with brain tumors have a monthly rate of Emergency Department (ED) visit higher than that of the general population (with a monthly mean cost of $48 vs. $3) (5).
Some regional registries (for example in Spain, Italy, and France) have also provided useful data (6-8), but clinical and biological information are rarely investigated despite their clear relevance.
It is generally acknowledged that the symptoms caused by the presence of brain tumors can be physical (e.g., focal signs, fatigue, headaches) or behavioral (e.g., hallucinations, depression, anxiety, decreased attention and concentration, memory problems), mainly according to the specific localization of the tumor (9). Nevertheless, precise information is almost lacking and, when available, it is also quite contradictory. For example, in a study of 124 patients previously diagnosed with brain tumors, the most common symptoms that could be recorded were fatigue, sleep disturbance, drowsiness, distress and dry mouth (10). Unlike these findings, six symptoms (i.e., fatigue, uncertainty about the future, motor difficulties, drowsiness, communication difficulties and headaches) were reported in >50% in a sample of patients with glioma, with a considerably negative impact on their quality of life (11). Weakness and headaches were also the two main symptoms reported in a sample of 92 patients with brain tumors by Davies et al. (12), whereas depression has been identified as the single most important symptom predicting quality of life in a cohort of 73 patients with primary brain tumors by Pelletier et al. (13). More recently, a study identified two clusters of symptoms in a group of newly diagnosed patients with brain tumors, thus including a language cluster (i.e., difficulty reading or writing and finding the right words) and a mood cluster (sadness, anxiety, depression) (14).
A significant part of patients who were not previously diagnosed with brain tumors present to the ED complaining for new symptoms. Although, as aforementioned, information exists on the prevalence of signs/symptoms in the general population of patients with brain tumors, little is known about the clinical presentation in the ED. Only a single retrospective study, referred to a mixed pediatric and adult population, has been published, describing the presenting signs and symptoms of patients with primary brain tumors diagnosed in the ED to the best of our knowledge (15). Briefly, a total of 101 patients, identified with a hospital discharge diagnosis of primary brain tumor, were admitted in hospital through the ED. The presenting signs and symptoms included headache (56 patients), altered mental status (51 patients), ataxia (41 patients), nausea or vomiting (37 patients), motor weakness (37 patients), papilledema (28 patients), weakness (27 patients), cranial nerve palsies (26 patients), speech deficits (21 patients), visual deficits (20 patients), and sensory abnormalities (18 patients). The average age was 43 years, with a range of 3 days to 88 years. In this study, the majority of tumors were malignant astrocytomas, and the prevalent tumor location was cortical (68 patients).
In pediatric patients, brain tumors diagnosed in the ED most commonly present with headache, symptoms related to hydrocephalus, nausea/vomiting, and gate disturbances (16).
Therefore, due to the lack of information regarding the ED presentation of patients with brain tumors, the aim of this study was to investigate the clinical presentation and the epidemiology of brain tumors firstly diagnosed in a large urban ED throughout a 10-year period.
Methods
The University Hospital of Parma (Italy) is a 1,150-bed teaching general hospital, which serves a general population of nearly 435,000 inhabitants, and is the only hospital in the geographical area of the city of Parma. The hospital is a level 2 trauma center, and also a referral center for stroke, neurosurgery, and acute myocardial infarction (AMI). In the local facility, children aged 14 years or younger are visited in the pediatric emergency room, and their medical information is recorded in a separate local database. Adolescents aged 14–18 years are sometimes visited in the ED, but on other occasions they directly access the Pediatric Emergency Room, so that this part of the population has been excluded from our study.
All the records of patients aged ≥18 years, discharged from the local ED with a diagnosis of brain tumor have hence been retrieved from the electronic hospital database, during a 10-year period (i.e., between January 1st, 2006 to December 31st, 2015). All the records were independently reassessed by two of the authors (i.e., I Comelli and F Servadei), and the classification was further supervised by two other authors (i.e., G Cervellin and V Campana), with the aim of selecting only brain tumors which were not previously diagnosed outside the ED (i.e., only including those which were firstly diagnosed in the ED). The symptoms at presentation were divided in six categories: (I) headache; (II) seizures; (III) focal signs; (IV) altered mental status; (V) nausea/vomiting/dizziness; (VI) trauma (i.e., occasional diagnosis in course of CT execution for trauma). In several cases the clinical presentation included more than one main symptom, e.g., headache plus altered mental status, so that the sum of the different rates is >100%.
For all selected cases, the complete hospital record was retrieved, to obtain additional information including the histologic classification of tumor. Due to the broad range of histologic types (see section “Discussion”), we classified all cases according to four main categories, for practical purposes: (I) glial tumors (including astrocytomas, glioblastomas, oligodendrogliomas etc.); (II) meningiomas; (III) metastases (when neoplasm not formerly known); (IV) others miscellaneous tumors (including medulloblastomas, ependymal tumors, schwannomas, hemangiomas, lymphomas etc.). Inflammatory neoformations (i.e., abscesses, mycetomas etc.) were obviously excluded from the study. The differences between groups were evaluated with one-way analysis of variance (ANOVA), using Analyse-it (Analyse-it Software Ltd, Leeds, UK).
