Abstract
Ultrasound imaging of the musculoskeletal system is an important element of the diagnostic and therapeutic protocol. Clinical decisions, including those regarding surgical procedures, are often based solely on ultrasound imaging. However, detailed knowledge on the anatomy and a correct scanning technique are crucial for an accurate diagnosis. Modern ultrasonographic equipment allows obtaining detailed anatomical images of muscle tendons, ligaments, nerves and vessels of the carpal area. Ventral wrist ultrasound is one of the most common diagnostic procedures in patients with suspected carpal tunnel syndrome. Ventral wrist evaluation is also often performed in patients with wrist pain of unclear etiology, rheumatic diseases, wrist injuries or symptoms of ulnar neuropathy. The aim of this paper is to present ultrasound images with corresponding anatomical schemes. The technique of ultrasound examination of the ventral wrist along with practical guidance to help obtain highly diagnostic images is also discussed. The present paper is the second part of an article devoted to ultrasound anatomy and wrist ultrasound technique – the part discussing the dorsal side of the wrist was published in the Journal of Ultrasonography, Vol. 15, No 61. The following anatomical structures should be visualized during an ultrasound examination of the ventral wrist, both in the carpal tunnel as well as proximally and distally to it: four flexor digitorum superficialis tendons, four flexor digitorum profundus tendons, flexor pollicis longus, flexor carpi radialis tendon, median nerve and flexor retinaculum; in the carpal tunnel as well as proximally and distally to it: the ulnar nerve, ulnar artery and veins; the tendon of the flexor carpi ulnaris muscle; carpal joints.
Keywords: ultrasound, tendons, wrist, peripheral nerves, hand
Introduction
The continuous development of ultrasound devices and transducers has led to a systematic increase in the importance of ultrasonography in the diagnosis of musculoskeletal diseases, including wrist pathologies(1–3). An assessment of the ventral wrist, similarly to the diagnosis of dorsal wrist pathologies described in the first part of the article published in the Journal of Ultrasonography Vol. 15, No. 61, includes tendinous and muscular structures, nerves, vessels and ligaments(4).
The ventral wrist assessment should include imaging of the following anatomical structures (Tab. 1):
Tab. 1.
Anatomical structures evaluated during ultrasound examination of the ventral wrist
| Wrist Ultrasound | |
|---|---|
| Ventral wrist | Carpal tunnel |
| Guyon’s canal | |
| Median nerve | |
| Ulnar nervec | |
| Joint capsule | |
| Intercarpal ligaments | |
in the carpal tunnel – four flexor digitorum superficialis (FDS) tendons, four flexor digitorum profundus (FDP) tendons, flexor pollicis longus (FPL), the median nerve along with its common palmar branches and the flexor retinaculum;
in the Guyon’s canal – the ulnar nerve along with its superficial branch innervating the skin of fingers 4-5, as well as the deep branch innervating hand muscles, the ulnar artery and ulnar veins;
the flexor carpi ulnaris (FCU) tendon along with its attachment to the pisiform bone;
the flexor carpi radialis (FCR) tendon along with its attachment to the base of the second metacarpal bone;
carpal joints.
The carpal tunnel
Bony landmarks play a major role in the assessment of the carpal tunnel. In the proximal part, these are the scaphoid tubercle on the radial side and the pisiform bone on the ulnar side. The distal border of the carpal tunnel is landmarked by the trapezium’s tubercle from the radial side and by the hook of the hamate bone from the ulnar side. The dimensions of the proximal carpal tunnel are slightly smaller than those of distal tunnel(5). The examination is performed in a sitting position, but it may be performed in a lying position in elderly or bedridden patients. The hand is in supination. The transducer is applied to the region of the palm fold in the transverse plane so that its edges were located above the scaphoid and the pisiform bone during scanning (Fig. 1).
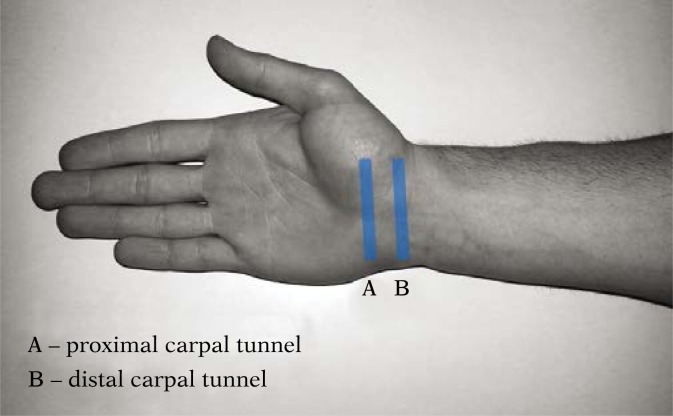
Fig. 1.
