ABSTRACT
Objective
Estimated fetal weight (EFW) and fetal biometry are complementary measures used to screen for fetal growth disturbances. Our aim was to provide international EFW standards to complement the INTERGROWTH‐21st Fetal Growth Standards that are available for use worldwide.
Methods
Women with an accurate gestational‐age assessment, who were enrolled in the prospective, international, multicenter, population‐based Fetal Growth Longitudinal Study (FGLS) and INTERBIO‐21st Fetal Study (FS), two components of the INTERGROWTH‐21st Project, had ultrasound scans every 5 weeks from 9–14 weeks' until 40 weeks' gestation. At each visit, measurements of fetal head circumference (HC), biparietal diameter, occipitofrontal diameter, abdominal circumference (AC) and femur length (FL) were obtained blindly by dedicated research sonographers using standardized methods and identical ultrasound machines. Birth weight was measured within 12 h of delivery by dedicated research anthropometrists using standardized methods and identical electronic scales. Live babies without any congenital abnormality, who were born within 14 days of the last ultrasound scan, were selected for inclusion. As most births occurred at around 40 weeks' gestation, we constructed a bootstrap model selection and estimation procedure based on resampling of the complete dataset under an approximately uniform distribution of birth weight, thus enriching the sample size at extremes of fetal sizes, to achieve consistent estimates across the full range of fetal weight. We constructed reference centiles using second‐degree fractional polynomial models.
Results
Of the overall population, 2404 babies were born within 14 days of the last ultrasound scan. Mean time between the last scan and birth was 7.7 (range, 0–14) days and was uniformly distributed. Birth weight was best estimated as a function of AC and HC (without FL) as log(EFW) = 5.084820 − 54.06633 × (AC/100)3 − 95.80076 × (AC/100)3 × log(AC/100) + 3.136370 × (HC/100), where EFW is in g and AC and HC are in cm. All other measures, gestational age, symphysis–fundus height, amniotic fluid indices and interactions between biometric measures and gestational age, were not retained in the selection process because they did not improve the prediction of EFW. Applying the formula to FGLS biometric data (n = 4231) enabled gestational age‐specific EFW tables to be constructed. At term, the EFW centiles matched those of the INTERGROWTH‐21st Newborn Size Standards but, at < 37 weeks' gestation, the EFW centiles were, as expected, higher than those of babies born preterm. Comparing EFW cross‐sectional values with the INTERGROWTH‐21st Preterm Postnatal Growth Standards confirmed that preterm postnatal growth is a different biological process from intrauterine growth.
Conclusions
We provide an assessment of EFW, as an adjunct to routine ultrasound biometry, from 22 to 40 weeks' gestation. However, we strongly encourage clinicians to evaluate fetal growth using separate biometric measures such as HC and AC, as well as EFW, to avoid the minimalist approach of focusing on a single value. © 2016 Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of International Society of Ultrasound in Obstetrics and Gynecology.
Keywords: birth weight, fetal growth, gestational age, screening, ultrasound
INTRODUCTION
One of the main objectives of antenatal care is screening for fetal growth disturbances1. Although biomarkers in maternal blood have shown some potential for detecting fetal growth restriction2, 3, a recent systematic review suggested that none is sufficiently accurate to be recommended for use in clinical practice4. Clinicians, therefore, still rely routinely on clinical markers, including ultrasound measurements, to identify fetuses at risk5.
Ultrasound evaluation of the fetus involves measuring head circumference (HC), abdominal circumference (AC) and femur length (FL), and the values can be combined to calculate an estimated fetal weight (EFW); this estimate is often used alone in clinical practice without considering the individual measurements. However, we believe that arguments concerning the most appropriate single parameter to use are inappropriate because clinicians should use all the tools available in their armamentarium for making crucial clinical decisions that have major implications for both mothers and newborns.
The development of international EFW standards is overdue, and these should share the same conceptual basis as the published INTERGROWTH‐21st standards for HC, AC and FL, size at birth and postnatal growth in preterm infants6, 7, 8, 9. These standards would perfectly complement the World Health Organization (WHO) Child Growth Standards10, thereby enabling continuity of assessment of human growth from early pregnancy to childhood11. Therefore, the objectives of this component of the INTERGROWTH‐21st Project were: (1) to develop a formula to estimate fetal weight based on ultrasound biometry and birth weight; and (2) to construct international EFW standards for fetuses at 22 to 40 weeks' gestation.
SUBJECTS AND METHODS
INTERGROWTH‐21st is an international, multicenter, population‐based project consisting of a number of components, including the Fetal Growth Longitudinal Study (FGLS) and INTERBIO‐21st Fetal Study (FS).
FGLS was conducted between 27 April 2009 and 2 March 2014 in eight urban areas: the cities of Pelotas (Brazil), Turin (Italy), Muscat (Oman), Oxford (UK) and Seattle (USA); the Shunyi County of Beijing (China); the central area of Nagpur (India); and the Parklands suburb of Nairobi (Kenya). The primary aim was to study longitudinally the health and development of fetuses into infancy, by monitoring growth, health, nutrition and neurodevelopment from less than 14 weeks' gestation to 2 years of age, so as to produce prescriptive growth standards to complement the existing WHO Child Growth Standards. This was achieved by studying a cohort of healthy, well‐nourished, pregnant women who were at low risk of adverse maternal and perinatal outcomes at both population and individual levels. The study details have been described elsewhere9, 12.
In contrast, FS recruited an unselected cohort of pregnant women, between 8 February 2012 and 24 December 2015, from three FGLS sites (Pelotas, Nairobi, Oxford), and three new sites (Aga Khan University Hospital, Karachi, Pakistan; Shoklo Malaria Research Unit, Mae Sot, Thailand; and Baragwanath Hospital, Soweto, South Africa). The primary aim was to study the effects of various intrauterine exposures (e.g. malnutrition, anemia, human immunodeficiency virus, malaria) on growth, health, nutrition, neurodevelopment and the epigenome, over the same developmental age range, i.e. from less than 14 weeks' gestation to 2 years of age.
To develop the EFW formula requires as many pregnancies as possible that have a standardized scan and birth‐weight measurement. In order to achieve this we included fetuses from both FGLS and FS; only those that had an ultrasound scan within 14 days of birth were included in the calculations. To develop the international standards for EFW, the formula derived was then applied to the healthy FGLS population from which the International Fetal Growth Standards were produced6.
The INTERGROWTH‐21st Project was approved by the Oxfordshire Research Ethics Committee ‘C’ (reference: 08/H0606/139), the research ethics committees of the individual participating institutions and the corresponding regional health authorities in which the project was implemented. Participants provided written consent to be involved in the study.
Standard procedures
In both studies women were recruited at less than 14 weeks' gestation. All women underwent ultrasound measurement of fetal crown–rump length (CRL) using standardized methodology13, 14. In FGLS, gestational age was based on the date of the last menstrual period (LMP) provided it was certain, the woman had a regular 24–32‐day menstrual cycle and she had not been using hormonal contraception or breastfeeding in the preceding 2 months, and any discrepancy between the gestational ages based on LMP and CRL, between 9 + 0 and 13 + 6 weeks, was ≤ 7 days. In FS, gestational age was determined by CRL measurement alone, using the same formula loaded onto all study ultrasound machines15; if known, the date of the LMP was recorded.