Due to the retrospective design of this study and maintenance of anonymity of the patients, ethical committee approval was unnecessary. Nevertheless, the study was approved by the local review Board and was performed in accordance with the Declaration of Helsinki, under the terms of relevant local legislation.
Results
A total of 205 patients (111 men, 94 women) with a firstly diagnosed brain tumor were identified among 870,135 ED visits throughout the study period, thus representing approximately 0.02% of the entire ED population. The demographic characteristics of the patient population are shown in Figure 1, whereas the histologically classified groups are summarized in Table 1. Glial tumors were the most frequently diagnosed (i.e., 46.3%), followed by meningiomas (21.9%), metastases (17.1%), and others miscellaneous (14.7%). No significant differences were observed between the mean age of patients with different histologically based groups (glioblastomas 65±16 years; meningiomas 66±14.20 years; metastases 66±13 years; other miscellaneous 66±19 years; P=0.972). The main signs and/or symptoms of presentation are reported in Table 2, with focal signs accounting for over than 50% of all clinical pictures.
Figure 1.
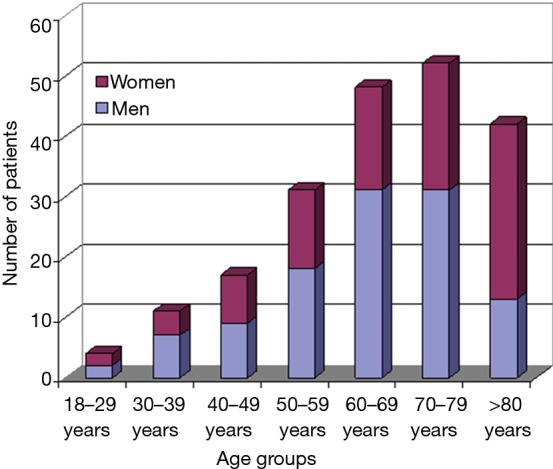
Age of the study population.
Table 1. Histological classification of brain tumors firstly diagnosed in the emergency department.
| Tumor class | Number (%) |
|---|---|
| Glial tumors | 95 (46.3) |
| Meningiomas | 45 (22.0) |
| Metastases | 35 (17.1) |
| Others miscellaneous | 30 (14.6) |
Table 2. Leading signs and symptoms of brain tumors firstly diagnosed in the emergency department.
| Main signs/symptoms | Number (%) |
|---|---|
| Focal signs | 122 (59.5) |
| Mental status alteration | 51 (24.9) |
| Headache | 30 (14.6) |
| Seizures | 29 (14.1) |
| Trauma (occasional) | 16 (7.8) |
| Nausea/vomiting/dizziness | 9 (4.4) |
Discussion
The signs and symptoms found more frequently in our population of primarily diagnosed brain tumor in the ED were focal signs, followed by mental status alteration, seizures, and headache. Notably, a considerable part was serendipitously diagnosed (i.e., 7.8%, thus approaching 2 cases per year), when undergoing a CT scan for head injury. This data substantially confirms that observed in a previous study (17). Glial tumors were the most frequently diagnosed in our sample, followed by meningiomas, metastases and others miscellaneous tumors.
The classification of brain tumors has been traditionally characterized by a high degree of uncertainty, and has been changed many times over the last two centuries. The first report about brain tumor classification was published by Virchow in 1863 (18), whereas the vast majority of currently used terms were introduced by Bailey and Cushing in 1926 (19). In 1949, Kernohan et al. simplified the classification by reducing the number of brain tumor types and introducing the concept of tumor grading (20). The first World Health Organization (WHO) classification of brain tumors was published in 1979 (21), and substantially used the original terminology from Cushing and Bailey. Revised WHO-based classifications have then been published in 1993, 2000, 2007 and, finally, in 2016 (22). The current WHO classification is extremely complex and certainly practical for neurosurgeons and oncologists, but is not actually applicable in an emergency medicine context. Considering the high number of histological subtypes, nearly each subtype of brain tumor could indeed be considered as a rare one. Moreover, it has been previously demonstrated that there is a substantial inter-observer and inter-center discordance in the diagnosis of specific subtypes (23). This is the reason why we originally decided to simplify the classification of our patient population by grouping similar tumor types in substantially homogeneous groups. The mean age of our patients was found to be higher than that previously reported (17), and this is probably due to the exclusion of pediatric patients from our study. All the age groups (i.e., >18 years) were represented in our population, with a higher prevalence of patients aged more than 50 years, but with no significant differences among the different histological subgroups.
Conclusions
Taken together, the results of our study show that first diagnosis of brain tumors is not very frequent in the ED, but it cannot be considered a rare event for the wide and heterogeneous population of patients admitted to a large urban ED, so that the emergency physicians should always be aware of this possibility.
Acknowledgements
The authors acknowledge Drs. Marco Brambilla and Marco Mignani of the University Hospital of Parma for the kind support in extracting data from electronic databases of the Institution.