The carpal tunnel. Scanning technique for the assessment of proximal and distal end of the carpal tunnel. The Guyon’s Canal is assessed using a similar transducer position as in the carpal tunnel (perpendicular to the long axis of the limb), however, the transducer should be slightly shifted to the ulnar side. Ultrasound images obtained at the indicated transducer positions are shown in Fig. 2
Tips and tricks: tilting the transducer superiorly and inferiorly may facilitate the imaging of carpal tunnel soft tissues (the use of anisotropic phenomenon).
In order to make deeper-seated structures more visible, the wrist should be gently bent dorsally and the scanning parameters, such as depth and focus, should be adjusted.
Once the bony landmarks are identified and the transducer is properly positioned, the flexor retinaculum and the tendons of the digital flexors, which are located in the carpal tunnel, are assessed. Apart from the tendons and their sheaths, attention should be also paid to possible anatomical muscle variants, bone lesions (traumatic, degenerative) and tumors in the carpal tunnel. Inflammation of the tendon sheaths of the first through fifth digital flexors, low-descending FDS muscle belly or other lesions (traumatic, tumor) and ganglions may cause carpal tunnel syndrome (6) (Tab. 2).
Tab. 2.
Anatomy review of superficial and deep digital flexors
| Superficial digital flexor | Deep digital flexor |
|---|---|
|
Origin: humeral-ulnar head on the medial epicondylus of the humeral bone and the coronoid process of the ulnar bone radial head – proximal part of the anterior surface of the radial bone, distally from the radial tuberosity Insertion: middle 2-5 phalanges on lateral and middle surfaces Blood supply: tętnica promieniowa i tętnica łokciowa Nerve: the median nerve Actions: flexion of fingers 2-5 in the metacarpophalangeal and proximal interphalangeal joints, bending the hand in the radiocarpal joint, weak flexor of the ulnar joint |
Origin: anterior surface of the ulnar bone (proximal and middle part), adjacent interosseous forearm membrane Insertion: ventral surface of the base of distal phalanges 2-5 Blood supply: ulnar artery and anterior interosseous artery Nerve: median and ulnar nerves Actions: flexion of fingers 2-5 in the metacarpophalangeal, proximal and distal interphalangeal joints, bending the hand in the radiocarpal joint |
Tips and tricks: Passive bending and straightening of each finger during ultrasound examination will allow for a precise identification of the tendon affected by the visualized pathology.
The FCR tendon is located on the radial side of the carpal tunnel, superficially to the flexor retinaculum (the transverse carpal ligament). Thumb movement will allow distinguishing between FCR and FPL. The FCU tendon is very narrow; its assessment should preferably begin at its insertion to the pisiform bone (Fig. 2).
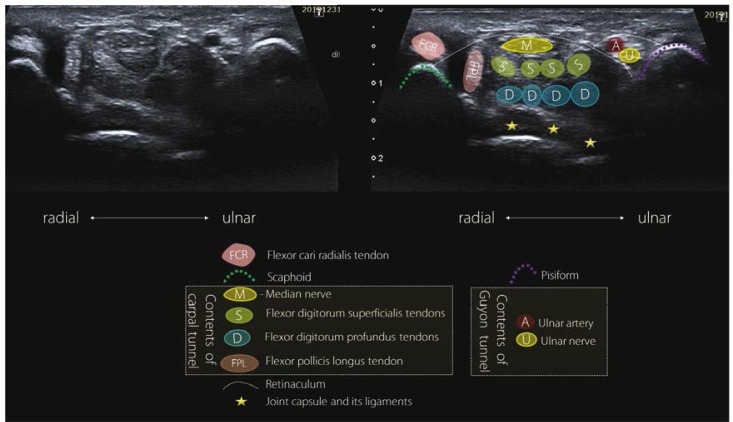
Fig. 2.
Proximal carpal tunnel and Guyon’s canal in a cross-section. Flexor carpi radialis (FCR) and flexor pollicis longus (FPL). The median nerve (M) is located superficially relative to the tendon of flexor digitorum superficialis (S) and the tendons of flexor digitorum profundus (D). In the Guyon’s canal: the ulnar artery (A) and the ulnar nerve (U)
In order to scan the distal part of the carpal tunnel, the transducer should be applied above two bony landmarks formed by the trapezium’s tubercle from the radial side and the hook of the hamate bone from the ulnar side.