Following the dating scan, women were scanned every 5 weeks (±1 week), so that the possible ranges were 14–18, 19–23, 24–28, 29–33, 34–38 and 39–42 weeks' gestation. At each visit, fetal HC, biparietal diameter (BPD), occipitofrontal diameter (OFD), AC and FL were measured three times from three separately obtained ultrasound images of each structure. The detailed measurement protocols, including graphical displays of measurement techniques, and the unique standardization procedures for all measurements and sonographer training have been reported elsewhere13, 16. In addition, all documentation, protocols, quality‐control procedures, data collection forms and electronic transfer strategies are freely available on the INTERGROWTH‐21st website.
Briefly, head measurements were taken in an axial view at the level of the thalami, with an angle of insonation as close as possible to 90°. The head had to be oval in shape, symmetrical, centrally positioned and filling at least 30% of the monitor screen. The midline echo (representing the falx cerebri) had to be broken anteriorly, at a third of its length, by the cavum septi pellucidi. The thalami had to be located symmetrically on either side of the midline. Calipers were then placed on the outer border of the parietal bones (outer to outer) at the widest or longest part of the skull for the BPD and OFD, respectively; HC was measured using the ellipse facility on the outer border of the skull.
AC measurements were taken in a cross‐sectional view of the fetal abdomen as close as possible to circular in shape, with the umbilical vein in the anterior third (at the level of the portal sinus), with the stomach bubble visible. The sonographer was instructed to avoid applying too much pressure with the transducer, which can distort the circular shape of the fetal abdomen. The abdomen had to fill at least 30% of the monitor screen, and the spine had to be at either the 3 or 9 o'clock position to avoid internal shadowing; the kidneys and bladder had not to be visible. For the measurements, the contour of the ellipse was placed on the outer border of the abdomen.
Finally, FL was measured using a longitudinal view of the fetal thigh closest to the probe and with the femur as close as possible to the horizontal plane. The angle of insonation of the ultrasound beam was about 90°, with the full length of the bone visualized, unobscured by shadowing from adjacent bony parts, and the femur had to fill at least 30% of the monitor screen. The intersection of the calipers was placed on the outer borders of the edges of the femoral diaphysis (outer to outer) ensuring clear femoral edges; ultrasound artifacts of the femoral edges such as the proximal trochanter or pointed femoral spurs were not included in the measurement (detailed methods and a graphical display of how the bone structures are localized are available on the INTERGROWTH‐21st website).
The same type of ultrasound machine, a Philips HD‐9 with curvilinear abdominal transducers C5‐2, C6‐3 and V7‐3 (Philips Ultrasound, Bothell, WA, USA), was used at all sites. To avoid expected value bias, the machine was adapted so that fetal measurements were not visible to the sonographer on the screen. Only after three measurements of each structure had been recorded were the average values revealed for clinical purposes. All ultrasound data were submitted electronically to the study database. Data were entered locally directly onto the web‐based system17.
After taking each set of measurements, sonographers scored the quality of their images on the basis of standard image‐scoring criteria18, 19. Images that did not score the maximum number of points were repeated until the best possible score was achieved. The quality‐control methods used across all sites are described in detail elsewhere18, 20.
Birth weight was measured within 12 h of birth using identical electronic scales (Seca, Hangzhou, China) at all sites. The equipment, which was calibrated twice a week, was selected for accuracy, precision and robustness, as shown previously21. Measurement procedures were standardized on the basis of WHO recommendations to ensure maximum validity and each measurement was collected independently by two study anthropometrists22, 23. If the difference between the two measurements exceeded the maximum allowable difference of 5 g, then both observers independently retook that measurement a second and, if necessary, a third time. The training, standardization, monitoring processes and quality‐control methods used across all sites are described in detail elsewhere22, 23.
Statistical analysis
Estimation of fetal weight
From the FGLS and FS cohorts, we identified all live babies without any congenital abnormality who were born at > 24 weeks' gestation and within 14 days of the last ultrasound scan. Given the study design, we expected the births to have occurred uniformly between 0 and 14 days after the last ultrasound scan, i.e. we expected there to be a mean time of 7–8 days between the last scan and birth. This cut‐off allowed a greater number of births at low gestational ages to be included, for which most of the existing formulae have been prone to prediction error, probably because scant data exist for estimation24. Potential predictors for birth weight were:
HC, BPD, OFD, AC and FL, in cm or transformed into Z‐scores using the INTERGROWTH‐21st equations6;
gestational age on the day of the last scan, in weeks;
symphysis–fundus height, in cm;
amniotic fluid, assessed by the deepest vertical pool and amniotic fluid index in cm;
cross‐sectional head area and abdominal area computed from their orthogonal diameters, in cm2.
We hypothesized that the contribution of any given anthropometric measurement to EFW might vary with gestational age. Therefore, we also considered interactions between HC, BPD, OFD, AC and FL and gestational age on the day of the last scan. Statistical modeling was conducted using second‐degree fractional polynomials25.
Some prediction bias would be expected because of significant growth between the day of the last scan and birth24, 26, 27. We addressed this issue by calculating the expected EFW on the day of the ultrasound scan, using the following steps: (1) in pregnancies from FGLS and FS delivering within 14 days from the last scan, we developed a model to predict birth weight from the most recent ultrasound measurements; (2) in the complete FGLS dataset, we calculated EFW from ultrasound biometry using the previous model and fitted a second‐degree fractional polynomial for mean weight as a function of gestational age between 22 and 40 weeks; (3) returning to the dataset of births within 14 days (step 1), we calculated, for each fetus, the expected weight at the time of the last scan by subtracting the average weight gain between the time of the last scan and birth using the model built in step 2; (4) this calculated weight was then used for further modeling.
As expected, owing to the prospective, population‐based design of FGLS, most births occurred close to 40 weeks' gestation, meaning that the scatter of observations across the 22–40‐week window was very uneven. We were aware that estimation using the complete dataset would yield very accurate estimates at 40 weeks' gestation, where the greatest contribution of the data is found, but with limited model validity for lower birth weights. To overcome this problem and allow accurate birth‐weight estimation over the whole range of observed data, we constructed a bootstrap model selection and estimation procedure based on resampling of the complete dataset under an approximately uniform distribution of birth weight28, 29, 30, i.e. birth weight was divided into 500‐g strata and each sample was built by randomly selecting five observations with replacement from each stratum. In a first resampling run of 100 samples, candidate models, which include three elements (the variables, the coefficients and the respective fractional polynomial powers), were elicited using the backward elimination algorithm described by Ambler and Royston31, which provides protection against over‐fitting. In a second step, the coefficients of all candidate models were estimated in B = 1000 bootstrap samples: in each sample, a single model was selected using Akaike's Information Criterion. Candidate models were then ordered by their frequency of selection within the 1000 samples, and the five most frequent models were kept for further assessment of goodness of fit.
Assessment of goodness of fit in the complete dataset relied on inspection of residuals with quantile–quantile (q‐q) plots and residuals vs fitted plots. Given that we estimated fetal weight at the time of the last scan using an average model for growth, we investigated the bias of our model for EFW by calculating the mean of percent prediction errors defined by the formula (100 × (EFW − birth weight)/birth weight), for decreasing time‐to‐birth intervals (i.e. from 14 to 0 days). Finally, we also calculated the absolute percent prediction error defined by the mean of the absolute prediction errors.
Construction of reference centiles
The construction of reference centiles was based solely on FGLS data. The sample size was based on pragmatic and statistical considerations; the latter focused on the precision and accuracy of one extreme centile, i.e. the 3rd or 97th centile, and regression‐based reference limits32, 33. We have shown that a sample of 4000 women would obtain a precision of 0.03 SD at the 3rd or 97th centile. Further details on the precision obtained at the 5th or 10th centile by sample size (ranging from 500–6000) have been included in a table in a previous publication34.