Ethical Statement: The study was approved by the local review Board.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Forman D, Bray F, Brewster DH, et al. editors. Cancer incidence in five continents, vol X. Lyon: IARC, 2014. [Google Scholar]
- 2.Ostrom QT, Gittleman H, Fulop J, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol 2015;17:iv1-62. 10.1093/neuonc/nov189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crocetti E, Trama A, Stiller C, et al. Epidemiology of glial and non-glial brain tumours in Europe. Eur J Cancer 2012;48:1532-42. 10.1016/j.ejca.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 4.American Cancer Society. Cancer facts and figures. Available online: http://www.cancer.org. Last accessed April 15th 2017.
- 5.Kutikova L, Bowman L, Chang S, et al. Utilization and cost of health care services associated with primary malignant brain tumors in the United States. J Neurooncol 2007;81:61-5. 10.1007/s11060-006-9197-y [DOI] [PubMed] [Google Scholar]
- 6.Baldi I, Gruber A, Alioum A, et al. Descriptive epidemiology of CNS tumors in France: results from the Gironde registry for the period 2000-2007. Neuro Oncol 2011;13:1370-8. 10.1093/neuonc/nor120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruiz-Tovar M, López-Abente G, Pollán M, et al. Brain cancer incidence in the province of Zaragoza and Navarre (Spain): effect of age, period and birth cohort. J Neurol Sci 1999;164:93-9. 10.1016/S0022-510X(99)00048-9 [DOI] [PubMed] [Google Scholar]
- 8.Caldarella A, Crocetti E, Paci E. Is the incidence of brain tumors really increasing? A population-based analysis from a cancer registry. J Neurooncol 2011;104:589-94. 10.1007/s11060-011-0533-5 [DOI] [PubMed] [Google Scholar]
- 9.Shaw EG, Robbins ME. The management of radiation-induced brain injury. Cancer Treat Res 2006;128:7-22. 10.1007/0-387-25354-8_2 [DOI] [PubMed] [Google Scholar]
- 10.Armstrong TS, Gning I, Mendoza TR, et al. Clinical utility of the MDASI-BT in patients with brain metastases. J Pain Symptom Manage 2009;37:331-40. 10.1016/j.jpainsymman.2008.02.011 [DOI] [PubMed] [Google Scholar]
- 11.Osoba D, Brada M, Prados MD, et al. Effect of disease burden on health-related quality of life in patients with malignant gliomas. Neuro Oncol 2000;2:221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies E, Clarke C. Early symptoms of brain tumours. J Neurol Neurosurg Psychiatry 2004;75:1205-6. 10.1136/jnnp.2003.033308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pelletier G, Verhoef MJ, Khatri N, et al. Quality of life in brain tumor patients: the relative contributions of depression, fatigue, emotional distress, and existential issues. J Neurooncol 2002;57:41-9. 10.1023/A:1015728825642 [DOI] [PubMed] [Google Scholar]
- 14.Gleason JF, Case D, Rapp SR, et al. Symptom clusters in patients with newly-diagnosed brain tumors. J Support Oncol 2007;5:427-33. [PubMed] [Google Scholar]
- 15.Snyder H, Robinson K, Shah D, et al. Signs and symptoms of patients with brain tumors presenting to the emergency department. J Emerg Med 1993;11:253-8. 10.1016/0736-4679(93)90042-6 [DOI] [PubMed] [Google Scholar]
- 16.Lanphear J, Sarnaik S. Presenting Symptoms of Pediatric Brain Tumors Diagnosed in the Emergency Department. Pediatr Emerg Care 2014;30:77-80. 10.1097/PEC.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 17.Darlix A, Zouaoui S, Rigau V, et al. Epidemiology for primary brain tumors: a nationwide population-based study. J Neurooncol 2017;131:525-46. 10.1007/s11060-016-2318-3 [DOI] [PubMed] [Google Scholar]
- 18.Virchow R. editor. Die Krankhaften Geschwulste. Berlin: Hirschwald, 1863. [Google Scholar]
- 19.Bailey P, Cushing H. editors. A classification of tumors of the glioma group on a histogenetic basis with a correlation study of prognosis. Philadelphia: Lippincott, 1926. [Google Scholar]
- 20.Kernohan JW, Mabon RF, Svien HJ, et al. A simplified classification of the gliomas. Symposium on a new simplified concept of gliomas. Mayo Clin Proc 1949;35:71-5. [PubMed] [Google Scholar]
- 21.Zülch KJ, Avtsyn AP, Barnar RO, et al. editors. Histological typing of tumours of the central nervous system. Geneva: Office of Publications, World Health Organization, 1979. [Google Scholar]
- 22.Louis DN, Ohgaki H, Wiestler OD, et al. editors. WHO classification and grading of tumours of the central nervous system. Lyon: IARC Press, 2016. [Google Scholar]
- 23.van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol 2010;120:297-304. 10.1007/s00401-010-0725-7 [DOI] [PMC free article] [PubMed] [Google Scholar]