The median nerve
The median nerve runs in the distal part of the forearm, between the FDS and the FDP. In the region of the wrist, the nerve extends towards the radial side and, before entering the carpal tunnel, it extends superficially along the lateral edge of the FDS. In the carpal tunnel, the median nerve passes directly under the flexor retinaculum and superficially to FPL tendons and the superficial flexor tendon of the second digit(5). The cross-sectional appearance of the median nerve varies as it passes through the carpal tunnel. It appears oval in the initial segment to become more flat-shaped at the level of the hook of the hamate bone.
The median nerve usually supplies (there are many variants) the palmar side of fingers 1–3 and the radial half of finger 4. Proximally to the transverse ligament of the wrist, the median nerve gives off a palmar branch, which is a sensory nerve supplying the skin of the radial part of the palm. Since the nerve passes superficially to the flexor retinaculum, its function remains intact in patients with carpal tunnel syndrome. In the region of the distant edge of the transverse carpal ligament, the median nerve gives a retrograde branch innervating the thenar eminence. Due to its varying course (according to the classification proposed by Poisel et al.(7), three types of median nerve retrograde branch, i.e. extraligamentous, subligamentous, and transligamentous, may be distinguished depending on its relation with the transverse ligament of the wrist), this branch may be damaged during carpal tunnel syndrome surgery. The nerve has been called the “million dollar injury” due to the compensations awarded in lawsuits.
The median nerve supplies the palmar side of fingers 1–3 and the radial half of finger 4.
It is assessed in the transverse or longitudinal sections using B-mode. The visualization of the nerve in a longitudinal section may be difficult due to its winding course; therefore it is often assessed in a cross-section. Furthermore, attention should be paid to the anatomical variants, such as median nerve dichotomy and trichotomy as well as persistent median artery(8). In the diagnosis of median nerve neuropathy, the symptom of ‘indentation’, i.e. an image of nerve narrowing at the level of the proximal border of the carpal tunnel, indicates nerve compression, while the symptom of ‘reverse indentation’ indicates an increased thickness of the nerve at the level of the distal border of the flexor retinaculum(9). Under normal conditions, the nerve exhibits a sliding motion relative to the flexor retinaculum and flexor tendons during a dynamic ultrasound examination (during bending of the wrist and fingers). Identification of scarring and adhesions helps in surgical planning(6,10) (Fig. 3).
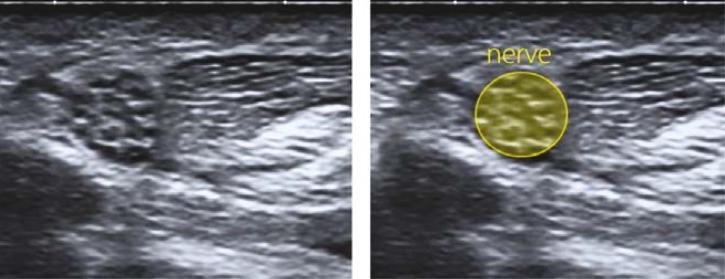
Fig. 3.
The median nerve. A characteristic oval shape in a cross-section. Difficult to visualize in a longitudinal section due to its winding course and echogenicity similar to that of adjacent tendons. We used the ‘elevator technique’, i.e. an assessment of the whole length of nerve in a cross-section proximally and distally relative to the flexor retinaculum
The flexor retinaculum, also known as the transverse carpal ligament
The transverse carpal ligament is a strong bond extending between the tubercle of the scaphoid bone and the tubercle of the trapezium bone on the radial side as well as the pisiform bone and the hook of the hamate bone on the ulnar side. The flexor retinaculum anteriorly closes the carpal tunnel containing the median nerve, FDS, FDP, and FPL tendons.
The clinical symptoms of median nerve neuropathy are mostly due to its compression; therefore it is important to evaluate its structure, thickening, flattening and the presence of enhanced vascularization. In the case of persistent median artery, its patency should be evaluated. Cases of median artery thrombosis with dilation compressing nerve bundles, which is crucial for the choice of treatment method, have been reported.
An estimation of the completeness of the section through the flexor retinaculum is important for postoperative assessment.
Anatomical differences in the structure of the tunnel may predispose to carpal tunnel syndrome. A narrow carpal tunnel, accessory muscles or tendons in the tunnel increase the risk of median nerve compression(11,12). Other factors that reduce the space in the carpal tunnel may include ganglions, cysts, as well as displaced wrist fractures(11). Nerve edema at the entry into the tunnel, edema (reduced echogenicity, increased cross-sectional area) and congestion of the nerve proximally to the site of compression in Doppler option are ultrasound symptoms indicating carpal tunnel syndrome. Nerve flattening at the compression site is a less sensitive parameter(1).