The data from all the study sites were pooled to construct the Fetal Growth Standards6, 12, using the same statistical approach adopted by WHO in constructing their Child Growth Standards10. The statistical methods used were based on published recommendations complemented by recent scientific reviews5, 35, 36, 37, 38. Our overall aim was to produce centiles that change smoothly with age and maximize simplicity without compromising model fit.
We explored the following statistical methods: mean and SD method using fractional polynomials25; Cole's lambda (λ), mu (μ), and sigma (σ) (LMS) method39, 40, 41, which estimates three age‐specific parameters (the median (μ), coefficient of variation (σ), and a Box–Cox power transformation at each gestational age to remove skewness (λ), thereby making the data roughly normally distributed); the LMST method (λ, μ, σ, assuming Box–Cox t distribution), which assumes a shifted and scaled (truncated) t distribution to take account of skewness and leptokurtosis42; and the LMSP method (λ, μ, σ, assuming Box–Cox power exponential distribution), which assumes a Box–Cox power exponential distribution to take account of skewness, platykurtosis and leptokurtosis43. Furthermore, to present the curves, we assessed three smoothing techniques: fractional polynomials, cubic splines and penalized splines25, 44, 45.
Using de‐trended q‐q plots (worm plots), significant evidence of deviations from normality was seen so we resorted to using the more complex LMS, LMST and LMSP methods allowing for skewness and kurtosis46.
As most of the women had four to six ultrasound scans, the effect of correlated data within fetuses was investigated. First, in a sensitivity analysis, a random observation time was sampled for each fetus and the modeled centiles in this subset were compared visually with the complete dataset. The approach is justified by the experimental design of the study, which ensures non‐informative observation times47. This analysis showed minimal or no change in estimated centiles (median, 3rd and 97th centiles) over the whole 22–40 weeks' gestational‐age range. Second, we considered mixed‐effect models accounting for repeated measurements within LMS, LMST and LMSP frameworks. This analysis also showed no impact on the estimated centiles. The best fit was found using a three‐parameter Box–Cox Gaussian distribution (i.e. the LMS method) for the response variable with a second‐degree fractional polynomial functional form for gestational age. This method also gives estimated SDs of EFW, allowing estimation of centiles.
Goodness of fit for the overall model was assessed by comparing empirical centiles (calculated per completed week of gestation) with the fitted centiles, using de‐trended q‐q plots of the residuals across gestational age46, and plots of residuals vs fitted values.
All analyses were carried out in R statistical software48 using the Generalised Additive Models for Location, Scale and Shape (GAMLSS) framework49, 50.
RESULTS
To create an EFW formula, the subsets of 2404 babies in the FGLS (n = 1556) and FS (n = 848) who were born within 14 days of the last ultrasound scan were examined (Table 1): 130 (5.4%) were born preterm (< 37 weeks' gestation) and 78 (3.2%) were born term with low birth weight (< 2500 g and ≥ 37 weeks' gestation). The mean time between the last ultrasound scan and birth was 7.7 (range, 0–14) days and was uniformly distributed, except for 0 days (i.e. birth on day of last scan), which occurred in only 34 (1.4%) cases.
Table 1.
Gestational age at birth and birth weight of a subset of babies in the INTERBIO‐21st Fetal Study (FS) and the Fetal Growth Longitudinal Study (FGLS) of the INTERGROWTH‐21st Project who were born within 14 days of last ultrasound scan
| Parameter | FS (n = 848) | FGLS (n = 1556) | Total (n = 2404) |
|---|---|---|---|
| Gestational age at birth | |||
| < 28 weeks | 2 (0.2) | 1 (0.1) | 3 (0.1) |
| 28–32 weeks | 3 (0.4) | 6 (0.4) | 9 (0.4) |
| 32–37 weeks | 56 (6.6) | 62 (4.0) | 118 (4.9) |
| 37–43 weeks | 787 (92.8) | 1487 (95.6) | 2274 (94.6) |
| Birth weight | |||
| < 1000 g | 1 (0.1) | 2 (0.1) | 3 (0.1) |
| 1000–1499 g | 5 (0.6) | 1 (0.1) | 6 (0.2) |
| 1500–1999 g | 9 (1.1) | 15 (1.0) | 24 (1.0) |
| 2000–2499 g | 79 (9.3) | 76 (4.9) | 155 (6.4) |
| ≥ 2500 g | 754 (88.9) | 1462 (94.0) | 2216 (92.2) |
Data are given as n (%).
Following correction for potential growth between the last scan and birth (steps 1–4 in the statistical methods), the actual fetal weight at the time of the last scan was best estimated as a function of AC and HC with the following formula:
where EFW is expressed in g, AC and HC in cm, and the log function designates the natural logarithm.
None of the other covariates including FL, BPD, OFD, gestational age, symphysis–fundus height, amniotic fluid indices or interactions between biometric measurements and gestational age was retained in the selection process. This model suggests a linear relationship between log(EFW) and HC. Despite the negative coefficients, the two terms involving AC describe an increasing sigmoid‐shaped relationship between AC and birth weight (Figure S1) for a fixed HC value of 26 cm (the average value at 28 weeks' gestation6). The relationship between birth weight and HC is plotted in Figure S2, for a fixed AC value of 23 cm (the average at 28 weeks' gestation6).
The performance of the formula for EFW was assessed both by mean and absolute percent prediction errors; mean percent prediction error is used as a measure of potential bias of EFW due to growth between the last scan and birth, while mean absolute prediction error represents the dispersion of the errors. The mean percent prediction error steadily tended towards zero as the time interval between the last scan and birth decreased. Prediction error was −10.7% (95% CI, −12.1 to −9.4%) in babies born exactly 14 days after the last scan (n = 196) and −0.8% (95% CI, −2.3 to 0.6%) in those born within 1 day (n = 198) (Figure S3), showing that our model was unbiased for predicting weight at the time of the last scan and that the correction we applied to compensate for time to birth was appropriate. In the group born within 1 day of the last scan, the mean absolute prediction error was 7.6%, with 80%, 90% and 95% of predicted weights falling within 11%, 14% and 18% of the true birth weight, respectively.
Creation of the international EFW standards was based on the complete FGLS dataset. The gestational age‐specific observed and smoothed centiles for EFW are presented in Figure 1. Similarities between smoothed centile curves (3rd, 50th and 97th centiles) and observed values, assessed by gestational age‐specific comparisons, demonstrated excellent agreement. The overall differences between empirical and smoothed centiles were small, with mean ± SD differences of 16 ± 28 g, 13 ± 17 g and 5 ± 33 g for the 3rd, 50th and 97th centiles, respectively.
Figure 1.
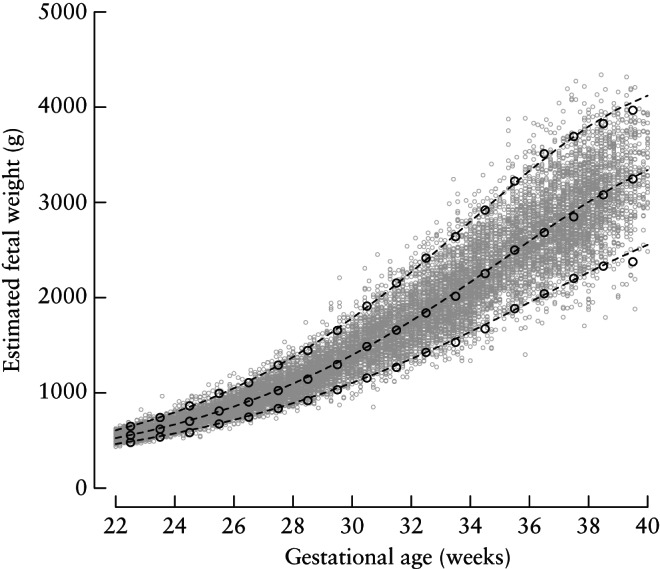
Empirical ( ) and smoothed (
) and smoothed ( ) 3rd, 50th and 97th centiles for estimated fetal weight between 22 and 40 weeks' gestation.
) 3rd, 50th and 97th centiles for estimated fetal weight between 22 and 40 weeks' gestation.
The 3rd, 10th, 50th, 90th and 97th fitted centile curves for EFW according to gestational age, which represent the international standards, are presented in Figure 2. The corresponding equations for λ(t), μ(t) and σ(t), are presented in Table 2, allowing readers to calculate Z‐scores. By estimating the EFW and knowing the gestational age, desired centiles can be calculated. For example, if AC = 26 cm and HC = 29 cm, at 30 + 0 weeks:
Therefore, EFW = exp(7.312292) = 1499 g.
Figure 2.
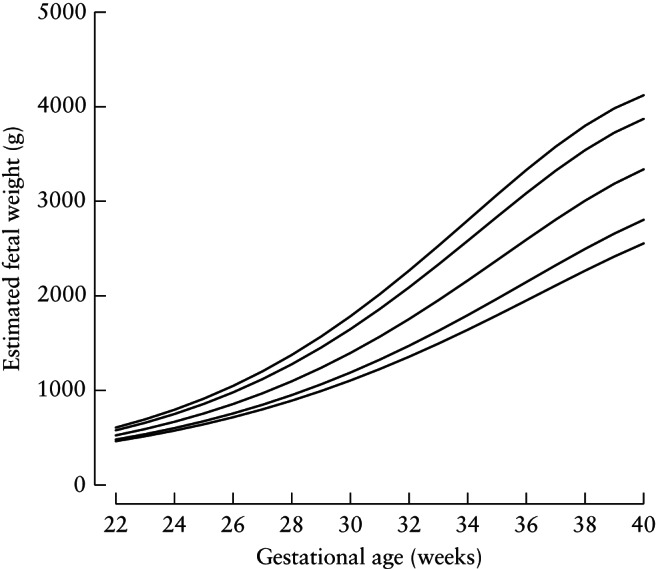
Smoothed 3rd, 10th, 50th, 90th and 97th centile curves for estimated fetal weight.
Table 2.
Equations for parameters and computation of Z‐scores and centiles for estimated fetal weight (EFW) in relation to gestational age (GA) in exact weeks
| Parameter | Equation |
|---|---|
| Skewness | λ(GA) = − 4.257629 − 2162.234 × GA− 2 + 0.0002301829 × GA3 |
| Mean | μ(GA) = 4.956737 + 0.0005019687 × GA3 − 0.0001227065 × GA3 × log(GA) |
| Coefficient of variation | σ(GA) = 10− 4 × (− 6.997171 + 0.057559 × GA3 − 0.01493946 × GA3 × log(GA)) |
| Z‐score | Y = log(EFW) |
| If λ(GA) = 0, Z(GA) = σ(GA)− 1 × log[Y/μ(GA)] | |
| If λ(GA) ≠ 0, Z(GA) = [σ(GA) × λ(GA)]− 1 × [(Y/μ(GA))λ(GA) − 1] | |
| Centiles | Zαdefined by Pr(z ≤ Zα) = α for z ∼ N(0, 1), i. e. Zα = Φ− 1(α) |
| If λ(GA) = 0, log[Cα(GA)] = μ(GA) × exp[σ(GA) × Zα] | |
| If λ(GA) ≠ 0, log[Cα(GA)] = μ(GA) × [Zα × σ(GA) × λ(GA) + 1]1/λ(GA) |
To compute the corresponding Z‐score at 30 weeks' gestation, using the equations in Table 2 we must first calculate:
Finally,
Similarly, the 3rd centile (α = 0.03), i.e. Z = −1.88 at 30 + 0 weeks, is calculated as follows using the equations in Table 2:
 |
The 3rd centile for EFW at 30 weeks' gestation is therefore: C0.03(30) = exp(7.008552) = 1106 g.
The actual values for the 3rd, 10th, 50th, 90th and 97th centiles according to gestational age are presented in Table S1.
DISCUSSION
The INTERGROWTH‐21st Project provides standards for early human growth based on populations that conform to the prescriptive approach recommended by the WHO21, 51. By prescriptive, we mean that we observed a cohort of prospectively enrolled women whose risk of adverse maternal and perinatal outcomes (including fetal growth restriction) was low, based on their individual clinical profiles and the socioeconomic and demographic characteristics of the underlying geographically diverse populations. In fact, the INTERGROWTH‐21st Project is unique because it has produced, for the first time, fetal ultrasound, newborn size and preterm postnatal growth datasets that have all been collected from the same underlying populations using the same rigorously applied methodologies.
We now present international EFW standards to complement the existing set, along with a formula for EFW based on HC and AC. Compared with several previous formulae24, we found that FL did not improve the EFW, which agrees with previous work, in particular in growth‐restricted fetuses52. Furthermore, it is likely that incorporating FL into the formula would increase the prediction error, as its measurement is associated with the highest inter‐ and intraobserver variability compared with AC and HC53.
Unusually, we lowered the starting gestational age to 22 weeks, 2 weeks below the customary cut‐off of 24 weeks' gestation for viability, for two reasons: to facilitate early recognition of fetal growth restriction around the recommended time of the second‐trimester anatomy scan and to anticipate a possible extension of the limit of viability54, 55.
At the upper end of gestation, the centiles closely match those of the INTERGROWTH‐21st Newborn Size Standards at 40 weeks7. The 3rd, 50th and 97th EFW centiles at 40 weeks are 2554 g, 3338 g and 4121 g, respectively (Table S1), whereas for newborns (sexes combined) they are 2591 g, 3321 g and 4154 g, respectively (Figure S4). These similarities between fetal‐ and birth‐weight centiles suggest that our model is valid for developing a formula for EFW using ultrasound biometry.
In contrast, there are significant discrepancies earlier in pregnancy (Figure 3). For example, at 33 weeks' gestation, the 3rd, 50th and 97th EFW centiles are 1495 g, 1954 g and 2529 g, respectively (Table S1); for newborns (sexes combined), they are 1190 g, 1903 g and 2715 g, respectively. It is possible that these differences are due to an overrepresentation of small, as well as, to a lesser extent, large babies in preterm births, even in the selected pregnant and newborn populations we studied.
Figure 3.
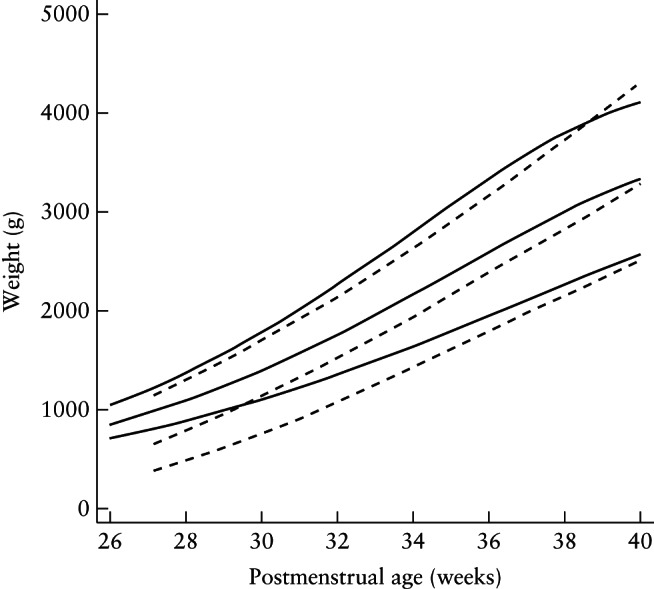
Comparison of fitted 3rd, 50th and 97th centiles for estimated fetal weight ( ) with those of INTERGROWTH‐21st preterm postnatal weight, with both sexes combined (
) with those of INTERGROWTH‐21st preterm postnatal weight, with both sexes combined ( ).