Guyon’s canal
Guyon’s canal is a fibro-osseous space extending superficially on the ulnar side relative to the carpal tunnel. This space is bordered by the pisiform bone from the ulnar side and the hook of the hamate bone from the radial side. The canal is bordered anteriorly by a layer of superficial fibers of the transverse ligament, and by a deep layer of the same ligament and the pisiform-hamate ligament from the dorsal side. The canal contains the ulnar nerve on the ulnar side and the ulnar artery on the radial side, as well as the ulnar vein(s). The ulnar nerve in the Guyon’s canal divides into superficial sensory and deep motor branches. The deep branch passes between the abductor and the short muscle of the fifth digit; it arches the hook of the hamate bone, leaving the Guyon’s canal, and extends towards the radial side on the palmar surface of the interosseous muscles, slightly distally from the deep palmar arch. The superficial branch extends on the surface of the hook of the hamate bone to later divide into the proper palmar digital branch (innervating the medial portion of the fifth digit) and the common palmar digital branch (which after branching innervates the lateral portion of the fifth digit and medial portion of the fourth digit). Neurological manifestations may suggest which part of the nerve is irritated or damaged. The course of the nerve and its branches may be divided into three anatomical zones. The first zone corresponds to the level of the pisiform bone and mainly contains the ulnar nerve along with motor and sensory fibers. Zones 2 and 3 are located more distally, at the level of the hamate bone. The second zone contains motor nerve fibers. The third zone is located superficially and contains a sensory branch of the ulnar nerve(5). Depending on the zone with nerve compression, the symptoms may be associated with motor fibers, sensory fibers or both.
The pisiform bone is a landmark for the position of transducer during imaging. The transducer is placed medially, in a transverse plane. The examination may help diagnose ganglions originating from the pisiform- triquetral joint, lipomas, ulnar aneurysms, traumatic lesions within the hook of the hamate bone, accessory muscles, as well as traumatic lesions of the nerve or its branches(3,13,14).
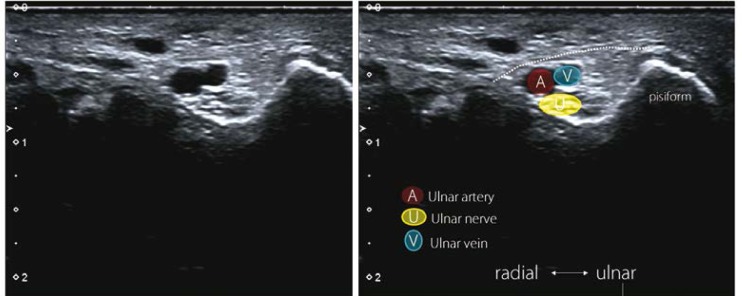
An accessory abductor of the little finger is the most common anatomical pathology found in this region (Fig. 4).
Fig. 4.
Guyon’s canal. Guyon’s canal contains the ulnar nerve (U), ulnar artery (A) and ulnar vein(s) (V). Cross-sectional images of the nerve show the sites of its division into two branches: deep motor and superficial sensory branch
The ulnar nerve
In the distal forearm, the ulnar nerve extends on the radial side of the flexor carpi ulnaris muscle. The ulnar artery passes on the radial side of the nerve. In this region, the ulnar nerve gives off two branches innervating skin, palmar branch and dorsal branch. Then, the nerve passes superficially relative to the transverse carpal ligament and through the Guyon’s canal, where it gives off two final branches. These are the superficial sensory branch and the deep motor branch.
The ulnar nerve supplies sensory innervations to the median palm, finger 5 and the median half of finger 4. The motor branch supplies the adductor pollicis muscle, two medial lumbricals, hypothenar muscles and inter-osseous muscles.
The flexor carpi radialis muscle
The origin of the FCR is located on the medial epicondyle of the humerus and the fascia of the forearm. The insertion is located on the base of the second metacarpal bone. The vasculature derives from the branch of the radial artery, while the innervation is supplied by the median nerve. The FCR passes medially to the pronator teres muscle. In the carpal tunnel, it passes separately under the superficial fibers of the flexor retinaculum, followed by the groove of the trapezium bone to later form an attachment on the base of the second metacarpal bone. As opposed to FCU, the tendon of this muscle has a sheath.