).
The EFW formula and standards we present are also unique because we avoided the many common limitations identified by previous reviews5, 24: retrospective design; use of routinely obtained measurements; suboptimal pregnancy dating strategies; variable time‐to‐birth without controlling for bias; absence of prospective ultrasound quality control, standardization and calibration of equipment; hospital‐based sampling; absence of sampling from a healthy, well‐nourished, underlying population; and no blinding of measurements.
Conversely, our standards are prescriptive, whereas reference charts describe only fetal size at a given place and time. The standards were derived prospectively, population‐based and multinational. We have shown (using several analytical strategies) that the eight populations were consistently similar and could be pooled to create international standards51. Uniform research methods, protocols, processes and measurement tools were used throughout; these were combined with standardized identical equipment, training, a centralized electronic data management system and close monitoring of staff. The analytical approach aimed at identifying and correcting potential biases, and followed WHO recommendations to present the observed and smoothed data and explore the best fitting model with an a‐priori strategy56.
Using ultrasound, we examined separately HC, AC and FL, providing a comprehensive evaluation of structures that have different growth patterns; these measurements are often combined to calculate EFW. There are advantages in using a summary approximation: it is the most commonly measured marker of size at birth; as birth weight is associated with morbidity and mortality, it is helpful when counseling parents and enables pediatricians to make management decisions57; it may also help to refine the management of large babies.
However, there are also disadvantages in using only a single summary measure of size: first, there is a loss of the most granular information available when using the individual measurements, in terms of fetal skeletal and fat‐based growth. Second, the fact that the individual measurement errors are compounded means that estimation is prone to inaccuracy; previous studies have shown that 95% prediction intervals for random error are in the region of ± 14% of birth weight, and this is a particular problem in low‐ and high‐birth‐weight babies24. Finally, as for other ultrasound measurements, there are numerous locally‐derived EFW equations and reference charts24 but, until now, no international standards existed, unlike the situation for newborn size and infant growth7, 8, 10. This may be, at least partly, responsible for the poor efficiency of screening strategies using biometry and EFW58.
Therefore, we strongly recommend that, for clinical use, all individual fetal measurements, together with the summary measure of EFW, should be used together to make clinical decisions. In perinatal medicine, there is no room for a quick, minimalist approach that might lead to the early delivery of an at‐risk fetus. Finally, implementation of the standards may raise concerns regarding the generalizability of data originating from a limited number of sites and/or a highly selected, low‐risk population. As we have argued previously11, having separate standards for a given country, institution or ethnic group has no biological basis and makes little sense in modern, multicultural societies. The international INTERGROWTH‐21st standards describe optimal growth and can be used to assess both individuals and populations.
Supporting information
Appendix S1 Members of the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st and INTERBIO‐21st) and its Committees
Figure S1 Relationship between fetal weight and abdominal circumference in the final model, plotted for a fixed head circumference of 26 cm.
Figure S2 Relationship between fetal weight and head circumference in the final model, plotted for a fixed abdominal circumference of 23 cm.
Figure S3 Bias in estimation of fetal weight as a function of time to birth, showing mean percent prediction error and 95% CI according to time between last ultrasound scan and birth.
Figure S4 Gestational age‐specific centiles for estimated fetal weight (blue) and birth weight (red). 3rd, 10th, 50th, 90th and 97th centiles are shown.
Table S1 Estimated fetal weight per completed week of gestation at 3rd, 10th, 50th, 90th and 97th centiles
ACKNOWLEDGMENTS
This project was supported by a generous grant from the Bill & Melinda Gates Foundation to the University of Oxford, for which we are very grateful. We would also like to thank the Health Authorities in Pelotas, Brazil; Beijing, China; Nagpur, India; Turin, Italy; Nairobi, Kenya; Kilifi, Kenya; Muscat, Oman; Karachi, Pakistan; Johannesburg, South Africa; Mae Sot, Thailand; Oxford, UK and Seattle, USA, who facilitated the project by allowing participation of these study sites as collaborating centers. We are extremely grateful to Philips Medical Systems, who provided the ultrasound equipment and technical assistance throughout the project. We also thank MedSciNet UK Ltd for setting up the INTERGROWTH‐21st and INTERBIO‐21st websites and for the development, maintenance and support of the online data management system. We are indebted to GAPPS for the supply of sample processing kits for INTERBIO‐21st.
We thank the parents and infants who participated in the studies and the more than 200 members of the research teams who made the implementation of this project possible. The participating hospitals included: Brazil, Pelotas (Hospital Miguel Piltcher, Hospital São Francisco de Paula, Santa Casa de Misericórdia de Pelotas, and Hospital Escola da Universidade Federal de Pelotas); China, Beijing (Beijing Obstetrics & Gynecology Hospital, Shunyi Maternal & Child Health Centre, and Shunyi General Hospital); India, Nagpur (Ketkar Hospital, Avanti Institute of Cardiology Private Limited, Avantika Hospital, Gurukrupa Maternity Hospital, Mulik Hospital & Research Centre, Nandlok Hospital, Om Women's Hospital, Renuka Hospital & Maternity Home, Saboo Hospital, Brajmonhan Taori Memorial Hospital, and Somani Nursing Home); Italy, Turin (Ospedale Infantile Regina Margherita Sant' Anna and Azienda Ospedaliera Ordine Mauriziano); Kenya, Nairobi (Aga Khan University Hospital, MP Shah Hospital and Avenue Hospital); Kenya, Kilifi, (The Kilifi District Hospital); Oman, Muscat (Khoula Hospital, Royal Hospital, Wattayah Obstetrics & Gynaecology Poly Clinic, Wattayah Health Centre, Ruwi Health Centre, Al‐Ghoubra Health Centre and Al‐Khuwair Health Centre); Pakistan, Karachi (Aga Khan Hospital); South Africa, Johannesburg (Chris Hani Baragwanath Academic Hospital); Thailand, Mae Sot (Maela , Wang Pha, and Mawker Thai Clinics); UK, Oxford (John Radcliffe Hospital) and USA, Seattle (University of Washington Hospital, Swedish Hospital, and Providence Everett Hospital). Members of the INTERGROWTH‐21st and its committees are listed in Appendix S1. Full acknowledgement of all those who contributed to the development of the INTERGROWTH‐21st Project protocol appears at www.intergrowth21.org.uk and www.interbio21.org.uk.
Contributor Information
A. T. Papageorghiou, Email: aris.papageorghiou@obs-gyn.ox.ac.uk.
for the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st):
Scientific Advisory Committee, M Katz, MK Bhan, C Garza, S Zaidi, A Langer, PM Rothwell, Sir D Weatherall, Steering Committees, INTERGROWTH‐21st, ZA Bhutta, J Villar, S Kennedy, DG Altman, FC Barros, E Bertino, F Burton, M Carvalho, L Cheikh Ismail, WC Chumlea, MG Gravett, YA Jaffer, A Lambert, P Lumbiganon, JA Noble, RY Pang, AT Papageorghiou, M Purwar, J Rivera, C Victora, INTERBIO‐21st, R Uauy, S Kennedy, J Villar, DG Altman, FC Barros, J Berkley, F Burton, M Carvalho, L Cheikh Ismail, WC Chumlea, A Lambert, S Munim, S Norris, F Nosten, AT Papageorghiou, C Victora, Executive Committee, J Villar, DG Altman, L Cheikh Ismail, S Kennedy, A Lambert, JA Noble, AT Papageorghiou, ZA Bhutta, In addition for INTERBIO 21st, R Craik, R Uauy, Project Coordinating Unit, J Villar, L Cheikh Ismail, S Kennedy, A Lambert, AT Papageorghiou, M Shorten, L Hoch, HE Knight, EO Ohuma, C Cosgrove, I Blakey, S Ash, R Craik, Data Analysis Group, DG Altman, EO Ohuma, E Staines Urias, J Villar, Data Management Group, DG Altman, F Roseman, N Kunnawar, SH Gu, JH Wang, MH Wu, M Domingues, P Gilli, L Juodvirsiene, L Hoch, N Musee, H Al‐Jabri, S Waller, C Cosgrove, D Muninzwa, EO Ohuma, D Yellappan, A Carter, D Reade, R Miller, In addition for INTERBIO 21st, I Ahmed, S Ash, C Condon, M Mainwaring, D Muninzwa, MF da Silveira, E Staines Urias, L Walusuna, S Wiladphaingern, Ultrasound Group, AT Papageorghiou, L Salomon, A Leston, A Mitidieri, F Al‐Aamri, W Paulsene, J Sande, WKS Al‐Zadjali, C Batiuk, S Bornemeier, M Carvalho, M Dighe, P Gaglioti, N Jacinta, S Jaiswal, JA Noble, K Oas, M Oberto, E Olearo, MG Owende, J Shah, S Sohoni, T Todros, M Venkataraman, S Vinayak, L Wang, D Wilson, QQ Wu, S Zaidi, Y Zhang, P Chamberlain, D Danelon, I Sarris, J Dhami, C Ioannou, CL Knight, R Napolitano, S Wanyonyi, C Pace, V Mkrtychyan, In addition for INTERBIO‐21st:, M Buckle, N Jackson, A Mitidieri, S Munim, H Mwangudzah, T Norris, J Shah, G Zainab, Anthropometry Group, L Cheikh Ismail, WC Chumlea, F Al‐Habsi, ZA Bhutta, A Carter, M Alija, JM Jimenez‐Bustos, J Kizidio, F Puglia, N Kunnawar, H Liu, S Lloyd, D Mota, R Ochieng, C Rossi, M Sanchez Luna, YJ Shen, HE Knight, DA Rocco, IO Frederick, In addition for INTERBIO‐21st:, J Kizidio, B Monyepote, M Salim, R Salam, VI Carrara, Laboratory Processing Group, R Craik, D Alam, Y Guman, J Kilonzo, A Min, V Ngami, I Olivera, G Deutsch, Neonatal Group, ZA Bhutta, E Albernaz, M Batra, BA Bhat, E Bertino, P Di Nicola, F Giuliani, I Rovelli, K McCormick, R Ochieng, RY Pang, V Paul, V Rajan, A Wilkinson, R Uauy, A Varalda, Environmental Health Group, B Eskenazi, A Bradman, O Burnham, LA Corra, H Dolk, F Farhi, D Finkton, J Golding, A Matijasevich, T de Wet, J Villar, JJ Zhang, Neurodevelopment Group, A Stein, M Fernandes, A Abubakar, J Acedo, L Aranzeta, L Cheikh Ismail, F Giuliani, D Ibanez, S Kennedy, M Kihara, E de Leon, CR Newton, S Savini, A Soria‐Frisch, J Villar, K Wulff, Participating countries and local investigators, FC Barros, M Domingues, S Fonseca, A Leston, A Mitidieri, D Mota, IK Sclowitz, MF da Silveira, RY Pang, YP He, Y Pan, YJ Shen, MH Wu, QQ Wu, JH Wang, Y Yuan, Y Zhang, M Purwar, A Choudhary, S Choudhary, S Deshmukh, D Dongaonkar, M Ketkar, V Khedikar, N Kunnawar, C Mahorkar, I Mulik, K Saboo, C Shembekar, A Singh, V Taori, K Tayade, A Somani, E Bertino, P Di Nicola, M Frigerio, G Gilli, P Gilli, M Giolito, F Giuliani, M Oberto, L Occhi, C Rossi, I Rovelli, F Signorile, T Todros, W Stones, M Carvalho, J Kizidio, R Ochieng, J Shah, S Vinayak, N Musee, C Kisiang'ani, D Muninzwa, In addition for INTERBIO‐21st:, J Kilonzo, J Sande, J Berkley, B Kemp, H Barsosio, S Mwakio, H Mwangudzah, V Ngami, M Salim, A Seale, L Walusuna, YA Jaffer, J Al‐Abri, J Al‐Abduwani, FM Al‐Habsi, H Al‐Lawatiya, B Al‐Rashidiya, WKS Al‐Zadjali, FR Juangco, M Venkataraman, H Al‐Jabri, D Yellappan, S Munim, G Zainab, I Ahmed, D Alam, A Raza, R Salam, S Norris, Y Guman, T Lephoto, S Macauley, L Malgas, F Nosten, N Jackson, R McGready, A Min, VI Cararra, S Wiladphaingern, S Kennedy, L Cheikh Ismail, A Lambert, S Lloyd, R Napolitano, EO Ohuma, AT Papageorghiou, B Patel, F Puglia, F Roseman, S Roseman, C Ioannou, I Sarris, In addition for INTERBIO‐21st:, S Ash, M Baricco, A Capp, R Craik, S Hussein, A Laister, T Lewis, E Maggiora, T Norris, M Sharps, A Varalda, R Carew, MG Gravett, C Batiuk, M Batra, S Bornemeier, M Dighe, K Oas, W Paulsene, D Wilson, IO Frederick, HF Andersen, SE Abbott, AA Carter, H Algren, DA Rocco, TK Sorensen, D Enquobahrie, and S Waller
REFERENCES
- 1. de Onis M, Habicht J‐P. Anthropometric reference data for international use: recommendations from a World Health Organization Expert Committee. Am J Clin Nutr 1996; 64: 650–658. [DOI] [PubMed] [Google Scholar]
- 2. Bakalis S, Peeva G, Gonzalez R, Poon LC, Nicolaides KH. Prediction of small‐for‐gestational‐age neonates: screening by biophysical and biochemical markers at 30–34 weeks. Ultrasound Obstet Gynecol 2015; 46: 446–451. [DOI] [PubMed] [Google Scholar]
- 3. Lesmes C, Gallo DM, Gonzalez R, Poon LC, Nicolaides KH. Prediction of small‐for‐gestational‐age neonates: screening by maternal serum biochemical markers at 19–24 weeks. Ultrasound Obstet Gynecol 2015; 46: 341–349. [DOI] [PubMed] [Google Scholar]
- 4. Conde‐Agudelo A, Papageorghiou AT, Kennedy SH, Villar J. Novel biomarkers for predicting intrauterine growth restriction: a systematic review and meta‐analysis. BJOG 2013; 120: 681–694. [DOI] [PubMed] [Google Scholar]
- 5. Ioannou C, Talbot K, Ohuma E, Sarris I, Villar J, Conde‐Agudelo A, Papageorghiou AT. Systematic review of methodology used in ultrasound studies aimed at creating charts of fetal size. BJOG 2012; 119: 1425–1439. [DOI] [PubMed] [Google Scholar]
- 6. Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Cheikh Ismail L, Lambert A, Jaffer YA, Bertino E, Gravett MG, Purwar M, Noble JA, Pang R, Victora CG, Barros FC, Carvalho M, Salomon LJ, Bhutta ZA, Kennedy SH, Villar J; International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st) . International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH‐21st Project. Lancet 2014; 384: 869–879. [DOI] [PubMed] [Google Scholar]
- 7. Villar J, Ismail LC, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Gravett MG, Purwar M, Frederick IO, Noble AJ, Pang R, Barros FC, Chumlea C, Bhutta ZA, Kennedy SH. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross‐Sectional Study of the INTERGROWTH‐21st Project. Lancet 2014; 384: 857–868. [DOI] [PubMed] [Google Scholar]
- 8. Villar J, Giuliani F, Bhutta ZA, Bertino E, Ohuma EO, Ismail LC, Barros FC, Altman DG, Victora C, Noble JA, Gravett MG, Purwar M, Pang R, Lambert A, Papageorghiou AT, Ochieng R, Jaffer YA, Kennedy SH; International Fetal and Newborn Growth Consortium for the 21(st) Century (INTERGROWTH‐21(st)). Postnatal growth standards for preterm infants: the Preterm Postnatal Follow‐up Study of the INTERGROWTH‐21(st) Project. Lancet Glob Health 2015; 3: e681–691. [DOI] [PubMed] [Google Scholar]
- 9. Villar J, Altman DG, Purwar M, Noble JA, Knight HE, Ruyan P, Cheikh Ismail L, Barros FC, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Bertino E, Gravett MG, Bhutta ZA, Kennedy SH; International Fetal and Newborn Growth Consortium for the 21st Century . The objectives, design and implementation of the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 9–26. [DOI] [PubMed] [Google Scholar]
- 10. Onis M de, Garza C, Onyango AW, Martorell R. WHO | Acta Paediatrica supplement on the WHO Child Growth Standards. WHO. http://www.who.int/childgrowth/standards/acta_supplement/en/. Published 2006.