The flexor carpi ulnaris muscle
The flexor carpi ulnaris muscle is located most medially on the forearm. It has two heads: humeral and ulnar. The origin of the humeral head is located on the medial epicondyle of the humerus and the fascia of the forearm. The origin of the ulnar head is located on the ulnar process and the posterior edge of the ulnar bone. It runs adjacent to the FDS. A tendon that ends on the pisiform bone is the insertion for FCU. The muscle is supplied by the brachial artery via lateral arteries and branches from the ulnar artery. The muscle is innervated by the ulnar nerve. The insertion of this muscle has no synovial sheath. Enthesopathy, usually mineralized scars, at the attachment to the pisiform bone, is the most common pathology of the tendon seen on an ultrasound scan. Therefore, pain is usually localized in the region of the pisiform bone (Tab. 3).
Tab. 3.
Anatomy review of radial and ulnar carpal flexors
| Flexor carpi radialis | Flexor carpi ulnaris |
|---|---|
|
Origin: medial epicondylus of the humeral bone, fascia of the forearm Insertion: the base of the second metacarpal bone Blood supply: radial artery Nerve: the median nerve Actions: radial flexion and abduction of the hand, forearm pronation, minor flexion in the ulnar joint |
Origin: humeral head - medial epicondylus of the humeral bone, fascia of the forearm ulnar head – ulnar process and the posterior ridge of the ulnar bone Insertion: pisiform bone Blood supply: humeral artery via lateral arteries, ulnar artery Nerve: ulnar nerve Actions: flexion and ulnar adduction of the hand |
Summary
Ultrasonography is one of the most commonly used imaging techniques for the diagnosis of carpal pathology. Knowledge on ultrasound anatomy, anatomical variants and examination technique is crucial for an effective use of this tool.
Conflict of interests
None.
References
- 1.Han HY, Kim HM, Park SY, Kim MW, Kim JM, Jang DH. Clinical findings of asymptomatic carpal tunnel syndrome in patients with diabetes mellitus. Ann Rehabil Med. 2016;40:489–495. doi: 10.5535/arm.2016.40.3.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kasundra GM, Sood I, Bhargava AN, Bhushan B, Rana K, Jangid H, et al. Carpal tunnel syndrome: Analyzing efficacy and utility of clinical tests and various diagnostic modalities. J Neurosci Rural Pract. 2015;6:504–510. doi: 10.4103/0976-3147.169867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dębek A, Czyrny Z, Nowicki P. Sonography of pathological changes in the hand. J Ultrason. 2014;14:74–99. doi: 10.15557/JoU.2014.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olchowy C, Łasecki M, Zaleska-Dorobisz U. Wrist ultrasound examination – scanning technique and ultrasound anatomy. Part 1: Dorsal wrist. J Ultrason. 2015;15:172–188. doi: 10.15557/JoU.2015.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bianchi S, Martinoli C. Ultrasound of the Musculoskeletal System. Berlin – Heidelberg – New York: Springer Google Scholar; 2007. [Google Scholar]
- 6.Botchu R, Khan A, Jeyapalan K. Pictorial essay: Role of ultrasound in failed carpal tunnel decompression. Indian Journal Radiol Imaging. 2012;22:31–34. doi: 10.4103/0971-3026.95401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poisel S, Ursprung und Verlauf des R. muscularis des Nervus digitalis palmaris communis I (N. medianus) Chir Praxis. 1974;18:471–474. [Google Scholar]
- 8.Kowalska B, Sudoł-Szopińska I. Ultrasound assessment on selected peripheral nerve pathologies. Part I: Entrapment neuropathies of the upper limb – excluding carpal tunnel syndrome. J Ultrason. 2012;12:307–318. doi: 10.15557/JoU.2012.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapuścińska K, Urbanik A. High-frequency ultrasound in carpal tunnel syndrome: assessment of patient eligibility for surgical treatment. J Ultrason. 2015;15:283–291. doi: 10.15557/JoU.2015.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kowalska B, Sudoł-Szopińska I. Ultrasound assessment of selected peripheral nerve pathologies. Part III: Injuries and postoperative evaluation. J Ultrason. 2013;13:82–92. doi: 10.15557/JoU.2013.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teh J, Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol. 2014;80:47–63. doi: 10.1259/bjr/53596176. [DOI] [PubMed] [Google Scholar]
- 12.Zaniewicz-Kaniewska K, Sudoł-Szopińska I. Usefulness of sonography in the diagnosis of rheumatoid hand. J Ultrason. 2013;13:329–336. doi: 10.15557/JoU.2013.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong DC, Wansaicheong GK, Tsou IY. Ultrasonography of the hand and wrist. Singapore Med J. 2009;50:219–225. [PubMed] [Google Scholar]
- 14.Kowalska B, Sudoł-Szopińska I. Normal and sonographic anatomy of selected peripheral nerves. Part II: Peripheral nerves of the upper limb. Journal of Ultrasonography. 2012;12:131–147. doi: 10.15557/JoU.2012.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]