- 11. Villar J, Papageorghiou AT, Pang R, Salomon LJ, Langer A, Victora C, Purwar M, Chumlea C, Qingqing W, Scherjon SA, Barros FC, Carvalho M, Altman DG, Giuliani F, Bertino E, Jaffer YA, Cheikh Ismail L, Ohuma EO, Lambert A, Noble JA, Gravett MG, Bhutta ZA, Kennedy SH. Monitoring human growth and development: a continuum from the womb to the classroom. Am J Obstet Gynecol 2015; 213: 494–499. [DOI] [PubMed] [Google Scholar]
- 12. Villar J, Papageorghiou AT, Pang R, Ohuma EO, Cheikh Ismail L, Barros FC, Lambert A, Carvalho M, Jaffer YA, Bertino E, Gravett MG, Altman DG, Purwar M, Frederick IO, Noble JA, Victora CG, Bhutta ZA, Kennedy SH; International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st) . The likeness of fetal growth and newborn size across non‐isolated populations in the INTERGROWTH‐21st Project: the Fetal Growth Longitudinal Study and Newborn Cross‐Sectional Study. Lancet Diabetes Endocrinol 2014; 2: 781–792. [DOI] [PubMed] [Google Scholar]
- 13. Ioannou C, Sarris I, Hoch L, Salomon LJ, Papageorghiou AT; International Fetal and Newborn Growth Consortium for the 21st Century . Standardisation of crown–rump length measurement. BJOG 2013; 120 (Suppl 2): 38–41. [DOI] [PubMed] [Google Scholar]
- 14. Wanyonyi SZ, Napolitano R, Ohuma EO, Salomon LJ, Papageorghiou AT. Image‐scoring system for crown–rump length measurement. Ultrasound Obstet Gynecol 2014; 44: 649–654. [DOI] [PubMed] [Google Scholar]
- 15. Robinson HP, Fleming JE. A critical evaluation of sonar “crown–rump length” measurements. Br J Obstet Gynaecol 1975; 82: 702–710. [DOI] [PubMed] [Google Scholar]
- 16. Papageorghiou AT, Sarris I, Ioannou C, Todros T, Carvalho M, Pilu G, Salomon LJ; International Fetal and Newborn Growth Consortium for the 21st Century . Ultrasound methodology used to construct the fetal growth standards in the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 27–32. [DOI] [PubMed] [Google Scholar]
- 17. Ohuma EO, Hoch L, Cosgrove C, Knight HE, Cheikh Ismail L, Juodvirsiene L, Papageorghiou AT, Al‐Jabri H, Domingues M, Gilli P, Kunnawar N, Musee N, Roseman F, Carter A, Wu M, Altman DG; International Fetal and Newborn Growth Consortium for the 21st Century . Managing data for the international, multicentre INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 64–70. [DOI] [PubMed] [Google Scholar]
- 18. Sarris I, Ioannou C, Ohuma EO, Altman DG, Hoch L, Cosgrove C, Fathima S, Salomon LJ, Papageorghiou AT; International Fetal and Newborn Growth Consortium for the 21st Century . Standardisation and quality control of ultrasound measurements taken in the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 33–37. [DOI] [PubMed] [Google Scholar]
- 19. Salomon LJ, Bernard JP, Duyme M, Doris B, Mas N, Ville Y. Feasibility and reproducibility of an image‐scoring method for quality control of fetal biometry in the second trimester. Ultrasound Obstet Gynecol 2006; 27: 34–40. [DOI] [PubMed] [Google Scholar]
- 20. Sarris I, Ioannou C, Dighe M, Mitidieri A, Oberto M, Qingqing W, Shah J, Sohoni S, Al Zidjali W, Hoch L, Altman DG, Papageorghiou AT; International Fetal and Newborn Growth Consortium for the 21st Century . Standardization of fetal ultrasound biometry measurements: improving the quality and consistency of measurements. Ultrasound Obstet Gynecol 2011; 38: 681–687. [DOI] [PubMed] [Google Scholar]
- 21. de Onis M, Onyango AW, Van den Broeck J, Chumlea WC, Martorell R. Measurement and standardization protocols for anthropometry used in the construction of a new international growth reference. Food Nutr Bull 2004; 25 (1 Suppl): S27–S36. [DOI] [PubMed] [Google Scholar]
- 22. Cheikh Ismail L, Knight HE, Ohuma EO, Hoch L, Chumlea WC; International Fetal and Newborn Growth Consortium for the 21st Century . Anthropometric standardisation and quality control protocols for the construction of new, international, fetal and newborn growth standards: the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cheikh Ismail L, Knight HE, Bhutta Z, Chumlea WC; International Fetal and Newborn Growth Consortium for the 21st Century . Anthropometric protocols for the construction of new international fetal and newborn growth standards: the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dudley NJ. A systematic review of the ultrasound estimation of fetal weight. Ultrasound Obstet Gynecol 2005; 25: 80–89. [DOI] [PubMed] [Google Scholar]
- 25. Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. Appl Stat 1994; 43: 429–467. [Google Scholar]
- 26. Kurmanavicius J, Burkhardt T, Wisser J, Huch R. Ultrasonographic fetal weight estimation: accuracy of formulas and accuracy of examiners by birth weight from 500 to 5000 g. J Perinat Med 2004; 32: 155–161. [DOI] [PubMed] [Google Scholar]
- 27. Cohen JM, Hutcheon JA, Kramer MS, Joseph KS, Abenhaim H, Platt RW. Influence of ultrasound‐to‐delivery interval and maternal–fetal characteristics on validity of estimated fetal weight. Ultrasound Obstet Gynecol 2010; 35: 434–441. [DOI] [PubMed] [Google Scholar]
- 28. Efron B, Tibshirani RJ. An Introduction to the Bootstrap. CRC Press, 1994. [Google Scholar]
- 29. Sauerbrei W. The use of resampling methods to simplify regression models in medical statistics. J R Stat Soc Ser C Appl Stat 1999; 48: 313–329. [Google Scholar]
- 30. Bland JM, Altman DG. Statistics Notes: Bootstrap resampling methods. BMJ 2015; 350: h2622. [DOI] [PubMed] [Google Scholar]
- 31. Ambler G, Royston P. Fractional polynomial model selection procedures: investigation of Type I error rate. J Stat Comput Simul 2001; 69: 89–108. [Google Scholar]
- 32. Bellera CA, Hanley JA. A method is presented to plan the required sample size when estimating regression‐based reference limits. J Clin Epidemiol 2007; 60: 610–615. [DOI] [PubMed] [Google Scholar]
- 33. Royston P. Constructing time‐specific reference ranges. Stat Med 1991; 10: 675–690. [DOI] [PubMed] [Google Scholar]
- 34. Altman DG, Ohuma EO; International Fetal and Newborn Growth Consortium for the 21st Century . Statistical considerations for the development of prescriptive fetal and newborn growth standards in the INTERGROWTH‐21st Project. BJOG 2013; 120 (Suppl 2): 71–76. [DOI] [PubMed] [Google Scholar]
- 35. Altman DG, Chitty LS. Design and analysis of studies to derive charts of fetal size. Ultrasound Obstet Gynecol 1993; 3: 378–384. [DOI] [PubMed] [Google Scholar]
- 36. Royston P, Altman DG. Design and analysis of longitudinal studies of fetal size. Ultrasound Obstet Gynecol 1995; 6: 307–312. [DOI] [PubMed] [Google Scholar]
- 37. Wright EM, Royston P. A comparison of statistical methods for age‐related reference intervals. J R Stat Soc Ser A Stat Soc 1997; 160: 47–69. [Google Scholar]
- 38. Hynek M. Approaches for constructing age‐related reference intervals and centile charts for fetal size. Eur J Biomed Inform 2010; 6: 51–60. [Google Scholar]
- 39. Cole TJ. Fitting smoothed centile curves to reference data. J R Stat Soc Ser A Stat Soc 1988; 151: 385–418. [Google Scholar]
- 40. Cole TJ. Using the LMS method to measure skewness in the NCHS and Dutch National height standards. Ann Hum Biol 1989; 16: 407–419. [DOI] [PubMed] [Google Scholar]
- 41. Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 1992; 11: 1305–1319. [DOI] [PubMed] [Google Scholar]
- 42. Rigby RA, Stasinopoulos DM. Using the Box–Cox t distribution in GAMLSS to model skewness and kurtosis. Stat Model 2006; 6: 209–229. [Google Scholar]
- 43. Rigby RA, Stasinopoulos DM. Smooth centile curves for skew and kurtotic data modelled using the Box–Cox power exponential distribution. Stat Med 2004; 23: 3053–3076. [DOI] [PubMed] [Google Scholar]
- 44. Green PJ, Silverman BW. Nonparametric Regression and Generalized Linear Models: A Roughness Penalty Approach. CRC Press, 1993. [Google Scholar]
- 45. Eilers PHC, Marx BD. Flexible smoothing with B‐splines and penalties. Stat Sci 1996; 11: 89–121. [Google Scholar]
- 46. van Buuren S, Fredriks M. Worm plot: a simple diagnostic device for modelling growth reference curves. Stat Med 2001; 20: 1259–1277. [DOI] [PubMed] [Google Scholar]
- 47. Wade A, Kurmanavicius J. Creating unbiased cross‐sectional covariate‐related reference ranges from serial correlated measurements. Biostatistics 2009; 10: 147–154. [DOI] [PubMed] [Google Scholar]
- 48. R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. https://www.R-project.org. [Google Scholar]
- 49. Rigby RA, Stasinopoulos DM. Generalized additive models for location, scale and shape. J R Stat Soc Ser C Appl Stat 2005; 54: 507–554. [Google Scholar]
- 50. Stasinopoulos DM, Rigby RA. Generalized additive models for location scale and shape (GAMLSS) in R. J Stat Software 2007; 23: 1–46. [Google Scholar]
- 51. Garza C, de Onis M. Rationale for developing a new international growth reference. Food Nutr Bull 2004; 25 (1 Suppl): S5–S14. [DOI] [PubMed] [Google Scholar]
- 52. Proctor LK, Rushworth V, Shah PS, Keunen J, Windrim R, Ryan G, Kingdom J. Incorporation of femur length leads to underestimation of fetal weight in asymmetric preterm growth restriction. Ultrasound Obstet Gynecol 2010; 35: 442–448. [DOI] [PubMed] [Google Scholar]
- 53. Sarris I, Ioannou C, Chamberlain P, Ohuma E, Roseman F, Hoch L, Altman DG, Papageorghiou AT; International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st) . Intra‐ and interobserver variability in fetal ultrasound measurements. Ultrasound Obstet Gynecol 2012; 39: 266–273. [DOI] [PubMed] [Google Scholar]
- 54. Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Hernandez‐Andrade E, Johnsen SL, Kalache K, Leung KY, Malinger G, Munoz H, Prefumo F, Toi A, Lee W; ISUOG Clinical Standards Committee . Practice guidelines for performance of the routine mid‐trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 2011; 37: 116–126. [DOI] [PubMed] [Google Scholar]
- 55. Pignotti MS, Donzelli G. Perinatal care at the threshold of viability: an international comparison of practical guidelines for the treatment of extremely preterm births. Pediatrics 2008; 121: e193–198. [DOI] [PubMed] [Google Scholar]
- 56. Borghi E, de Onis M, Garza C, Van den Broeck J, Frongillo EA, Grummer‐Strawn L, Van Buuren S, Pan H, Molinari L, Martorell R, Onyango AW, Martines JC. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med 2006; 25: 247–265. [DOI] [PubMed] [Google Scholar]
- 57. Medchill MT, Peterson CM, Kreinick C, Garbaciak J. Prediction of estimated fetal weight in extremely low birth weight neonates (500–1000 g). Obstet Gynecol 1991; 78: 286–290. [PubMed] [Google Scholar]
- 58. Stirnemann JJ, Benoist G, Salomon LJ, Bernard J‐P, Ville Y. Optimal risk assessment of small‐for‐gestational‐age fetuses using 31–34‐week biometry in a low‐risk population. Ultrasound Obstet Gynecol 2014; 43: 311–316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Members of the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH‐21st and INTERBIO‐21st) and its Committees
Figure S1 Relationship between fetal weight and abdominal circumference in the final model, plotted for a fixed head circumference of 26 cm.
Figure S2 Relationship between fetal weight and head circumference in the final model, plotted for a fixed abdominal circumference of 23 cm.
Figure S3 Bias in estimation of fetal weight as a function of time to birth, showing mean percent prediction error and 95% CI according to time between last ultrasound scan and birth.
Figure S4 Gestational age‐specific centiles for estimated fetal weight (blue) and birth weight (red). 3rd, 10th, 50th, 90th and 97th centiles are shown.
Table S1 Estimated fetal weight per completed week of gestation at 3rd, 10th, 50th, 90th and 97th centiles


